Abstract
Septic shock is provoked by hyper-activation of the pro-inflammatory response after infection and the patient requires anti-inflammatory treatment. However, the immune system develops a compensatory mechanism where the resulting feedback leads to an anti-inflammatory response after the initial state, which is referred to as immunodeficiency. Therefore, the initial therapeutic treatment with anti-inflammatory intervention has failed for almost 20 years and it has been changed in the last 10 years based on modulation of the inflammatory response. Using in silico methods, it is possible to develop a new approach based on physiopathology for treating septic shock. According to our new mathematical model, we can consider the dysfunctional immune system in a patient with septic shock and modify two parameters at different times to determine a possible treatment, and bearing out the single nucleoid polymorphism (SNP) may predominate the further deterioration of sepsis. The result represents the initial anti-inflammatory treatment with interleukin-10 activation and an increased risk of mortality over time for the septic shock patient, excluding the early stages. However, a hypothetical treatment based on interleukin-10 inhibition can change the patient’s immune stage and provide a new therapy according to our results, and show that the frequency of pro-inflammatory related gene SNP can be the possibility of increase sepsis risk. In conclusion, our proposed in silico method can explore therapeutic strategies and predict their associated efficacy and important factors, with the ultimate objective of improving treatments to reduce mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Septic syndromes represent a major problem worldwide and account for thousands of deaths each year [1,2,3,4,5,6,7,8,9,10,11,12,13]. In particular, septic shock is characterized by multiple organ dysfunctions and hypotension, with a mortality rate of 30–40% [6,7,8,9,10,11,12,13,14]. Sepsis remains the main cause of mortality in intensive care units (ICUs) and no new therapies have improved the prognosis despite many clinical trials of adjunctive therapies [11,12,13,14,15]. In addition, septic shock patients are characterized by high heterogeneity, and the main reasons for the failure to improve the prognosis are probably the rapid and sometimes antagonistic modifications of inflammation and immunity during this process [12,13,14, 16, 17].
In the early stage of the disease, monocytes, macrophages and neutrophils activate the innate immune system, which correspond to increases in pro-inflammatory cytokines and chemokines, to help the fight against infection [11,12,13, 17, 18]. However, when extreme reactions occur, they can also lead to harmful failures of various organs [6, 8, 9, 11,12,13, 17,18,19,20]. This response is balanced by negative feedback leading to the release of anti-inflammatory mediators, which protect against extreme inflammation. In severe sepsis and septic shock, this activation can have defensive effects during the first few hours, but it may become deleterious if it persists over time by leading to drastic reductions in the usual immune system functions [6,7,8,9, 11,12,13, 18, 21,22,23,24]. This phenomenon is called sepsis-induced immunosuppression and it is illustrated by the difficulties fighting primary bacterial infections and the decreased resistance to secondary nosocomial infections in a prolonged hypo-immune state [6, 8, 9, 21,22,23,24].
Interestingly, if early and aggressive treatments (appropriate antibiotherapy, fluid resuscitation) are applied, the prognosis is improved in the first hours of shock and many patients now survive after this critical step [6, 14, 17, 18, 21,22,23,24,25,26]. However, a significant proportion of these patients enter an immunosuppressed stage and die after a delayed phase of the disease. According to recent estimates, this process accounts for 50% of septic shock patients and represents > 65% of the total mortalities [21,22,23,24, 27]. Thus, a key issue is providing targeted therapy at the appropriate time to patients because the same drug may be beneficial or deleterious depending on the time-course of the disease.
Numerical modeling has been applied to studies of the immune system and models may help to understand the relationships between various immune system components and the physiopathology of sepsis, thereby explaining phenomena that cannot be predicted intuitively [28, 29]. Models could also help a physician to analyze a disease and make an optimal decision regarding the patient’s treatment [29]. Furthermore, models can be used to simulate and test new therapeutic interventions. Thus, numerical modeling appears to be suitable for analyzing a complex syndrome such as septic shock. In the present study, we based our approach on the model developed by Calvano et al. [28], who considered an example of infection by a Gram-negative bacterium, where two complex behaviors observed in patients were stimulated: (1) the explosion of inflammatory phenomena following a sufficient level of stimulus, as seen in septic shock; and (2) the occurrence of endotoxin tolerance [30,31,32,33].
In order to consider the increasing importance of epigenetic regulation (including microRNA; miRNA) in sepsis [34,35,36,37,38], the objective of the present study was to improve the model proposed by Calvano et al. [28] by adding epigenetic regulatory loops. Moreover, we aimed to obtain further insights into the therapeutic options for modifying the pro-/anti-inflammatory balance by including a pharmacology modeling stratum. This enhanced model appears to exhibit more realistic behavior when simulating septic shock. We illustrated our aim by considering two opposing strategies (“interleukin [IL]-10-like” or “anti-IL-10-like”) at different time points in the disease time course, and we compared our results with those obtained in clinical trials and experimental data from animal models. Recently, different researcher groups find the minor frequency of gene SNP of different pro-inflammatory cytokines associated with increased sepsis risk [39,40,41,42,43]. By introduce the new parameter value in the model, we simulate the SNP phenomena in different gene regulation, and identify which have strong influence in the impact of sepsis.
2 Materials and methods
2.1 Numerical model
In the model proposed by Calvano et al. [28], the inflammatory response is activated when endotoxin (lipopolysaccharide; LPS) is recognized by the Toll-like receptor 4 (TLR4), which stimulates complex signaling cascades and activates transcriptional factors (e.g. nuclear factor kappa-B (NF-κB) and activator protein 1 (AP-1)) [17, 18, 20, 34, 44]. This amplified signal activates the transcription of inflammatory genes. In this cascade of events, there is a delay in the counter-regulation of the anti-inflammatory response, which is considered to be negative feedback that inhibits activation of the pro-inflammatory response. This mechanism protects the immune system and ultimately decreases the expression of genes used in cellular bio-energetic processes (Fig. 1). These transcriptional events can be captured using indirect response models, which are employed widely in pharmacodynamics and pharmacogenomics modeling [45, 46]. The indirect response model includes eight variables: LPS, R (LPS binding receptor TLR4), mRNA-R, LPSR (LPS-R complex), SI* (signaling pathway of TLR4 following its activation by LPS), P (pro-inflammatory response), A (anti-inflammatory response), and E (energy production) [28]. These numerical model parameters were estimated based on the expression levels
Calvano et al. [28]. Qualitative structure of the indirect response model. LPS binds to the receptor (R) and forms the complex (LPSR), which activates the signaling complex (SI*) and indirectly stimulates the production rate KinP of the pro-inflammatory (P) response. The pro-inflammatory response then indirectly stimulates the production rate of the energetic (E) response (KinE) and the production rate of the anti-inflammatory (A) response (KinA). The energetic response stimulates both pro-inflammation and anti-inflammation, while anti-inflammation serves as the immuno-regulatory component of the system by restoring intracellular homeostasis
Mathematical representation of an indirect response model of endotoxin-induced human inflammation
-
(a)
\(\frac{{\text{dLPS}}}{{\text{dt}}} = {\text{K}}_{{{{\rm lps}}1}} \times {\text{LPS}} \times \left( {1 - {\text{LPS}}} \right) - {\text{K}}_{{{{\rm lps}}2}} \times {\text{LPS}}\)
-
(b)
\(\frac{{\text{dR}}}{{\text{dt}}} = {\text{K}}_{{\rm syn}} \times {\text{mRNA}},{\text{R}} + {\text{K}}_{2} \times \left( {\text{LPSR}} \right) - {\text{K}}_{1} \times {\text{LPS}} \times {\text{R}} - {\text{K}}_{{\rm syn}} \times {\text{R}}\)
-
(c)
\(\frac{{{\text{dmRNA}},{\text{R}}}}{\text{dt}} = {\text{K}}_{{{\text{in}},{\text{mRNA}},{\text{R}}}} \times \left( {1 + {\text{H}}_{{\rm mSI}} } \right) - {\text{K}}_{{{\text{out}},{\text{mRNA}},{\text{R}}}} \times {\text{mRNA}},{\text{R}}\)
-
(d)
\(\frac{{{\text{d}}\left( {\text{LPSR}} \right)}}{\text{dt}} = {\text{K}}_{1} \times {\text{LPS}} \times {\text{R}} - {\text{K}}_{3} \times \left( {\text{LPSR}} \right) - {\text{K}}_{2} \times \left( {\text{LPSR}} \right)\)
-
(e)
\(\frac{{{\text{d}}\left[ {{\text{SI}}^{ *} } \right]}}{\text{dt}} = {\text{K}}_{3} \times \frac{{\text{LPSR}}}{{\text{A}}} + {\text{K}}_{{\rm c}} \times \left( {\frac{{\left[ {{\text{SI}}^{ *} } \right]^{5} }}{{1 + \left[ {{\text{SI}}^{ *} } \right]^{5} }}} \right) - {\text{K}}_{4} \times \left[ {{\text{SI}}^{ *} } \right]\)
-
(f)
\(\frac{{\text{dP}}}{{\text{dt}}} = \frac{{{\text{K}}_{{\rm inP}} }}{\text{A}} \times \left( {1 + {\text{H}}_{{\rm PSI}} } \right) \times \left( {1 + {\text{H}}_{{\rm PE}} } \right) - {\text{K}}_{{\rm outP}} \times {\text{P }}\)
-
(g)
\(\frac{{\text{dA}}}{{\text{dt}}} = {\text{K}}_{{\rm inA}} \times \left( {1 + {\text{H}}_{{\rm AP}} } \right) \times \left( {1 + {\text{H}}_{{\rm AE}} } \right) - {\text{K}}_{{\rm outA}} \times {\text{A}}\)
-
(h)
\(\frac{{\text{dE}}}{{\text{dt}}} = \frac{{{\text{K}}_{{\rm inE}} }}{\text{A}} \times \left( {1 + {\text{H}}_{{\rm EP}} } \right) - {\text{K}}_{{\rm outE}} \times {\text{E}}\)
-
(i)
\({\text{H}}_{{\rm mSI}} = {\text{K}}_{{\rm mSI}} \times {\text{SI}}^{ *}\)
-
(j)
\({\text{H}}_{{\rm PSI}} = {\text{K}}_{{\rm PSI}} \times {\text{SI}}^{ *}\)
-
(k)
\({\text{H}}_{{\rm PE}} = {\text{K}}_{{\rm PE}} \times {\text{E}}\)
-
(l)
\({\text{H}}_{{\rm AP}} = {\text{K}}_{{\rm AP}} \times {\text{A}}\)
-
(m)
\({\text{H}}_{{\rm AE}} = {\text{K}}_{{\rm AE}} \times {\text{E}}\)
-
(n)
\({\text{H}}_{{\rm EP}} = {\text{K}}_{{\rm EP}} \times {\text{P}}\)
of leukocyte genes in the blood of eight human subjects at 0 (before endotoxin infusion), 2, 4, 6, 9 and 24 h after receiving an intravenous injection of either endotoxin at a dose of 2 ng/kg body weight or 0.9% sodium chloride (placebo treated subjects) [47] (Table 1). The fifth variable represents SI*, which activates the immune system. This equation includes a positive feedback loop responsible for maintaining self-activation and provoking the irreversible hyper-activation response regardless of the stimulus level. The inflammatory response exhibits hyper-activation when the concentration of LPS exceeds a critical threshold (LPS = 4), because the host responds to the endotoxin rather than the stimulus itself. These responses progress toward a systemic inflammatory response, which fails to improve as if the immune regulation system has been perturbed.
The model was then modified under the hypothesis that another regulatory level is involved with the degradation of the pro- and anti-inflammatory responses according to the two equations for A and P, which should be considered. SI* acts as the regulatory center, which activates the production of P. P corresponds to the early upregulation response of the immune system function and it induces negative feedback via the production of A, which inhibits the immune system function. These mechanisms can be characterized by the three balances represented in Fig. 2a for P regulation, A regulation, and equilibration of these two processes.
Mechanism of the model representing the interactions between the three variables: SI*, P, and A. a Red and blue arrows represent activation and inhibition, respectively. There are three balances: Kin–Kout (P), Kin–Kout (A) and A–P. b The dotted arrow represent the new regulatory unknown introduced in the two parts of Kout
In general, gene expression involves two states: the dynamic gene transcription state produces pre-mRNA, where a transcription factor can activate or inhibit the transcription level; and the post-transcriptional state comprises splicing, translation, translocation, etc., which modify the pre-mRNA to yield mature mRNA. The equations for P and A (f, g) describe the dynamics of gene transcription, which are controlled by the transcription rate and decay rate, where these are represented by KinA and KoutA for anti-inflammation, respectively (KinP and KoutP for pro-inflammation, respectively). These two equations represent how indirect regulation stimulates the transcription rate. However, we assume that the post-transcription state controls the decay rate. We also assume that miRNA comprise an important post-transcriptional regulatory mechanism for gene expression in many cellular processes, including the immune response, as well as playing a crucial role in the endotoxin tolerance system [34,35,36,37,38, 48,49,50]. For example, when miR146, miR155 and miR125b are stimulated by LPS in human monocytic cells [51,52,53], they can inhibit TLR4/IL-1R signaling via the post-transcriptional regulation of signaling proteins such as IL-1 receptor-associated kinase 1 (IRAK-1) and TNF receptor-associated factor 6 (TRAF6) [49, 53]. Thus, miRNA may act by inhibiting the SI* and P responses in the post-transcriptional state [30, 50, 53, 54]. However, the miRNA (miR98) can control the production of IL-10 in the post-transcriptional state [55, 56].
In addition, Cytochrome P450s (CYPs) are superfamily proteins including a variety of enzymes and can convert the proinflammatory 20-hydroxyeicosatetraenoic acid (20-HETE) and anti-inflammatory epoxyeicosatrienoic acids (EETs) [57]. The CYP450 gene can motive during the inflammation progression and lead to the activation, suppression and resolution of the inflammation [57,58,59]. In general, CYP gene expression is reduced by high concentration of pro-inflammatory cytokine, such as IL-6, TNF-α and interferon-β [57, 60,61,62,63]. CYP450 can play an important role in maintaining the correction of pro/anti-inflammatroy balance [57,58,59]. Finally, we consider that miRNAs as components of P and A can regulate P and A in the post-transcription state, and CYP450 may activate or inhibit the P and A to form the cycle regulation.
In order to introduce this new regulatory level, we suggest that at the levels of KoutA and KoutP, this new regulatory loop can be activated by the opposing factor but in two different directions, where the production level of A will stimulate the post-transcriptional degradation of P, whereas the production of P will inhibit the post-transcriptional degradation of A. This can be viewed as changing the fundamental point of the balance support (f1, g1; Fig. 2b).
-
(f)
\(\frac{dP}{dt} = \frac{{K_{inP} }}{A}*\left( {1 + H_{P.SI*} } \right)*\left( {1 + H_{P.E} } \right) - K_{outP} *P\)
-
(g)
\(\frac{dA}{dt} = K_{inA} *\left( {1 + H_{A.P} } \right)*\left( {1 + H_{A.E} } \right) - K_{outA} *A\)
-
(f1)
\(\frac{dP}{dt} = \frac{{K_{inP} }}{A}*\left( {1 + H_{P.SI*} } \right)*\left( {1 + H_{P.E} } \right) - K_{outP} *P*A\)
-
(g1)
\(\frac{dA}{dt} = K_{inA} *\left( {1 + H_{A.P} } \right)*\left( {1 + H_{A.E} } \right) - K_{outA} *\frac{A}{P}\)
2.2 Virtual treatment
In this study, we aimed to simulate immune system treatments for sepsis. We tested two possible logical treatments for sepsis shock: activating A by increasing the rate of production for the A response (by changing the A production rate parameter, where an increase in KinA, replicates activation by IL-10 treatment); or limiting A by increasing clearance of the A response (by changing the A decay rate parameter, where an increase in KoutA replicates an anti-IL-10 treatment). We simulated these two possibilities as virtual treatments, Thus, the activation of IL-10 and inhibition of IL-10 were tested using our in silico model and with the initial model proposed by Calvano et al. [28] at different times in the initial phase of septic shock, i.e., 0.2 h following the infectious stimulus, and in later phases at 30, 72 and 120 h after the infectious stimulus.
2.3 SNP simulation
We considered the SNP of gene could play the regulated role during the sepsis and may increase the expression of the TLR and pro-inflammation cytokines [39,40,41,42,43]. Through our new numeric model, we suppose the ratio of the parameter of Kin,mRNA,R for simulating the activation of SNP to TLR4 receptor during the LPS activation. However, the parameter Kc is control factor of SI to P for identification of the gene SNP which regulate the expression of pro-inflammatory cytokine. Thus, the modification of two parameter value was introduced in the new mathematic model and try different initial LPS value to test the SNP regulation consequence.
3 Results
3.1 In silico simulation of septic shock
When the infectious stimulus exceeded a critical threshold (LPS = 4), the system exhibited an irreversible hyper-stimulated status, which we considered similar to the loss of control seen during septic shock. At this time, the host immune system lost control of the ability to stabilize the system by self-hyper-activation of complex signaling, which can be viewed as an accurate representation of immunodysfunction.
When the same stimulus was applied with LPS = 4, the new model exhibited an irreversible response in terms of SI*, which was similar to the original. However, A became sufficiently strong to not return to a normal state following explosive deregulation. A had a higher value when LPS = 4 in the dysfunctional system compared with the maximum value when LPS = 1, 2, or 3. However P decreased to a lower value, which corresponded to the maximum value when LPS = 2. A reached a higher activity level compared with that of P, thereby leading to an imbalance in the immune system that favored the production of anti-inflammatory mediators, such as IL-10, and overall strong inhibition of the immune function (Fig. 3a). E was at lower level following explosive deregulation, which could have important health consequences. It is important to note that the immune system downregulated P and E, but upregulated A after stimulation with LPS. Monneret et al. [8] represented the immunoparalysis by initial system inflammatory response that is reduced by the anti-inflammatory process as the negative feedback during the sepsis. The clinical data showed that the anti-inflammatory response can dominate the septic patient for the long term [8, 21,22,23,24]. The new model simulated result showed that the anti-inflammatory response resists the high level, can compensated pro-inflammatory response which is hyper-active at the beginning stage after 24 h injection of LPS = 4 (Fig. 3a). In addition, when LPS = 4 the new model showed that energy response was at lower level which correspond the mitochondrial dysfunction and a consequence of a progressive decrease in energy availability during the septic process proposed by Singer et al. [64,65,66,67,68,69,70,71,72]. Finally, we considered the result is similar to the immunosuppression mechanism associated with septic shock.
Temporal responses of the critical inflammatory components to various initial conditions for the inflammatory stimulus. A high concentration of LPS could lead to a malfunction in terms of the dynamics of the host response to infection, which is represented by an exacerbated inflammatory response (red line). (A) New model: yellow solid line: LPS (0) = 1, green dashed line: LPS (0) = 2; blue dotted line: LPS (0) = 3; red dash-dotted line: LPS (0) = 4. (B) Initial model: yellow solid line: LPS (0) = 1, green dashed line: LPS (0) = 2; blue dotted line: LPS (0) = 3; red dash-dotted line: LPS (0) = 4
3.2 Comparison of the two models
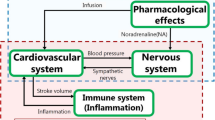
After the injection of LPS < 4 at t = 0 h, there was a large difference between the two models. The result obtained by the new model indicated an earlier response compared with the original model and the maximum value was low. The two models had the same critical threshold for the injection of LPS (= 4), which led to the hyper-activation of SI* and malfunction of the host immune system function. However, after the injection of LPS = 4 at t = 0 h, hyper-activation of P and A were exhibited by the original model, whereas our model indicated an imbalance that favored the hyper-activation of A (Fig. 3), and E was abnormal when the system lost control of intracellular signaling. By contrast, Calvano et al. [28] used the reciprocal energy response to determine the energy failure and negative regulation of the energetic process, but we consider that this result explains the metabolic flux event (Fig. 1). In the model, the energy response activates the entire system, and thus we consider it as an action due to energy consumption (or demand). The result obtained by the new model differed from those produced by the initial model after the modification, although the overall model was not changed, and we did not obtain exact measurements.
We compared the three terms for endotoxin tolerance in the two models where after a double stimulus, the new model had a second peak in the anti-inflammatory response corresponding to the second injection of LPS, which was not present in the initial model (data not show) [28]. In general, the immune system and cellular bio-energetic processes reacted faster than those in the initial model [28], which was also the case after the re-stimulation by LPS. Finally, the new model did not change the compartments in the initial model and can simulate mechanism of septic shock, so we can consider it as a version of the sepsis model.
3.3 Virtual treatments
The activation of A (as IL-10) as a treatment was applied during the initial stage at t = 0.2 h, which resulted in the reduced activation of P and the severity of sepsis in the earlier shock stage (Fig. 4). The application of this treatment at a later stage, e.g., 30, 72 and 120 h, also led to an increase in immunoparalysis, which increased A, but decreased P and E to lower values than those obtained without treatment (Fig. 4). In particular, the treatment at 0.2 h suppressed the irreversible SI* response and returned the immune system to a normal state (Fig. 4).
Virtual treatment to simulate the activation of anti-inflammation at four times: 0.2, 30, 72, and 120 h. Red solid line: LPS = 10, KinA = 0.256 (t = 0 h), KinA = 2.56 (t = 0.2 h). Blue dashed line: LPS = 10, KinA = 0.256 (t = 0 h), KinA = 2.56 (t = 30 h). Green dotted line: LPS = 10, KinA = 0.256 (t = 0 h), KinA = 2.56 (t = 72 h). Yellow dash-dotted line: LPS = 10, KinA = 0.256 (t = 0 h), KinA = 2.56 (t = 120 h). Black solid line: LPS = 10, KinA = 0.256 (t = 0 h)
The virtual treatment comprising the inhibition of A (as IL-10) at t = 0.2 h led to increases in P and the severity of sepsis (Fig. 5) during the earlier shock state. However, after continuing these treatments, P and E increased, whereas A remained unchanged (the result was the same at 30, 72, and 120 h) (Fig. 5) compared with the results of without treatment. Thus, the inhibition of A shifted the pro-inflammatory and anti-inflammatory balance toward the activation of P in the post shock state.
Virtual treatment to simulate the inhibition of anti-inflammation at four times: 0.2, 30, 72, and 120 h. Red solid line: LPS = 10, KoutA = 0.7 (t = 0 h), KoutA = 7 (t = 0.2 h). Blue dashed line: LPS = 10, KoutA = 0.7 (t = 0 h), KoutA = 7 (t = 30 h). Green dotted line: LPS = 10, KoutA = 0.7 (t = 0 h), KoutA = 7 (t = 72 h). Yellow dash-dotted line: LPS = 10, KoutA = 0.7 (t = 0 h), KoutA = 7 (t = 120 h). Black solid line: LPS = 10, KoutA = 0.7 (t = 0 h)
After introducing these virtual treatments into the initial model (data not shown), the activation of A at 0.2 h interrupted the formation of the irreversible SI* response and hyper-activated E. The results obtained after treatment in the later states (30, 72, and 120 h) showed that the activation of anti-inflammation could reduce the hyper-activation of P, activate E, and possibly balance the immune system. By contrast, the inhibition of A in the long term led to the hyper-activation of P and E decreased. Finally, the results obtained with the virtual treatments in the initial model showed that the activation of anti-inflammation is the best solution for re-establishing the immune system after hyper-stimulation by endotoxin.
3.4 SNP simulation
The parameter Kin,mRNA is considered the gene SNP frequency of the LPS receptor TLR4 regulation and Kc is as the gene SNP frequency of the pro-inflammatory cytokine. Therefore, we increase the value simulate fort sensibility of SNP with initial LPS value 1, 2, 3, 4 at t = 0 (Figs. 6, 7). Normal the model show the LPS = 4 can produce the sepsis shock phenomena, but when we changing the Kin,mRNA,R = 10 (minimal) via 0.2114 or Kc = 4 (minimal) via 3, at t = 0 LP = 3 might destroy the balance of immune system and increase the sepsis possible (Figs. 6, 7). So that the Kc increased 1.3 fold may cause the septic shock, in contrast Kin,mRNA,R need 46.7 fold change may cause the septic shock by the in silico simulation. We hypotheses that the gene SNP of the pro-inflammatory cytokine could play important role for the sepsis risk.
Gene SNP of TLR4 simulation by modifier the parameter Kin,mRNA,R at t = 0 with different initial LPS introduce value. A high concentration of LPS could lead to a malfunction in terms of the dynamics of the host response to infection, which is represented by an exacerbated inflammatory response (blue dotted and red dash-dotted line). Yellow solid line: LPS (0) = 1, green dashed line: LPS (0) = 2; blue dotted line: LPS (0) = 3; red dash-dotted line: LPS (0) = 4
Gene SNP of pro-inflammatory cytokine simulation by modifier Kc the parameter at t = 0 with different initial LPS introduce value. A high concentration of LPS could lead to a malfunction in terms of the dynamics of the host response to infection, which is represented by an exacerbated inflammatory response (blue dotted and red dash-dotted line). Yellow solid line: LPS (0) = 1, green dashed line: LPS (0) = 2; blue dotted line: LPS (0) = 3; red dash-dotted line: LPS (0) = 4
4 Discussion
The pathogenesis of sepsis is not clearly understood, but in the last few decades, new observations have suggested that the course of septic shock can be divided into two contrasting stages. In the early stage, the massive release of inflammatory mediators is responsible for organ dysfunctions and hypo-perfusion. In the late stage, the anti-inflammatory response persists and leads to immune paralysis. The capacity to treat patients during the early hours of shock has improved (early and intensive initial supportive therapy) and many patients now survive this critical stage, but they eventually die later in an immunosuppressed state due to difficulties fighting the primary bacterial infection and decreased resistance to secondary nosocomial infections [6, 8, 9, 11, 18, 21,22,23,24,25,26].
LPS is a component of the Gram-negative bacterial cell wall and its effects represents an appropriate model for studying endotoxin tolerance [32,33,34, 44, 73] as well the immuno-inflammatory response during infection [11,12,13, 17,18,19,20, 73,74,75]. In this model, the host inflammatory response is a consequence of multiple and complex cascades of mediators, where the endotoxin binds to a pattern recognition receptor, i.e., TLR4. The binding of endotoxin to this receptor activates signaling of the intracellular transcriptional factor NF-κB, which seems to play a central role [18,19,20, 76,77,78,79,80] in driving the immune response and changing the inflammatory state. This model comprises eight variables that are considered to play parts in the indirect response [45, 46] to simulate the effects of LPS.
In this study, we explored a simulation using a numerical model after modifying an initial model by introducing a novel regulatory mechanism. Figure 2 (Kin corresponds to the transcription rate and Kout corresponds to the post-transcription rate) shows the new regulatory mechanism added to Kout. This regulatory factor appeared to modify the fundamental point of the balance between the Kin and Kout, where the results of the simulation were closer to reality after its introduction. By injecting a high concentration of LPS (LPS ≥ 4) at t = 0, the host immune system was blocked by a strong positive feedback loop and P remained at a low level, whereas the value of A stayed at a high level, which differed from the maximum value when LPS < 4 at t = 0. Thus, we consider that A plays an important role in the sequence of dysfunctions in the immune system, where it inhibits the function of the immune system and provokes immunoparalysis. We also note that the energy response declined below the normal level during immunoparalysis and this poor energy response might impair the functions of organs. After applying a virtual treatment, the first injection of LPS = 10 may simulated the septic shock syndrome and immunoparalysis in the post-shock state. We conclude that treatment via the inhibition of A (as IL-10) produced better results in the post-shock state (at 30, 72 and 120 h) because it reactivated the immune system so P and E were at high levels. However, when we began the treatment in a premature shock stage at t = 0.2 h, P increased during the earlier stage of septic shock and the severity of sepsis increased. By contrast, treatment by activating A (as IL-10) at t = 0.2 h reduced the shock and removed the blockage of SI*. However, when we continued this treatment or began it at a later time (30, 72, and 120 h) the immune system entered more severe immunoparalysis. These results demonstrate that the application of different septic shock therapies will have diverse outcomes in each stage of the syndrome. The results obtained by the treatment according to the initial model showed that activation by anti-inflammatory therapeutics would be efficient at helping a patient to survive sepsis throughout the whole process. However, in septic patients, the immunosuppressed state cannot follow activation by the anti-inflammatory treatment, which can increase the severity of immunoparalysis. Finally, the new version of the model simulated the immunosuppressed state of sepsis patients better and allowed us to explore possible treatments.
Importantly, our results agree with the outcomes observed in clinics as well as in animal models where various approaches related to IL-10 have been tested [17, 24, 81,82,83,84,85,86,87,88]. Especially our activation of IL-10 result showed the increasing of anti-inflammatory response and inhibition of pro-inflammatory response cause aggravation of immunoparalysis as animal model testing result [89,90,91,92]. In addition, AS101 with capacity to inhibit the IL-10, have been shown the increasing survival and restore the pro-inflammatory cytokines: IFN-gamma, TNF-alpha and IL-1 beta in the septic animal model as demonstrated in our result of anti-IL-10 virtual treatment [86, 93]. Considering the schematic representation of the pro-/anti-inflammatory balance in the pathophysiology of sepsis, we suggest that if possible, a very early anti-inflammatory therapy would be helpful, whereas a pro-inflammatory strategy would be more appropriate in the delayed stage of this disease. We showed that IL-10 treatment had beneficial effects only when it was applied at 20 min, after which it had no effects or deleterious outcomes. This very narrow therapeutic window may explain the failure of many clinical assessments of various anti-inflammatory drugs [94]. Indeed, this window is already closed when most patients are admitted to ICUs. By contrast, the pro-inflammatory strategy appears to be beneficial after 30 h, as suggested recently by experts [27, 31, 95]. In addition to the convincing “IL-10/anti-IL-10” results, this model may facilitate further investigation of new therapeutic strategies.
The SNP simulation result showed that pro-inflammatory cytokine gene regulation can influence the immune system and increase the sepsis risk after infection [43]. However, the TLR4 gene regulation of SNP can be negligent. By our numeric model, we can analyze the different possibilities of gene SNP regulation, which may play an important role in the sepsis. In addition, the sensibility of the SNP may be depending on the patient condition, age, gender, etc. [41, 42]. Furthermore, for SNP regulation, new equation may be added to the mathematical model to better simulate the mechanism and better understand genetic regulation pathway in sepsis.
In conclusion, our improvements allowed the initial mathematical model to simulate sepsis. Our changes are based on new research results obtained in recent years. Sepsis may cause a series of physiological changes, particularly in terms of gene expression, including gene reprogramming and post-transcriptional regulation. However, we introduced the novel regulatory mechanism into the part responsible for the degradation of P and A. This type of regulation is a post-transcription mechanism and it establishes the balance of the immune system. Thus, this new model can reflect septic shock better. Finally, new therapies for immunoparalysis may be explored in two new areas based on cellular energy and signal transduction pathways, and a numerical model can be used to simulate these two areas in a more complex model in order to understand the function of inflammation .
References
Adrie C, Francais A, Alvarez-Gonzalez A, Mounier R, Azoulay E, Zahar JR, Clec’h C, Goldgran-Toledano D, Hammer L, Descorps-Declere A, Jamali S, Timsit JF, Outcomerea Study Group (2009) Model for predicting short term mortality of severe sepsis. Crit Care 13(3):R72
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D, Sepsis Occurrence in Acutely Ill Patients Investigators (2006) Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 34(2):344–353
Sprung CL, Sakr Y, Vincent JL, Le Gall JR, Reinhart K, Ranieri VM, Gerlach H, Fielden J, Groba CB, Payen D (2006) An evaluation of systemic inflammatory response syndrome signs in the Sepsis Occurrence in Acutely Ill Patients (SOAP) study. Intensive Care Med 32(3):421–427
Alberti C, Brun-Buisson C, Chevret S, Antonelli M, Goodman SV, Martin C, Moreno R, Ochagavia AR, Palazzo M, Werdan K, Le Gall JR, European Sepsis Study Group (2005) Systemic inflammatory response and progression to severe sepsis in critically ill infected patients. Am J Respir Crit Care Med 171(5):461–468
Vincent JL, Abraham E (2006) The last 100 years of sepsis. Am J Respir Crit Care Med 173(3):256–263
Hotchkiss RS, Karl IE (2003) The pathophysiology and treatment of sepsis. N Engl J Med 348(2):138–150
Remick DG (2007) Pathophysiology of sepsis. Am J Pathol 170(5):1435–1444
Monneret G, Venet F, Pachot A, Lepape A (2008) Monitoring immune dysfunctions in the septic patient: a new skin for the old ceremony. Mol Med 14(1–2):64–78
Venet F, Lepape A, Monneret G (2009) Monitoring immune dysfunction in septic patients: toward tailored immunotherapy. In: Vincent JL (ed) Yearbook of intensive care and emergency medicine. Springer, Berlin. https://doi.org/10.1007/978-3-540-92276-6_8. ISBN 978-3-540-92276-6
Kamisoglu K, Haimovich B, Calvano SE, Coyle SM, Corbett SA, Langley RJ, Kingsmore SF, Androulakis IP (2015) Human metabolic response to systemic inflammation: assessment of the concordance between experimental endotoxemia and clinical cases of sepsis/SIRS. Crit Care 3(19):71. https://doi.org/10.1186/s13054-015-0783-2
Keeley A, Hine P, Nsutebu E (2017) The recognition and management of sepsis and septic shock: a guide for non-intensivists. Postgrad Med J 93(1104):626–634. https://doi.org/10.1136/postgradmedj-2016-134519
Osborn TM (2017) Severe sepsis and septic shock trials (ProCESS, ARISE, ProMISe): what is optimal resuscitation? Crit Care Clin 33(2):323–344. https://doi.org/10.1016/j.ccc.2016.12.004
Makic MBF, Bridges E (2018) CE: managing sepsis and septic shock: current guidelines and definitions. Am J Nurs 118(2):34–39. https://doi.org/10.1097/01.NAJ.0000530223.33211.f5
Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, Angus DC, Rubenfeld GD, Singer M, Sepsis Definitions Task Force (2016) Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):775–787. https://doi.org/10.1001/jama.2016.0289
Dombrovskiy VY, Martin AA, Sunderram J, Paz HL (2007) Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med 35(5):1244–1250
Kellum JA, Kong L, Fink MP, Weissfeld LA, Yealy DM, Pinsky MR, Fine J, Krichevsky A, Delude RL, Angus DC, GenIMS Investigators (2007) Understanding the inflammatory cytokine response in pneumonia and sepsis: results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Arch Intern Med 167(15):1655–1663
Ludwig KR, Hummon AB (2017) Mass spectrometry for the discovery of biomarkers of sepsis. Mol BioSyst 13(4):648–664. https://doi.org/10.1039/c6mb00656f
Minasyan H (2017) Sepsis and septic shock: pathogenesis and treatment perspectives. J Crit Care 40:229–242. https://doi.org/10.1016/j.jcrc.2017.04.015
Rittirsch D, Flierl MA, Ward PA (2008) Harmful molecular mechanisms in sepsis. Nat Rev Immunol 8(10):776–787
Guha M, Mackman N (2001) LPS induction of gene expression in human monocytes. Cell Signal 13(2):85–94
Hamers L, Kox M, Pickkers P (2015) Sepsis-induced immunoparalysis: mechanisms, markers, and treatment options. Minerva Anestesiol 81(4):426–439
Stolk RF, van der Poll T, Angus DC, van der Hoeven JG, Pickkers P, Kox M (2016) Potentially inadvertent immunomodulation: norepinephrine use in sepsis. Am J Respir Crit Care Med 194(5):550–558. https://doi.org/10.1164/rccm.201604-0862CP
Arens C, Bajwa SA, Koch C, Siegler BH, Schneck E, Hecker A, Weiterer S, Lichtenstern C, Weigand MA, Uhle F (2016) Sepsis-induced long-term immune paralysis—results of a descriptive, explorative study. Crit Care 29(20):93. https://doi.org/10.1186/s13054-016-1233-5
Papadopoulos P, Pistiki A, Theodorakopoulou M, Christodoulopoulou T, Damoraki G, Goukos D, Briassouli E, Dimopoulou I, Armaganidis A, Nanas S, Briassoulis G, Tsiodras S (2017) Immunoparalysis: clinical and immunological associations in SIRS and severe sepsis patients. Cytokine 92:83–92. https://doi.org/10.1016/j.cyto.2017.01.012
Nguyen HB, Jaehne AK, Jayaprakash N, Semler MW, Hegab S, Yataco AC, Tatem G, Salem D, Moore S, Boka K, Gill JK, Gardner-Gray J, Pflaum J, Domecq JP, Hurst G, Belsky JB, Fowkes R, Elkin RB, Simpson SQ, Falk JL, Singer DJ, Rivers EP (2016) Early goal-directed therapy in severe sepsis and septic shock: insights and comparisons to ProCESS, ProMISe, and ARISE. Crit Care 20(1):160. https://doi.org/10.1186/s13054-016-1288-
Chen X, Zhu W, Tan J, Nie H, Liu L, Yan D, Zhou X, Sun X (2017) Early outcome of early-goal directed therapy for patients with sepsis or septic shock: a systematic review and meta-analysis of randomized controlled trials. Oncotarget 8(16):27510–27519. https://doi.org/10.18632/oncotarget.15550
Venet F, Lukaszewicz AC, Payen D et al (2013) Monitoring the immune response in sepsis: a rational approach to administration of immunoadjuvant therapies. Curr Opin Immunol 25(4):477–483
Foteinou PT, Calvano SE, Lowry SF, Androulakis IP (2009) Modeling endotoxin-induced systemic inflammation using an indirect response approach. Math Biosci 217(1):27–42
Namas RA, Vodovotz Y (2016) From static to dynamic: a sepsis-specific dynamic model from clinical criteria in polytrauma patients. Ann Transl Med 4(24):492
Biswas SK, Lopez-Collazo E (2009) Endotoxin tolerance: new mechanisms, molecules and clinical significance. Trends Immunol 30(10):475–487. https://doi.org/10.1016/j.it.2009.07.009
Hotchkiss RS, Monneret G, Payen D (2013) Immunosuppression in sepsis: a novel understanding of the disorder and a new therapeutic approach. Lancet Infect Dis 13(3):260–268
Wiśnik E, Pikus E, Duchnowicz P, Koter-Michalak M (2017) Tolerance of monocytes and macrophages in response to bacterial endotoxin. Postepy Hig Med Doswiadczalnej (Online) 71:176–185
Huber R, Bikker R, Welz B, Christmann M, Brand K (2017) TNF tolerance in monocytes and macrophages: characteristics and molecular mechanisms. J Immunol Res 2017:9570129. https://doi.org/10.1155/2017/9570129
Biswas SK, Shalova IN (2012) Endotoxin tolerance as a key mechanism for immunosuppression. In: Kapur S (ed) Immunosuppression—role in health and diseases. InTech, Rijeka. ISBN 978-953-51-0152-9
Funahashi Y, Kato N, Masuda T, Nishio F, Kitai H, Ishimoto T, Kosugi T, Tsuboi N, Matsuda N, Maruyama S, Kadomatsu K (2019) miR-146a targeted to splenic macrophages prevents sepsis-induced multiple organ injury. Lab Investig. https://doi.org/10.1038/s41374-019-0190-4
Dai Y, Jia P, Fang Y, Liu H, Jiao X, He JC, Ding X (2016) miR-146a is essential for lipopolysaccharide (LPS)-induced cross-tolerance against kidney ischemia/reperfusion injury in mice. Sci Rep 2(6):27091. https://doi.org/10.1038/srep27091
Hu Q, Gong W, Gu J, Geng G, Li T, Tian R, Yang Z, Zhang H, Shao L, Liu T, Wan L, Jia J, Yang C, Shi Y, Shi H (2019) Plasma microRNA profiles as a potential biomarker in differentiating adult-onset still’s disease from sepsis. Front Immunol 11(9):3099. https://doi.org/10.3389/fimmu.2018.03099
Ma H, Wang X, Ha T, Gao M, Liu L, Wang R, Yu K, Kalbfleisch JH, Kao RL, Williams DL, Li C (2016) MicroRNA-125b prevents cardiac dysfunction in polymicro bial sepsis by targeting TRAF6-mediated nuclear factor κB activation and p53-mediated apoptotic signaling. J Infect Dis 214(11):1773–1783
Eslam M, McLeod D, Kelaeng KS, Mangia A, Berg T, Thabet K, Irving WL, Dore GJ, Sheridan D, Grønbæk H, Abate ML, Hartmann R, Bugianesi E, Spengler U, Rojas A, Booth DR, Weltman M, Mollison L, Cheng W, Riordan S, Mahajan H, Fischer J, Nattermann J, Douglas MW, Liddle C, Powell E, Romero-Gomez M, George J, International Liver Disease Genetics Consortium (ILDGC) (2017) IFN-λ3, not IFN-λ4, likely mediates IFNL3-IFNL4 haplotype-dependent hepatic inflammation and fibrosis. Nat Genet 49(5):795–800. https://doi.org/10.1038/ng.3836
Nielsen KR, Rodrigo-Domingo M, Steffensen R, Baech J, Bergkvist KS, Oosterhof L, Schmitz A, Bødker JS, Johansen P, Vogel U, Vangsted A, Dybkær K, Bøgsted M, Johnsen HE (2017) Interactions between SNPs affecting inflammatory response genes are associated with multiple myeloma disease risk and survival. Leuk Lymphoma 58(11):2695–2704. https://doi.org/10.1080/10428194.2017.1306643
Watanabe E, Buchman TG, Hirasawa H, Zehnbauer BA (2010) Association between lymphotoxin-alpha (tumor necrosis factor-beta) intron polymorphism and predisposition to severe sepsis is modified by gender and age. Crit Care Med 38(1):181–193. https://doi.org/10.1097/CCM.0b013e3181bc805d
Montoya-Ruiz C, Jaimes FA, Rugeles MT, López JÁ, Bedoya G, Velilla PA (2016) Variants in LTA, TNF, IL1B and IL10 genes associated with the clinical course of sepsis. Immunol Res 64(5–6):1168–1178
Giamarellosbourboulis EJ, Opal SM (2016) The role of genetics and antibodies in sepsis. Ann Transl Med 4(17):328
Cavaillon JM, Adib-Conquy M (2006) Bench-to-bedside review: endotoxin tolerance as a model of leukocyte reprogramming in sepsis. Crit Care 10(5):233
Krzyzanski W, Jusko WJ (1998) Integrated functions for four basic models of indirect pharmacodynamic response. J Pharm Sci 87(1):67–72
Sharma A, Ebling WF, Jusko WJ (1998) Precursor-dependent indirect pharmacodynamic response model for tolerance and rebound phenomena. J Pharm Sci 87(12):1577–1584
Calvano SE, Xiao W, Richards DR, Felciano RM, Baker HV, Cho RJ, Chen RO, Brownstein BH, Cobb JP, Tschoeke SK, Miller-Graziano C, Moldawer LL, Mindrinos MN, Davis RW, Tompkins RG, Lowry SF, Inflamm and Host Response to Injury Large Scale Collab. Res. Program (2005) A network-based analysis of systemic inflammation in humans. Nature 437(7061):1032–1037
Bartel DP (2009) MicroRNAs: target recognition and regulatory functions. Cell 136(2):215–233
Baltimore D, Boldin MP, O’Connell RM, Rao DS, Taganov KD (2008) MicroRNAs: new regulators of immune cell development and function. Nat Immunol 9(8):839–845
Prabowo AS, van Scheppingen J, Iyer AM, Anink JJ, Spliet WG, van Rijen PC, Schouten-van Meeteren AY, Aronica E (2015) Differential expression and clinical significance of three inflammation-related microRNAs in gangliogliomas. J Neuroinflamm 20(12):97. https://doi.org/10.1186/s12974-015-0315-7
O’Connell RM, Taganov KD, Boldin MP, Cheng G, Baltimore D (2007) MicroRNA-155 is induced during the macrophage inflammatory response. Proc Natl Acad Sci USA 104(5):1604–1609
Taganov KD, Boldin MP, Chang KJ, Baltimore D (2006) NF-kappaB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proc Natl Acad Sci USA 103(33):12481–12486
Tili E, Michaille JJ, Cimino A, Costinean S, Dumitru CD, Adair B, Fabbri M, Alder H, Liu CG, Calin GA, Croce CM (2007) Modulation of miR-155 and miR-125b levels following lipopolysaccharide/TNF-alpha stimulation and their possible roles in regulating the response to endotoxin shock. J Immunol 179(8):5082–5089
El Gazzar M, McCall CE (2010) MicroRNAs distinguish translational from transcriptional silencing during endotoxin tolerance. J Biol Chem 285(27):20940–20951
Liu Y, Chen Q, Song Y, Lai L, Wang J, Yu H, Cao X, Wang Q (2011) MicroRNA-98 negatively regulates IL-10 production and endotoxin tolerance in macrophages after LPS stimulation. FEBS Lett 585(12):1963–1968
Quinn EM, Wang J, Redmond HP (2012) The emerging role of microRNA in regulation of endotoxin tolerance. J Leukoc Biol 91(5):721–727. https://doi.org/10.1189/jlb.1111571
Spector AA, Kim HY (2015) Cytochrome P450 epoxygenase pathway of polyunsaturated fatty acid metabolism. Biochim Biophys Acta 1851(4):356–365
Christmas P (2015) Role of cytochrome P450s in inflammation. Adv Pharmacol 74:163–192
Gilroy DW, Edin ML, Maeyer RPHD et al (2016) CYP450-derived oxylipins mediate inflammatory resolution. Proc Natl Acad Sci USA 113(23):E3240
Christensen H, Hermann M (2012) Immunological response as a source to variability in drug metabolism and transport. Front Pharmacol 3:8
Harvey RD, Morgan ET (2014) Cancer, inflammation, and therapy: effects on cytochrome P450-mediated drug metabolism and implications for novel immunotherapeutic agents. Clin Pharmacol Ther 96(4):449–457
Morgan ET (2001) Regulation of cytochrome p450 by inflammatory mediators: why and how? Drug Metab Dispos 29:207–212
Sun HY, Yan YJ, Li YH et al (2018) Reversing effects of ginsenosides on LPS-induced hepatic CYP3A11/3A4 dysfunction through the pregnane X receptor. J Ethnopharmacol 229:246–255
Carré JE, Orban JC, Re L, Felsmann K, Iffert W, Bauer M, Suliman HB, Piantadosi CA, Mayhew TM, Breen P, Stotz M, Singer M (2010) Survival in critical illness is associated with early activation of mitochondrial biogenesis. Am J Respir Crit Care Med 182:745–751
Brealey D, Karyampudi S, Jacques TS, Novelli M, Stidwill R, Taylor V, Smolenski RT, Singer M (2004) Mitochondrial dysfunction in a long-term rodent model of sepsis and organ failure. Am J Physiol Regul Integr Comp Physiol 286(3):R491–R497
Singer M (2007) Mitochondrial function in sepsis: acute phase versus multiple organ failure. Crit Care Med 35(9 Suppl):S441–S448
Brealey DA, Singer M, Terblanche M (2011) Potential metabolic consequences of statins in sepsis. Crit Care Med 39(6):1514–1520
Brealey D, Brand M, Hargreaves I, Heales S, Land J, Smolenski R, Davies NA, Cooper CE, Singer M (2002) Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet 360(9328):219–223
Svistunenko DA, Davies N, Brealey D, Singer M, Cooper CE (2006) Mitochondrial dysfunction in patients with severe sepsis: an EPR interrogation of individual respiratory chain components. Biochim Biophys Acta 1757(4):262–272
Stanzani G, Duchen MR, Singer M (2019) The role of mitochondria in sepsis-induced cardiomyopathy. Biochim Biophys Acta Mol Basis Dis 1865(4):759–773. https://doi.org/10.1016/j.bbadis.2018.10.011
Arulkumaran N, Pollen S, Greco E, Courtneidge H, Hall AM, Duchen MR, Tam FWK, Unwin RJ, Singer M (2018) Renal tubular cell mitochondrial dysfunction occurs despite preserved renal oxygen delivery in experimental septic acute kidney injury. Crit Care Med 46(4):e318–e325. https://doi.org/10.1097/CCM.0000000000002937
Pinto BB, Dyson A, Umbrello M, Carré JE, Ritter C, Clatworthy I, Duchen MR, Singer M (2017) Improved survival in a long-term rat model of sepsis is associated with reduced mitochondrial calcium uptake despite increased energetic demand. Crit Care Med 45(8):e840–e848. https://doi.org/10.1097/CCM.0000000000002448
Biswas SK, Tergaonkar V (2007) Myeloid differentiation factor 88-independent Toll-like receptor pathway: sustaining inflammation or promoting tolerance? Int J Biochem Cell Biol 39(9):1582–1592
Fannin RD, Auman JT, Bruno ME, Sieber SO, Ward SM, Tucker CJ, Merrick BA, Paules RS (2005) Differential gene expression profiling in whole blood during acute systemic inflammation in lipopolysaccharide-treated rats. Physiol Genom 21(1):92–104
Talwar S, Munson PJ, Barb J, Fiuza C, Cintron AP, Logun C, Tropea M, Khan S, Reda D, Shelhamer JH, Danner RL, Suffredini AF (2006) Gene expression profiles of peripheral blood leukocytes after endotoxin challenge in humans. Physiol Genom 25:20315
Chen F, Bower J, Demers LM, Shi X (2001) Upstream signal transduction of NF-kB activation. Atlas Database. https://doi.org/10.4267/2042/37857
Müller JM, Ziegler-Heitbrock HWL, Baeuerle PA (1993) Nuclear factor kappa B, a mediator of lipopolysaccharide effects. Immunobiology 187:233–256
Medzhitov R, Janeway C Jr (2000) Innate immunity. N Engl J Med 343(5):338–344
Boudieu L, Mountadem S, Lashermes A, Meleine M, Ulmann L, Rassendren F, Aissouni Y, Sion B, Carvalho FA, Ardid D (2019) Blocking α(2)δ-1 subunit reduces bladder hypersensitivity and inflammation in a cystitis mouse model by decreasing NF-kB pathway activation. Front Pharmacol. 26(10):133. https://doi.org/10.3389/fphar.2019.00133
Lai JL, Liu YH, Liu C, Qi MP, Liu RN, Zhu XF, Zhou QG, Chen YY, Guo AZ, Hu CM (2017) Indirubin inhibits LPS-induced inflammation via TLR4 abrogation mediated by the NF-kB and MAPK signaling pathways. Inflammation 40(1):1–12. https://doi.org/10.1007/s10753-016-0447-7
Howard M, Muchamuel T, Andrade S, Menon S (1993) Interleukin 10 protects mice from lethal endotoxemia. J Exp Med 177(4):1205–1208
van der Poll T, Marchant A, Buurman WA, Berman L, Keogh CV, Lazarus DD, Nguyen L, Goldman M, Moldawer LL, Lowry SF (1995) Endogenous IL-10 protects mice from death during septic peritonitis. J Immunol 155(11):5397–5401
Kelly JL, Lyons A, Soberg CC, Mannick JA, Lederer JA (1997) Anti-interleukin-10 antibody restores burn-induced defects in T-cell function. Surgery 122(2):146–152
Nicoletti F, Mancuso G, Ciliberti FA, Beninati C, Carbone M, Franco S, Cusumano V (1997) Endotoxin-induced lethality in neonatal mice is counteracted by interleukin-10 (IL-10) and exacerbated by anti-IL-10. Clin Diagn Lab Immunol 4(5):607–610
Lyons A, Goebel A, Mannick JA, Lederer JA (1999) Protective effects of early interleukin 10 antagonism on injury-induced immune dysfunction. Arch Surg 134(12):1317–1323
Kalechman Y, Gafter U, Gal R, Rushkin G, Yan D, Albeck M, Sredni B (2002) Anti-IL-10 therapeutic strategy using the immunomodulator AS101 in protecting mice from sepsis-induced death: dependence on timing of immunomodulating intervention. J Immunol 169(1):384–392
Chen X, Xu W, Wang Y, Luo H, Quan S, Zhou J, Yang N, Zhang T, Wu L, Liu J, Long X, Zhu N, Xie H, Luo Z (2014) Hydrogen sulfide reduces kidney injury due to urinary-derived sepsis by inhibiting NF-κB expression, decreasing TNF-α levels and increasing IL-10 levels. Exp Ther Med 8(2):464–470
Claser C, De Souza JB, Thorburn SG, Grau GE, Riley EM, Rénia L, Hafalla JCR (2017) Host resistance to plasmodium-induced acute immune pathology is regulated by interleukin-10 receptor signaling. Infect Immun. https://doi.org/10.1128/iai.00941-16
Kulkarni U, Herrmenau C, Win SJ, Bauer M, Kamradt T (2018) IL-7 treatment augments and prolongs sepsis-induced expansion of IL-10-producing B lymphocytes and myeloid-derived suppressor cells. PLoS ONE 13(2):e0192304. https://doi.org/10.1371/journal.pone.0192304
Bah I, Kumbhare A, Nguyen L, McCall CE, El Gazzar M (2018) IL-10 induces an immune repressor pathway in sepsis by promoting S100A9 nuclear localization and MDSC development. Cell Immunol 332:32–38. https://doi.org/10.1016/j.cellimm.2018.07.003
Andrade EB, Alves J, Madureira P, Oliveira L, Ribeiro A, Cordeiro-da-Silva A, Correia-Neves M, Trieu-Cuot P, Ferreira P (2013) TLR2-induced IL-10 production impairs neutrophil recruitment to infected tissues during neonatal bacterial sepsis. J Immunol 191(9):4759–4768. https://doi.org/10.4049/jimmunol.1301752
Chuang TY, Chang HT, Chung KP, Cheng HS, Liu CY, Liu YC, Huang HH, Chou TC, Chang BL, Lee MR, Lin CJ, Lee SW, Yu CJ, Hsueh PR (2014) High levels of serum macrophage migration inhibitory factor and interleukin 10 are associated with a rapidly fatal outcome in patients with severe sepsis. Int J Infect Dis 20:13–17. https://doi.org/10.1016/j.ijid.2013.12.006
Muenzer JT, Davis CG, Chang K, Schmidt RE, Dunne WM, Coopersmith CM, Hotchkiss RS (2010) Characterization and modulation of the immunosuppressive phase of sepsis. Infect Immun 78(4):1582–1592. https://doi.org/10.1128/iai.01213-09
Zeni F, Freeman B, Natanson C (1997) Anti-inflammatory therapies to treat sepsis and septic shock: a reassessment. Crit Care Med 25(7):1095–1100
Leentjens J, Kox M, Jg VDH et al (2013) Immunotherapy for the adjunctive treatment of sepsis: from immunosuppression to immunostimulation Time for a paradigm change? Am J Respir Crit Care Med 187(12):1287
Funding
This study was supported by Plan of Funding Outstanding Science and Technology Projects launched by Talents Returning from Studying Overseas in 2018 (Tianjin, China); DHOS-Inserm “Recherche Clinique Translationnelle 2009” (FR)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, G., Gueyffier, F., Monneret, G. et al. Mathematical modeling of septic shock: an innovative tool for assessing therapeutic hypotheses. SN Appl. Sci. 1, 717 (2019). https://doi.org/10.1007/s42452-019-0747-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s42452-019-0747-2