Key summary points
To evaluate the combined effect of sex- and age-related physiological and biological changes on drug pharmacokinetics.
AbstractSection FindingsMedian peak concentration and drug exposure were on average 22% and 20% higher in women compared with men. With increasing age, sex differences in peak concentration tended to be more pronounced but remained similar for drug exposure.
AbstractSection MessageThe pharmacokinetic differences between women and men are modest and, with the exception of peak concentration, remain constant with increasing age.
Abstract
Purpose
The proportion of women increases with advanced age, but older women are often underrepresented in clinical trials. Therefore, little is known about the combined effect of sex- and age-related physiological changes on drug pharmacokinetics.
Methods
We compiled clinical studies, which investigated sex-related pharmacokinetic differences both in older and young women and men. The ratio women/men was calculated for various pharmacokinetic parameters across adulthood to assess sex-related differences in drug pharmacokinetics with aging. The contribution of body weight and drug characteristics to sex-related pharmacokinetic differences were explored using analysis of variance.
Results
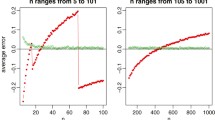
We found 67 studies reporting the pharmacokinetics for 56 drugs both in older and young women and men. Median peak concentration (Cmax) (interquartile range (IQR)) and drug exposure (AUC) (IQR) were 22% (8–41%) and 20% (0–39%) higher in women compared with men whereas time to peak concentration (tmax), apparent volume of distribution (VdF) and elimination half-life (t1/2) were not significantly different. Body weight and the drug main elimination pathway contributed to sex-related differences in Cmax and AUC. Relative to men, women had a modest increase in Cmax with increasing age (r = 0.19, p = 0.04). Conversely, sex-related differences in AUC remained constant with increasing age.
Conclusion
The pharmacokinetic differences between women and men were modest and, with the exception of Cmax, remained constant with increasing age. The higher plasma concentration might be correlated to more adverse events in older women and thus, drug treatment should be started on the lower recommended dosage when appropriate particularly for drugs characterized by a narrow therapeutic index.



Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available in the article and supplementary material of this article.
Code availability
The mathematical code for the statistical analysis is available from the corresponding author upon reasonable request.
References
Soldin OP, Mattison DR (2009) Sex differences in pharmacokinetics and pharmacodynamics. Clin Pharmacokinet 48:143–157
Stader F, Siccardi M, Battegay M, Kinvig H, Penny MA, Marzolini C (2019) Repository describing an aging population to inform physiologically based pharmacokinetic models considering anatomical, physiological, and biological age-dependent changes. Clin Pharmacokinet 58:483–501
Chetty M, Mattison D, Rostami-Hodjegan A (2012) Sex differences in the clearance of CYP3A4 substrates: exploring possible reasons for the substrate dependency and lack of consensus. Curr Drug Metab 13:778–786
Stader F, Courlet P, Kinvig H, Battegay M, Decosterd LA, Penny MA, Siccardi M, Marzolini C (2020) Effect of ageing in antiretroviral drug pharmacokinetics using clinical data combined with modelling and simulation. Br J Clin Pharmacol 87:458–470
Stader F, Kinvig H, Penny MA, Battegay M, Siccardi M, Marzolini C (2020) Physiologically based pharmacokinetic modelling to identify pharmackokinetic parameters driving drug exposure changes in the elderly. Clin Pharmacokinet 59:383–401
Pinnow E, Sharma P, Parekh A, Gevorkian N, Uhl K (2009) Increasing participation of women in early phase clinical trials approved by the FDA. Womens Health Issues 19:89–93
US Food and Drug Administration (2014) Bioavailability and bioequivalence studies submitted in NDAs or INDs—general considerations
Jamei M, Dickinson GL, Rostami-Hodjegan A (2009) A framework for assessing inter-individual variability in pharmacokinetics using virtual human populations and integrating general knowledge of physical chemistry, biology, anatomy, physiology and genetics: a tale of ‘bottom-up’vs ‘top-down’recognition of covariates. Drug Metab Pharmacokinet 24:53–75
Schwartz JB (2003) The influence of sex on pharmacokinetics. Clin Pharmacokinet 42:107–121
Franconi F, Campesi I (2014) Pharmacogenomics, pharmacokinetics and pharmacodynamics: interaction with biological differences between men and women. Br J Pharmacol 2014:580–594
Yang L, Li Y, Hong H et al (2012) Sex differences in the expression of drug metabolizing and transporter genes in human liver. J Drug Metab Toxicol 3:1000119
Bebia Z, Buch SC, Wilson JW et al (2004) Bioequivalence revisited: influence of age and sex on CYP enzymes. Clin Pharmacol Ther 76:618–627
Achour B, Barber J, Rostami-Hodjegan A (2014) Expression of hepatic drug-metabolizing cytochrome p450 enzymes and their intercorrelations: a meta-analysis. Drug Metab Dispos 42:1349–1356
Greenblatt DJ, Harmatz JS, von Moltke LL, Wright CE, Durol ALB, Harrel-Joseph LM, Shader RI (2000) Comparative kinetics and response to the benzodiazepine agonists triazolam and zolpidem: evaluation of sex-dependent differences. J Pharmacol Exp Ther 293:435–443
Abernethy DR, Greenblatt DJ, Divoll D, Moschitto LJ, Harmatz JS, Shader RI (1983) Interaction of cimetidine with the triazolobenzodiazepines alprazolam and triazolam. Psychopharmacology 80:275–278
Watts G (2012) Why the exclusion of older people from clinical research must stop. BMJ 344:1–3
Gervasoni C, Meraviglia P, Landonio S, Riva A, Galli M, Rizzardini G, Cattaneo D (2013) Tenofovir plasma concentrations in post-menopausal versus pre-menopausal HIV-infected women. J Antimicrob Chemother 68:1206–1207
Cottrell ML, Patterson KB, Prince HM, Jones A, White N, Wang R, Kashuba AD (2015) Effect of HIV infection and menopause status on raltegravir pharmacokinetics in the blood and genital tract. Antivir Ther 20:795
Nazir S, Iqbal Z, Nasir F (2016) Impact of menopause on pharmacokinetics of rosuvastatin compared with premenopausal women. Eur J Drug Metab Pharmacokinet 41:505–509
Harris RZ, Tsunoda SM, Mroczkowski P, Wong H, Benet LZ (1996) The effects of menopause and hormone replacement therapies on prednisolone and erythromycin pharmacokinetics. Clin Pharmacol Ther 59:429–435
Medicines for Women (2015) Editor Harrison-Woolrych M. Springer International Publishing, Berlin
Rodighiero V (1989) Effects of cardiovascular disease on pharmacokinetics. Cardiovasc Drugs Ther 3:711–730
Rowland Yeo K, Aarabi M, Jamei M, Rostami-Hodjegan A (2011) Modeling and predicting drug pharmacokinetics in patients with renal impairment. Expert Rev Clin Pharmacol 4:261–274
Watson S, Caster O, Rochon PA, den Ruijter H (2019) Reported adverse drug reactions in women and men: aggregated evidence from globally collected individual case reports during half a century. EClinicalMedicine. 17:100188
Martin RM, Biswas PN, Freemantle SN, Pearce GL, Mann RD (1998) Age and sex distribution of suspected adverse drug reactions to newly marketed drugs in general practice in England: analysis of 48 cohort studies. Br J Clin Pharmacol 46:505–511
Pouyanne P, Haramburu F, Imbs JL, Bégaud B (2000) Admissions to hospital caused by adverse drug reactions: cross sectional incidence study. BMJ 320:1036
Naidoo P, Chetty M (2019) Progress in the consideration of possible sex differences in drug interaction studies. Curr Drug Metab 20:114–123
Funding
The study was financially supported by the Swiss National Science Foundation (Grant no. 166204), the OPO Foundation, and the Isaac Dreyfus Foundation.
Author information
Authors and Affiliations
Contributions
Designed research: FS and CM; acquisition of data: FS and CM; performed research: FS; analysis and interpretation of data: FS and CM; drafting of the manuscript: FS and CM.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has a conflict of interest to declare.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Stader, F., Marzolini, C. Sex-related pharmacokinetic differences with aging. Eur Geriatr Med 13, 559–565 (2022). https://doi.org/10.1007/s41999-021-00587-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00587-0