Abstract
Intervertebral disc degenerative disease (IDD), which usually causes lower back and neck pain, is one of the most widespread musculoskeletal disorders and often causes a low quality of life. However, the surgical and conservative treatments commonly used in clinical practice are not effective. Previous studies have identified curcumin (Cur) as a potential therapeutic agent. However, its development in this regard has been limited due to its low dissolution, instability in water, and rapid metabolism. In this study, we developed a novel anti-inflammatory composite hydrogel scaffold with curcumin encapsulated in solid lipid nanoparticles and mixed it with gelatin methacrylate (GelMA) hydrogel to treat IDD. The hydrogel scaffold, denoted Cur-solid lipid nanoparticles (SLNs)/GelMA, promoted the restoration of Collagen type II (Col II) and aggrecan expression levels in vivo, indicating that the regeneration of the intervertebral discs was effective. Combined in vitro studies showed that Cur-SLNs inhibited the expression of the inflammatory factors TNF-α and IL-6. Additionally, immunofluorescence and western blotting experiments verified that Cur-SLNs regulated the recovery of Col II and aggrecan in an inflammatory environment and promoted the metabolic homeostasis of the extramedullary cell matrix. In conclusion, this study provides a new strategy to promote IDD regeneration, which brings new application prospects.
Article highlights
-
The combination of Cur encapsulated with SLNs and GelMA hydrogel in the treatment of IDD can reestablish the metabolic homeostasis of the pathologic process and reduce the inflammatory response.
-
This novel anti-inflammatory composite hydrogel scaffold can facilitate the repair of IDD and offers new perspectives for the treatment of IDD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Intervertebral disc degeneration (IDD) is one of the most widespread disorders of the musculoskeletal system and is the main pathological cause of lower back pain (LBP) [1]. However, surgical and conservative drug treatments that are commonly used in clinical practice have not achieved conclusive therapeutic results. IDD is the progressive failure of the intervertebral discs (IVD) and is caused by aging, as well as socioenvironmental and genetic factors. This leads to the continuous deterioration of the microenvironment of the nucleus pulposus (NP) gelatinous tissue at the center of the IVD, and abnormal metabolic reactions of the nucleus pulposus cells (NPC) [2,3,4]. During this process, the overexpression of matrix metalloproteinase (MMP) leads to the progressive damage of the extracellular matrix (ECM). This enhances NPC aging and death and accelerates ECM degradation and mechanical changes [5,6,7]. Therefore, the most likely mechanism leading to IDD is an imbalance in NP anabolic activity, where the inflammatory process is dominated by interleukin-1β (IL-1β) and tumor necrosis factor-α (TNF-α) [8, 9]. The most effective way to repair IDD is to re-establish ECM metabolic homeostasis and reduce the inflammatory response. The NP maintains biological functions through the production of the ECM, including Col II and polymeric proteins. Among the spinal tissues, the NP is subjected to the highest amount of mechanical stress and activity [10, 11]. Therefore, the key to improving regenerative therapy for IDD lies in repairing the NP [12]. The biomaterials used to replace the NP are mainly injectable synthetic or bio-based hydrogels [13,14,15].
Synthetic or bio-based hydrogels such as those derived from polyacrylate, polyacrylamide, hyaluronic acid, collagen in the ECM, and chitosan have received considerable attention because of their biocompatibility and natural biodegradability [14, 16,17,18]. As 3D scaffolds for both tissue repair and drug delivery systems, synthetic hydrogels are important components in tissue repair engineering [19]. Hydrogels are in increasing demand because of their similarity to the cellular microenvironment [20]. Among them, gelatin methacrylate (GelMA) has become a representative hydrogel that is widely used in the biomedical field [21]. For example, GelMA can be combined with bioactive supramolecular nanofibers to accomplish autologous chondrocyte repair of osteochondral defects [22]. Zhu et al. have reported that GelMA hydrogels, with the addition of ECM and platelet-rich plasma (PRP), can coordinate immunomodulatory responses, reduce inflammation, and promote angiogenesis [23]. These results suggest that GelMA hydrogels are good vehicles for drug, gene, or growth factor delivery. However, after disc injuries are incurred, hydrogels alone are unable to directly modulate the microenvironment. Tissue degeneration, inflammatory responses, and metabolic imbalances occurring at the site of IDD injury require medication for critical treatment.
Curcumin (Cur) is a naturally occurring polyphenolic compound extracted from turmeric [24]. Several researchers have previously reported the anti-inflammatory effects of Cur on injuries of the cartilaginous tissue, tendons, and bone, as well as on injury-related skin infections [25,26,27]. In addition, its anti-aging, -bacterial, -oxidant, and -tumor properties are well documented [28]. Cur has been shown to alleviate disc degeneration by protecting chondrocytes during intermittent cyclic tension, and by mediating autophagy, which enhances the adaptation of endplate chondrocytes to high-intensity loading [29]. A previous study revealed the suppressive effect of Cur on the nuclear transcription factor-κB (NF-κB) pathway when treating lumbar disc degeneration [30]. Furthermore, Cur inhibits the production of the inflammatory factors TNF-α and IL-1βand restricts oxidative stress [31,32,33]. Nevertheless, Cur is a highly hydrophobic molecule with low solubility and instability in water and is therefore rapidly metabolized and poorly bioavailable [34]. Various approaches have been employed to alleviate the pharmacokinetic problems of Cur, including the encapsulation of Cur inside nanoparticles, nanoemulsions, liposomes, and microspheres [35,36,37,38].
Solid lipid nanoparticles (SLNs) combine many of the advantages of nanoparticles and liposomes, making them promising delivery vehicles [39]. Compared to nanoparticles, SLNs are composed mainly of physiologically acceptable lipid components, thus reducing immune rejection and decreasing the probability of acute or chronic toxicity [40]. At the same time, compared to liposomes, SLNs are more stable, largely free from drug leakage, and could prolong the release of drug molecules [41, 42]. Therefore, many studies have focused on Cur-SLNs and their potential in improving Cur bioavailability. SLNs loaded with Cur are effective in the treatment of Alzheimer’s disease [43] and in cancer treatments such as lung, rectal, and breast cancers [28, 44, 45]. To our knowledge, no studies have combined Cur encapsulated SLNs with GelMA for the therapeutic improvement of IDD pathological processes.
This study aimed to develop a novel anti-inflammatory composite hydrogel scaffold by combining Cur-coated SLNs with GelMA hydrogel scaffolds (Cur-SLNs/GelMA). This Cur-SLNs/GelMA was characterized, and numerous in vivo and in vitro experiments were used to verify that the scaffold could promote the balance of degenerative disc ECM metabolism, regulate the immune microenvironment of disc cells, and facilitate the repair treatment of IDD. This novel anti-inflammatory composite hydrogel scaffold provides new prospects for IDD therapy.
2 Materials and methods
2.1 Characterization of Cur-loaded SLNs
2.1.1 Preparation of Cur-loaded SLNs
Cur-SLNs were prepared using the solvent emulsion diffusion low-temperature solidification method as previously reported [46]. The oil phase: Cur (25 µM) was added to a solution of acetone and chloroform (V/V = 1:1) and dissolved at 70 °C in combination with stearic acid (100 mg), cholesterol (100 mg), and lecithin (220 mg). Poloxam (100 mg) was dissolved in pure water (1 mL) with Tween 80 and mixed to form the aqueous phase (70 °C). The oil phase was then injected into the aqueous phase at 1 mL/min, 600 rpm, and stirred for 120 min to form an emulsion. Ice water was added and stirred for 60 min to obtain cured Cur-SLNs. Control SLNs (excluding Cur) were prepared using the same method and kept at 4 °C.
2.1.2 Transmission electron microscopy (TEM) observation of Cur-loaded SLNs
The synthesized Cur-SLNs were diluted and aspirated in 10 µL drops on the copper network of the carbon film, which was negatively stained with phosphotungstic acid and dried. Finally, the size and morphology of the Cur-SLNs were observed by TEM (H-7500; Hitachi Ltd., Japan).
2.1.3 X-ray auto-diffractometer (XRD) detection of Cur-SLNs
Cur, lyophilized empty SLNs, and Cur-SLNs were weighed at 10 mg each and added to the grooves of the observation slides. The powder was then covered uniformly on the surface of the grooves with slides, and the XRD patterns of the samples were read in an X-ray diffraction analyzer (Rigaku Corporation, Japan). Parameter settings: copper target; voltage of 60 kV; current of 40 mA; scan interval of 5° to 90°; scan speed of 10°/min.
2.1.4 Fourier transform infrared spectrophotometric (FTIR) detection of Cur-SLNs
Cur, lyophilized empty SLNs, and Cur-SLN powders were weighed and sampled separately, mixed with KBr pellets, and then the infrared absorption peaks of the samples, in the wavelength range of 400 to 4000 cm−1 in FTIR spectra, were observed and recorded using an FTIR spectrometer (Thermo Fisher Nicolet iS 50, USA).
2.1.5 Encapsulation efficiency (EE) and drug loading capacity (DL) of Cur-SLNs
The prepared Cur-SLNs mentioned above were freeze-dried and weighed at 5 mg. 5 ml of anhydrous ethanol was added to dissolve the lyophilized sample, and then 1 ml of the dissolved sample was injected into the UV spectrophotometer to determine the absorption peak at 425 nm. The drug encapsulation rate and drug loading of the Cur-SLNs were then calculated using the Cur standard curve, Y = 0.0787X + 0.1028 (R² = 0.9991; n = 5). The specific calculation equation is as follows:
2.1.6 In vitro release profile of Cur-SLNs
The release of Cur from the Cur-SLNs was assessed using the methods of previous studies [28]. First, 30 mg of Cur-SLNs (about 3 mg of Cur) and an appropriate amount of free Cur (3 mg of Cur) were weighed into 10 mL of methanol solution and dispersed. Then 1 ml was added into a dialysis bag (dialysis molecular weight 14 kDa), immersed into a beaker containing 50 ml of a distilled water-methanol mixture (1:1, v/v), placed in a constant temperature water bath shaker (speed 100 rpm), and shaken at 37 °C. The dialysate was timed from 0 and removed at set time points (i.e., 1, 8, 16, 24, 48, 72 h) while replenishing the same volume of dialysate. The removed dialysate was filtered using a 0.45 μm membrane filter and the absorbance was measured by UV spectrophotometer (425 nm). The in vitro release profile of the curcumin solid lipid nanoparticles was then calculated.
2.2 Nuclear magnetic resonance (NMR) of gelatin and GelMA
Proton nuclear magnetic resonance (1H-NMR) spectra were examined for gelatin and GelMA using a 400 MHz spectrometer (NMR, Bruker 400 M, Switzerland), and the data were analyzed using MestReNova software. D2O was used as a solvent and all spectra were measured at room temperature. The degree of substitution was calculated by normalizing the number of free amino groups of the original gelatin [47].
2.3 Cur-SLNs/GelMA hydrogel preparation
Solutions of GelMA hydrogels were obtained by dissolving 0.05 g of lithium phenyl 2,4,6-trimethylbenzoyl phosphonate (LAP) (EFL, Suzhou, China) in 20 ml of phosphate-buffered saline (PBS) at 40–50 °C for 15 min in a water bath. GelMA (1 g) was then added to the LAP/PBS solution in a water bath at 60–70 °C for 20–30 min, protected from light until dissolved, with shaking every 5–10 min. For cell culture, the hydrogel solution was sterilized in advance using a sterile 0.22 μm needle filter [48].
Finally, appropriate amounts of Cur and Cur-SLNs were homogeneously mixed with the GelMA hydrogel solution to the desired concentration (25 µM) and cured under UV light to obtain the corresponding Cur/GelMA and Cur-SLN/GelMA hydrogel scaffolds.
2.4 Characterization of Cur-SLNs/GelMA hydrogel scaffolds
Hydrogel scaffolds were prepared as described above and subjected to material characterization tests. The scaffolds were freeze-dried with the use of a Eurotherm LS 40 (Severn Science Ltd, England). After spraying the hydrogel scaffolds with gold, photographs were taken using the Hitachi TM-1000 scanning electron microscope (SEM) (Hitachi, Japan). Energy spectral analysis was chosen to detect the surface composition of the scaffolds, and Image J software (NIH, USA) was selected to measure porosity and average pore size. In addition, we measured the hydrophilic properties using a Chengde Dingsheng JY-82 C video contact angle tester (Dataphysics, Germany) and Young’s modulus using a universal mechanical testing machine (E10000, Instron, USA).
2.5 In vitro anti-inflammatory analysis of NPCs on Cur-loaded SLNs
2.5.1 NPC isolation and culture
NPC was obtained from Sprague-Dawley (SD) rats of 200 to 230 g (Hefei Shushan Experimental Animal Centre). Briefly, intervertebral discs from the tails of SD rats were collected, and NP tissue was isolated. Tissues were treated with type II collagenase for 3 h and blow-dried every hour. The residual tissue was filtered through a 70 μm cell sieve (Biosharp, China), then the filtered cells were collected and incubated with DMEM/F12 (Gibco, USA) containing 10% fetal bovine serum (Gibco, USA) and 1% penicillin-streptomycin (Biosharp, China) in culture. Incubator conditions were maintained at 37 °C and 5% CO2, and third-generation cells were selected for the study.
2.5.2 Cell viability and proliferation assessment
To identify the toxic action of different concentrations of Cur on NPC, Cell Counting Kit-8 (CCK-8) (Invitrogen, USA) was applied to assay the growth activity of cells at different Cur concentrations. Cells were resuspended and uniformly dispersed in 96-well plates and co-cultured with different concentrations of Cur for 24 h. To prepare for the assay, the complete medium was removed, and fresh cultures containing 10% CCK-8 were added and incubated with the cells for 2 h under normal culture conditions. Finally, the absorbance at 450 nm was measured by a spectrophotometer (BioTek, USA) and counted.
2.5.3 Enzyme-linked immunosorbent assay
To assess the ability of Cur and Cur-SLNs to alleviate inflammation in NPCs, cytokine secretion levels under the effect of the pro-inflammatory factor IL-1β were detected by an enzyme-linked immunosorbent assay (ELISA) (RayBiotech, USA) kit, following the reagent instructions. Briefly, the blank control, Cur, and Cur-SLN groups were co-cultured with NPCs under the effect of IL-1β for 24 h. The cell supernatants were then mixed with reaction buffer to assay the extent of IL-6 and TNF-α secretion. Finally, the absorbance of the experimental samples was measured at the corresponding wavelengths using a microplate reader.
2.5.4 Immunofluorescence analysis
Briefly, after co-culturing different groups of NPCs with the inflammation-inducing factor IL-1β in 24-well plates, the associated protein expression levels in each group were examined. The supernatant was discarded, and the cells were immobilized in 4% paraformaldehyde for 20 min, permeabilized with 0.3% Triton X-100 for 5 min, then closed with a sealing solution containing 10% goat serum for 2 h at 4 °C. The supernatant was aspirated and incubated with Aggrecan antibody (Affinity, USA), Col II antibody (Affinity, USA), and NF-kB P65 antibody (Affinity, USA) overnight at 4 °C. After approximately 12 h, the cells were incubated with Goat Anti-Rabbit IgG(H + L) Fluor 488-conjugated (Affinity, USA) or Goat Anti-Rabbit IgG(H + L) Cy3-conjugated (Affinity, USA) for 2 h, and cell nuclei were incubated with DAPI (4′,6 -Diamidino-2-phenylindole) (Biosharp, China) for 10 min. Cells were observed and photographed using an inverted fluorescence microscope (Zeiss Axio Observer Z1, Germany).
2.5.5 Protein extraction and Western blotting analysis
Cells were lysed with Radio-Immunoprecipitation Assay (RIPA) lysis buffer (Thermo Scientific, USA) containing phosphatase and protease inhibitors, and cellular protein concentrations were determined using a Bicinchoninic acid (BCA) protein kit. Proteins were separated by 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), transferred to polyvinylidene fluoride (PVDF) membranes by electroblotting, and sealed with 5% bovine serum albumin (BSA) for 2 h. Afterward, blots were incubated overnight in the primary antibodies: beta-Actin Antibody (Affinity, USA), aggrecan Antibody (Affinity, USA), and Col II Antibody (Affinity, USA). Following this, they were incubated with the Goat Anti-Rabbit IgG(H + L) HRP (Proteintech, USA) for 2 h. The proteins were visualized with Super Signal West chemiluminescent substrate (Thermo Scientific, USA), and the protein bands were measured in grayscale and normalized using ImageJ software (NIH, USA).
2.6 In vivo anti-inflammatory analysis of NPCs on Cur-SLNs/GelMA hydrogel scaffolds
2.6.1 Construction of rat IDD model
Rat husbandry and experimental surgical procedures were authorized by the Ethics Committee of the Medical Faculty of Bengbu Medical College (approval number: 2,021,272) and performed following the National Institute of Health (NIH, Bethesda, MD) guidelines. Eight- to twelve-week-old SD rats (250 g) were used in this study, and were anesthetized by an intraperitoneal injection of ketamine with dimethoate (10:7,100 mg/kg). The rats were randomized into four groups: the control group for surgically induced IDD alone (n = 10), GelMA hydrogel scaffold treatment group (n = 10), Cur/GelMA hydrogel scaffold treatment group (n = 10), and Cur-SLNs/GelMA hydrogel scaffold treatment group (n = 10). The caudal vertebral Co6/7 or Co7/8 gap was selected for a puncture, and the selected caudal intervertebral segments were determined by finger palpation and fluoroscopy. The caudal skin was disinfected with iodophor, and a 20-gauge needle was inserted at the corresponding fibrous ring level to penetrate the NP to the opposite fibrous ring. Once complete penetration was achieved, the needle was spun 360 degrees and kept in place for 30 s. The experimental group was injected with the corresponding hydrogel solution into the penetrated disc, and photocoagulation was achieved using a fiber-optic wire. After the experiment, the rats were given a normal diet and a clean space in which to move around.
2.6.2 Haematoxylin-eosin staining analysis
The corresponding disc segments were removed for histological examination and analyzed at 6 and 12 weeks after the experimental injection was received. The disc segments were soaked in 4% paraformaldehyde for 48 h and then transferred to an EDTA decalcifying solution (Solarbio, China) for about a month. The EDTA decalcifying solution was replaced once a day. Subsequently, the disc blocks were paraffin-embedded and cut into midsagittal plane Sect. (8 μm thick). Sections were stained with hematoxylin and eosin (HE) to ascertain the number and morphology of the various tissue cells, as well as the number of ECM. For photographic analysis, the sections were observed under a microscope (Nikon, USA).
2.6.3 Immunohistochemical staining analysis
Sections were processed for immunohistochemical (IHC) analysis and paraffin-embedded sections were processed as described above. 8 μm thick histological sections were produced with a slicer and sections were first incubated with 5% (w/v) BSA, followed by overnight incubation with aggrecan Antibody (Affinity, USA) and Col II Antibody (Affinity, USA) primary antibodies. After approximately 12 h, the sections were incubated with horseradish peroxidase-coupled secondary antibody (Affinity, USA) for 2 h. Diaminobenzidine was used to produce brown precipitates. To evaluate the IHC staining, photographs were obtained using a light microscope (Nikon, USA).
2.7 Statistical analysis
A minimum of three independent replicate groups were used for each experiment, and all results were statistically analyzed with GraphPad Prism software (GraphPad Software, USA). The data are expressed as mean ± standard deviation, and analysis of variance (ANOVA) was used between groups (P < 0.05).
3 Results
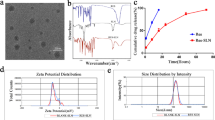
3.1 Characterization of Cur-SLNs
As shown in Fig. 1A, the TEM shows that the Cur-SLNs are all uniformly round with a size of about 80 nm. XRD analysis of Cur, SLN, and Cur-SLNs was then performed, as shown in Fig. 1B, Cur showed several sharp crystal diffraction peaks, including at 13.44°, 16.57°, 19.64°, 29.39°, and 40.12°, indicating that it is a crystalline material. In contrast, two broad diffraction peaks were observed at 12.5–22.5° and 22.5–30° for the empty SLNs or Cur-SLNs, and no crystalline diffraction peaks or diminished Cur-free drug characteristic peaks were observed for the drug-loaded particles. This indicated that Cur is encapsulated in the nanopreparations as amorphous powder or molecules. Combined with the infrared spectrum of Cur-SLNs, as shown in Fig. 1C, the FTIR spectrum of Cur-SLNs showed the characteristic C–H absorption peak of Cur (3300 cm−1) while containing the characteristic 2850–3000 cm−1 absorption peak of SLN, indicating that Cur has been stably combined with SLNs. In addition, EE and DL are important indicators to be observed in drug synthesis. We calculated the encapsulation rate of Cur-SLNs as 94.6 ± 1.2% and the drug loading as 8.91 ± 0.29% based on the standard curve. And we did a slow-release experiment comparing Cur-SLNs with free drug solution, and in Fig. 1D we can observe that Cur-SLNs prolonged the slow release of Cur. Sixteen hours later, the normal drug solution was almost completely slowed down, while the Cur-SLNs group was only slowed down by about 40%. This indicates that the model promotes the duration of Cur drug action.
3.2 Characterization of Cur-SLNs/GelMA hydrogel scaffolds
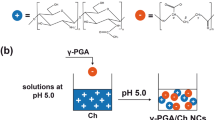
In our study, we first needed to determine the successful synthesis of GelMA. We used 1H-NMR spectra to determine the degree of methacryloyl functionalization (DoF) of GelMA, as shown in Fig. 2G. The NMR results of GelMA showed a peak of around 5.5 ppm corresponding to the acrylic acid proton of the methacryloyl group. 1.8–1.9 ppm of the signal corresponded to the methyl proton of the grafted methacryloyl group. At the same time, the position of the lysine methylene corresponding to gelatin was significantly lower, around 3.0 ppm. These variations between GelMA and gelatin indicate the degree of covalent functionalization of gelatin with methacryloyl, and we calculated the degree of substitution of GelMA from the peak area to be 30.9%. Then, to make sure that the Cur-SLNs had been successfully incorporated into the GelMA hydrogels, we did energy spectrum analysis experiments while using the SEM. As shown in Fig. 2B, we observed P and S elements in the Cur-SLNs/GelMA hydrogel scaffold, which are not present in the pure GelMA hydrogel scaffold and belong to the SLN composition. The detection of SLN components in the Cur-SLNs/GelMA hydrogel scaffolds indicated that Cur-SLNs had been successfully incorporated into the GelMA hydrogels. As shown in Fig. 2A and D, the SEM results of the GelMA, Cur/GelMA, and Cur-SLN/GelMA hydrogel scaffolds showed that all three lyophilized hydrogel scaffolds had large porosity, and the pore sizes (Fig. 2C) were appropriate for cell growth and proliferation. No significant difference was observed between the groups. Then the hydrophilicity of the hydrogel scaffolds was evaluated by measuring their water contact angles. As shown in Fig. 2E, the Cur-SLNs/GelMA hydrogel scaffold showed a significantly lower water contact angle, indicating that this hydrogel scaffold had the best hydrophilicity. Finally, we measured Young’s modulus of the GelMA, Cur/GelMA, and Cur-SLNs/GelMA hydrogel scaffolds, as shown in Fig. 2F, and found that Young’s modulus of Cur/GelMA and Cur-SLNs/GelMA was slightly reduced compared to that of GelMA, but this difference was not statistically significant. This suggests that the addition of Cur-SLNs did not affect Young’s modulus of the original hydrogel scaffolds.
Characterization of Cur-SLNs/GelMA hydrogel scaffolds. A Scanning electron microscopy photograph of the Cur-SLNs/GelMA hydrogel scaffolds. B Energy dispersive spectrum analysis of Cur-SLNs/GelMA scaffolds. C, D Quantification of the pore size and porosity of GelMA, Cur/GelMA, and Cur-SLNs/GelMA scaffolds. E, F WCA and Young’s modulus of different hydrogel scaffolds. G 1H NMR spectra and molecular structures of Gelatin and GelMA. (n = 3, *P < 0.05)
3.3 In vitro biocompatibility of the Cur-SLNs/GelMA hydrogel
To create a pathological inflammatory environment similar to that of IDD, we added an IL-1β-inducing factor to the NPC culture. As shown in Fig. 3A and B, we measured the cellular activity of NPC at different concentrations of IL-1β at 24 and 72 h. With an increase in IL-1β concentration, cell proliferation activity gradually decreased, indicating that IL-1β had an inhibitory effect on the proliferation of NPC. However, after simultaneously adding Cur or Cur-SLNs to the NPC co-culture, we found that the inhibited cellular activity was alleviated. As shown in Fig. 3C, SLNs encapsulating 25 µM curcumin had the best results after IL-1β-induced inflammation and the greatest cell proliferation viability at this concentration; therefore, we decided to use 25 µM curcumin in the experiments to follow.
Cell growth and proliferation activity. A, B Cell proliferation assay of NPCs in the inflammatory microenvironment at different periods (relative to the 0 ng/ml group). C Cell proliferation assay of differently treated NPCs in the inflammatory microenvironment (relative to the 0 + group; “−”: Without IL-1β; “+”: With IL-1β) (n = 3, *P < 0.05, **P < 0.01, ***P < 0.005)
3.4 Anti-inflammatory properties of Cur-SLNs/GelMA hydrogels in vitro
To further explore the in vitro anti-inflammatory properties of Cur-SLNs, an ELISA kit was used to detect the expression of the inflammatory regulators IL-6 and TNF-α in the blank control group, the experimental group with IL-1β alone, and the co-culture group with Cur or Cur-SLNs after the addition of IL-1β. TNF-α and IL-6 are associated with the degree of inflammatory response; therefore, measuring the fluorescence intensity of TNF-α and IL-6 can visually reflect the anti-inflammatory ability of each group. From Fig. 4A and B, it can be seen that Cur-SLNs have significant anti-inflammatory regulatory effects on cells, better than that of the direct addition of Cur.
3.5 Effects of Cur-SLNs on NPCs in the in vitro environment
To verify that Cur-SLNs can promote metabolic homeostasis of the degenerative intervertebral disc ECM, we performed immunofluorescence assays and western blotting on the co-cultured cells. As shown in Fig. 5A, the nuclei (blue) were stained with DAPI, and the results show cell growth in all groups. Furthermore, the expression of aggrecan was detectable in all groups. However, the second group (treated with IL-1β alone and excluding curcumin) showed extremely low expression levels of aggrecan. In contrast, aggrecan expression was observed in the third group (treated with Cur). However, these levels were not as high as those in the fourth group (treated with Cur-SLNs). Quantitative analysis of Fig. 5C revealed that the best recovery of aggrecan expression was that of the Cur-SLN group. As shown in Fig. 5B and D, the expression of Col II showed the same trend. Under the disruption of the IL-1β inflammatory factor, the Cur-SLN group restored Col II expression levels to a state that was similar to normal. This indicates that Cur-SLNs can regulate the inflammatory environment of NPCs and alleviate imbalances in ECM metabolism. In addition, gene expression was normalized by quantifying actin values (housekeeping genes), as shown in Fig. 5E, F, G, and H (Raw data available in the supplementary information document). Compared with the gene expression in blank control cells (excluding treatment), the expression intensity of aggrecan and Col II were the highest in the Cur-SLN group cells. Col II expression was similar to the normal level, while aggrecan expression was essentially indistinguishable from normal levels. This indicates that Cur-SLNs are effective in regulating the repair of aggrecan and Col II expression and can alleviate the imbalance of anabolic/catabolic activities in NPC, which is consistent with the immunofluorescence results. To further investigate the protective mechanism of Cur against NPCs and its inhibitory effect on ECM degradation, we measured the expression level of P65 by immunofluorescence assay to identify the activation level of the NF-kB pathway. As shown in Fig. 6A and B, P65 expression was extremely high in the IL-1β-treated group, indicating that IL-1β activated this pathway. However, this expression was suppressed in the Cur-SLN-treated group and returned to normal levels in the control group.
Results of immunofluorescence detection and western blotting. A, B Immunofluorescence staining of aggrecan and Col II in NPCs in different cultural environments. C, D Quantitative analysis of aggrecan and Col II positive cell expression. E Western blot of aggrecan and β-Actin (Different parts cut from the same gel). F Western blot of Col II and β-Actin (Different parts cut from the same gel). G, H Protein expression result of aggrecan and Col II in NPCs by semi-quantification of western blot. (n = 3, *P < 0.05, **P < 0.01, ***P < 0.005, ****P < 0.001)
3.6 Establishment of the intervertebral disc degeneration model in rats
To successfully construct an experimental model of IDD in SD rats, we localized the defect to a specific intervertebral disc space using a small-animal X-ray imaging technique. As shown in Fig. 7C, under a fluoroscopic lens, we directly observed the size of the rat intervertebral disc and the gap width, which aided in selecting an appropriately sized needle for direct puncture. We positioned the puncture at Co6/7 or Co7/8, which are the two most evident sites on X-ray film, are easily manipulated, and are the usual sites for IDD models. Figure 7 A shows the corresponding gap position according to the X-ray image, which aids in visualization. Figure 7B shows a macroscopic image obtained after needle insertion.
3.7 Effect of Cur-SLNs/GelMA hydrogel scaffolds on disc repair in vivo
Rat IDD models were used to verify whether the Cur-SLN/GelMA hydrogel scaffold alleviated the IDD process and promoted IDD healing. Rats were treated topically with GelMA, Cur/GelMA, or Cur-SLNs/GelMA hydrogel scaffolds at the sites of disc injury, and recovery of the defected sites was assessed by HE and IHC at 6 and 12 weeks. As shown in Fig. 8A, in the control group, the NP was degraded after 12 weeks, and the fibrous rings were squeezed into the NP with almost no remnants of NPC. In contrast, the GelMA and Cur/GelMA hydrogel scaffold groups still had some remnants of myeloid tissue, but the fibrous tissue arrangement was disorganized, and the cavity was evident at 6 weeks. The Cur-SLNs/GelMA hydrogel scaffold group had fuller NPC, and most of the NPC was restored by 12 weeks. Figure 8B and C shows the local distribution of Col II and aggrecan in the intervertebral disc. We examined the expression of Col II and aggrecan in each group by IHC staining. First, we observed that protein expression increased over time in all groups, and this increase was more pronounced in the Cur/GelMA and Cur-SLNs/GelMA hydrogel scaffolds. We observed that the medullary nuclei in the Cur-SLNs/GelMA hydrogel scaffold group were relatively well-arranged and well-integrated with the surrounding tissues. Finally, combined with the semi-quantitative data analysis of IHC staining (Fig. 8D, E), we determined that the expression of aggrecan and Col II proteins in the Cur-SLNs/GelMA hydrogel scaffold group was much higher than that in the other groups. This indicates that the Cur-SLNs/GelMA hydrogel scaffold can restore the metabolic balance of the ECM affected by the inflammatory environment and promote the repair of the intervertebral disc.
Analysis of HE and IHC results. A H&E staining of coccygeal discs from the different groups. B, C Immunohistochemical staining of coccygeal discs from the different groups. D, E Quantitative analysis of Col II and aggrecan from the different groups at 6 and 12 weeks after molding. Data are the mean ± SD of three independent experiments (n = 3, *P < 0.05, **P < 0.01, ***P < 0.005, ****P < 0.001)
4 Discussion
Intervertebral disc injuries are common clinical conditions that seriously affect patient health. The rapid development of biological tissue engineering has provided a rational pathway for the mitigation and repair of disc injury or degeneration. Biological tissue engineering comprises three core components: seed cells, scaffold materials, and growth factors. Among these, scaffolds can mimic the microenvironment for NPC proliferation and growth, and provide mechanical support for the extrusion environment of the intervertebral disc to facilitate the repair process. In recent years, GelMA hydrogels have been widely used because of their biocompatibility in mimicking the in vivo cell microenvironment and providing a good environment for cell growth and attachment [49, 50]. We chose GelMA hydrogel because of its ability to fit into the disc environment and fill the defective disc cavity in vivo, aiding in cell repair. As shown in Fig. 7A, the structural arrangement of the annulus fibrosus in the group treated with the hydrogel was more regular than that of the control group, which improved the healing process, because the defect was largely due to the disorganized tissue structure.
GelMA hydrogels have been combined with bioactive and functional nanomaterials, and specific drugs to improve their biological properties. It is therefore important to select one of these three elements in tissue engineering i.e., the correct biological factors. We chose to combine Cur and SLN, to investigate whether the combination could improve the effects of Cur. Our results confirmed that the Cur-SLN group outperformed the Cur group, both in vitro and in vivo. SLNs have been in use as drug carriers in pharmaceutical manufacturing for approximately 25 years, and their improved stability and ability to modulate drug delivery might be more advantageous than other systems [51, 52]. Previous studies have reported that SLNs containing Cur demonstrate superior results when compared to Cur alone, allowing for higher bioavailability of Cur and improved application in gastrointestinal diseases [53, 54]. However, to the best of our knowledge, this is the first time that Cur-SLNs have been applied to IDD therapy, and also the first time that the underlying mechanisms have been investigated.
Cur has been used in a variety of applications. It has been used to treat gastrointestinal problems by downregulating genes such as NF-kB and IL-6 [34] and to alleviate liver disease by inhibiting TGF-β [55]. In addition, Cur has been used in combination with conventional anticancer drugs, such as Adriamycin, paclitaxel, and cyclophosphamide, to enhance the effects of chemotherapy. This was achieved through decreasing transcriptional activation of the Pgp promoter (P65/P50) and inhibiting the expression of MMP-9, NF-kB, and COX-2 [56, 57]. In addition, it is well known that Cur can inhibit TNF-α, il-6,8,12, COX-2, and iNOS to regulate the inflammatory status [58]. It is therefore possible that Cur-SLNs can alleviate the inflammatory environment, in vitro, caused by IL-1β and restore the expression of aggrecan and Col II. We speculate that by alleviating the inflammatory response and maintaining ECM homeostasis, the Cur-SLN/GelMA hydrogel scaffold effectively treats disc injury in vivo in rats. We also investigated the changes in the P65 gene during the treatment process to further investigate the therapeutic mechanism of the Cur-SLNs/GelMA hydrogel scaffold.
Combined with the pathological process of IDD, we found that a distinctive feature of degenerated lumbar discs is the enhanced expression of NF-κB target genes, such as the inflammatory factors and MMP [59]. Previous studies have shown a massive accumulation of NF-κB in the degenerated NP tissue compared to normal lumbar disc tissue [30]. The NF-kB pathway is implicated in controlling the pathogenesis of IDD [60], and its activation leads to enhanced expression of inflammatory factors and the degradation of ECM [61]. In contrast, the heterodimer P50-P65 is considered to be the most abundant form of NF-κB and has been shown to regulate the expression of many genes [62]. We selected the P65 gene for immunofluorescence detection, thus using it to assess the activation level of the NF-κB pathway. Therefore, as illustrated in Fig. 5A and B, the expression level of P65 was extremely high in the IL-1β-treated group. The highest secretion of inflammatory factors (TNF-α and IL-6) in this group was also reflected in the ELISA results. This suggests that the NF-kB pathway is activated by IL-1β-treated NP cells. In contrast, the fluorescence expression values of P65 were markedly reduced in the Cur-SLN-treated cells compared with the IL-1β-treated cells alone, indicating that the NF-kB pathway was inactivated. This suggests that Cur-SLNs suppress inflammation and cell apoptosis through the inhibition of the NF-kB pathway. However, we only detected P65 by immunofluorescence, and the amount of data obtained was rather low. We plan to improve on the data surrounding the P65 experiments in future studies.
5 Conclusion
In this study, combining Cur-SLNs with a GelMA hydrogel solution to prepare a Cur-SLNs/GelMA hydrogel scaffold provides a new therapeutic strategy to alleviate intervertebral disc degeneration. It combines the advantages of nanoparticle-based and curcumin combination therapies with the superior mechanical properties of the GelMA hydrogel scaffold, resulting in excellent therapeutic effects. Compared to GelMA hydrogel scaffolds alone or GelMA hydrogel scaffolds combined with Cur, the Cur-SLNs/GelMA hydrogel scaffold has a therapeutic effect that is far greater. It can promote the remission of IDD by regulating the stability of ECM metabolism in the NP and reducing the inflammatory response. However, our results involving the NF-kB pathway are superficial and need further investigation. Therefore, the study of Cur-SLNs/GelMA hydrogel scaffolds for disc degeneration repair is still in the preliminary stage, and further exploration needs to be done before clinical translation is possible. Our strategy of combining Cur-SLNs with GelMA hydrogel offers a promising novel treatment for the regeneration of IDD.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Peng Y, Qing X, Lin H, Huang D, Li J, Tian S, Liu S, Lv X, Ma K, Li R et al (2021) Decellularized disc hydrogels for hBMSCs tissue-specific differentiation and tissue regeneration. Bioactive Mater 6(10):3541–3556. https://doi.org/10.1016/j.bioactmat.2021.03.014
Zheng G, Pan Z, Zhan Y, Tang Q, Zheng F, Zhou Y, Wu Y, Zhou Y, Chen D, Chen J et al (2019) TFEB protects nucleus pulposus cells against apoptosis and senescence via restoring autophagic flux. Osteoarthritis Cartilage 27(2):347–357. https://doi.org/10.1016/j.joca.2018.10.011
Wang WJ, Yang W, Ouyang ZH, Xue JB, Li XL, Zhang J, He WS, Chen WK, Yan YG, Wang C (2018) MiR-21 promotes ECM degradation through inhibiting autophagy via the PTEN/akt/mTOR signaling pathway in human degenerated NP cells. Biomed Pharmacother 99:725–734. https://doi.org/10.1016/j.biopha.2018.01.154
Kang L, Xiang Q, Zhan S, Song Y, Wang K, Zhao K, Li S, Shao Z, Yang C, Zhang Y (2019) Restoration of Autophagic Flux rescues oxidative damage and mitochondrial dysfunction to protect against intervertebral disc degeneration. Oxid Med Cell Longev 2019:7810320. https://doi.org/10.1155/2019/7810320
Poliseno L, Tuccoli A, Mariani L, Evangelista M, Citti L, Woods K, Mercatanti A, Hammond S, Rainaldi G (2006) MicroRNAs modulate the angiogenic properties of HUVECs. Blood 108(9):3068–3071. https://doi.org/10.1182/blood-2006-01-012369
Wang XH, Zhu L, Hong X, Wang YT, Wang F, Bao JP, Xie XH, Liu L, Wu XT (2016) Resveratrol attenuated TNF-alpha-induced MMP-3 expression in human nucleus pulposus cells by activating autophagy via AMPK/SIRT1 signaling pathway. Exp Biol Med (Maywood) 241(8):848–853. https://doi.org/10.1177/1535370216637940
Zamboni F, Ren G, Culebras M, O’Driscoll J, O’Dwyer J, Ryan EJ, Collins MN (2022) Curcumin encapsulated polylactic acid nanoparticles embedded in alginate/gelatin bioinks for in situ immunoregulation: characterization and biological assessment. Int J Biol Macromol 221:1218–1227. https://doi.org/10.1016/j.ijbiomac.2022.09.014
Wang Y, Che M, Xin J, Zheng Z, Li J, Zhang S (2020) The role of IL-1beta and TNF-alpha in intervertebral disc degeneration. Biomed Pharmacother 131:110660. https://doi.org/10.1016/j.biopha.2020.110660
Gruber HE, Hoelscher GL, Ingram JA, Norton HJ, Hanley EN Jr (2013) Increased IL-17 expression in degenerated human discs and increased production in cultured annulus cells exposed to IL-1ss and TNF-alpha. Biotech Histochem 88(6):302–310. https://doi.org/10.3109/10520295.2013.783235
Chuah YJ, Peck Y, Lau JE, Hee HT, Wang DA (2017) Hydrogel based cartilaginous tissue regeneration: recent insights and technologies. Biomater Sci 5(4):613–631. https://doi.org/10.1039/c6bm00863a
Han X, Leng X, Zhao M, Wu M, Chen A, Hong G, Sun P (2017) Resveratrol increases nucleus pulposus matrix synthesis through activating the PI3K/Akt signaling pathway under mechanical compression in a disc organ culture. Biosci Rep. https://doi.org/10.1042/BSR20171319
Bowles RD, Setton LA (2017) Biomaterials for intervertebral disc regeneration and repair. Biomaterials 129:54–67. https://doi.org/10.1016/j.biomaterials.2017.03.013
Xu H, Sun M, Wang C, Xia K, Xiao S, Wang Y, Ying L, Yu C, Yang Q, He Y et al (2020) Growth differentiation factor-5-gelatin methacryloyl injectable microspheres laden with adipose-derived stem cells for repair of disc degeneration. Biofabrication 13(1):015010. https://doi.org/10.1088/1758-5090/abc4d3
Borrelli C, Buckley CT (2020) Injectable disc-derived ECM hydrogel functionalised with chondroitin sulfate for intervertebral disc regeneration. Acta Biomater 117:142–155. https://doi.org/10.1016/j.actbio.2020.10.002
Panebianco CJ, Meyers JH, Gansau J, Hom WW, Iatridis JC (2020) Balancing biological and biomechanical performance in intervertebral disc repair: a systematic review of injectable cell delivery biomaterials. Eur Cell Mater 40:239–258. https://doi.org/10.22203/eCM.v040a15
Feng G, Zhang Z, Dang M, Rambhia KJ, Ma PX (2020) Nanofibrous spongy microspheres to deliver rabbit mesenchymal stem cells and anti-miR-199a to regenerate nucleus pulposus and prevent calcification. Biomaterials 256:120213. https://doi.org/10.1016/j.biomaterials.2020.120213
Prudnikova K, Lightfoot Vidal SE, Sarkar S, Yu T, Yucha RW, Ganesh N, Penn LS, Han L, Schauer CL, Vresilovic EJ et al (2018) Aggrecan-like biomimetic proteoglycans (BPGs) composed of natural chondroitin sulfate bristles grafted onto a poly(acrylic acid) core for molecular engineering of the extracellular matrix. Acta Biomater 75:93–104. https://doi.org/10.1016/j.actbio.2018.05.013
Choi UY, Joshi HP, Payne S, Kim KT, Kyung JW, Choi H, Cooke MJ, Kwon SY, Roh EJ, Sohn S et al (2020) An injectable hyaluronan-methylcellulose (HAMC) hydrogel combined with Wharton’s Jelly-derived mesenchymal stromal cells (WJ-MSCs) promotes degenerative disc repair. Int J Mol Sci. https://doi.org/10.3390/ijms21197391
Zhou X, Luo Z, Baidya A, Kim HJ, Wang C, Jiang X, Qu M, Zhu J, Ren L, Vajhadin F et al (2020) Biodegradable beta-cyclodextrin conjugated gelatin methacryloyl microneedle for delivery of water-insoluble drug. Adv Healthc Mater 9(11):e2000527. https://doi.org/10.1002/adhm.202000527
Daly AC, Riley L, Segura T, Burdick JA (2020) Hydrogel microparticles for biomedical applications. Nat Rev Mater 5(1):20–43. https://doi.org/10.1038/s41578-019-0148-6
Kurian AG, Singh RK, Patel KD, Lee JH, Kim HW (2022) Multifunctional GelMA platforms with nanomaterials for advanced tissue therapeutics. Bioact Mater 8:267–295. https://doi.org/10.1016/j.bioactmat.2021.06.027
Wu H, Shang Y, Sun W, Ouyang X, Zhou W, Lu J, Yang S, Wei W, Yao X, Wang X et al (2023) Seamless and early gap healing of osteochondral defects by autologous mosaicplasty combined with bioactive supramolecular nanofiber-enabled gelatin methacryloyl (BSN-GelMA) hydrogel. Bioact Mater 19:88–102. https://doi.org/10.1016/j.bioactmat.2022.03.038
Zhu B, Wang D, Pan H, Gong T, Ren Q, Wang Z, Guo Y (2023) Three-in-one customized bioink for islet organoid: GelMA/ECM/PRP orchestrate pro-angiogenic and immunoregulatory function. Colloids Surf B Biointerfaces 221:113017. https://doi.org/10.1016/j.colsurfb.2022.113017
Gupta SC, Patchva S, Koh W, Aggarwal BB (2012) Discovery of curcumin, a component of golden spice, and its miraculous biological activities. Clin Exp Pharmacol Physiol 39(3):283–299. https://doi.org/10.1111/j.1440-1681.2011.05648.x
Global Burden of Disease Study C (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet 386(9995):743–800. https://doi.org/10.1016/S0140-6736(15)60692-4
Xu YC, Gu Y, Cai F, Xi K, Xin TW, Tang JC, Wu L, Wang Z, Wang F, Deng LF et al (2020) Metabolism balance regulation via antagonist‐functionalized injectable microsphere for nucleus pulposus regeneration . Adv Funct Mater 30(52):2006333. https://doi.org/10.1002/adfm.202006333
Freemont AJ, Watkins A, Le Maitre C, Jeziorska M, Hoyland JA (2002) Current understanding of cellular and molecular events in intervertebral disc degeneration: implications for therapy. J Pathol 196(4):374–379. https://doi.org/10.1002/path.1050
Gupta T, Singh J, Kaur S, Sandhu S, Singh G, Kaur IP (2020) Enhancing Bioavailability and Stability of Curcumin using solid lipid nanoparticles (CLEN): a Covenant for its effectiveness. Front Bioeng Biotechnol 8:879. https://doi.org/10.3389/fbioe.2020.00879
Xiao L, Ding B, Gao J, Yang B, Wang J, Xu H (2020) Curcumin prevents tension-induced endplate cartilage degeneration by enhancing autophagy. Life Sci 258:118213. https://doi.org/10.1016/j.lfs.2020.118213
Ma T, Guo CJ, Zhao X, Wu L, Sun SX, Jin QH (2015) The effect of curcumin on NF-kappaB expression in rat with lumbar intervertebral disc degeneration. Eur Rev Med Pharmacol Sci 19(7):1305–1314
Gupta SC, Patchva S, Aggarwal BB (2013) Therapeutic roles of curcumin: lessons learned from clinical trials. AAPS J 15(1):195–218. https://doi.org/10.1208/s12248-012-9432-8
Umerska A, Gaucher C, Oyarzun-Ampuero F, Fries-Raeth I, Colin F, Villamizar-Sarmiento MG, Maincent P, Sapin-Minet A (2018) Polymeric nanoparticles for increasing oral bioavailability of curcumin. Antioxid (Basel). https://doi.org/10.3390/antiox7040046
Fu YS, Chen TH, Weng L, Huang L, Lai D, Weng CF (2021) Pharmacological properties and underlying mechanisms of curcumin and prospects in medicinal potential. Biomed Pharmacother 141:111888. https://doi.org/10.1016/j.biopha.2021.111888
Lopresti AL (2018) The problem of curcumin and its bioavailability: could its gastrointestinal influence contribute to its overall health-enhancing effects? Adv Nutr 9(1):41–50. https://doi.org/10.1093/advances/nmx011
Mancarella S, Greco V, Baldassarre F, Vergara D, Maffia M, Leporatti S (2015) Polymer-coated magnetic nanoparticles for curcumin delivery to cancer cells. Macromol Biosci 15(10):1365–1374. https://doi.org/10.1002/mabi.201500142
Moussa Z, Chebl M, Patra D (2017) Interaction of curcumin with 1,2-dioctadecanoyl-sn-glycero-3-phosphocholine liposomes: Intercalation of rhamnolipids enhances membrane fluidity, permeability and stability of drug molecule. Colloids Surf B Biointerfaces 149:30–37. https://doi.org/10.1016/j.colsurfb.2016.10.002
Vecchione R, Quagliariello V, Calabria D, Calcagno V, De Luca E, Iaffaioli RV, Netti PA (2016) Curcumin bioavailability from oil in water nano-emulsions: in vitro and in vivo study on the dimensional, compositional and interactional dependence. J Control Release 233:88–100. https://doi.org/10.1016/j.jconrel.2016.05.004
Tan B, Wu Y, Wu Y, Shi K, Han R, Li Y, Qian Z, Liao J (2021) Curcumin-microsphere/IR820 hybrid bifunctional hydrogels for in situ osteosarcoma chemo-co-thermal therapy and bone reconstruction. ACS Appl Mater Interfaces 13(27):31542–31553. https://doi.org/10.1021/acsami.1c08775
Parhi P, Suklabaidya S, Kumar Sahoo S (2017) Enhanced anti-metastatic and anti-tumorigenic efficacy of berbamine loaded lipid nanoparticles in vivo. Sci Rep 7(1):5806. https://doi.org/10.1038/s41598-017-05296-y
Rahat I, Rizwanullah M, Gilani SJ, Bin-Jummah MN, Imam SS, Kala C, Asif M, Alshehri S, Sharma SK (2021) Thymoquinone loaded chitosan-Solid lipid nanoparticles: formulation optimization to oral bioavailability study. J Drug Deliv Sci Tec 64:102565. https://doi.org/10.1016/j.jddst.2021.102565
El-Say KM, Hosny KM (2018) Optimization of carvedilol solid lipid nanoparticles: an approach to control the release and enhance the oral bioavailability on rabbits. PLoS ONE 13(8):e0203405. https://doi.org/10.1371/journal.pone.0203405
Alam M, Zameer S, Najmi AK, Ahmad FJ, Imam SS, Akhtar M (2020) Thymoquinone loaded solid lipid nanoparticles demonstrated antidepressant-like activity in rats via indoleamine 2, 3- dioxygenase pathway. Drug Res (Stuttg) 70(5):206–213. https://doi.org/10.1055/a-1131-7793
Shivananjegowda MG, Hani U, Osmani RAM, Alamri AH, Ghazwani M, Alhamhoom Y, Rahamathulla M, Paranthaman S, Gowda DV, Siddiqua A (2023) Development and evaluation of solid lipid nanoparticles for the clearance of abeta in Alzheimer’s disease. Pharmaceutics. https://doi.org/10.3390/pharmaceutics15010221
Rahman MA, Ali A, Rahamathulla M, Salam S, Hani U, Wahab S, Warsi MH, Yusuf M, Ali A, Mittal V et al (2023) Fabrication of sustained release curcumin-loaded solid lipid nanoparticles (Cur-SLNs) as a potential drug delivery system for the treatment of lung cancer: optimization of formulation and in vitro biological evaluation. Polym (Basel). https://doi.org/10.3390/polym15030542
Mohamed JM, Alqahtani A, Ahmad F, Krishnaraju V, Kalpana K (2021) Pectin co-functionalized dual layered solid lipid nanoparticle made by soluble curcumin for the targeted potential treatment of colorectal cancer. Carbohydr Polym 252:117180. https://doi.org/10.1016/j.carbpol.2020.117180
Wang P, Zhang L, Peng H, Li Y, Xiong J, Xu Z (2013) The formulation and delivery of curcumin with solid lipid nanoparticles for the treatment of on non-small cell lung cancer both in vitro and in vivo. Mater Sci Eng C Mater Biol Appl 33(8):4802–4808. https://doi.org/10.1016/j.msec.2013.07.047
Zhou P, Yan B, Wei B, Fu L, Wang Y, Wang W, Zhang L, Mao Y (2023) Quercetin-solid lipid nanoparticle-embedded hyaluronic acid functionalized hydrogel for immunomodulation to promote bone reconstruction. Regen Biomater 10:rbad025. https://doi.org/10.1093/rb/rbad025
Zhang Y, Li Z, Wang Z, Yan B, Shi A, Xu J, Guan J, Zhang L, Zhou P, Mao Y (2022) Mechanically enhanced composite hydrogel scaffold for in situ bone repairs. Biomater Adv 134:112700. https://doi.org/10.1016/j.msec.2022.112700
Luo Z, Sun W, Fang J, Lee K, Li S, Gu Z, Dokmeci MR, Khademhosseini A (2019) Biodegradable gelatin methacryloyl microneedles for transdermal drug delivery. Adv Healthc Mater 8(3):e1801054. https://doi.org/10.1002/adhm.201801054
Liu Y, Zhao X, Zhao C, Zhang H, Zhao Y (2019) Responsive porous microcarriers with controllable oxygen delivery for wound healing. Small 15(21):e1901254. https://doi.org/10.1002/smll.201901254
Duan Y, Dhar A, Patel C, Khimani M, Neogi S, Sharma P, Siva Kumar N, Vekariya RL (2020) A brief review on solid lipid nanoparticles: part and parcel of contemporary drug delivery systems. RSC Adv 10(45):26777–26791. https://doi.org/10.1039/d0ra03491f
Kabir MT, Rahman MH, Akter R, Behl T, Kaushik D, Mittal V, Pandey P, Akhtar MF, Saleem A, Albadrani GM et al (2021) Potential role of curcumin and its nanoformulations to treat various types of cancers. Biomolecules. https://doi.org/10.3390/biom11030392
Ban C, Jo M, Park YH, Kim JH, Han JY, Lee KW, Kweon DH, Choi YJ (2020) Enhancing the oral bioavailability of curcumin using solid lipid nanoparticles. Food Chem 302:125328. https://doi.org/10.1016/j.foodchem.2019.125328
Bunjes H (2011) Structural properties of solid lipid based colloidal drug delivery systems. Curr Opin Colloid In 16(5):405–411. https://doi.org/10.1016/j.cocis.2011.06.007
Rivera-Espinoza Y, Muriel P (2009) Pharmacological actions of curcumin in liver diseases or damage. Liver Int 29(10):1457–1466. https://doi.org/10.1111/j.1478-3231.2009.02086.x
Saghatelyan T, Tananyan A, Janoyan N, Tadevosyan A, Petrosyan H, Hovhannisyan A, Hayrapetyan L, Arustamyan M, Arnhold J, Rotmann AR et al (2020) Efficacy and safety of curcumin in combination with paclitaxel in patients with advanced, metastatic breast cancer: a comparative, randomized, double-blind, placebo-controlled clinical trial. Phytomedicine 70:153218. https://doi.org/10.1016/j.phymed.2020.153218
Wang K, Zhang C, Bao J, Jia X, Liang Y, Wang X, Chen M, Su H, Li P, Wan JB et al (2016) Synergistic chemopreventive effects of curcumin and berberine on human breast cancer cells through induction of apoptosis and autophagic cell death. Sci Rep 6:26064. https://doi.org/10.1038/srep26064
Fadus MC, Lau C, Bikhchandani J, Lynch HT (2017) Curcumin: an age-old anti-inflammatory and anti-neoplastic agent. J Tradit Complement Med 7(3):339–346. https://doi.org/10.1016/j.jtcme.2016.08.002
Yurube T, Takada T, Suzuki T, Kakutani K, Maeno K, Doita M, Kurosaka M, Nishida K (2012) Rat tail static compression model mimics extracellular matrix metabolic imbalances of matrix metalloproteinases, aggrecanases, and tissue inhibitors of metalloproteinases in intervertebral disc degeneration. Arthritis Res Ther 14(2):R51. https://doi.org/10.1186/ar3764
Ellman MB, Kim JS, An HS, Kroin JS, Li X, Chen D, Yan D, Buechter DD, Nakayama K, Liu B et al (2012) The pathophysiologic role of the protein kinase cdelta pathway in the intervertebral discs of rabbits and mice: in vitro, ex vivo, and in vivo studies. Arthritis Rheum 64(6):1950–1959. https://doi.org/10.1002/art.34337
Zheng ZM, Chen AQ, He HC, Chen Y, Chen J, Albashari AA, Li JW, Yin JY, He ZL, Wang QQ et al (2019) pH and enzyme dual-responsive release of hydrogen sulfide for disc degeneration therapy. J Mater Chem B 7(4):611–618. https://doi.org/10.1039/c8tb02566e
Baeuerle PA, Henkel T (1994) Function and activation of NF-kappa B in the immune system. Annu Rev Immunol 12:141–179. https://doi.org/10.1146/annurev.iy.12.040194.001041
Acknowledgements
Open access funding provided by grants from the 512 Talents Development Project of Bengbu Medical College (by51202302), the Opening Project of Anhui Province Key Laboratory of Tissue Transplantation in Bengbu Medical College (AHTT2022A001), the Domestic Visiting and Training Program for Outstanding Young Backbone Teachers in High Schools (gxgnfx2022036), and the Scientific Research Foundation of Bengbu Medical College (2021bypd006).
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
YM: conceived and designed the study. YW and YX: performed the experiments and wrote the paper. LS: collected and analyzed the data.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All animal experiments were authorized by the Ethics Committee of the Medical Faculty of Bengbu Medical College (approval number: 2021272) and performed following the National Institute of Health (NIH, Bethesda, MD) guideline
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Xu, Y., Shang, L. et al. GelMA hydrogel scaffold containing curcumin-loaded solid lipid nanoparticles promotes the regeneration of degenerative discs. SN Appl. Sci. 5, 243 (2023). https://doi.org/10.1007/s42452-023-05467-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s42452-023-05467-9