Abstract
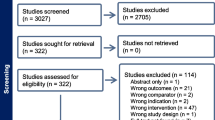
Migraine is a disabling condition that is currently underdiagnosed and undertreated. Transcutaneous vagus nerve stimulation (VNS) is among the most researched non-invasive brain stimulation techniques for migraine control. In this systematic review, we discuss the effects of VNS parameters (waveform, frequency, intensity, cycle, and current) and central and clinical mechanisms in auricular (taVNS) or cervical (tcVNS) transcutaneous VNS in the control of migraine pain. PubMed (National Library of Medicine), Cochrane Library, CAPES Journals (Portal of Journals of the Coordination for the Improvement of Higher Education Personnel), Virtual Health Library (VHL), and Google Scholar were searched by computer from the establishment of within the 10-year period (2011– 2021). Initially, a total of 10,017 articles were identified. After applying the exclusion criteria, 10,007 articles were excluded. The eligibility criteria were analyzed and only ten articles fulfilled the criteria. The most used parameters in this study for VNS were the frequencies of 1 Hz, 25 Hz, and 30 Hz. The 1-Hz stimulation caused a more significant reduction in the number of days with headache. The total stimulation time varies between studies, ranging from 2 to 240 min, and can be repeated for a period or a single session. Studies that used a longer treatment period showed clinical results in reducing pain and analyzed the scores. Moreover, studies have shown reduced intensity or severity of pain after taVNS. The studies performed taVNS or tcVNS, and both methods had positive effects on migraine control, pain reduction, and migraine score.
Key Message
An systematic literature review of transcutaneous vagus nerve stimulation (tVNS) on migraine pain management. The results indicate that auricular or cervical tVNS methods had positive effects on migraine control, pain reduction, and migraine score.

Similar content being viewed by others
Data availability
Not applicable.
Code Availability
Not applicable.
References
Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C, Akerman S. Pathophysiology of migraine: a disorder of sensory processing. Physiol Rev. 2017;97(2):553–622.
Steiner TJ, Birbeck GL, Jensen RH, Katsarava Z, Stovner LJ, Martelletti P. Headache disorders are third cause of disability worldwide. J Headache Pain. 2015;16:58.
Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388(10053):1545–602.
Deneris A, Rosati Allen P, Hart Hayes E, Latendresse G. Migraines in women: current evidence for management of episodic and chronic migraines. J Midwifery Womens Health. 2017;62(3):270–85.
Viana M, Sances G, Ghiotto N, Guaschino E, Allena M, Nappi G, et al. Variability of the characteristics of a migraine attack within patients. Cephalalgia. 2016;36(9):825–30.
Katsarava Z, Manack A, Yoon MS, Obermann M, Becker H, Dommes P, et al. Chronic migraine: classification and comparisons. Cephalalgia. 2011;31(5):520–9.
Evers S, Afra J, Frese A, Goadsby PJ, Linde M, May A, et al. EFNS guideline on the drug treatment of migraine–revised report of an EFNS task force. Eur J Neurol. 2009;16(9):968–81.
Silberstein SD, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78(17):1337–45.
Magis D. Neuromodulation in migraine: state of the art and perspectives. Expert Rev Med Devices. 2015;12(3):329–39.
Schoenen J, Roberta B, Magis D, Coppola G. Noninvasive neurostimulation methods for migraine therapy: the available evidence. Cephalalgia. 2016;36(12):1170–80.
Driessen AK. Vagal afferent processing by the paratrigeminal nucleus. Front Physiol. 2019;10:1110.
Henssen D, Derks B, van Doorn M, Verhoogt N, Cappellen Van, van Walsum AM, Staats P, et al. Vagus nerve stimulation for primary headache disorders: an anatomical review to explain a clinical phenomenon. Cephalalgia. 2019;39(9):1180–94.
Coppola G, Vandenheede M, Di Clemente L, Ambrosini A, Fumal A, De Pasqua V, et al. Somatosensory evoked high-frequency oscillations reflecting thalamo-cortical activity are decreased in migraine patients between attacks. Brain. 2005;128(Pt 1):98–103.
Yap JYY, Keatch C, Lambert E, Woods W, Stoddart PR, Kameneva T. Critical review of transcutaneous vagus nerve stimulation: challenges for translation to clinical practice. Front Neurosci. 2020;14:284.
Tassorelli C, Grazzi L, de Tommaso M, Pierangeli G, Martelletti P, Rainero I, et al. Noninvasive vagus nerve stimulation as acute therapy for migraine: the randomized PRESTO study. Neurology. 2018;91(4):e364–73.
Hord ED, Evans MS, Mueed S, Adamolekun B, Naritoku DK. The effect of vagus nerve stimulation on migraines. J Pain. 2003;4(9):530–4.
Mosqueira AJ, López-Manzanares L, Canneti B, Barroso A, García-Navarrete E, Valdivia A, et al. Vagus nerve stimulation in patients with migraine. Rev Neurol. 2013;57(2):57–63.
Yuan H, Silberstein SD. Vagus nerve and vagus nerve stimulation, a comprehensive review: Part I. Headache. 2016;56(1):71–8.
Yuan H, Silberstein SD. Vagus nerve stimulation and headache. Headache. 2017;57(Suppl 1):29–33.
Goadsby PJ, Grosberg BM, Mauskop A, Cady R, Simmons KA. Effect of noninvasive vagus nerve stimulation on acute migraine: an open-label pilot study. Cephalalgia. 2014;34(12):986–93.
Straube A, Ellrich J, Eren O, Blum B, Ruscheweyh R. Treatment of chronic migraine with transcutaneous stimulation of the auricular branch of the vagal nerve (auricular t-VNS): a randomized, monocentric clinical trial. J Headache Pain. 2015;16:543.
Grazzi L, Usai S, Bussone G. EHMTI-0036. GammaCore device for treatment of migraine attack: preliminary report. J Headache Pain. 2014;15(Suppl 1):G12-G.
Grazzi L, Egeo G, Calhoun AH, McClure CK, Liebler E, Barbanti P. Non-invasive vagus nerve stimulation (nVNS) as mini-prophylaxis for menstrual/menstrually related migraine: an open-label study. J Headache Pain. 2016;17(1):91.
Barbanti P, Grazzi L, Egeo G, Padovan AM, Liebler E, Bussone G. Non-invasive vagus nerve stimulation for acute treatment of high-frequency and chronic migraine: an open-label study. J Headache Pain. 2015;16:61.
Kinfe TM, Pintea B, Muhammad S, Zaremba S, Roeske S, Simon BJ, et al. Cervical non-invasive vagus nerve stimulation (nVNS) for preventive and acute treatment of episodic and chronic migraine and migraine-associated sleep disturbance: a prospective observational cohort study. J Headache Pain. 2015;16:101.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Allais G, Chiarle G, Sinigaglia S, Airola G, Schiapparelli P, Benedetto C. Gender-related differences in migraine. Neurol Sci. 2020;41(2):429–36.
Baksa D, Gecse K, Kumar S, Toth Z, Gal Z, Gonda X, et al. Circadian variation of migraine attack onset: a review of clinical studies. Biomed Res Int. 2019;2019:4616417.
Broner SW, Bobker S, Klebanoff L. Migraine in women. Semin Neurol. 2017;37(6):601–10.
Wijeratne T, Tang HM, Crewther D, Crewther S. Prevalence of migraine in the elderly: a narrated review. Neuroepidemiology. 2019;52(1–2):104–10.
Redgrave J, Day D, Leung H, Laud PJ, Ali A, Lindert R, et al. Safety and tolerability of transcutaneous vagus nerve stimulation in humans; a systematic review. Brain Stimul. 2018;11(6):1225–38.
Diener H-C, Holle-Lee D, Nägel S, Dresler T, Gaul C, Göbel H, et al. Treatment of migraine attacks and prevention of migraine: guidelines by the German Migraine and Headache Society and the German Society of Neurology. Clinical and Translational Neuroscience. 2019;3(1):2514183X18823377.
Chaudhry SR, Lendvai IS, Muhammad S, Westhofen P, Kruppenbacher J, Scheef L, et al. Inter-ictal assay of peripheral circulating inflammatory mediators in migraine patients under adjunctive cervical non-invasive vagus nerve stimulation (nVNS): a proof-of-concept study. Brain Stimul. 2019;12(3):643–51.
Silberstein SD, Calhoun AH, Lipton RB, Grosberg BM, Cady RK, Dorlas S, et al. Chronic migraine headache prevention with noninvasive vagus nerve stimulation: the EVENT study. Neurology. 2016;87(5):529–38.
Howland RH. Vagus Nerve Stimulation. Curr Behav Neurosci Rep. 2014;1(2):64–73.
Kiyokawa J, Yamaguchi K, Okada R, Maehara T, Akita K. Origin, course and distribution of the nerves to the posterosuperior wall of the external acoustic meatus. Anatomical science international. 2014;89(4):238–45.
Peuker ET, Filler TJ. The nerve supply of the human auricle. Clin Anat. 2002;15(1):35–7.
Farias MMMD, Wenceslau CV, Passos J, Teixeira DG, Araújo KPC, Ambrósio CE, et al. Comportamento dos nervos glossofaríngeo e vago, na região retrofaríngea de ovinos: origem aparente no crânio, trajeto, ramificação e distribuição. Pesquisa Veterinária Brasileira. 2007;27:115–23.
Zhang Y, Liu J, Li H, Yan Z, Liu X, Cao J, et al. Transcutaneous auricular vagus nerve stimulation at 1 Hz modulates locus coeruleus activity and resting state functional connectivity in patients with migraine: An fMRI study. Neuroimage Clin. 2019;24:101971.
Cao J, Zhang Y, Li H, Yan Z, Liu X, Hou X, et al. Different modulation effects of 1 Hz and 20 Hz transcutaneous auricular vagus nerve stimulation on the functional connectivity of the periaqueductal gray in patients with migraine. J Transl Med. 2021;19(1):354.
Lipton RB, Stewart WF, Sawyer J, Edmeads JG. Clinical utility of an instrument assessing migraine disability: the migraine disability assessment (MIDAS) questionnaire. Headache. 2001;41(9):854–61.
Yang M, Rendas-Baum R, Varon SF, Kosinski M. Validation of the Headache Impact Test (HIT-6™) across episodic and chronic migraine. Cephalalgia an international journal of headache. 2011;31(3):357–67.
Rendas-Baum R, Bloudek LM, Maglinte GA, Varon SF. The psychometric properties of the migraine specific quality of life questionnaire version 2.1 (MSQ) in chronic migraine-patients. Qual Life Res. 2013;22(5):1123–33.
Farrahi Moghaddam J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Reliability and validity of the Persian version of the Pittsburgh sleep quality index (PSQI-P). Sleep Breath. 2012;16(1):79–82.
Kühner C, Bürger C, Keller F, Hautzinger M. Reliabilität und Validität des revidierten Beck-Depressionsinventars (BDI-II). Nervenarzt. 2007;78(6):651–6.
Straube A, Eren O. tVNS in the management of headache and pain. Auton Neurosci. 2021;236:102875.
Rawson FJ. New dimensions in controlling cellular function with electroceutics. Ther Deliv. 2015;6(1):5–8.
Dietrich S, Smith J, Scherzinger C, Hofmann-Preiss K, Freitag T, Eisenkolb A, et al. A novel transcutaneous vagus nerve stimulation leads to brainstem and cerebral activations measured by functional MRI. Biomed Tech (Berl). 2008;53(3):104–11.
Yakunina N, Kim SS, Nam EC. Optimization of transcutaneous vagus nerve stimulation using functional MRI. Neuromodulation. 2017;20(3):290–300.
Vachon-Presseau E. Effects of stress on the corticolimbic system: implications for chronic pain. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):216–23.
Maizels M, Aurora S, Heinricher M. Beyond neurovascular: migraine as a dysfunctional neurolimbic pain network. Headache. 2012;52(10):1553–65.
Luo W, Zhang Y, Yan Z, Liu X, Hou X, Chen W, et al. The instant effects of continuous transcutaneous auricular vagus nerve stimulation at acupoints on the functional connectivity of amygdala in migraine without aura: a preliminary study. Neural Plast. 2020;2020:8870589.
Garcia RG, Lin RL, Lee J, Kim J, Barbieri R, Sclocco R, et al. Modulation of brainstem activity and connectivity by respiratory-gated auricular vagal afferent nerve stimulation in migraine patients. Pain. 2017;158(8):1461–72.
Van Bockstaele EJ, Peoples J, Telegan P. Efferent projections of the nucleus of the solitary tract to peri-locus coeruleus dendrites in rat brain: evidence for a monosynaptic pathway. J Comp Neurol. 1999;412(3):410–28.
Akerman S, Holland PR, Goadsby PJ. Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci. 2011;12(10):570–84.
Ossipov MH, Morimura K, Porreca F. Descending pain modulation and chronification of pain. Curr Opin Support Palliat Care. 2014;8(2):143–51.
Ellrich J, Messlinger K, Chiang CY, Hu JW. Modulation of neuronal activity in the nucleus raphé magnus by the 5-HT(1)-receptor agonist naratriptan in rat. Pain. 2001;90(3):227–31.
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES)—Finance Code 001. AFB is funded by CNPq (Grant number 305539/2021-3.
Author information
Authors and Affiliations
Contributions
Conception and design: JRTS, MLS, FXB, AFB. Administrative support: MLS, FXB, AFB. Provision of study materials or patients: ACC, ALCM, LLF, JRTS, FXB. Collection and assembly of data: ACC, ALCM, JRTS, MLS, AFB. Data analysis and interpretation: All authors. Manuscript writing: All authors. Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Carvalho, A.C., Marques, A.L.C., Ferreira, L.L. et al. Transcutaneous Vagus Nerve Stimulation: an Alternative Treatment of Chronic Migraine—a Systematic Review. SN Compr. Clin. Med. 4, 188 (2022). https://doi.org/10.1007/s42399-022-01268-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-022-01268-0