Key Summary Points
To determine adding lactate to SOFA and qSOFA score improves the performance of the predicting mortailty of older patients.
AbstractSection FindingsCut-off value for lactate was 2.3 mmol/L in our ROC analyses. The lactate 2.3 mmol/L threshold-based SOFA-Lactate2.3 and qSOFA-Lactate2.3 scores performs better than standard SOFA and qSOFA identifying hospital mortality risks of patients over 65 who are admitted to the ICU.
AbstractSection MessageLactate value in olders critically ill patients may predict mortality alone and with other scores.
Abstract
Aim
The aim of this study was to determine whether the addition of the lactate level to the SOFA score (SOFA-Laktat) and qSOFA Score (qSOFA-Laktat) improves the performance of the SOFA score and qSOFA score alone in predicting the hospital mortality of critically ill older patients.
Material and method
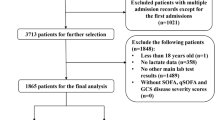
A total of 799 patients over 65 years of age admitted to Emergency Department and hospitalized to intensive care unit (ICU) of our hospital between May 1, 2016, and April 30, 2017, were included in this study. The parameters gender, age, initial complaint, duration of time between the start of their complaint and emergency admission, comorbidities, SOFA scores, qSOFA scores, arterial lactate (AL) values and reason for acute admission, which intensive care unit admitted to, length of stay and patients outcomes (discharge, exitus) were recorded. The primary outcome was to evaluate whether the addition of the evaluation of AL value increased the performance of the SOFA score and qSOFA score in predicting hospital mortality.
Results
Data of 799 patients were analyzed, in which 52.8% (n = 422) were male and 47.3% (n = 377) were female. Most frequently hospitalized clinic was coronary ICU (34.7%, n = 277). Mean duration of hospitalization was 5.2 ± 8.7 days. Hospitalization was prolonged with increased lactate, SOFA and qSOFA levels. Cutoff value for lactate was 2.3 mmol/L in our ROC analyses. Predictive value of SOFA-Lactate2.3 for mortality was significantly higher than SOFA score (p < 0.001). Also, predictive value of qSOFA-Lactate2.3 for mortality was significantly higher than qSOFA score (p < 0.001).
Conclusion
The lactate 2.3 mmol/L threshold-based SOFA-Lactate2.3 and qSOFA-Lactate2.3 scores perform better than SOFA and qSOFA alone in identifying hospital mortality risks of patients over 65 who are admitted to the ICU.



Similar content being viewed by others
References
Topeli A (2000) Elderly patient in the intensive care unit. Turk J Geriatr 3(4):151–154
Sanders AB (1992) Care of the elderly in emergency departments: conclusion and recommendations. Ann Emerg Med 21:8304
Ghosh R, Pepe P (2009) The critical care cascade: a systems approach. Curr Opin Crit Care 15(4):279–283
Gunning K, Rowan K (1999) ABC of intensive care: outcome data and scoring systems. BMJ Br Med J 319(7204):241–244
Kizilarslanoglu MC, Civelek R, Kilic MK, Sumer F, Varan HD, Kara O, Arik G, Turkoglu, Aygencel G, Ulger Z (2017) Is frailty a prognostic factor for critically ill elderly patients? Aging Clin Exp Res 29(2):247–255
Vincent JL, Moreno R, Takala J et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22(7):707–710
Moreno R et al (1999) The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multicentre study. Intensive Care Med 25(7):686–696
Vincent JL et al (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Crit Care Med 26(11):1793–1800
Singer M et al (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315(8):801–810
Seymour CW, Liu VX, Iwashyna TJ et al (2016) Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):762–774
Rhodes A et al (2017) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 43(3):304–377
Neville AL, Nemtsev D, Manasrah R, Bricker SD, Putnam BA (2011) Mortality risk stratification in elderly trauma patients based on initial arterial lactate and base deficit levels. Am Surg 77(10):1337–1341
Jansen TC, van Bommel J, Mulder PG, Rommes JH, Schieveld SJM, Bakker J (2008) The prognostic value of blood lactate levels relative to that of vital signs in the prehospital setting: a pilot study. Crit Care 12(6):1–7
MedCalc Statistical Software version 18.11.3 (2019) MedCalc Software bvba, Ostend, Belgium. https://www.medcalc.org. Accessed 02 Mar 2019
Herring AA et al (2013) Increasing critical care admissions from U.S. emergency departments, 2001–2009. Crit Care Med 41(5):1197–1204
Karabıyık L (2010) Intensive care scoring systems. J Intensive Care Med 9(3):129–143
Lankoandé M, Bonkoungou P, Simporé A, Somda G, Kabore RAF (2018) Inhospital outcome of elderly patients in an intensive care unit in a Sub-Saharan hospital. BMC Anesthesiol 18(118):2–6
Uysal N et al (2010) Prognosis of patients in a medical intensive care unit of a tertiary care centre. J Intensive Care Med 1(1):1–5
Angus DC, Van Der Poll T (2013) Severe sepsis and septic shock. N Engl J Med 369(9):840–851
Mouncey PR et al (2015) Trial of early, goal-directed resuscitation for septic shock. N Engl J Med 372(14):1301–1311
Duke GJ et al (2013) Development and validation of the critical care outcome prediction equation, version 4. Crit Care Resusc 15(3):191–197
Solligård E, Damås JK (2017) SOFA criteria predict infection-related in-hospital mortality in ICU patients better than SIRS criteria and the qSOFA score. Evid Based Med 22(6):211–211
Shapiro NI et al (2005) Serum lactate as a predictor of mortality in emergency department patients with infection. Ann Emerg Med 45(5):524–528
Rabello Filho R, Rocha LL, Corrêa TD, Pessoa CMS, Colombo G, Assuncao MSC (2016) Blood lactate levels cutoff and mortality prediction in sepsis—time for a reappraisal? A retrospective cohort study. Shock (Augusta GA) 46(5):480–485
Kruse O, Grunnet N, Barfod C (2011) Blood lactate as a predictor for in-hospital mortality in patients admitted acutely to hospital: a systematic review. Scand J Trauma Resusc Emerg Med 19(1):74
Guirgis FW et al (2017) Development of a simple sequential organ failure assessment score for risk assessment of emergency department patients with sepsis. J Intens Care Med. https://doi.org/10.1177/0885066617741284
Shetty A et al (2017) Lactate ≥ 2 mmol/L plus qSOFA improves utility over qSOFA alone in emergency department patients presenting with suspected sepsis. Emerg Med Australas 29(6):626–634
Ho KM, Lan NS (2017) Combining quick Sequential Organ Failure Assessment with plasma lactate concentration is comparable to standard Sequential Organ Failure Assessment score in predicting mortality of patients with and without suspected infection. J Crit Care 38:1–5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interests to declare.
Ethical approval
This study started after obtaining ethics approval from the T.C. The Ministiry of Health, Health Sciences University Adana Numune Training and Research Hospital Scientific Research Evaluation Commission.
Informed consent
The patients were included in the study after taken informed consent from the patients’ relatives if not possible to take it from the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aksu, A., Gulen, M., Avci, A. et al. Adding lactate to SOFA and qSOFA scores predicts in-hospital mortality better in older patients in critical care. Eur Geriatr Med 10, 445–453 (2019). https://doi.org/10.1007/s41999-019-00179-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-019-00179-z