Abstract
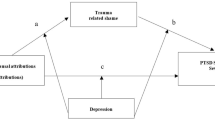
Shame has been identified as a key emotional response to trauma exposure and is implicated in the development and maintenance of PTSD. Despite this, there is a lack of empirical research explaining how and why shame emerges following trauma exposure. Current theoretical models of shame converge on the idea that shame is elicited through internal, stable, and global attributions about the precipitating event. A systematic review was conducted to assess the relationship between causal attributions, shame, and PTSD symptomology. A database search of PsycINFO, PubMED, Medline, EMBASE and PTSDPubs identified articles published between 1980 to 2022 that enabled examination of the relationship between attributions, shame, and PTSD. A total of eight articles met inclusion criteria for this review. There were cross-sectional relationships between internal attributions, shame, and PTSD symptoms, with shame demonstrating the strongest relationship with PTSD symptoms. Significant indirect effects were found between internal attributions, shame, and PTSD. Concerns surrounding reliability of measurements and sampling bias made it difficult to draw definitive conclusions. The current evidence is too preliminary to offer strong support for the mediation hypothesis. However, it does offer important avenues for future research that will have important clinical applications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Was it me? The role of attributions and shame in posttraumatic stress disorder (PTSD): A systematic review
Posttraumatic Stress Disorder (PTSD) is one of the most common psychological sequelae following the direct witnessing or experiencing of a traumatic event (American Psychiatric Association [APA], 2013). It consists of a set of cognitive, emotional, and physiological symptoms including recurring, intrusive re-experiencing traumatic memories that are involuntary triggered by trauma related cues.
Historically, PTSD has been conceptualised primarily as an anxiety, fear-based disorder (see North et al., 2016 for a discussion on the evolution of PTSD diagnostic criterion) that has been thought to arise from a failure to emotionally process the traumatic event due to maladaptive and excessive fear associations with the traumatic memory (Foa & Kozak, 1986). Over time, these symptoms lead to an increased hypersensitivity to threat (Ehlers et al., 2002, 2004), and physiological hyperarousal that promotes cognitive and behavioural avoidance.
More recently, there have been suggestions that addressing fear alone using exposure based therapies may not be sufficient in resolving PTSD symptoms altogether, with up to 50% of patients with PTSD remaining symptomatic post treatment (Bradley et al., 2005). Left untreated, PTSD runs a chronic course, with significant psychiatric comorbidity and increased suicide risk (Kessler, 2000), underscoring the need to improve existing treatment models. In response, researchers have begun implicating other potentially dysregulated emotions, such as shame as a possible contributor to PTSD (Lee et al., 2001; Lopez-Castro et al., 2019; Taylor, 2015; Wilson et al., 2006). Beyond exposure-based therapies, other evidenced approaches have emerged to address additional diagnostic features of PTSD. For example, Cognitive Processing Therapy (CPT) (Resick & Schnicke, 1992; Resick et al., 2016) focuses on cognitive behavioural principles, and includes a greater focus on processing and challenging appraisals related to shame. Although promising, outcome studies examining shame’s response to treatment are only just emerging (e.g., Resick et al., 2008).
Trauma related shame has been associated with intrusive recollections, hyperarousal, and avoidance (Dewey et al., 2014; Dorahy et al., 2013; Sippel & Marshall, 2011). Immediate reactions of shame following a traumatic event have also been found to mediate the relationship between trauma exposure, and posttraumatic stress symptoms (PTSS) up to six months post trauma (Andrews et al., 2000; Beck et al., 2011). Despite converging evidence demonstrating significant associations between shame and PTSD (Lopez-Castro et al., 2019), the mechanisms that could account for therapeutic change are still unclear. Thus, future research explicating how and why shame is elicited following a trauma, is still needed.
Shame is conceptualised as a self-conscious emotion as it relates to our perceptions of ourselves; a painful, negative self-evaluative emotion that prompts negative self-judgement (Tracy et al., 2007). It is considered a cognitively complex emotion as it arises through a series of cognitive appraisals. In particular, for shame to arise, an individual first has to make an individual makes an internal attribution pertaining to the cause of the eliciting event (Tangney & Dearing, 2002; Tracy et al., 2007). Although it is often used synonymously with guilt, both have distinct phenomenological experiences. Shame is thought to arise through a global negative evaluation of the self, where the individual fails to meet a perceived internal or external standard. Subsequently, the self is viewed as flawed, inadequate, or even worthless (e.g., “I am bad”). (Lewis, 1971, 2003; Tangney & Dearing, 2002). Sources of shame might originate through negative schematic representations of the self (Lee et al., 2001), or externally through stigmatisation and/or public condemnation (Gilbert, 1997). Guilt relates to a specific focus pertaining to one’s behaviour (e.g., “I did a bad thing”). This distinction is important as both affective experiences prompt divergent responses. Guilt tends to elicit prosocial behaviour, whilst the experience of shame, tends to motivate withdrawal due to the desire to hide oneself.
Current theoretical models of shame (Lazarus, 1991; Lewis, 1971; Tangney & Dearing, 2002; Tangney et al., 2007; Tracy et al., 2007) converge on the idea that beyond the causal locus, two additional attribution dimensions are critical to the elicitation of self-conscious emotions. Specifically, causal dimensions regarding the globality, or generality and the stability or permanence. The model holds that after an internal attribution is made, the individual evaluates whether the cause pertains to them, and whether this is likely to change. Shame is said to arise through internal, stable, and global attributions, such as one’s personality or character. In contrast, guilt, is purported to arise through internal, unstable, and specific attributions, such as one’s behaviour.
It stands to reason that following a potentially traumatic event, individuals may be inclined to attribute blame to themselves or others. This assumption is consistent with the cognitive model of PTSD (Ehlers & Clark, 2000), which holds that negative appraisals of the trauma and its sequalae is a key maintaining factor that leads to a sense of serious, and current threat. In particular, it implicates erroneous causal attributions of one’s trauma to the self; self-blame, as one of the key cognitions predictive of PTSD symptoms (Foa et al., 1999). However, findings demonstrating the link between self-blame and PTSD are mixed (Gómez de La Cuesta et al., 2019), with suggestions that self-blame may be a self-protective cognition against PTSD (Nickerson et al., 2013). Possible explanations for this discrepancy include the methodological limitations associated with current measures of trauma- attributions in the context of PTSD.
The examination of the cognitive antecedents of shame provides an opportunity for future research to inform current or new treatments for shame. To do so, an important first step is to better understand the current research linking attributions, shame, and PTSD and to establish an empirical foundation.
The current paper aims to provide a comprehensive review of the literature regarding the relationship between attributions, shame, and PTSD. As shame and attributions can be considered both states and/or traits, the review will refer to these constructs interchangeably. Specifically, it aims to synthesise and evaluate the research evidence pertaining to this association. Due to the specificity of the research question, and the possibility that few studies will be included, studies that reported on both children and adults will be included. Both child, adolescent and adult studies will be examined separately to identify potentially distinct or similar associations between target variables within these populations. A discussion of the key findings from each study will also be included along with recommendations for future research and the implications for clinical practice.
Method
Search Strategy and Selection Review
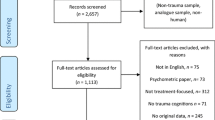
This review protocol was registered with PROSPERO, the internal prospective register of systematic reviews (Registration number: CRD42020148804). The review process was followed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., 2021).
Electronic searches were conducted of the following databases: PsycINFO, PubMed, Medline, EMBASE, and PTSDPubs (formally known as PILOTS). The search was carried out between 26 August 2019 and 3 October 2019, updated on 25 November 2022. The following search terms were identified in the title, abstract, keywords and MeSH terms for shame: (shame*) in combination with PTSD, PTSS (Posttraumatic stress symptoms) and related terms (post traumatic stress disorder OR post traumatic stress symptoms OR post traumatic stress reactions OR trauma* OR Psychotrauma OR psychol* trauma*) and trauma related attributions (causal attribution* OR trauma attribution* OR self blame OR attribution* OR cognitive appraisal* OR appraisal*). All databases were searched from 1980 (when PTSD was formally introduced into the Diagnostic and Statistical Manual of Mental Disorders (DSM)) to 2022. Reference lists of included studies were manually screened for additional relevant papers. All references were managed using Endnote. Duplicates were removed iteratively using Endnote's duplication identification tool, then manually.
Inclusion and Exclusion Criteria
Articles were identified using the following inclusion criteria: empirical peer reviewed journal articles, written in English, which included:
-
1.
Child, adolescent, and adult samples.
-
2.
A quantitative measure of PTSD symptoms, either through a semi structured interview or self-report questionnaire.
-
3.
A quantitative measure of shame, attribution style and/or trauma-related causal attributions.
Articles were excluded from the review based on the following criteria:
-
1.
Studies not published in English and without English translation.
-
2.
Articles without empirical data such as qualitative studies and/or review papers.
-
3.
Categorical, single-item measures of any of the target variables, as they have indeterminant reliability (Wanous & Reichers, 1996). Further, single item measures are not appropriate to assess PTSD symptom severity.
-
4.
Studies that do not contain all target variables (attributions, shame, and PTSD).
-
5.
Studies that involved treatments either through routine clinical interventions and/or Randomised Controlled Trials (RCTs) that could influence participants’ attributions, shame and/or PTSD symptoms.
Study Selection and Quality Assessment
The first and second author independently screened both abstracts and full texts according to the inclusion and exclusion criteria. There was almost perfect agreement between the two reviewers, κ = .928 (95% CI, .879 to .977), p < .05. A total of 734 records (excluding duplicates) were identified. After screening of abstracts and titles, 77 articles were identified for full text review. More than half (N = 46) were excluded on the basis that they did contain measures of all the target variables. Twelve papers were identified as meeting the inclusion criteria. However, four studies (Feiring et al., 2001, 2002a, 1998; Feiring & Taska, 2005) were excluded on the basis that they consisted of participants from the same recruitment sample (Feiring et al., 1998). To preserve the integrity of the current review, only Feiring et al. (2002b) was included as it explicitly investigated the relationship between the target variables. Eight studies (three child/adolescent, five adult) were included that met full eligibility criteria (Alix et al., 2020, 2017; Bhuptani & Messman, 2021; Carretta & Szymanski, 2020; Feiring et al. (2002b); Uji et al., 2007; Wojcik et al., 2022; Zerach & Levi-Belz, 2018).
Methodological Quality
The papers were evaluated for methodological quality using The Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Analytical Cross Sectional Studies and Cohort Studies (Joanna Briggs Institute, 2020; Porritt et al., 2014). Both checklists consist of eight and eleven questions, respectively. Each question is answered through four options Yes (Y), No (N), Unclear (U) and Not Applicable (NA). The risk of bias percentage is calculated based on the number of “Y” selected. Items where “N/A” was selection are not considered in the calculation. Studies with between 0–49% of “yes” responses are considered as being low quality, between 50–69% as moderate quality, 70–100% (Buckingham et al., 2021; Goplen et al., 2019).
Results
Overview of Studies
Figure 1 depicts a summary of the search and screening process, reasons for exclusion. Eight papers in the review originated from the United States, Japan, Israel, and Canada. Sample sizes across participants ranged from 98 to 367. Half of the studies recruited treatment seeking samples from specialist clinics for sexual assault (Alix et al., 2020, 2017; Feiring et al. 2002b; Wojcik et al., 2022). Two were from outpatient community samples from universities (Bhuptani & Messman, 2021; Uji et al., 2007), one from an online convenience sample of women (Carretta & Szymanski, 2020), and another from a sample of Israeli veterans (Zerach & Levi-Belz, 2018). Table 1 presents a summary of studies included in the review.
Quality Appraisal
Included articles were assessed for methodological quality. Cross-sectional and prospective studies were appraised separately. See Supplementary Material Table 1 and 2 for more information. Out of the six cross-sectional studies, four were determined to be high quality, and one of moderate quality as they lacked appropriate statistical methods or design to identify or control for confounding factors. The study that was rated low quality lacked the same and did not adequately describe the inclusion and exclusion criteria for their sample. Results were inconsistently reported, which included non-reporting of confidence intervals (du Prel et al., 2009), and inconsistent use of standardised and non-standardised regression coefficients. Further, it was unclear how confounds were addressed statistically. Among the two prospective studies, similar issues were noted, with one study rated as high and another as moderate quality. It is worth noting that both prospective studies (Alix et al., 2020; Feiring et al., 2002b) recruited participants from specialist services, and it was unclear whether participants were receiving any form of intervention or treatment between baseline assessment and follow-up.
Measurement of Trauma and PTSD
Almost all of the studies in the review utilised clinical analogues, as they did not utilise a gold standard assessment of PTSD (e.g., Clinician-Administered PTSD Scale for DSM-5; CAPS-5) (Weathers et al., 2013a) to establish a DSM-5 PTSD diagnosis. All studies used developmentally appropriate, self-report measures of PTSD symptoms according to either the DSM-4-TR (Association Psychiatric Association [APA], 2000) and/or DSM-5 (American Psychiatric Association [APA], 2013) criteria for PTSD. This included the Child Impact of Traumatic Events Scale (CITES) (Wolfe, 2002) and the Impact of Events Scale Revised (IES-R) (Weiss & Marmar, 1997) for children and adolescents, and the PTSD Checklist-5 (PCL-5) (Weathers et al., 2013b) for adults. All of these are validated measures with good reliability/consistency.
In terms of trauma exposure, almost all studies (n = 7) used some form of validated or study specific checklist (e.g., Feiring et al., 2002b; Uji et al., 2007) assess for the trauma exposure of interest. None of the studies assessed for broad trauma history.
Measurement of Attributions
For trauma related attributions, the use of abuse specific attribution measures along with individual attributional styles, that is the tendency to attribute negative events to oneself, were used. The Abuse-specific internal attributional style was developed by Feiring et al. (2002b) which includes items that describe internal and external attributions for abuse. It was subsequently utilised in the other three studies (Alix et al., 2020, 2017; Uji et al., 2007) as a proxy for abuse specific attributions.
Feiring et al. (2002b) also assessed for general attributional style using the Children’s Attributional Style Questionnaire – Revised (CASQ-R) (Thompson et al., 1998). This measure consists of 24 hypothetical events with half describing a positive outcome and the other, a negative outcome. Each event has two possible attributions and respondents are asked to pick why each event occurred. Each description relates to one of the three attributional dimensions (internal, stable, and global). A pessimistic attribution style was calculated as the difference between attributions for negative events and positive events; a lower score indicated a tendency to attribute events to internal, stable, and global causes for both positive and negative events. Coversely, Zerach and Levi-Belz (2018) utilised the Depressive Attributions Questionnaire (DAQ) (Kleim et al., 2011) to examine internal attributional styles based on the Hopelessness and Learned Helplessness model of depression (Abramson et al., 1978; Seligman et al., 1979), and the Cognitive Model of depression (Beck et al., 1979). In their study, they refer to this as Depressive Attributions.
Measurement of Shame
Five studies utilised an abuse specific shame measure that was originally designed by Feiring and colleagues (Feiring et al., 2002a, b; Feiring & Taska, 2005). All other adult studies utilised a broad trauma specific measure, The Trauma-Related Shame Inventory (TRSI) (Øktedalen et al., 2014) which assesses shame tethered to the trauma of interest. It also distinguishes internal and external sources of trauma-related shame (Gilbert, 1997).
Bhuptani and Messman (2021) assessed different types of shame; trait and general shame along with trauma-specific shame, or rape related shame. State shame (general shame) referred to the general feelings of shame, whilst trait shame (shame proneness) was assessed as the propensity for one to experience shame across a range of scenarios that typically evoke personal transgressions. General shame was assessed as experiences of experiential, cognitive and behavioural components of shame in the past year. Shame proneness was evaluated as the propensity to examine guilt and shame across a range of hypothetical personal transgressions. The study utilised the shame negative evaluations scale which focuses on evaluations characteristic of shame (e.g., “I am a bad person”, “I am incompetent”; Tangney & Dearing, 2002).
Aim 1: The Relationship Between Attributions, Shame, and PTSD
Table 2 presents a summary of bivariate correlations between key variables and key findings from each paper.
Child and Adolescent Studies
Cross sectionally, all studies reported weak-moderate, albeit significant relationships between abuse specific attributions and PTSD symptoms. Consistently, abuse specific shame exhibited moderately strong relationships with PTSD symptoms.
Three studies examined relationships between key variables prospectively. Both Alix et al. (2020) and Feiring et al. (2002b) found significant relationships between shame at baseline and PTSD symptoms at 6 months (r = .44, p < .001) and 12 months (r = 0.67, p ≤ .0001). In contrast, Alix et al. (2020) found a significant relationship between abuse attributions as baseline and PTSD symptoms 6 months later (r = .33, p < .001). In terms of general attribution risk, Feiring et al., (2002b) found weak significant relationship cross-sectionally for shame (r = -.20, p ≤ .01), but not at follow-up. General attribution risk exhibited weak, non-significant relationships with PTSD at both baseline and follow-up.
Adult Studies
Across all adult studies, shame consistently exhibited a moderately significant relationship with PTSD symptoms. Similarly, attributions, measured either through attributional style of trauma-specific attributions exhibited a slightly weaker, albeit still significant relationship with shame and PTSD. Bhuptani and Messman (2021) was the only study that assessed trauma specific shame, shame-proneness, and state shame. Their study found that trauma-specific shame had the strongest relationship with both attributions and PTSD. Shame proneness was not significantly related to both attributions and PTSD symptoms.
Aim 2: Does Shame Mediate the Relationship Between Attributions and PTSD?
Half of the studies (n = 4) in the review examined the possibility that shame might explain the relationship between attributions and PTSD symptoms. As not all coefficients were standardised, key findings are reported separately.
Child and Adolescent Studies
In Feiring et al. (2002b) the authors examined whether shame mediated the relationship between general attribution risk and subsequent PTSD symptoms one year after discovery of sexual abuse. The authors did not find a mediation effect. However, further regression analyses indicated that, a reduction in shame (β = -.20, p ≤ .01), and abuse related attribution (β = -.31, p ≤ .0001), was associated with improvements in PTSD symptoms. Changes in both variables accounted for 19% of the variance in PTSD symptoms.
Alix et al. (2017) also found that shame also indirectly mediated the relationship between abuse specific attributions and PTSD symptoms (β = .24, p < .05), [95%CI = .14 to .35] and PTSD, with the indirect effect explaining 45% of variance in PTSD symptoms.
Adult Studies
Both Uji et al. (2007) and Bhuptani and Messman (2021) examined both direct and indirect effects of self-blame (internal attributions) and PTSD via shame in adult women who experienced some form of sexual assault. Both studies found significant indirect effects between internal attributions (self-blame) and PTSD via trauma-related shame. In Uji et al. (2007), there was a significant direct effect between shame and PTSD (β = .40, p < .000) and self-blame and shame (β = .43, p < .000). However, the indirect effect was not reported. Bhuptani and Messman (2021) found a larger direct effects for shame and PTSD symptoms (b = .58, p < .001) and for self-blame and rape-related shame (b = .94, p < .001). There was an indirect effect for self-blame and PTSD (b = .54, 95% CI [.32 to .82] via rape related shame, but not for general shame (b = .06, 95% CI [-.00 to .17].
In contrast, Zerach and Levi-Belz (2018) examined whether the relationship between veterans who had experienced a potentially morally injurious event that involved betrayal (MIES-Betrayal) and their respective PTSD symptoms would be mediated by several psychological factors. In a serial integrated model, MIES-Betrayal was significantly associated with depressive attributions, and subsequently trauma related intrinsic shame and higher levels of PTSS. They found that two-step indirect effects to PTSD were significant (b = .20, p < .01; 95% CI [.05 to .51]). Specifically, MIES-Betrayal was significantly associated with depressive attributions (β = .22, p < .01), that associated with intrinsic trauma-related shame (.45, p < .001), which in turn was associated with more severe PTSD symptoms (β = .29, p < . 001).
Discussion
The aim of this systematic review was to summarise the available evidence on the relationship between attributions, shame and PTSD, and the possibility that shame would explain the relationship between attributions and PTSD. The review was sparse, yielding only eight studies that met inclusion criteria. Majority of studies obtained from the search were excluded on the basis that they did not contain measurements of all key variables.
Studies with adult samples used a mix of convenient sampling across university and/or online or specifically from intervention centres. In contrast, all child and adolescent studies (Alix et al., 2020, 2017; Feiring et al., 2002b) focused on CSA survivors and recruited participants from various child sexual abuse (CSA) treatment centres.
In terms of measures, child and adolescent studies utilised sexual abuse specific measures to assess for attributions and shame. Across adult studies, these measures varied, ranging from state and trait measures of shame to abuse specific measures and broad trauma-related shame. Regardless of the trauma of interest, none of the studies assessed did not seek to obtain broader trauma history, and control for exposure as a potential confound. This is important as multiple trauma exposures is expected to be the rule, not the exception (Kessler et al., 2017) with increased trauma exposure related to more severe PTSD symptoms (Benjet et al., 2016; Karam et al., 2014). Regardless of what shame measure was used, across both child and adult studies, the most consistent finding was that shame was most strongly associated with PTSD symptoms. The relationship between attributions, trauma-specific or attributional style were also significantly associated with both shame and PTSD symptoms. These relationships were similar in magnitude. These findings were consistent with theoretical and empirical discussions indicating that self-blame is a key feature of PTSD, and associated with both shame and PTSD symptoms (Ehlers & Clark, 2000; Gómez de La Cuesta et al., 2019; Saraiya & Lopez-Castro, 2016).
The second aim of the review was to assess whether shame would mediate the relationship between attributions and PTSD. Although only half of studies included in the review reported on the mediation effect, indicating that shame mediates the relationship between attributions and PTSD. Nevertheless, further studies that utilise other trauma exposed samples and broad trauma attributions and shame measures will still be needed to generalise current findings. For example, majority of studies in this review were primarily focused on CSA or survivors of sexual assault. Except for Bhuptani and Messman, (2021) and Wojcik et al. (2022), the remaining studies utilised abuse specific trauma and attribution measures that were designed for the body of research conducted by Feiring and colleagues (Feiring et al., 2001; Feiring et al., 2002a; Feiring et al., 1998; Feiring et al., 2002b; Feiring & Taska, 2005).
Similarly, although Zerach and Levi-Belz (2018) focused on veterans exposed to morally injurious events, the study utilised a depressive attributional style measure which refers to the tendency to make depressogenic (internal, stable, and global) attributions across a range of negative events. Without prospective data, it is unclear to what extent attributional style functions as a predisposing factor toward shame independently of trauma exposure. It is likely that there is also a bidirectional effect between one’s attributional style and trauma exposure. Further, although specific types of trauma exposure may increase the propensity for one to make internal attributions and experience shame, future empirical work assessing these constructs across different trauma types is still needed.
As majority of studies were cross-sectional, it is not possible to draw conclusions about causality. Optimistically, Alix et al. (2020) and Feiring et al. (2002b) attempted to report longitudinal associations at baseline and follow-up, indicating that shame may be predictive of PTSD.
As both studies recruited participants from various CSA treatment centres, it was unclear whether participants had or were receiving any subsequent interventions between baseline and follow-up. Further, both studies only assessed change over two timepoints, which limits the characterisation of how strong this relationship holds over time. Future studies utilising multiple follow-up points could help clarify the prospective relationship between shame, PTSD, and maladjustment.
It is worth considering that studies included in the review used both DSM-4 (Association Psychiatric Association [APA], 2000) and DSM-5 (American Psychiatric Association [APA], 2013) criteria for PTSD. As previously asserted, changes to the DSM-5 diagnostic criteria included an additional category that includes alterations in cognition and mood as a core symptom cluster. Within this, shame and self-blame are both potential diagnostic features. Despite this, none of the studies that utilised the DSM-5 criteria conducted sensitivity analyses to exclude this symptom cluster.
Limitations and Directions for Future Research
As far as the authors are aware, this is the first systematic review to investigate the relationships between attributions, shame, and PTSD across the lifespan. The current review included a rigorous method of searching and evaluating the relevant literature. A large number of databases were used, and a broad search strategy was employed to include all types of attributions and shame measures. PRISMA guidelines were followed, and there was strong inter-rater agreement for inclusion of studies between both reviewers. All included studies were peer-reviewed. However, there is still a risk of publication bias, as published articles tend to report positive findings.
The review examined the influence of attributions and shame on overall PTSD symptom severity. Accordingly, we included studies that reported on PTSD symptoms according to both the DSM-4 (APA, 2000) and DSM-5 (APA, 2013) criteria. The DSM-5 (APA, 2013) subsumes a broad range of emotional responses to trauma – including shame – within the negative alterations in cognitions and mood symptom cluster. Accordingly, there is a potential for further research to understand how attributions relate to shame when shame is considered part of PTSD itself.
The review also revealed some important methodological limitations within the literature. Included studies predominately consisted of female sexual assault survivors from childhood or adulthood. Thus, additional research is still needed in other population groups to generalise findings. Prospective studies using multivariate statistics that consider and/or control for the effects of potential risk factors, such as type of trauma history, time since trauma exposure and cumulative exposure, is encouraged (Brewin et al., 2000; Conrad et al., 2017; Tran et al., 2019).
The use of prospective, population-based studies could potentially inform the literature regarding possible fluctuations of shame over time and the relative stability and relationships, if any of key variables over time. This would be useful in identifying whether targeting attributions will contribute to changes in shame and PTSD or vice versa.
Conclusions
Research has acknowledged shame as a key posttraumatic response, responsible for the maintenance and development of PTSD (Lopez-Castro et al., 2019). Theoretical models of hsame indicate that causal attributions are key cognitive antecedent to shame (Tangney & Dearing, 2002; Tracy et al., 2007), which is theoretically consistent with current cognitive theories of PTSD (Ehlers & Clark, 2000). This review highlights some of the key findings that have examined attributions, shame, and PTSD. Unfortunately, methodological limitations of included studies limit the extent to which findings can be interpreted and generalised. Additional research is necessary to design appropriate measures relevant to broader trauma populations and to consider the impact of trauma history and type. The limited number of studies eligible for inclusion in our systematic review precludes definitive conclusions from being drawn. Nevertheless, the findings presented in this review indicate that appraisals such as internal causal attributions contribute to the development of shame and subsequently PTSD. As the experience of shame is not always volunteered or recognised, identifying, and taking into consider attributions as a potential pathway toward shame, clinicians can become more aware of the potential presence of shame and address it accordingly.
Data Availability
The data came from the analysis of eight previously published papers included in this review, indexed in the PsycINFO, PubMED, Medline, EMBASE and PTSDPubs.
Code Availability
Not applicable.
References
Abramson, L. Y., Seligman, M. E., & Teasdale, J. D. (1978). Learned helplessness in humans: Critique and reformulation. Journal of Abnormal Psychology, 87(1), 49. https://doi.org/10.1037/0021-843X.87.1.49
Alix, S., Cossette, L., Hébert, M., Cyr, M., & Frappier, J.-Y. (2017). Posttraumatic Stress Disorder and Suicidal Ideation Among Sexually Abused Adolescent Girls: The Mediating Role of Shame. Journal of Child Sexual Abuse, 26(2), 158–174. https://doi.org/10.1080/10538712.2017.1280577
Alix, S., Cossette, L., Cyr, M., Frappier, J.-Y., Caron, P.-O., & Hébert, M. (2020). Self-blame, shame, avoidance, and suicidal ideation in sexually abused adolescent girls: A longitudinal study. Journal of Child Sexual Abuse, 29(4), 432–447. https://doi.org/10.1080/10538712.2019.1678543
Andrews, B., Brewin, C. R., Rose, S., & Kirk, M. (2000). Predicting PTSD symptoms in victims of violent crime: The role of shame, anger, and childhood abuse. Journal of Abnormal Psychology, 109(1), 69–73. https://doi.org/10.1037//0021-843x.109.1.69
Andrews, B., Qian, M., & Valentine, J. D. (2002). Predicting depressive symptoms with a new measure of shame: The Experience of Shame Scale. British Journal of Clinical Psychology, 41(1), 29–42. https://doi.org/10.1348/014466502163778
Association, American Psychiatric, & [APA]. (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Text Revision, DSM-IV-TR): American Psychiatric Association.
Association, American Psychiatric, & [APA]. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). DSM-V): American Psychiatric Association.
Beck, A., Rush, A., Shaw, B., & Emery, G. (1979). Cognitive therapy of depression. Guilford Press.
Beck, J., McNiff, J., Clapp, J., Olsen, S., Avery, M., & Hagewood, J. (2011). Exploring Negative Emotion in Women Experiencing Intimate Partner Violence: Shame, Guilt, and PTSD. Behavior Therapy, 42(4), 740–750. https://doi.org/10.1016/j.beth.2011.04.001
Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., Shahly, V., Stein, D. J., Petukhova, M., Hill, E., Alonso, J., Atwoli, L., Bunting, B., Bruffaerts, R., Caldas-de-Almeida, J. M., de Girolamo, G., Florescu, S., Gureje, O., Huang, Y., . . . Koenen, K. C. (2016). The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327–343. https://doi.org/10.1017/S0033291715001981
Bhuptani, P., & Messman, T. (2021). Role of blame and rape-related shame in distress among rape victims. Psychological Trauma: Theory, Research, Practice, and Policy. https://doi.org/10.1037/tra0001132
Bradley, R., Greene, J., Russ, E., Dutra, L., & Westen, D. (2005). A multidimensional meta-analysis of psychotherapy for PTSD. The American Journal of Psychiatry, 162(2), 214–227. https://doi.org/10.1176/appi.ajp.162.2.214
Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. https://doi.org/10.1037//0022-006x.68.5.748
Buckingham, P., Moulton, J. E., Subasinghe, A. K., Amos, N., & Mazza, D. (2021). Acceptability of immediate postpartum and post-abortion long-acting reversible contraception provision to adolescents: A systematic review. Acta Obstetricia et Gynecologica Scandinavica, 100(4), 629–640. https://doi.org/10.1111/aogs.14129
Carretta, R. F., & Szymanski, D. M. (2020). Stranger Harassment and PTSD Symptoms: Roles of Self-Blame, Shame, Fear, Feminine Norms, and Feminism. Sex Roles, 82(9), 525–540. https://doi.org/10.1007/s11199-019-01073-5
Cohen, T. R., Wolf, S. T., Panter, A. T., & Insko, C. A. (2011). Introducing the GASP scale: A new measure of guilt and shame proneness. Journal of Personality and Social Psychology, 100(5), 947–966. https://doi.org/10.1037/a0022641
Conrad, D., Wilker, S., Pfeiffer, A., Lingenfelder, B., Ebalu, T., Lanzinger, H., Elbert, T., Kolassa, I.-T., & Kolassa, S. (2017). Does trauma event type matter in the assessment of traumatic load? European Journal of Psychotraumatology, 8(1), 1344079–1344079. https://doi.org/10.1080/20008198.2017.1344079
Dewey, D., Schuldberg, D., & Madathil, R. (2014). Do Peritraumatic Emotions Differentially Predict PTSD Symptom Clusters? Initial Evidence for Emotion Specificity. Psychological Reports, 115(1), 1–12. https://doi.org/10.2466/16.02.PR0.115c11z7
Dorahy, M. J., Corry, M., Shannon, M., Webb, K., McDermott, B., Ryan, M., & Dyer, K. F. (2013). Complex trauma and intimate relationships: The impact of shame, guilt and dissociation. Journal of Affective Disorders, 147(1–3), 72–79. https://doi.org/10.1016/j.jad.2012.10.010
du Prel, J.-B., Hommel, G., Röhrig, B., & Blettner, M. (2009). Confidence interval or p-value?: Part 4 of a series on evaluation of scientific publications. Deutsches Arzteblatt International, 106(19), 335–339. https://doi.org/10.3238/arztebl.2009.0335
Ehlers, A., & Clark, D. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. https://doi.org/10.1016/s0005-7967(99)00123-0
Ehlers, A., Hackmann, A., Steil, R., Clohessy, S., Wenninger, K., & Winter, H. (2002). The nature of intrusive memories after trauma: The warning signal hypothesis. Behaviour Research and Therapy, 40(9), 995–1002. https://doi.org/10.1016/S0005-7967(01)00077-8
Ehlers, A., Hackmann, A., & Michael, T. (2004). Intrusive re-experiencing in post-traumatic stress disorder: Phenomenology, theory, and therapy. Memory, 12(4), 403–415. https://doi.org/10.1080/09658210444000025
Fairchild, K., & Rudman, L. A. (2008). Everyday Stranger Harassment and Women’s Objectification. Social Justice Research, 21(3), 338–357. https://doi.org/10.1007/s11211-008-0073-0
Feiring, C., & Taska, L. S. (2005). The persistence of shame following sexual abuse: A longitudinal look at risk and recovery. Child Maltreatment, 10(4), 337–349. https://doi.org/10.1177/1077559505276686
Feiring, C., Taska, L., & Lewis, M. (1998). The Role of Shame and Attributional Style in Children’s and Adolescents’ Adaptation to Sexual Abuse. Child Maltreatment, 3(2), 129–142. https://doi.org/10.1177/1077559598003002007
Feiring, C., Coates, D. L., & Taska, L. S. (2001). Ethnic Status, Stigmatization, Support, and Symptom Development Following Sexual Abuse. Journal of Interpersonal Violence, 16(12), 1307–1329. https://doi.org/10.1177/088626001016012005
Feiring, C., Taska, L., & Chen, K. (2002a). Trying to understand why horrible things happen: Attribution, shame, and symptom development following sexual abuse. Child Maltreatment, 7(1), 26–41. https://doi.org/10.1177/1077559502007001003
Feiring, C., Taska, L., & Lewis, M. (2002b). Adjustment following sexual abuse discovery: The role of shame and attributional style. Developmental Psychology, 38(1), 79. https://doi.org/10.1037//0012-1649.38.1.79
Feiring, C., Simon, V. A., & Cleland, C. M. (2009). Childhood sexual abuse, stigmatization, internalizing symptoms, and the development of sexual difficulties and dating aggression. Journal of Consulting and Clinical Psychology, 77(1), 127–137. https://doi.org/10.1037/a0013475
Foa, E., & Kozak, M. (1986). Emotional Processing of Fear: Exposure to Corrective Information. Psychological Bulletin, 99(1), 20–35. https://doi.org/10.1037/0033-2909.99.1.20
Foa, E. B., Ehlers, A., Clark, D. M., Tolin, D. F., & Orsillo, S. M. (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11(3), 303–314. https://doi.org/10.1037/1040-3590.11.3.303
Frazier, P. A. (2003). Perceived control and distress following sexual assault: A longitudinal test of a new model. Journal of Personality and Social Psychology, 84, 1257–1269. https://doi.org/10.1037/0022-3514.84.6.1257
Gilbert, P. (1997). The evolution of social attractiveness and its role in shame, humiliation, guilt and therapy. British Journal of Medical Psychology, 70(2), 113–147. https://doi.org/10.1111/j.2044-8341.1997.tb01893.x
Gómez de La Cuesta, G., Schweizer, S., Diehle, J., Young, J., & Meiser-Stedman, R. (2019). The relationship between maladaptive appraisals and posttraumatic stress disorder: A meta-analysis. European Journal of Psychotraumatology, 10(1), 1620084. https://doi.org/10.1080/20008198.2019.1620084
Goplen, C. M., Verbeek, W., Kang, S. H., Jones, C. A., Voaklander, D. C., Churchill, T. A., & Beaupre, L. A. (2019). Preoperative opioid use is associated with worse patient outcomes after Total joint arthroplasty: A systematic review and meta-analysis. BMC Musculoskeletal Disorders, 20(1), 234. https://doi.org/10.1186/s12891-019-2619-8
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat Duty in Iraq and Afghanistan, Mental Health Problems, and Barriers to Care. New England Journal of Medicine, 351(1), 13–22. https://doi.org/10.1056/NEJMoa040603
Joanna Briggs Institute. (2020). JBI Critical Appraisal Tools. https://jbi.global/critical-appraisal-tools
Karam, E. G., Friedman, M. J., Hill, E. D., Kessler, R. C., McLaughlin, K. A., Petukhova, M., Sampson, L., Shahly, V., Angermeyer, M. C., Bromet, E. J., de Girolamo, G., de Graaf, R., Demyttenaere, K., Ferry, F., Florescu, S. E., Haro, J. M., He, Y., Karam, A. N., Kawakami, N., . . . Koenen, K. C. (2014). Cumulative traumas and risk thresholds: 12-month PTSD in the World Mental Health (WMH) surveys. Depression and Anxiety, 31(2), 130–142. https://doi.org/10.1002/da.22169
Kessler, R. (2000). Posttraumatic stress disorder: The burden to the individual and to society. The Journal of Clinical Psychiatry, 61(Suppl 5), 4–12. discussion 13-14.
Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., Degenhardt, L., de Girolamo, G., Dinolova, R. V., Ferry, F., Florescu, S., Gureje, O., Haro, J. M., Huang, Y., Karam, E. G., Kawakami, N., Lee, S., Lepine, J.-P., Levinson, D., . . . Koenen, K. C. (2017). Trauma and PTSD in the WHO World Mental Health Surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. https://doi.org/10.1080/20008198.2017.1353383
Kleim, B., Gonzalo, D., & Ehlers, A. (2011). The Depressive Attributions Questionnaire (DAQ): Development of a short self-report measure of depressogenic attributions. Journal of Psychopathology and Behavioral Assessment, 33(3), 375–385. https://doi.org/10.1007/s10862-011-9234-9
Lazarus, R. S. (1991). Progress on a cognitive-motivational-relational theory of emotion. American Psychologist, 46(8), 819–834. https://doi.org/10.1037/0003-066X.46.8.819
Lee, D. A., Scragg, P., & Turner, S. (2001). The role of shame and guilt in traumatic events: A clinical model of shame-based and guilt-based PTSD. British Journal of Medical Psychology, 74(Pt 4), 451–466. https://doi.org/10.1348/000711201161109
Lewis, H. (1971). Shame and guilt in neurosis. International University Press.
Lewis, M. (2003). The role of the self in shame. Social Research, 70(40), 1181–1204. http://www.jstor.org/stable/40971966
Lopez-Castro, T., Saraiya, T., Zumberg-Smith, K., & Dambreville, N. (2019). Association Between Shame and Posttraumatic Stress Disorder: A Meta-Analysis. Journal of Traumatic Stress, 32(4), 484–495. https://doi.org/10.1002/jts.22411
Messman-Moore, T. L., Walsh, K. L., & DiLillo, D. (2010). Emotion dysregulation and risky sexual behavior in revictimization. Child Abuse & Neglect, 34(12), 967–976. https://doi.org/10.1016/j.chiabu.2010.06.004
Nickerson, A., Aderka, I. M., Bryant, R. A., & Hofmann, S. G. (2013). The role of attribution of trauma responsibility in posttraumatic stress disorder following motor vehicle accidents. Depression and Anxiety, 30(5), 483–488. https://doi.org/10.1002/da.22006
North, C. S., Surís, A. M., Smith, R. P., & King, R. V. (2016). The evolution of PTSD criteria across editions of DSM. Annals of Clinical Psychiatry, 28(3), 197–208.
Øktedalen, T., Hagtvet, K. A., Hoffart, A., Langkaas, T. F., & Smucker, M. (2014). The Trauma Related Shame Inventory: Measuring Trauma-Related Shame Among Patients with PTSD. Journal of Psychopathology and Behavioral Assessment, 36(4), 600–615. https://doi.org/10.1007/s10862-014-9422-5
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., . . . Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Systematic Reviews, 10(1), 89. https://doi.org/10.1186/s13643-021-01626-4
Porritt, K., Gomersall, J., & Lockwood, C. (2014). JBI’s systematic reviews: Study selection and critical appraisal. The American Journal of Nursing, 114(6), 47–52. https://doi.org/10.1097/01.NAJ.0000450430.97383.64
Resick, P., & Schnicke, M. (1992). Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology, 60(5), 748–756. https://doi.org/10.1037//0022-006x.60.5.748
Resick, P. A., Galovski, T. E., Uhlmansiek, M. O. B., Scher, C. D., Clum, G. A., & Young-Xu, Y. (2008). A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology, 76(2), 243. https://doi.org/10.1037/0022-006X.76.2.243
Resick, P., Monson, C., & Chard, K. (2016). Cognitive processing therapy for PTSD: A comprehensive manual. Guilford Press.
Saraiya, T., & Lopez-Castro, T. (2016). Ashamed and Afraid: A Scoping Review of the Role of Shame in Post-Traumatic Stress Disorder (PTSD). Journal of Clinical Medicine, 5(11), 94. https://doi.org/10.3390/jcm5110094
Seligman, M. E., Abramson, L. Y., Semmel, A., & Von Baeyer, C. (1979). Depressive attributional style. Journal of Abnormal Psychology, 88(3), 242. https://doi.org/10.1037/0021-843X.88.3.242
Sippel, L. M., & Marshall, A. D. (2011). Posttraumatic stress disorder symptoms, intimate partner violence perpetration, and the mediating role of shame processing bias. Journal of Anxiety Disorders, 25(7), 903–910. https://doi.org/10.1016/j.janxdis.2011.05.002
Tangney, J., & Dearing, R. (2002). Shame and Guilt. Guilford Press.
Tangney, J. P., Stuewig, J., & Mashek, D. J. (2007). Moral emotions and moral behavior. Annual Review of Psychology, 58, 345–372. https://doi.org/10.1146/annurev.psych.56.091103.070145
Taylor, T. F. (2015). The influence of shame on posttrauma disorders: Have we failed to see the obvious? European Journal of Psychotraumatology, 6, 28847–28847. https://doi.org/10.3402/ejpt.v6.28847
Thompson, M., Kaslow, N. J., Weiss, B., & Nolen-Hoeksema, S. (1998). Children's attributional style questionnaire—revised: Psychometric examination 10, 166–170. https://doi.org/10.1037/1040-3590.10.2.166
Tracy, J., Robins, R., & Tangney, J. (2007). The self-conscious emotions: Theory and Research. Guilford Press.
Tran, H. N., Lipinski, A. J., Peter, S. C., Dodson, T. S., Majeed, R., Savage, U. C., & Beck, J. G. (2019). The Association Between Posttraumatic Negative Self-Conscious Cognitions and Emotions and Maladaptive Behaviors: Does Time Since Trauma Exposure Matter? Journal of Traumatic Stress, 32(2), 249–259. https://doi.org/10.1002/jts.22388
Uji, M., Shikai, N., Shono, M., & Kitamura, T. (2007). Contribution of shame and attribution style in developing PTSD among Japanese University women with negative sexual experiences. Archives of Women’s Mental Health, 10(3), 111–120. https://doi.org/10.1007/s00737-007-0177-9
Wanous, J., & Reichers, A. (1996). Estimating the Reliability of a Single-Item Measure. Psychological Reports, 78(2), 631–634. https://doi.org/10.2466/pr0.1996.78.2.631
Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. (2013a). The clinician-administered PTSD scale for DSM-5 (CAPS-5). [Assessment] Available from www.ptsd.va.gov
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schunurr, P. P. (2013b). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov
Wei, M., Alvarez, A. N., Ku, T.-Y., Russell, D. W., & Bonett, D. G. (2010). Development and validation of a Coping with Discrimination Scale: Factor structure, reliability, and validity. Journal of Counseling Psychology, 57(3), 328. https://doi.org/10.1037/a0019969
Weiss, D., & Marmar, C. (1997). The Impact of Event Scale-Revised. In J. Wilson & T. Keane (Eds.), Assessing Psychological Trauma and PTSD (pp. 399–411). Guilford Press.
Wilson, J. P., Drozdek, B., & Turkovic, S. (2006). Posttraumatic shame and guilt. Trauma Violence & Abuse, 7(2), 122–141. https://doi.org/10.1177/1524838005285914
Wojcik, K. D., Cox, D. W., Kealy, D., Grau, P. P., Wetterneck, C. T., & Zumbo, B. (2022). Maladaptive Schemas and Posttraumatic Stress Disorder Symptom Severity: Investigating the Mediating Role of Posttraumatic Negative Self-Appraisals among Patients in a Partial Hospitalization Program. Journal of Aggression, Maltreatment & Trauma, 31(3), 322–338. https://doi.org/10.1080/10926771.2021.1994496
Wolfe, V. (2002). Children’s Impact of Traumatic Events Scale-II. Unpublished assesment instrument.
Wolfe, V., Gentile, C., & Bourdeau, P. (1987). History of victimization form (unpublished assessment instrument). London Health Science Centre.
Wolfe, V. V., Gentile, C., Michienzi, T., Sas, L., & Wolfe, D. A. (1991). The children’s impact of traumatic events scale: A measure of post-sexual abuse PTSD symptoms. Behavioral Assessment, 13, 359–383.
Zerach, G., & Levi-Belz, Y. (2018). Moral injury process and its psychological consequences among Israeli combat veterans. Journal of Clinical Psychology, 74(9), 1526–1544. https://doi.org/10.1002/jclp.22598
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
RS and DB contributed to the development of the study concept and methodology. RS was responsible for data acquisition, abstract and full-text screening, and data extraction. KD assisted with abstract and full text screening. RS was responsible for data analysis and interpretation, manuscript write-up. All authors approved the final version of the paper for submission.
Corresponding author
Ethics declarations
Ethics Approval
This is a systematic review, and no ethical approval is required.
Informed Consent
Informed consent was not required as this is a review of existing peer reviewed research that has been de-identified by respective authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seah, R., Dwyer, K. & Berle, D. Was it me? The Role of Attributions and Shame in Posttraumatic Stress Disorder (PTSD): A Systematic Review. Trends in Psychol. (2023). https://doi.org/10.1007/s43076-023-00315-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s43076-023-00315-6