Abstract
Background
This study aimed to assess the survival outcomes among patients with out-of-hospital cardiac arrest (CA) who received cardiopulmonary resuscitation (CPR) in China.
Methods
Relevant studies, published between January 1, 2010 and September 5, 2022, were retrieved from databases, including EMBASE, PubMed, Cochrane Library, the China Biology Medicine disk, China National Knowledge Infrastructure, and Wanfang databases. We included clinical studies in which all patients were diagnosed with CA and underwent out-of-hospital CPR, and the outcome variables were at least one of the following: return of spontaneous circulation (ROSC), survival to admission, survival to hospital discharge, 1-month survival, achieved good neurological outcomes, and 1-year survival. Two investigators independently extracted the study data and assessed its quality using a modified Newcastle–Ottawa Scale tool. The data were pooled using random-effects models.
Results
Of the 3620 identified studies, 49 (63,378 patients) were included in the meta-analysis. The pooled ROSC rate was 9.0% (95% confidence interval [CI] 7.5–10.5%, I2 = 97%), the pooled survival to admission rate was 5.0% (95% CI 2.7–8.0%, I2 = 98%), and the pooled survival to discharge rate was 1.8% (95% CI 1.2–2.5%, I2 = 95%). Additionally, the ROSC rate of patients with bystander CPR was significantly higher than that of those without bystander CPR, and the pooled odds ratio (OR) was 7.92 (95% CI 4.32–14.53, I2 = 85%). The ROSC rate of participants who started CPR within 5 min was significantly higher than that of those who started CPR after 5 min, and the pooled OR was 5.92 (95% CI 1.92–18.26, I2 = 85%). The ROSC rate of participants with defibrillation was significantly higher than that of those without defibrillation, and the pooled OR was 8.52 (95% CI 3.72–19.52, I2 = 77%).
Conclusion
The survival outcomes of out-of-hospital CPR in China are far below the world average. Therefore, the policy of providing automated external defibrillators (AEDs) in public places and strengthening CPR training for healthcare providers and public personnel should be encouraged and disseminated nationwide.
Trial registration This study was registered in PROSPERO (CRD42022326165) on 29 April 2022.
Similar content being viewed by others
Background
Out-of-hospital cardiac arrest (CA) is a major public health challenge [1]. In China, there are more than 230 million people with cardiovascular disease, and 550,000 individuals experience CA every year [2]. However, survival after out-of-hospital CA is poor. For example, in Beijing, the capital of China and where medical technology was well developed, only 1.3% of the patients with out-of-hospital CA were discharged alive, and only 1.0% had a favorable neurological outcome in 2012 [3]. The outcomes reported in other cities in China were similar [4, 5]. Therefore, the survival rate of out-of-hospital CA in China is estimated at less than 1%, which has been widely cited in many previous studies [2, 6,7,8,9,10,11]. Nevertheless, evidence from meta-analysis is still lacking.
In 2016, Gu et al. published a meta-analysis with 57 included studies and reported the pooled “heartbeat recovery rate” in patients with out-of-hospital CA was 17.1% [12]. In 2020, Gu et al. published an updated meta-analysis with 116 studies and reported similar results [13]. However, because of the improper inclusion and exclusion criteria, many low-quality studies were included in these two meta-analyses, and overestimation of the outcomes of out-of-hospital cardiopulmonary resuscitation (CPR) was inevitable. Moreover, the outcomes of “heartbeat recovery” or “success rate” used in the two studies were confusing.
Using uniform terms and definitions to assess survival outcomes for out-of-hospital resuscitation is the premise to compare the outcomes inter- and intrasystem and drive to quality improvement [14]. In 1991, the international guidelines for reporting and registering the outcomes of out-of-hospital CA were published, namely, Utstein reporting model [14], which was upgraded and simplified twice in 2004 [15] and 2015 [16]. Therefore, a meta-analysis using the international Utstein reporting model is necessary to assess the survival rate of patients with out-of-hospital CA who received CPR in China.
Materials and methods
We performed this meta-analysis according to the preferred reporting items for systematic reviews and meta-analyses guidelines [17]. This study was registered in PROSPERO (CRD42022326165) on 29 April 2022.
Literature retrieval
Relevant studies, published between January 1, 2010 and September 5, 2022, were retrieved from databases, including EMBASE, PubMed, Cochrane Library, the China Biology Medicine disk, China National Knowledge Infrastructure, and Wanfang databases. The English keywords were “Out-of-Hospital Cardiac Arrest,” “Cardiopulmonary Resuscitation,” and “China [Affiliation].” The Chinese keywords were “心脏骤停” and “心肺复苏.” In addition, reference lists of the relevant articles were manually checked for other potentially relevant papers.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) the study population was composed of adults (age ≥ 18 years); (2) patients with CA that caused by heart problem; (3) patients were diagnosed with CA and underwent out-of-hospital CPR; and (4) the outcome variables were at least one of the following: return of spontaneous circulation (ROSC), survival to admission, survival to hospital discharge, 1-month survival, achieved good neurological outcomes, and 1-year survival. The definition of CA and these outcomes is shown in Additional file 1: Table S1.
The exclusion criteria were as follows: (1) ≥ 20% of patients were children; (2) ≥ 20% of patients with specific causes of CA, such as trauma, myocardial infarction, or drowning; (3) studies in that only specific patients were selected, such as patients with mechanical compression or hands-only CPR; (4) with the absence or ambiguous definitions of CA; (5) with the absence or ambiguous definitions of survival outcomes, such as “successful recovery” or “heartbeat recovery”; and (6) abstract, reviews, case reports, case–control studies, and animal studies.
Two investigators (YW and ZHS) independently screened article titles and abstracts retrieved from the literature search. Full texts of potentially eligible studies were further assessed for final inclusion. A third investigator (GZZ) cross-checked extracted data, and disagreements were resolved through consensus.
Data extraction and quality evaluation
For each paper, the first author, year of publication, country or region of publication, sample size, sex, age, and other patient-related data were extracted. The ROSC, survival to admission, survival to hospital discharge, 1-month survival, and achieved good neurological outcomes were also analyzed as outcome variables. Two investigators (YW and ZHS) independently extracted data from individual studies. Full texts of potentially eligible studies were further assessed for final inclusion. A third investigator (GZZ) cross-checked extracted data, and disagreements were resolved through consensus.
A modified version of Newcastle–Ottawa Scale (NOS) was used to assess the quality of each study. Studies with NOS score of 1–2, 3–4, and 5–6 were considered of low, intermediate, and high quality, respectively. Two investigators (YW and ZHS) independently assessed the methodological quality of a quarter of the studies, and the third investigator (GZZ) independently reviewed those assessments. Disagreements were resolved through consensus.
Statistical analysis
A random-effects model was used to calculate pooled results and a 95% confidence interval (CI). I2 statistic was used to assess heterogeneity of included studies [18], with I2 > 50% suggesting significant heterogeneity. “Acsine” test was set as a parameter in publication bias detection. All P-values were two sided. A P-value < 0.05 was considered statistically significant. This meta-analysis was conducted using the “meta” package in R statistical software version 3.4.3 (Schwarzer, 2007; Team, 2017).
Results
Characteristics of the selected studies
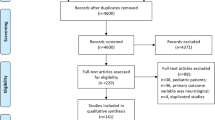
A total of 3620 papers were retrieved. After excluding duplicate and irrelevant papers, a total of 49 studies, including 63,378 patients, were included. The literature retrieval flow chart is shown in Fig. 1.
Of the 49 studies, 42 were from Eastern China, and 7 were from Western China. Additionally, 25 studies included adults, 15 included adults and children, and 9 did not state the age of the participants. Only 20 studies reported information on bystander CPR, and only 6 stated that more than 20 participants received bystander CPR. For detailed characteristics of study individuals, see Additional file 1: Table S2.
The characteristics of the included papers are shown in Additional file 1: Table S2. The results of the evaluation of the study quality, according to the NOS scale, are shown in Additional file 1: Fig. S1.
Return of spontaneous circulation (ROSC)
A total of 46 studies with 62,751 participants were eligible for the calculation of the ROSC rate, and the pooled rate was 9.0% (95% CI 7.5–10.5%, I2 = 97%), see Fig. 2. Subgroup analyses showed that the ROSC rate of group with less than 500 participants was significant more than that of group with participants of more than 500, with pooled rate of (14.4%; 95% CI 10.5–18.7%, I2 = 96%) and (4.2%; 95% CI 3.4–5.1%, I2 = 96%), respectively. In addition, subgroup analyses also showed differences in the ROSC rate by age of participants and proportion of bystander CPR, however, the 95% CIs were overlapped, See Table 1.
Survival to admission
Ten studies with 13,922 participants were eligible for the comparison of the calculation of survival to admission rate, and the pooled rate was 5.0% (95% CI 2.7–8.0%, I2 = 98%), see Fig. 3. Subgroup analyses showed differences in survival to admission rate by year of publication, area, proportion of bystander CPR, and number of participants, however, the 95% CIs were overlapped, see Table 1.
Survival to discharge
Eighteen studies with 43,905 participants were eligible for the comparison of calculation of the survival to discharge rate, and the pooled rate was 1.8% (95% CI 1.2–2.5%, I2 = 95%), see Fig. 4. Subgroup analyses showed that the survival to discharge rate of group with less than 500 participants was significant more than that of group with participants of more than 500, with pooled rate of (4.3%; 95% CI 2.0–7.4%, I2 = 87%) and (0.7%; 95% CI 0.4–1.2%, I2 = 94%), respectively. In addition, Subgroup analyses also showed differences in survival to discharge rate by the year of publication, proportion of males, proportion of bystander CPR and quality of the included studies, however, the 95% CIs were overlapped, see Table 1.
One-month survival and achieved good neurological outcomes
Only two studies with 1,154 participants were eligible for the comparison of calculation of the 1-month survival rate, and the pooled rate was 2.7% (95% CI 0.0–14.5%, I2 = 95%). Likewise, only three studies with 2267 participants were eligible for the comparison of calculation of achieved good neurological outcomes rate, and the pooled rate was 2.5% (95% CI 0.2–7.0%, I2 = 94%), see Table 1.
Contributors for ROSC rate
As shown in Table 2 and Additional file 1: Figs. S1–S4, the ROSC rate of participants with bystander CPR was significantly higher than that of those without bystander CPR, and the pooled OR was 7.92 (95% CI 4.32–14.53, I2 = 85%). The ROSC rate of the participants who started CPR within 5 min was significantly higher than that of those who started CPR after 5 min, and the pooled OR was 5.92 (95% CI 1.92–18.26, I2 = 85%). The ROSC rate of participants with defibrillation was significantly higher than that of those without defibrillation, and the pooled OR was 8.52 (95% CI 3.72–19.52, I2 = 77%). However, there was no difference between participants with and without advanced airways, and the pooled OR was 1.12 (95% CI 0.84–1.78, I2 = 76%).
Publication bias
The funnel plot was symmetrical for the meta-analysis of the incidence of ROSC, survival to admission, and survival to discharge in patients with out-of-hospital CA who received CPR (see Additional file 1: Fig. S5). The “Acsine” test revealed no evidence of publication bias in survival to admission (P = 0.1284) and survival to discharge (P = 0.0883). However, there was a publication bias in ROSC (P = 0.0011).
Discussion
To the best of our knowledge, this is the first meta-analysis to assess survival outcomes among out-of-hospital CPR using Utstein reporting model in China. We found that the pooled ROSC rate was 9.0% (95% CI 7.5–10.5%, I2 = 97%), the pooled survival to admission rate was 5.0% (95% CI: 2.7–8.0%, I2 = 98%), and the pooled survival to discharge rate was 1.8% (95% CI 1.2–2.5%, I2 = 95%).
In 2020, Yan et al. assessed the global survival rate among adult out-of-hospital CPR and found that the pooled ROSC rate was 29.7% (95% CI 27.6–31.7%), the pooled survival to admission rate was 22.0% (95% CI 20.7–23.4%), and the pooled survival to discharge rate was 8.8% (95% CI 8.2–9.4%)[19]. Even in Asia, which has the lowest survival rate, the pooled ROSC rate was 22.1% (95% CI 18.1–26.0%), the pooled survival to admission rate was 15.6% (95% CI 13.2–18.0%), and the pooled survival to discharge rate was 4.5% (95% CI 3.1–5.9%)[19]. Therefore, our study found very frustrating results; that is, the survival outcomes of out-of-hospital CA in China are far below the world average.
It should be pointed out that almost all the included studies were from large or medium cities, irrespective of the eastern or western regions. Currently, few studies from small cities or rural areas in China have been published. Moreover, our subgroup analysis found that survival rates were affected by the number of participants in our meta-analysis, and the group with participants more than 500 was lower than that of group with participants less than 500. Large sample studies usually have better research designs and provide more reliable results [4, 20, 21]. Therefore, the actual survival outcomes in China may be lower than that of our pooled results. More pessimistically, our subgroup analysis showed no difference in the survival outcomes between the 2010–2015 and 2016–2022 groups, which means that the survival rate of out-of-hospital CA might not have increased in the past 12 years.
Our meta-analysis revealed that the ROSC rate of those who started CPR within 5 min was 5.92 times that of those who started CPR after 5 min. In addition, the ROSC rate of those with bystander CPR was 7.92 times that of those without bystander CPR. Our results support that early bystander CPR is a key determinant of survival [22,23,24,25]. However, the implementation rate for bystander CPR in China is low (11.4% in Beijing [3, 26], 8.83% in Zhenzhou [27], and 0.59% in Hefei [4], vs. 39.4% in the United States [28] and 39% in Australia [29]) since the prevalent training rate in China is less than 1% and skill retention training is also rare [2]. Our meta-analysis also revealed that the ROSC rate of those with defibrillation was 8.52 times that of those without defibrillation. Recently, the Chinese government has begun to attach importance to out-of-hospital CA. Provision of automated external defibrillators in public places and financial support for public training provide the possibility to improve the survival rate in the future.
In Gu et al.’s meta-analysis [12, 13], unclear outcomes of “heartbeat recovery” or “success rate” were used, which reflected that researchers were unfamiliar with Utstein reporting model. In fact, we conducted a survey on the perception of Utstein model among Chinese healthcare providers in 2017 [30]; 41.2% of 10,224 participants reported that they had not heard of Utstein model. In addition, Chinese healthcare providers always use “successful resuscitation” to assess the outcome of CPR. However, the understanding of the term is confused in China. In the survey, 40.9%, 23.1%, and 21.6% of Chinese medical staff considered the recovery of spontaneous rhythm, pulse, and breathing as “successful resuscitation,” respectively. Therefore, it is urgent to strengthen the perception training and application of Utstein registration model in China.
Limitation
The meta-analysis had several limitations. First, most included studies were from large or medium cities. Second, most included studies were retrospective observational studies. Third, while obvious heterogeneity was present in several groups, subgroup analyses were not possible to identify the source of heterogeneity.
Conclusion
The survival outcomes of out-of-hospital CA in China are far below the world average. Therefore, providing AED in public places and strengthening CPR training for healthcare providers and public personnel should be encouraged and disseminated nationwide.
Availability of data and materials
Data may be made available by contacting the corresponding author.
Abbreviations
- AED:
-
Automated external defibrillator
- CA:
-
Cardiac arrests
- CPR:
-
Cardiopulmonary resuscitation
- CI:
-
Confidence interval
- NOS:
-
NEWCASTLE–Ottawa Scale tool
- OR:
-
Odds ratio
- ROSC:
-
Return of spontaneous circulation
References
Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–87.
Xu F, Zhang Y, Chen Y. cardiopulmonary resuscitation training in China: current situation and future development. JAMA Cardiol. 2017;2:469–70.
Shao F, Li CS, Liang LR, Li D, Ma SK. Outcome of out-of-hospital cardiac arrests in Beijing. China Resusc. 2014;85:1411–7.
Wang Y, Zhang Q, Qu GB, Fang F, Dai XK, Yu LX, et al. Effects of prehospital management in out-of-hospital cardiac arrest: advanced airway and adrenaline administration. BMC Health Serv Res. 2022;22:546.
Li X, Teng F, Xu P, Li M, Liu R, Fang P, et al. Analysis of out-of-hospital emergency treatment for ventricular fibrillation between 2013 and 2016 in Shanghai. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2017;29:871–6.
Jiang Y, Wu B, Long L, Li J, Jin X. Attitudes and willingness toward out-of-hospital cardiopulmonary resuscitation: a questionnaire study among the public trained online in China. BMJ Open. 2020;10: e038712.
Mao J, Chen F, Xing D, Zhou H, Jia L, Zhang Y. Knowledge, training and willingness to perform bystander cardiopulmonary resuscitation among university students in Chongqing, China: a cross-sectional study. BMJ Open. 2021;11: e046694.
Zhang L, Luo M, Myklebust H, Pan C, Wang L, Zhou Z, et al. When dispatcher assistance is not saving lives: assessment of process compliance, barriers and outcomes in out-of-hospital cardiac arrest in a metropolitan city in China. Emerg Med J. 2021;38:252–7.
Yan S, Gan Y, Wang R, Song X, Zhou N, Lv C. Willingness to attend cardiopulmonary resuscitation training and the associated factors among adults in China. Crit Care. 2020;24:457.
Zhang L, Li B, Zhao X, Zhang Y, Deng Y, Zhao A, et al. Public access of automated external defibrillators in a metropolitan city of China. Resuscitation. 2019;140:120–6.
Wang LX, Meng QY, Yu T. National consensus on cardiopulmonary resuscitation in China. Chinese J Dis Med. 2016;5:1–23.
Gu XM, Li ZH, He ZJ, Zhao ZW, Liu SQ. A meta-analysis of the success rates of heartbeat restoration within the platinum 10 min among outpatients suffering from sudden cardiac arrest in China. Mil Med Res. 2016;3:6.
Gu XM, Yao SB, He ZJ, Wang YG, Li ZH. Meta-analysis of the success rate of heartbeat recovery in patients with prehospital cardiac arrest in the past 40 years in China. Mil Med Res. 2020;7:34.
Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. a statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991;84:960–75.
Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. a statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European resuscitation council, Australian resuscitation council, New Zealand Resuscitation council, heart and stroke Foundation of Canada, InterAmerican heart Foundation, Resuscitation council of Southern Africa). Resuscitation. 2004;63:233–49.
Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the international liaison committee on resuscitation; and the american heart association emergency cardiovascular care committee and the council on cardiopulmonary, critical care. Perioper Resusc Circ. 2015;132:1286–300.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339: b2700.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24:61.
Shao F, Li H, Ma S, Li D, Li C. Outcomes of out-of-hospital cardiac arrest in Beijing: a 5-year cross-sectional study. BMJ Open. 2021;11: e041917.
Chen Y, Yue P, Wu Y, Li J, Lei Y, Gao D, et al. Trend in survival after out-of-hospital cardiac arrest and its relationship with bystander cardiopulmonary resuscitation: a six-year prospective observational study in Beijing. BMC Cardiovasc Disord. 2021;21:625.
Nas J, Thannhauser J, Konijnenberg L, van Geuns RM, van Royen N, Bonnes JL, et al. Long-term effect of face-to-face vs virtual reality cardiopulmonary resuscitation (CPR) training on willingness to perform CPR, retention of knowledge, and dissemination of CPR awareness: a secondary analysis of a randomized clinical trial. JAMA Netw Open. 2022;5: e2212964.
Nas J, Thannhauser J, Herrmann JJ, van der Wulp K, van Grunsven PM, van Royen N, et al. Changes in automated external defibrillator use and survival after out-of-hospital cardiac arrest in the Nijmegen area. Neth Heart J. 2018;26:600–5.
Malta Hansen C, Kragholm K, Pearson DA, Tyson C, Monk L, Myers B, et al. Association of bystander and first-responder intervention with survival after out-of-hospital cardiac arrest in North Carolina, 2010–2013. JAMA. 2015;314:255–64.
Kragholm K, Wissenberg M, Mortensen RN, Hansen SM, Malta Hansen C, Thorsteinsson K, et al. Bystander efforts and 1-year outcomes in out-of-hospital cardiac arrest. N Engl J Med. 2017;376:1737–47.
Zheng K, Bai Y, Zhai QR, Du LF, Ge HX, Wang GX, et al. Correlation between the warning symptoms and prognosis of cardiac arrest. World J Clin Cases. 2022;10:7738–48.
Yingxin C, Sisen Z, Yanzhang S, Libin L. Investigation of out-of-hospital cardiac arrest in Zhengzhou City and the risk factors of prognosis of cardiopulmonary resuscitation: case analysis for 2016–2018. Chin Crit Care Med. 2019;3:439–43.
Ok Ahn K, McNally B, Al-Araji R, Cisneros C, Chan PS. Sex differences in the association between bystander CPR and survival for Out-of-Hospital cardiac arrest. Resuscitation. 2022. https://doi.org/10.1016/j.resuscitation.2022.09.016.
Munot S, Rugel EJ, Von Huben A, Marschner S, Redfern J, Ware S, et al. Out-of-hospital cardiac arrests and bystander response by socioeconomic disadvantage in communities of New South Wales. Australia Resusc Plus. 2022;9: 100205.
Jinglin Li LY, Zhenzhou Wang SQ, Zhou G. A survey on the perception of utstein model and the success of resuscitation among the Chinese medical staffs. J Kunming Med Univ. 2020;11:43–149.
Acknowledgements
The authors are grateful to Shunli Cai and Xin Guo for their careful examination for this manuscript.
Funding
Our study was financed by the Talent Project of Kunming Health Science and Technology (NO. 2022-SW [Leading Talents]-001) and the Special Project “Spring City Plan” Famous Doctor (NO. C202012016).
Author information
Authors and Affiliations
Contributions
GZZ, YW, ZZW, and CS initiated the project and were responsible for protocol design. GZZ, YW, and ZHS performed the literature review, collected the data, assessed the quality of studies, and analyzed the data. MQY, YLM, QXW, CYW, and JX interpreted the data. GZZ and CS wrote the initial draft of the manuscript. All the authors were responsible for critical revision of the manuscript and provided important intellectual input. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval was not required for this systematic review.
Consent for publication
Not applicable.
Competing interests
The authors declare that this study was conducted in the absence of any commercial or financial relationships that could be construed as a potential competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Definition of survival outcomes. Table S2. Detailed individual study characteristics. Figure S1. The quality of included studies. Figure S2. Forest plot of the odds ratio of ROSC rate with bystander CPR vs. without bystander CPR. Figure S3. Forest plot of the odds ratio of ROSC rate in start CPR time within 5 minutes vs. more than 5 minutes. Figure S4. Forest plot of the odds ratio of ROSC rate with defibrillation vs. without defibrillation. Figure S5. Forest plot of the odds ratio of ROSC rate with advanced airway (AA) vs. without advanced airway. Figure S6 Funnel plot of ROSC rate, survival to admission rate and survival to discharge rate ROSC rate (A), survival to admission rate (B), and survival to discharge rate (C).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, G., Wang, Y., Sun, Z. et al. Survival outcome among patients with out-of-hospital cardiac arrest who received cardiopulmonary resuscitation in China: a systematic review and meta-analysis. Eur J Med Res 28, 8 (2023). https://doi.org/10.1186/s40001-022-00955-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-022-00955-x