Abstract
The duration of cardiopulmonary resuscitation (CPR) affects neurological outcomes. Conclusive data on its decremental effect on neurological outcomes have not been explored before in a quantitative review. PubMed and Google Scholar were searched for relevant studies from 2015 up to May 2023 using relevant keywords. The odds of good neurological outcomes were studied. Binary random effects were used to estimate pooled odds ratios (OR) and 95% confidence intervals (CI). A leave-one-out sensitivity analysis was performed. Heterogeneity was assessed using I2 statistics. For outcomes showing moderate to high heterogeneity, subgroup analysis was performed for follow-up duration or type of study. A p value of < 0.05 was considered statistically significant. A total of 349,027 cardiac arrest patients (mean age, 70.2 years; males, 56.6%) from four studies were included in the meta-analysis. Of them, the initial rhythm was shockable in 11% (38,465/349,027) and non-shockable in 88.97% (310,562/349,027) of the population. Odds of having favorable neurological outcomes were 0.32 (95% CI 0.10–1.01, p = 0.05) for 6–10 min (n = 14,118), 0.10 (95% CI 0.02–0.64, p = 0.02) for 11–15 min (n = 43,885), 0.05 (95% CI 0.01–0.36, p 0.01) for 16–20 min (n = 66,174), 0.04 (95% CI 0.01–0.21, p < 0.01) for > 20 min (n = 181,262), and 0.03 (95% CI 0.00–1.55, p = 0.08) for > 30 min (n = 66,461) when compared to patients receiving CPR for < 5 min (n = 6420). Steady decremental odds of favorable neurological outcomes were seen with every 5 min of increased CPR duration, with a statistically significant decline seen in CPR duration from 11 to 15 min onwards.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post-cardiac arrest brain injury (PCABI) is the main cause of death in patients resuscitated from cardiac arrest and the main cause of long-term disability in those who survive the acute phase [1]. As medical advancements and swift interventions have led to more patients surviving cardiac arrest, it becomes imperative to shift our focus towards improving the neurological outcomes and overall quality of life for these survivors. Effective strategies to minimize brain injury after resuscitation include early intervention with cardiopulmonary resuscitation and defibrillation, restoration of normal physiology, and targeted temperature management [2].
While there have been many new developments in resuscitation protocols and post cardiac arrest care in recent years, still the chance of survival with good neurological outcome in an out-of-hospital cardiac arrest (OHCA) is dismally low at 8% [3]. Approximately one in three patients admitted to intensive care will survive, many of whom will need intensive, tailored rehabilitation after discharge to have the best outcomes [4]. Given this data and alarming survival rates, it is imperative to analyze the factors that affect neurological prognostication in post cardiac arrest survivors to enable healthcare personnel educate families to make informed treatment decisions. Identifying people who might have a poor outcome is essential to enabling informed choices about the continuation or withdrawal of life-sustaining treatments.
Studies have shown that age, etiology of arrest, preexisting comorbid conditions, response time, duration of cardiopulmonary resuscitation (CPR), and quality of CPR do play important roles in determining the outcome after cardiac arrest [5]. While neurological outcome post cardiac arrest is dependent on many factors, there is still paucity of data regarding the role duration of resuscitation plays in neurological outcomes of post cardiac arrest survivors. The objective of this review and meta-analysis is to investigate whether CPR duration influences neurological outcomes in cardiac arrest patients. The findings from this study will provide healthcare providers with evidence-based guidance, on determining CPR duration ultimately aiming to enhance outcomes and improve patient survival.
Methods
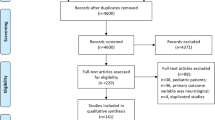
We performed an extensive search across prominent electronic databases, such as PubMed and Google Scholar, encompassing studies on neurological outcomes post cardiac arrest patients from 2015 until May 2023. Additionally, we manually searched through reference lists of pertinent articles and conference abstracts. The search strategy was formulated with the following selected keywords: “Anoxic Brain injury” or “Anoxic Encephalopathy”, “neurological outcome” and “prospective”, “longitudinal”, “Cardiac Arrest”. We presented a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram mentioning the study selection process and the inclusion and exclusion counts at each phase of our meta-analysis (Fig. 1).
To ensure rigorous study selection, two independent reviewers evaluated the titles and abstracts of relevant studies. Any discrepancies between the two reviewers were resolved through discussion and consensus. We included studies that reported neurological outcomes in patients with cardiac arrest who received CPR at various intervals, which were published in English, and excluded studies that were not original research articles (e.g., reviews, letters, editorials), did not report on neurological outcomes, and did not report on durations of CPR. Two independent reviewers conducted data extraction and encompassed study characteristics (e.g., author, publication year, study design, sample size), patient characteristics (e.g., age, gender, comorbidities), intervention characteristics (e.g., CPR duration, rhythm type—shockable or non-shockable), and data on outcome (e.g., neurological outcome type, odds ratio, and confidence intervals).
The Newcastle Ottawa scale was used for quality appraisal of the included studies, specifically observational and cohort studies (Table 1). We conducted the meta-analysis of the included studies using a random-effects model. Binary random effects were used to estimate pooled odds ratios (OR) and 95% confidence intervals (CI). Furthermore, leave-one-out sensitivity analysis was performed and I2 statistics were used to assess for heterogeneity of the included studies. We conducted subgroup analyses based on follow-up duration or study type in the outcomes demonstrating substantial heterogeneity. We used OpenMetaAnalyst and Microsoft Excel for all data extraction and statistical analyses and p < 0.05 was statistically significant.
Results
A total of 4 studies were included in our meta-analysis [6,7,8,9]. Of them, we had 2 retrospective and 2 prospective cohort studies (1 from the United States, 1 from Europe, and 2 from Japan). In total, 349,027 cardiac arrest patients were included in this study. The mean age of study population was 70.2 years and majority of them were males (56.5%). In the studied population, around 283,642 cardiac arrests (81.2%) were out-of-hospital cardiac arrests, and around 190,082 (54.4%) arrests were at private homes or residential locations. Median emergency personnel response time was 7 min. Witnessed arrests or bystander CPR was noted in 156,983 (44.9%) patients. Of total events, 89% were non-shockable rhythms whereas 11% were shockable rhythms. The baseline characteristics of the included study population are described in Table 2.
Odds of having favorable neurological outcomes were OR 0.32 (95% CI 0.10–1.01, p = 0.05) for 6–10 min (n = 14,118), OR 0.10 (95% CI 0.02–0.64, p = 0.02) for 11–15 min (n = 43,885), OR 0.05 (95% CI 0.01–0.36, p < 0.01) for 16–20 min (n = 66,174), OR 0.04 (95% CI 0.01–0.21, p < 0.01) for > 20 min (n = 181,262), and OR 0.03 (95% CI 0.00–1.55, p = 0.08) for > 30 min (n = 66,461) when compared to patients receiving CPR for < 5 min (n = 6420) (Fig. 2).
Discussion
The studies included in the meta-analysis have included the cerebral performance category (CPC) scale to quantify neurological recovery. Good neurological outcome was defined as CPC category 1 or 2, while poor neurological outcome was defined as a CPC score of 3–5. A CPC score of 1 corresponds to survival with no or minor neurological deficits and no impairment of everyday functioning. A CPC score of 2 indicates moderate cerebral disability, which affects professional life but leaves patients still capable of managing their everyday tasks on their own. A CPC score of 3 indicates severe cerebral disability and dependence on support from others for everyday living. Patients in a coma or vegetative state are given a CPC score of 4, while brain death is given a CPC score of 5 [10]. It has been theorized that brain cells may undergo cell death as early as 1 min into oxygen deprivation, leading to significant neurological damage at the 3-min mark. In theory, the longer the duration of oxygen deprivation, the more severe the irreversible neurological damage can ensue, potentially impacting the chances of recovery. Hence, the quality and duration of CPR play an important role in determining the outcomes [11].
Our study demonstrates that the duration of CPR directly correlates with neurological outcomes in patients with cardiac arrest. Based on our study, we see that the chances of having a good neurological recovery in patients who have achieved return of spontaneous circulation (ROSC) after 6 to 10 min of CPR are 32%. This falls to a dismal rate of 10% if CPR occurs for 5 more minutes. According to our research, there is a steady decremental odds of good neurological outcome for every additional 5 min of CPR. Additionally, we found that when CPR time increased to 11–15 min, there was a statistically significant drop (OR 0.1 [0.02–0.64], p 0.01) in favorable neurological outcomes. While other studies have studied the role of CPR duration on neurological outcome, our study is unique in the regard that we establish decremental odds on the neurological outcomes measured by objective standardized scoring, which has not been established by any study before. Our cumulative sample size is also the largest so far compared to all existing studies.
In a study done by Reynolds et al., it was shown that chances of good neurological outcome after 15 min of CPR fell close to 2% [12]. In a study by Goto et al., it was noted that CPR duration of less than 20 min was independently associated with improved 1 month good neurological outcomes [13]. Another study by Arima et al. conducted in Japan also shows that prognosis of out-of-hospital cardiac arrest patients deteriorated with the increase in prehospital CPR duration [14]. Overall, our study is consistent with past research showing that achievement of ROSC with CPR performed for shorter periods results in better neurological outcomes. Additionally, our analysis demonstrates an inverse relationship between CPR duration and good neurological outcomes.
While time does play an important role, a study by Park et al. noted that favorable neurological outcomes can be expected despite prolonged CPR, based on each patient’s resuscitation-related factors [15]. While this study emphasizes the role of initial rhythm, other patient-related factors playing a role in neurological outcomes despite prolonged CPR, it is similar to our study in the fact that they also report that total CPR duration was inversely associated with a CPC of 1–2 at discharge. According to another study conducted in Saudi Arabia by Albnali et al., patient-related characteristics such as age and preexisting medical comorbidities were much more important than CPR time in determining the neurological outcome [16]. Despite these factors playing a role, they also report that shorter duration of CPR was associated with favorable neurological outcomes, as seen in our study.
It is also crucial to note that one large-scale study on in-hospital cardiac arrests (IHCA) by Goldberger et al. noted that patients at hospitals with longer CPR duration protocols have a higher likelihood of return of spontaneous circulation (ROSC) and survival to discharge [6]. Although the study does describe increased ROSC, they did not note any statistically significant difference in good neurological outcome between different hospitals with short or long CPR duration protocols. It is also important to note that emergency response time also likely plays a crucial role in determining the result of CPR. In one study in Denmark conducted by Hoybe et al., it was noted that IHCA had better outcomes than OHCA likely due to quick response given witnessed arrest, although the differences disappeared on subgroup analysis of similar patient population characteristics [17]. In our study population given the way data is available to use, we were unable to determine if cardiac arrest that occurred both within and outside of a hospital had any different effects on neurological outcomes.
Along with duration of CPR, initial presenting rhythm also plays a crucial role in predicting post-cardiac arrest survival and the likelihood of a good neurological outcome. Shockable rhythm such as ventricular tachycardia or ventricular fibrillation has usually been shown to have a better neurological outcome than non-shockable rhythm. A study by Stankovic et al. notes that shockable rhythm was associated with increased ROSC, 30-day and 1-year survival [18]. Another recent large-scale study by Ho et al. notes that initial shockable rhythm and also patients who convert from non-shockable to shockable rhythms during arrest were noted to have favorable neurological outcome [19]. While it is quite clear that shockable rhythm is associated with good neurological outcome, it is also a fact that worldwide the incidence of shockable initial rhythm in OHCA is on the decline. Some studies have reported initial shockable rhythm in OHCA as low as 24%, thus explaining the dismal survival seen in OHCA patients [20]. In our meta-analysis as well, shockable rhythm was seen in only 11% of patients, thus likely explaining the poor outcomes.
Along with the rhythm, other factors like old age, witnessed or unwitnessed arrest, and comorbidities also play an important role in determining the outcome after cardiac arrest [21, 22]. The mean age of our study population was 70 years old, but age as a prognostic factor in survival post cardiac arrest is not well elucidated yet. While some studies have reported increased mortality in elderly, other studies failed to show any statistical difference in neurological outcomes irrespective of age [23, 24]. Others have suggested using frailty scores to assess chances of poor neurological outcomes in elderly rather than age [25]. Further research into effects of age on neurological outcomes in survivors post cardiac arrest is needed. Until then, it remains controversial as a prognostic tool.
While abovementioned factors help clinicians prognosticate, there are also newer prognostication techniques like neurofilament light, which reflects white matter damage and is done after 48 h of return of circulation and has been shown to accurately prognosticate unfavorable neurologic outcomes in patients following cardiac arrest [26]. Another study was done to assess if cerebral oximetry played a role in assessing neurological outcomes, but it was limited in size and did not show promising results [27]. The decision about when to withdraw care following cardiac arrest due to a chance of poor outcome is more nuanced and dependent on a lot of variable factors, but with our study we would like to guide clinicians, patients, and families to make an informed choice.
This systematic review and the results of the meta-analyses should be interpreted with caution. First, the meta-analyses are limited by the heterogeneity of the included studies. Despite using random-effects methods, the results should therefore be interpreted carefully. Leave-one-out: the sensitivity analysis done on our study demonstrated consistent outcomes. Second, given the way the data was available, we were unable to determine if cardiac arrest that occurred both within and outside of a hospital had any different effects on neurological outcomes. Thirdly, the inclusion and exclusion criteria may be a further limitation of this study. Our search was limited to papers in English, which could introduce language bias. And finally, our search was also limited to studies published after 2015 to maintain a relatively narrow time frame in which CPR protocols remain consistent. There are also newer advances like extracorporeal membrane oxygenation and targeted temperature management that have been shown to improve outcomes, but given our scope of review, we had to exclude papers pertaining to these.
Predicting neurological outcomes in cardiac arrest survivors is extremely important and more research is needed to expand on the prognostic markers and techniques, so as to help healthcare teams and families make informed decisions. Newer randomized controlled studies to assess the outcomes of extracorporeal CPR (ECPR) in comparison to conventional CPR are needed. Some observational studies have already shown promising results with increased survival and neurological outcomes in ECPR patients [28]. Also, further standardized protocols based on multimodality approaches including clinical exam, neuron-specific biomarkers, imaging, and EEG are needed to help maintain uniformity of care.
Conclusions
Most patients experiencing cardiac arrest had a non-shockable rhythm during the event. Unfortunately, most of the study population suffered from poor neurological outcomes rather than good ones. Moreover, we discovered that the chances of achieving a positive neurological outcome decrease with every additional 5 min of CPR delay. While we elucidate our findings regarding CPR duration and neurological outcomes, we do emphasize that determining optimal cut-off for CPR duration is much more nuanced and needs further studies.
Data Availability
All data generated or analyzed during this study are included in this published article. Further data is available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Abbreviations
- PCABI :
-
Post-cardiac arrest brain injury
- CPR :
-
Cardiopulmonary resuscitation
- ROSC :
-
Return of spontaneous circulation
- CPC :
-
Cerebral performance category
- OHCA :
-
Out-of-hospital cardiac arrest
- IHCA:
-
In-hospital cardiac arrest
References
Sandroni C, Cronberg Tobias, et al. Brain injury after cardiac arrest: pathophysiology, treatment, and prognosis”. Intensive Care Medicine. 2021;47(12):1393–414. https://doi.org/10.1007/s00134-021-06548-2s.
Perkins GD, Callaway C, Haywood K, et al. Brain injury after cardiac arrest. The Lancet. 2021;398(10307):1269–78. https://doi.org/10.1016/s0140-6736(21)00953-3.
Geocadin RG, Callaway CW, Fink EL, et al. Standards for studies of neurological prognostication in comatose survivors of cardiac arrest: a scientific statement from the american heart association. Circulation. 2019;140(9):e517–42.
Sandroni C, D.A.S., Nolan JP. Prognostication after cardiac arrest. Critical Care. 2018;22(1). https://doi.org/10.1186/s13054-018-2060-7.
Xue JK, Leng QY, Gao YZ, et al. Factors influencing outcomes after cardiopulmonary resuscitation in emergency department. World J Emerg Med. 2013;4(3):183–9.
Goldberger ZD, Chan P, Berg RA, Kronick SL, Cooke CR, Lu M, Banerjee M, Hayward RA, Krumholz HM: American Heart Association Get With The Guidelines—Resuscitation (formerly National Registry of Cardiopulmonary Resuscitation) Investigators. Nallamothu BK. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380(9852):1473–81. https://doi.org/10.1016/S0140-6736(12)60862-9.
Kishimori T, Matsuyama T, Kiyohara K, Kitamura T, Shida H, Kiguchi T, Nishiyama C, Kobayashi D, Okabayashi S, Shimamoto T, Sado J, Kawamura T, Iwami T. Prehospital cardiopulmonary resuscitation duration and neurological outcome after adult out-of-hospital cardiac arrest by location of arrest. Eur Heart J Acute Cardiovasc Care. 2020;9(4_suppl):S90–9. https://doi.org/10.1177/2048872620921598.
Matsuyama T, Kitamura T, Kiyohara K, Nishiyama C, Nishiuchi T, Hayashi Y, Kawamura T, Ohta B, Iwami T. Impact of cardiopulmonary resuscitation duration on neurologically favourable outcome after out-of-hospital cardiac arrest: a population-based study in Japan. Resuscitation. 2017;113:1–7. https://doi.org/10.1016/j.resuscitation.2017.01.005.
Rajan S, Folke F, Kragholm K, Hansen CM, Granger CB, Hansen SM, Peterson ED, Lippert FK, Søndergaard KB, Køber L, Gislason GH, Torp-Pedersen C, Wissenberg M. Prolonged cardiopulmonary resuscitation and outcomes after out-of-hospital cardiac arrest. Resuscitation. 2016;105:45–51. https://doi.org/10.1016/j.resuscitation.2016.05.004.
Jennett B. Assessment of outcome after severe brain damage a practical scale. The Lancet. 1975;305(7905):480–4.
Jang DH, Jo YH, Park SM, Lee KJ, Kim YJ, Lee DK. Association of the duration of on-scene advanced life support with good neurological recovery in out-of-hospital cardiac arrest. Am J Emerg Med. 2021;50:486–91.
Reynolds JC, Frisch A, Rittenberger JC, Callaway CW. Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: when should we change to novel therapies? Circulation. 2013;128(23):2488–94.
Goto Y, Funada A, Goto Y. Relationship between the duration of cardiopulmonary resuscitation and favorable neurological outcomes after out-of-hospital cardiac arrest: a prospective, nationwide, population-based cohort study. JAHA. 2016;5(3):e002819.
Arima T, Nagata O, Sakaida K, et al. Relationship between duration of prehospital resuscitation and favorable prognosis in ventricular fibrillation. Am J Emerg Med. 2015;33(5):677–81.
Park S, Lee SW, Han KS, et al. Optimal cardiopulmonary resuscitation duration for favorable neurological outcomes after out-of-hospital cardiac arrest. Scand J Trauma Resusc Emerg Med. 2022;30(1):5.
Albinali H, Alumran A, Alrayes S. Impact of cardiopulmonary resuscitation duration on the neurological outcomes of out-of-hospital cardiac arrest. Int J Emerg Med. 2022;15(1):12.
Høybye M, Stankovic N, Holmberg M, Christensen HC, Granfeldt A, Andersen LW. In-hospital vs. out-of-hospital cardiac arrest patient characteristics and survival. Resuscitation. 2021;158:157–65.
Stankovic N, Høybye M, Holmberg MJ, Lauridsen KG, Andersen LW, Granfeldt A. Factors associated with shockable versus non-shockable rhythms in patients with in-hospital cardiac arrest. Resuscitation. 2021;158:166–74.
Ho AFW, Lee KY, Nur S, et al. Association between conversion to shockable rhythms and survival with favorable neurological outcomes for out-of-hospital cardiac arrests. Prehosp Emerg Care. 2024;28(1):126–134. https://doi.org/10.1080/10903127.2023.2212039.
Oving I, de Graaf C, Karlsson L, et al. Occurrence of shockable rhythm in out-of-hospital cardiac arrest over time: a report from the COSTA group. Resuscitation. 2020;151:67–74.
Hirlekar G, Karlsson T, Aune S, et al. Survival and neurological outcome in the elderly after in-hospital cardiac arrest. Resuscitation. 2017;118:101–106. https://doi.org/10.1016/j.resuscitation.2017.07.013.
Andersen LW, Bivens MJ, Giberson T, et al. The relationship between age and outcome in out-of-hospital cardiac arrest patients. Resuscitation. 2015;94:49–54.
Van Gijn MS, Frijns D, van de Glind EMM, van Munster CB, Hamaker ME. The chance of survival and the functional outcome after in-hospital cardiopulmonary resuscitation in older people: a systematic review. Age Ageing. 2014;43(4):456–63.
Brindley PG, Markland DM, Mayers I, Kutsogiannis DJ. Predictors of survival following in-hospital adult cardiopulmonary resuscitation. CMAJ. 2002;167(4):343–8.
Hamlyn J, Lowry C, Jackson TA, Welch C. Outcomes in adults living with frailty receiving cardiopulmonary resuscitation: a systematic review and meta-analysis. Resusc Plus. 2022;11:100266.
Hoiland RL, Rikhraj KJK, Thiara S, et al. Neurologic prognostication after cardiac arrest using brain biomarkers: a systematic review and meta-analysis. JAMA Neurol. 2022;79(4):390–8.
Ibrahim AW, Trammell AR, Austin H, et al. Cerebral oximetry as a real-time monitoring tool to assess quality of in-hospital cardiopulmonary resuscitation and post cardiac arrest care. J Am Heart Assoc. 2015;4(8):e001859.
Inoue A, Hifumi T, Sakamoto T, Kuroda Y. Extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest in adult patients. JAHA. 2020;9(7):e015291.
Author information
Authors and Affiliations
Contributions
AM: writing—original draft, writing—review and editing, visualization, project administration, data extraction, screening of studies; SD: writing—original draft, writing—review and editing, visualization, project administration, data extraction, screening of studies; PP: writing—original draft, writing—review and editing, data extraction, screening of studies; MM: writing—original draft, writing—review and editing, data extraction; BB: writing—original draft, writing—review and editing, data extraction; AK: writing—original draft, writing—review and editing, data extraction; QD: writing—original draft, writing—review and editing, data extraction; SB: writing—original draft, writing—review and editing, data extraction; RD: conceptualization, methodology, software, formal analysis, resources, data curation, writing—original draft, writing—review and editing, project administration, supervision.
Corresponding author
Ethics declarations
Ethics Approval
Since the data included in this review were deidentified and already available in publicly accessible databases, the IRB review was not mandatory. This review was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Study Highlights
• CPR duration directly influences neurological outcomes in cardiac arrest patients in this comprehensive review of 349,027 cases.
• Declining odds of favorable neurological outcomes with each 5-min CPR increment, with a significant drop after 11–15 min.
• These findings emphasize the significance of timely intervention during cardiac arrest incidents in order to maximize positive neurological outcomes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mondal, A., Dadana, S., Parmar, P. et al. Unfavorable Neurological Outcomes with Incremental Cardiopulmonary Resuscitation Duration in Cardiac Arrest Brain Injury: A Systematic Review and Meta-Analysis. SN Compr. Clin. Med. 6, 23 (2024). https://doi.org/10.1007/s42399-024-01652-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-024-01652-y