Abstract
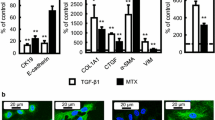
Methotrexate (MTX) is widely used to treat various diseases. However, it induces adverse reactions like serious lung injury, including pulmonary fibrosis. Increasing evidence suggests that epithelial-mesenchymal transition (EMT) in injured alveolar epithelium contributes to the development of the pathophysiological state of the lung. We demonstrated that MTX induced EMT in cultured alveolar epithelial cell lines. Integrin-mediated signaling is considered a significant factor in recognizing the EMT process. However, the relationship between MTX-induced EMT and integrin family members is poorly understood. In the present study, we aimed to clarify the role of integrin in MTX-induced EMT in A549 and NCI-H1299 (H1299) cells by focusing on the integrin alpha 2 (ITGA2) subunit, selected based on our microarray analysis. MTX treatment for 72 h significantly increased the mRNA and cell surface expression of ITGA2 in both cell lines. However, this upregulation by MTX was suppressed by co-treatment with SB431542 and folic acid, which are inhibitors of MTX-induced EMT in A549 cells. The mRNA expression levels of EMT-related genes were more affected in the MTX-treated A549 cells with high ITGA2 expression than in those with low ITGA2 expression. Finally, E7820, an ITGA2 inhibitor, suppressed MTX-induced EMT-related phenotypic changes, such as morphology and mRNA and protein expression of α-smooth muscle actin, a representative EMT marker. These findings suggest that ITGA2 may play a key role in MTX-induced EMT in alveolar epithelial cells.






Similar content being viewed by others
References
Koźmiński P, Halik PK, Chesori R, Gniazdowska E (2020) Overview of dual-acting drug methotrexate in different neurological diseases, autoimmune pathologies and cancers. Int J Mol Sci 14:3483. https://doi.org/10.3390/ijms21103483
Cronstein BN (2005) Low-dose methotrexate: a mainstay in the treatment of rheumatoid arthritis. Pharmacol Rev 57:163–172. https://doi.org/10.1124/pr.57.2.3
Chou RC, Kane M, Ghimire S, Gautam S, Gui J (2016) Treatment for rheumatoid arthritis and risk of alzheimer’s disease: a nested case-control analysis. CNS Drugs 30:1111–1120. https://doi.org/10.1007/s40263-016-0374-z
Zhou M, Xu R, Kaelber DC, Gurney ME (2020) Tumor Necrosis Factor (TNF) blocking agents are associated with lower risk for Alzheimer’s disease in patients with rheumatoid arthritis and psoriasis. PLoS ONE 15:e0229819. https://doi.org/10.1371/journal.pone.0229819
Karadag AS, Kanbay A, Ozlu E, Uzuncakmak TK, Gedik C, Akdeniz N (2015) Pulmonary fibrosis developed secondary to methotrexate use in a patient with psoriasis vulgaris. North Clin Istanbul 2:159–161. https://doi.org/10.14744/nci.2015.97759
Jakubovic BD, Donovan A, Webster PM, Shear NH (2013) Methotrexate-induced pulmonary toxicity. Can Respir J 20:153–155. https://doi.org/10.1155/2013/527912
Imokawa S, Colby TV, Leslie KO, Helmers RA (2000) Methotrexate pneumonitis: review of the literature and histopathological findings in nine patients. Eur Respir J 15:373–381. https://doi.org/10.1034/j.1399-3003.2000.15b25.x
Nieto MA, Huang RY, Jackson RA, Thiery JP (2016) Emt: 2016. Cell 166:21–45. https://doi.org/10.1016/j.cell.2016.06.028
Chen T, You Y, Jiang H, Wang ZZ (2017) Epithelial–mesenchymal transition (EMT): A biological process in the development, stem cell differentiation, and tumorigenesis. J Cell Physiol 232:3261–3272. https://doi.org/10.1002/jcp.25797
Zhang Y, Weinberg RA (2018) Epithelial-to-mesenchymal transition in cancer: complexity and opportunities. Front Med 12:361–373. https://doi.org/10.1007/s11684-018-0656-6
Stone RC, Pastar I, Ojeh N, Chen V, Liu S, Garzon KI, Tomic-Canic M (2016) Epithelial-mesenchymal transition in tissue repair and fibrosis. Cell Tissue Res 365:495–506. https://doi.org/10.1007/s00441-016-2464-0
Salton F, Volpe MC, Confalonieri M (2019) Epithelial-mesenchymal transition in the pathogenesis of idiopathic pulmonary fibrosis. Medicina (Kaunas) 55:83. https://doi.org/10.3390/medicina55040083
Bartis D, Mise N, Mahida RY, Eickelberg O, Thickett DR (2014) Epithelial-mesenchymal transition in lung development and disease: does it exist and is it important? Thorax 69:760–765. https://doi.org/10.1136/thoraxjnl-2013-204608
Kawami M, Harabayashi R, Miyamoto M, Harada R, Yumoto R, Takano M (2016) Methotrexate-induced epithelial–mesenchymal transition in the alveolar epithelial cell line A549. Lung 194:923–930. https://doi.org/10.1007/s00408-016-9935-7
Weng J, Chen H, Wu H, Tu M, Wang Z, Chen D, Wang Z, Chen C (2020) Amiodarone induces epithelial-mesenchymal transition in A549 cells via activation of TGF-β1. Drug Chem Toxicol 43:415–422. https://doi.org/10.1080/01480545.2018.1497055
Weng CM, Li Q, Chen KJ, Xu CX, Deng MS, Li T, Zhang DD, Duan ZX, Chen ZQ, Li GH, Chen J, Wang JM (2020) Bleomycin induces epithelial-to-mesenchymal transition via bFGF/PI3K/ESRP1 signaling in pulmonary fibrosis. Biosci Rep. https://doi.org/10.1042/bsr20190756
Tsukui T, Ueha S, Abe J, Hashimoto S, Shichino S, Shimaoka T, Shand FH, Arakawa Y, Oshima K, Hattori M, Inagaki Y, Tomura M, Matsushima K (2013) Qualitative rather than quantitative changes are hallmarks of fibroblasts in bleomycin-induced pulmonary fibrosis. Am J Pathol 183:758–773. https://doi.org/10.1016/j.ajpath.2013.06.005
Konaka T, Kawami M, Yamamoto A, Yumoto R, Takano M (2020) miR-484: a possible indicator of drug-induced pulmonary fibrosis. J Pharm Pharm Sci 23:486–495
Kawami M, Takenaka S, Kadekaru Y, Akai M, Konaka T, Yumoto R, Takano M (2021) Evaluation on epithelial-mesenchymal state and microRNAs focusing on isolated alveolar epithelial cells from bleomycin injured rat lung. Toxicology 461:152903. https://doi.org/10.1016/j.tox.2021.152903
Kawami M, Harabayashi R, Harada R, Yamagami Y, Yumoto R, Takano M (2018) Folic acid prevents methotrexate-induced epithelial-mesenchymal transition via suppression of secreted factors from the human alveolar epithelial cell line A549. Biochem Biophys Res Commun 497:457–463. https://doi.org/10.1016/j.bbrc.2018.02.111
Yamagami Y, Kawami M, Ojima T, Futatsugi S, Yumoto R, Takano M (2020) Role of plasminogen activator inhibitor-1 in methotrexate-induced epithelial-mesenchymal transition in alveolar epithelial A549 cells. Biochem Biophys Res Commun 525:543–548. https://doi.org/10.1016/j.bbrc.2020.02.131
Cohen P, Cross D, Jänne PA (2021) Kinase drug discovery 20 years after imatinib: progress and future directions. Nat Rev Drug Discov 20:551–569. https://doi.org/10.1038/s41573-021-00195-4
Kawami M, Harada R, Ojima T, Yamagami Y, Yumoto R, Takano M (2019) Association of cell cycle arrest with anticancer drug-induced epithelial-mesenchymal transition in alveolar epithelial cells. Toxicology 424:152231. https://doi.org/10.1016/j.tox.2019.06.002
Semba T, Funahashi Y, Ono N, Yamamoto Y, Sugi NH, Asada M, Yoshimatsu K, Wakabayashi T (2004) An angiogenesis inhibitor E7820 shows broad-spectrum tumor growth inhibition in a xenograft model: possible value of integrin alpha2 on platelets as a biological marker. Clin Cancer Res 10:1430–1438. https://doi.org/10.1158/1078-0432.ccr-0109-03
Ojima T, Kawami M, Yumoto R, Takano M (2020) Differential mechanisms underlying methotrexate-induced cell death and epithelial-mesenchymal transition in A549 cells. Toxicol Res 37:293–300. https://doi.org/10.1007/s43188-020-00067-w
Kawami M, Honda N, Hara T, Yumoto R, Takano M (2019) Investigation on inhibitory effect of folic acid on methotrexate-induced epithelial-mesenchymal transition focusing on dihydrofolate reductase. Drug Metab Pharmacokinet 34:396–399. https://doi.org/10.1016/j.dmpk.2019.08.003
Hynes RO (2002) Integrins: bidirectional, allosteric signaling machines. Cell 110:673–687. https://doi.org/10.1016/S0092-8674(02)00971-6
Kechagia JZ, Ivaska J, Roca-Cusachs P (2019) Integrins as biomechanical sensors of the microenvironment. Nat Rev Mol Cell Biol 20:457–473. https://doi.org/10.1038/s41580-019-0134-2
Adorno-Cruz V, Liu H (2019) Regulation and functions of integrin α2 in cell adhesion and disease. Genes Dis 6:16–24. https://doi.org/10.1016/j.gendis.2018.12.003
Koenig A, Mueller C, Hasel C, Adler G, Menke A (2006) Collagen type I induces disruption of E-cadherin-mediated cell-cell contacts and promotes proliferation of pancreatic carcinoma cells. Cancer Res 66:4662–4671. https://doi.org/10.1158/0008-5472.can-05-2804
Naci D, Vuori K, Aoudjit F (2015) Alpha2beta1 integrin in cancer development and chemoresistance. Semin Cancer Biol 35:145–153. https://doi.org/10.1016/j.semcancer.2015.08.004
Keizer RJ, Funahashi Y, Semba T, Wanders J, Beijnen JH, Schellens JH, Huitema AD (2011) Evaluation of α2-integrin expression as a biomarker for tumor growth inhibition for the investigational integrin inhibitor E7820 in preclinical and clinical studies. AAPS J 13:230–239. https://doi.org/10.1208/s12248-011-9260-2
Mita M, Kelly KR, Mita A, Ricart AD, Romero O, Tolcher A, Hook L, Okereke C, Krivelevich I, Rossignol DP, Giles FJ, Rowinsky EK, Takimoto C (2011) Phase I study of E7820, an oral inhibitor of integrin alpha-2 expression with antiangiogenic properties, in patients with advanced malignancies. Clin Cancer Res 17:193–200. https://doi.org/10.1158/1078-0432.ccr-10-0010
Uehara T, Minoshima Y, Sagane K, Sugi NH, Mitsuhashi KO, Yamamoto N, Kamiyama H, Takahashi K, Kotake Y, Uesugi M, Yokoi A, Inoue A, Yoshida T, Mabuchi M, Tanaka A, Owa T (2017) Selective degradation of splicing factor CAPERα by anticancer sulfonamides. Nat Chem Biol 13:675–680. https://doi.org/10.1038/nchembio.2363
Cheli Y, Kanaji S, Jacquelin B, Chang M, Nugent DJ, Kunicki TJ (2007) Transcriptional and epigenetic regulation of the integrin collagen receptor locus ITGA1-PELO-ITGA2. Biochim Biophys Acta 1769:546–558. https://doi.org/10.1016/j.bbaexp.2007.06.004
Dong J, Wang R, Ren G, Li X, Wang J, Sun Y, Liang J, Nie Y, Wu K, Feng B, Shang Y, Fan D (2017) HMGA2-FOXL2 Axis regulates metastases and epithelial-to-mesenchymal transition of chemoresistant gastric cancer. Clin Cancer Res 23:3461–3473. https://doi.org/10.1158/1078-0432.ccr-16-2180
Su YJ, Lin WH, Chang YW, Wei KC, Liang CL, Chen SC, Lee JL (2015) Polarized cell migration induces cancer type-specific CD133/integrin/Src/Akt/GSK3β/β-catenin signaling required for maintenance of cancer stem cell properties. Oncotarget 6:38029–38045. https://doi.org/10.18632/oncotarget.5703
Wang Q, Cao T, Guo K, Zhou Y, Liu H, Pan Y, Hou Q, Nie Y, Fan D, Lu Y, Zhao X (2020) Regulation of integrin subunit alpha 2 by miR-135b-5p modulates chemoresistance in gastric cancer. Front Oncol 10:308. https://doi.org/10.3389/fonc.2020.00308
Georgiou KR, Nadhanan RR, Fan CM, Xian CJ (2015) Methotrexate-induced bone marrow adiposity is mitigated by folinic acid supplementation through the regulation of Wnt/β-catenin signalling. J Cell Physiol 230:648–656. https://doi.org/10.1002/jcp.24788
Zaidel-Bar R, Itzkovitz S, Ma’ayan A, Iyengar R, Geiger B (2007) Functional atlas of the integrin adhesome. Nat Cell Biol 9:858–867. https://doi.org/10.1038/ncb0807-858
Aguirre Ghiso JA (2002) Inhibition of FAK signaling activated by urokinase receptor induces dormancy in human carcinoma cells in vivo. Oncogene 21:2513–2524. https://doi.org/10.1038/sj.onc.1205342
Yamamoto A, Kawami M, Konaka T, Takenaka S, Yumoto R, Takano M (2019) Anticancer drug-induced epithelial-mesenchymal transition via p53/miR-34a axis in A549/ABCA3 cells. J Pharm Pharm Sci 22:516–524. https://doi.org/10.18433/jpps30660
Funding
This work was supported by the Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (JP18H02586, JP18K06749, and JP19K16447).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Kawami, M., Ojima, T., Yumoto, R. et al. Role of integrin α2 in methotrexate-induced epithelial-mesenchymal transition in alveolar epithelial A549 cells. Toxicol Res. 38, 449–458 (2022). https://doi.org/10.1007/s43188-022-00127-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43188-022-00127-3