Abstract
Background
Constraint-induced movement therapy (CIMT) is a recommended intervention for improving arm recovery following stroke and traumatic brain injury; however, delivery in practice remains rare.
Purpose
The aim of this study was to investigate the costs and cost effectiveness of CIMT delivery, and the use of a CIMT implementation package designed to improve CIMT uptake and delivery by therapists in Sydney, Australia.
Methods
This economic evaluation was conducted with a subset of CIMT programmes (n = 20) delivered by neurological rehabilitation teams at five varied hospitals within a mixed methods implementation study (ACTIveARM). The costs of delivering the CIMT implementation package and publicly funded CIMT were calculated using a bottom-up approach. A cost-effectiveness analysis was conducted, using decision analytic modelling. We compared the uptake and outcomes of people who received CIMT from health services that had received a CIMT implementation package, with those receiving standard upper limb therapy. An Australian health care system perspective was used in the model, over a 3-week time horizon (the average timeframe of a CIMT programme). All costs were calculated in Australian dollars (AUD). Inputs were derived from the ACTIveARM study and relevant literature. The Action Research Arm Test was used to measure arm outcomes. Sensitivity analyses assessed the impact of improving CIMT uptake, scale-up of the implementation package and resource adjustment, including a ‘best-case’ scenario analysis.
Results
The total cost of delivering the implementation package to nine teams across five hospitals was $110,336.43 AUD over 18 months. The mean cost of delivering an individual CIMT programme was $1233.38 AUD per participant, and $936.03 AUD per participant for group-based programmes. The incremental cost-effectiveness ratio (ICER) of individual CIMT programmes was $8052 AUD per additional person achieving meaningful improvement in arm function, and $6045 AUD for group-based CIMT. The ICER was most sensitive to reductions in staffing costs. In the ‘best-case’ scenario, the ICER for both individual and group-based CIMT was $245 AUD per additional person gaining a meaningful change in function.
Conclusion
Therapists improved CIMT uptake and delivery with the support of an implementation package, however cost effectiveness was unclear.
Clinical Trial Registration
https://anzctr.org.au/Trial ID: ACTRN12617001147370.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Constraint-induced movement therapy (CIMT) is an evidence based, clinically effective and recommended intervention for arm recovery after stroke and traumatic brain injury. CIMT is a time-intensive and complex intervention, which has limited its translation into practice. |
With investment in training and support to allied health staff, CIMT can be implemented into acute, rehabilitation, inpatient and outpatient public health services and results in important improvements in arm function for patients. |
This is one of the first studies to examine the costs and cost effectiveness of CIMT when delivered with implementation support. Our findings suggest that, in the best-case scenario, when therapists are supported to provide best-practice CIMT within usual care it likely represents good value for money. |
1 Introduction
Stroke is a leading cause of long-term disability, with around 40% of Australian stroke survivors experiencing disability impacting their independence with daily activities [1, 2]. Arm impairment is common after stroke and traumatic brain injury (TBI). Approximately two-thirds of stroke survivors experience arm impairment affecting their function [3]. Stroke and TBI also have a large economic impact. The estimated Australian healthcare expenditure for stroke was over $606 million Australian dollars (AUD, $1 AUD = $0.78 USD 1 June 2021 [4]) between 2008 and 2009, accounting for 0.5% of total healthcare expenditure nationwide ($113.6 billion AUD) [1]. Similarly, the lifetime costs associated with TBI are high. Lifetime costs per person who sustains a TBI have been estimated to be $2.5 million AUD per person with moderate TBI and $4.8 million AUD per person with severe TBI [5].
Whilst there are published studies exploring the cost effectiveness of models of stroke care [6] and the introduction or scale up of acute stroke interventions [7,8,9,10,11], there has been limited exploration of the cost effectiveness of stroke and acquired brain injury rehabilitation interventions. Stroke rehabilitation costs around $150 million AUD per year in Australia, forming the largest component of first-year costs post-stroke, at almost 30% [12]. Healthcare costs in Australia for moderate and severe TBI have been estimated at $269.1 million AUD and $308.0 million AUD, respectively, with substantial costs also associated with long-term care ($962.5 million AUD for severe TBI) and productivity losses ($256.3 million AUD) [5]. Considering these significant costs, investigation of the costs and cost effectiveness of rehabilitation interventions are needed. Additionally, there has been limited exploration of the costs and cost effectiveness of providing clinicians with support to implement evidence-based interventions into practice, which is vital to improve the long-term outcomes for stroke survivors [13] and people with TBI.
Constraint-induced movement therapy (CIMT) is a highly effective intervention for arm recovery after stroke [14] and has also been demonstrated to improve arm function after TBI [15,16,17]. CIMT comprises three core components: a high intensity, task-specific retraining programme using the affected arm, a restraint (mitt) worn on the non-affected hand encouraging use of the affected hand, and a transfer package comprising behaviour change strategies to encourage generalisation of skills into daily life [18]. CIMT has evolved over time, with different models of CIMT delivery described in the literature, varying in intensity, duration and restraint-wearing time [14]. CIMT is recommended as an intervention for eligible stroke survivors and people with brain injury in the Australian stroke guidelines [19], and clinical practice guidelines for acquired brain injury internationally [20, 21], yet routine delivery of CIMT is rare. A recent national audit indicated that only 12% of eligible Australian stroke survivors received CIMT during their rehabilitation [22]. Barriers to implementing CIMT have been explored in several studies [23,24,25,26] where therapists identified a perceived lack of knowledge and skills, insufficient support from colleagues and lack of time and resources as key barriers. Another barrier to CIMT implementation are the costs associated with delivering the intervention. In Australia, CIMT has primarily been offered by private practitioners at a significant out-of-pocket expense to the patient of between $5000 and $10,000 AUD for a 2-week programme with limited reimbursement options via private health insurance or government funding. Similarly, in the United States of America (USA) the structure of reimbursement for interventions via health insurance often does not support the intensive model of CIMT [18], preventing access to funding support for eligible people to receive the intervention.
Research investigating the costs and cost effectiveness of CIMT is limited. A cost-impact analysis conducted in the Ontario Health Service, Canada, calculated the costs of CIMT in addition to usual upper limb rehabilitation. Usual upper limb rehabilitation was calculated at 30 minutes per day, 5 days per week [27]. CIMT costs were based on a range of six treatment options, including variations in programme duration (10 days vs 15 days), and therapy time (total therapy range 30–52.5 h) [27]. They found CIMT cost was between $884 and $1857 Canadian dollars (CAD) per stroke survivor when combined with usual care, compared with $177 CAD for usual upper limb care alone [13]. This equates to between $0.59 million and $1.22 million CAD additional costs if all eligible stroke survivors in Ontario received CIMT in 2011. In the United Kingdom, a systematic review that included modelling of resource use, costs and effectiveness for repetitive functional task practice found that this therapy, which included CIMT, was cost effective, with an incremental cost-effectiveness ratio (ICER) of £10,870 GBP per quality-adjusted life-year (QALY) [28]. Research on the cost effectiveness of CIMT from the societal viewpoint has also been limited. One retrospective study of participants who had received CIMT in the USA (n = 121) found that after the CIMT programme, some participants’ caregivers were able to resume employment, even though the CIMT participants themselves may have retired from the workforce [29].
To date, the costs and cost effectiveness of supporting therapists to implement CIMT in routine practice have not been explored. Similarly, there is limited evidence on the costs and cost effectiveness of CIMT delivery, particularly in the Australian context. Our aim was to investigate the costs and cost effectiveness of a CIMT implementation support package provided to therapists treating adults with arm impairment after stroke or TBI, and the costs of CIMT programme delivery.
The objectives were to estimate
-
1.
The costs of delivering a CIMT implementation support package.
-
2.
The costs of delivering CIMT (either individual or group-based) at a service level within a public health setting.
-
3.
The cost effectiveness of a CIMT implementation support package in terms of the arm recovery of stroke survivors and people with TBI.
2 Method
2.1 Design
We conducted a bottom-up costing of an implementation support package and delivery of CIMT in practice. CIMT cost effectiveness was modelled from the Australian health system perspective, as the purpose of the ACTIveARM study was to inform health system policy and improve delivery of CIMT within the health service. The cost-effectiveness model compared the uptake of CIMT in practice following delivery of the implementation package and associated arm outcomes with standard care. This study was embedded within a larger mixed methods implementation study, the ACTIveARM project (Australian Constraint Therapy Implementation study of the ARM) [30].
2.2 The ACTIveARM Implementation Support Package
The ACTIveARM implementation support package targeted behaviour change among physiotherapists, occupational therapists and allied health assistants to increase delivery of CIMT to eligible stroke survivors and people with brain injury. The implementation package included 2-day training workshops, monthly community of practice meetings, onsite support, quarterly audit and feedback to teams about their practice, and poster reminders.
The implementation package was delivered to participating teams between March 2017 and September 2018. The primary outcome for the ACTIveARM project was the proportion of eligible people who were offered, and received, CIMT. CIMT is a suitable intervention for those with mild to moderate upper limb impairment after stroke or TBI. Eligibility for CIMT was determined in accordance with the Australian national clinical guidelines for stroke management [19], which recommends that to be eligible for CIMT, individuals should have some movement in at least two fingers and thumb in the affected hand.
Outcomes were collected using file audits at three baseline timepoints (T1–T3) prior to delivery of the implementation package, and then quarterly for 18 months during the supported implementation period (T4–T9). The final audit and feedback cycle was 6 months after withdrawal of the implementation package (T10). Secondary outcomes relating to CIMT participants’ arm function were collected pre-CIMT, post-CIMT and 4 weeks after programme completion. Arm outcomes were measured using the Action Research Arm Test (ARAT) [31], Canadian Occupational Performance Measure [32], Nine Hole Peg Test [33], Box and Block Test [34], and Motor Activity Log [35].
Each team in the ACTIveARM project implemented a locally tailored model of CIMT service that maintained the three core components of CIMT. CIMT was delivered using either a one therapist/one participant model (individual) or group therapy. Programmes were delivered either 5 days/week for 2 weeks or 3 days/week for 3 weeks as a range of CIMT protocols have been demonstrated to achieve efficacious outcomes [14, 36,37,38].
2.3 Setting
The study was conducted within the public healthcare system of South Western Sydney Local Health District, Australia. This District is one of the largest in New South Wales (NSW), servicing suburban and regional communities [39]. Four acute hospitals and one subacute hospital providing specialist acute and rehabilitation services for people with stroke and TBI participated in the ACTIveARM project. Services included inpatient acute care and subacute care, outpatient and community-based rehabilitation teams. Services are provided under the Australian universal healthcare (Medicare) system at no cost to individuals [40]. Refer to Supplementary Table A in the electronic supplementary material (ESM) for further details regarding participating teams.
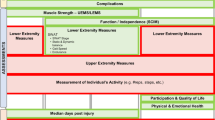
2.4 Model Structure
Our model compared the costs and effectiveness of CIMT against standard care, when CIMT was implemented with the support of an implementation package. We developed a decision tree using Microsoft Excel (Fig. 1) to reflect the relatively simple clinical pathway and short time horizon [41]. The decision tree time horizon was 3 weeks, consistent with the time from determining a person’s eligibility for CIMT to completion of the CIMT programme (maximum 3 weeks) and the duration of standard rehabilitation upper limb therapy (average 2.5 weeks).
2.5 Model Inputs: Costs
Supplementary Table B summarises the parameters used in the model (see ESM). All costs are expressed in 2017–2018 Australian dollars (AUD). Costs of the implementation package and therapist time delivering CIMT were collected using a bottom-up approach. Costs associated with delivery of the implementation package to nine teams across five hospitals, including printing and travel costs, were recorded by the research team. Treating therapists self-reported time spent preparing, delivering and following up CIMT programmes (in minutes) for a subset of CIMT programmes conducted during the ACTIveARM mixed methods implementation study. Information from a subset of 20 CIMT programmes (15 individual and five group programmes) delivered during the ACTIveARM study implementation period (T4-T9) that involved 34 patient participants were collated for therapist inputs. Data were also collected on therapist resource use and equipment (such as restraint mitts). As the implementation package was delivered at the level of the team, and it is unknown in advance which patients will be eligible for CIMT and which will not, implementation package costs were spread across both eligible and ineligible patients, consistent with an implementation science approach and application of training in a real-world setting. Therapy costs associated with CIMT were assigned only to patients who received CIMT.
Therapist costs were based on the salary level of individual staff using the appropriate NSW Health Awards for the relevant financial year [42,43,44,45,46,47]. Resources used for delivery of both the therapist implementation package and CIMT programmes for patient participants were costed using actual purchase prices. As the time horizon for the cost-effectiveness period was < 12 months, neither costs nor outcomes were discounted.
2.6 Model Inputs: Outcomes
2.6.1 CIMT Uptake
CIMT uptake was defined and measured as the proportion of eligible individuals with stroke or TBI who were offered and received CIMT 18 months after delivery of the implementation package (timepoint T9). At this timepoint, 46% of eligible individuals received CIMT (n = 41 people eligible, n = 19 received a CIMT programme). The 18-month uptake rate allowed adequate time for services to deliver multiple CIMT programmes and embed CIMT into routine practice. For the standard care arm of the model, the average pre-implementation baseline delivery of CIMT (2%) was assumed to stay consistent. Refer to Supplementary Table A in the ESM for details of CIMT delivery per team.
2.6.2 CIMT Effectiveness
The primary effectiveness outcome measure in the economic model was the proportion of patients who achieved a clinically meaningful improvement in arm function on the ARAT [48] post-CIMT programme from a sample of 64 CIMT participants (n = 57 stroke survivors [89%], n = 7 TBI survivors [11%]) over the course of the ACTIveARM study. Due to the lack of an established minimal clinically important difference (MCID) for the ARAT in a TBI population, we used the established MCID for acute and chronic stroke populations for both stroke and TBI participants. A clinically meaningful improvement in arm function, or MCID, was defined for the ARAT as an improvement of 12 points or more for individuals in the acute phase of recovery [49], an improvement of 5.7 points or more for individuals in the chronic phase of recovery [50, 51] or achieving the maximum score of 57/57. Tasks completed to achieve the maximum score on the ARAT include being able to pick up a cup and pour water from it, lifting an object to above shoulder height and picking up small objects (including a marble) between the index finger and thumb [48].
2.7 Standard Care
Standard care estimates for the model came from data describing upper limb therapy provided to inpatient stroke survivors and their arm outcomes in a previously published cohort study at one of the ACTIveARM hospital sites [52, 53]. Inpatient stroke survivors at that site completed a mean of two upper limb therapy sessions per week [52]. Approximately half (53%) were reported to achieve either the MCID or the maximum score (57/57) on the ARAT between admission and discharge with standard upper limb rehabilitation [53]. CIMT was not routinely offered at this hospital site at the time these data were collected.
2.8 Incremental Cost-Effectiveness Ratios (ICER)
ICERs were calculated as the additional costs required for an additional person to achieve a clinically meaningful improvement in arm function (measured as achieving the MCID or maximum score on the ARAT) after completing CIMT compared with standard care. An ICER was calculated for CIMT delivered as an individual programme, CIMT delivered as a group-based programme, and CIMT individual and group programmes combined by using the average costs of individual and group programmes.
Because there is no standard accepted threshold for the value of achieving the MCID on the ARAT, we are unable to define at what ICER the intervention is deemed cost effective within the Australian public health care setting; however, we have calculated confidence intervals (CIs) around the ICER and present a cost-effectiveness acceptability curve (CEAC) to aid interpretation.
2.9 Sensitivity Analysis: One-Way Sensitivity Analysis and Scenario Analysis
One-way sensitivity analyses were conducted to understand the impact of different parameter assumptions on the baseline ICER, with results presented in a tornado plot. We investigated:
-
(a)
Varying uptake of CIMT within a health service. This analysis was conducted in three ways. First, an attainable and objective benchmark was established using the Achievable Benchmark of Care (ABC) method [54]. Using this methodology, we ranked the nine ACTIveARM teams in relation to their delivery of CIMT, adjusting for teams with small patient numbers. Based on this, uptake for the sensitivity analysis was set at 58% of eligible people receiving CIMT. Second, we considered it realistic for health services to set a goal of offering CIMT to all eligible patients (i.e. 100%), since CIMT is the only upper limb intervention that is strongly recommended in the Australian stroke guidelines [13]. Assuming some patients may decline CIMT due to personal preference, we set uptake as 80% of eligible people receiving CIMT. Finally, we considered that following withdrawal of the implementation package, therapists may reduce their delivery of CIMT by 50% without the availability of support. We therefore reduced the proportion of eligible people who received a CIMT programme to 21%.
-
(b)
Implementation package delivered at scale We assumed the CIMT implementation package would be scaled up and delivered across other health districts (for example, as part of a state-wide rollout). For this we only included ongoing implementation package costs and costs of CIMT delivery. Costs such as production of training videos and development of workshop materials were excluded as they had already been prepared. Costs included provision of two training workshops per health district, one day of onsite support during each team’s first CIMT programme, and monthly CIMT community of practice teleconferences for 12 months.
-
(c)
Varying resourcing costs In the base-case scenario, resourcing (i.e. staffing) costs are estimated as additional to existing time spent delivering standard upper limb therapy. However, as no additional staff were employed to run CIMT, and staff workloads were adjusted to accommodate CIMT, we conducted a sensitivity analysis to assume no opportunity cost when staff delivered CIMT instead of standard therapy (i.e. staff integrated CIMT into their usual work practices). We therefore only included the additional costs of the implementation package (e.g. training workshops) to support therapists to initially implement then sustain CIMT programmes over time, along with resource costs such as assessment kits. We also explored the impact on outcomes if costs to deliver CIMT and the implementation package had been underestimated and costs were to increase by 30%.
Finally, we also conducted a scenario-based sensitivity analysis. We developed a ‘best-case’ scenario for each assumption in the model, based on the literature and experience in the ACTIveARM study. In this best-case scenario, we assumed 80% of people who were eligible for CIMT received CIMT (as some eligible people may decline CIMT based on personal preferences), that 67% of those who completed CIMT achieved a MCID or full score on the ARAT (based on patient outcome data from the ACTIveARM study), and that only the additional costs of the implementation package were paid for by the health service, with staff time reallocated from existing resources and therefore no costs associated with staff time.
2.10 Stochastic Sensitivity Analysis
As the ICER is a ratio and cost data is typically skewed, non-parametric methods are required to calculate confidence intervals for the ICER [55]. We used non-parametric bootstrap, where repeated random samples from the ACTIveARM CIMT population, of the same size as the original sample (n = 64), were taken from 1000 replications. We present the bootstrapped CI along with the cost-effectiveness plane [56] for the bootstrapped cost-effectiveness pairs for the base-case analysis.
Given the uncertainty around willingness to pay for improvements in upper limb function, we also present the bootstrapped cost-effectiveness results as a CEAC [55]. This displays the probability of cost effectiveness at thresholds between $0 and $50,000 per additional participant achieving either the MCID or maximum score on the ARAT, and we report the probabilities for the threshold values of the average daily cost ($1701 AUD) and the average total cost ($10,890 AUD) of a hospital admission for a stroke with intermediate complexity [57] to illustrate interpretation of the graph.
3 Results
3.1 Costs of Delivering a CIMT Implementation Package
Supplementary Table B shows the various costs of delivering the CIMT implementation package. The total cost of the implementation package when delivered to therapists across nine teams was $110,336.43 AUD. This equates to $98.08 AUD per person that was potentially eligible to receive CIMT during the ACTIveARM study (n = 1125).
3.2 Costs of Delivering a CIMT Programme
The mean cost of delivering an individual CIMT programme was $1233.38 AUD per participant, and the group format was $936.03 AUD per participant compared with $263.70 AUD for standard therapy (see Table 1). The mean time spent by therapists preparing for, delivering then providing follow-up after an individual CIMT programme was 33.5 h per participant (range 13.1–61.9 h), and 24.6 h per participant when delivered in a group (range 5.7–53.0 h) (see Table 1).
3.3 The Cost-Effectiveness of a CIMT Implementation Package in Terms of Arm Recovery
Sixty-seven percent of people who received a CIMT programme achieved the MCID or full marks on the ARAT compared with 53.1% in the usual care group. Taking into account that not all people who were eligible received CIMT and assuming equal effectiveness of group and individual therapy, overall effectiveness was 59.6% for people who were eligible for CIMT (incremental effect 6.5%). Similarly, total costs, accounting for uptake, used in the cost-effectiveness analysis were $811.14 AUD for individual CIMT and $673.34 AUD for group CIMT in the intervention arm, compared with $286.39 AUD for individual therapy and to $279.43 AUD for group therapy in the standard care arm (incremental cost for individual CIMT = $524.75 AUD; group CIMT = $393.91 AUD).
The ICER equated to a cost of $8052 AUD for individual CIMT, $6045 AUD for group-based CIMT, and $7048.39 AUD for combined individual and group CIMT per additional person gaining a meaningful change in arm function as measured by the ARAT (See Table 2).
3.4 Sensitivity Analyses: One-Way and Scenario Analyses
Results of the one-way sensitivity analyses are presented in Fig. 2. All results relate to outcomes per person achieving meaningful change in arm function. Increasing the delivery of CIMT within a health service from 46% of eligible people to the ABC-derived benchmark level of 58% had almost no impact on cost effectiveness ($7819 AUD for individual CIMT and $5789 AUD for group-based CIMT). Further increasing the delivery and uptake of CIMT to 80% of eligible people also had only a small impact on cost effectiveness ($7566 AUD for individual CIMT and $5513 AUD for group-based CIMT). Reducing the delivery and uptake of CIMT in a pessimistic scenario to 21% of eligible people increased the ICER by 56% for individual CIMT programmes ($9448 AUD) and by 25% for group CIMT ($7569 AUD).
Adjustment to the delivery of the implementation package at scale had a small impact on the ICER ($6735 AUD for individual CIMT and $4727 AUD for group-based CIMT). An increase in CIMT programme costs by 30% reduced cost effectiveness ($11,653 AUD for individual CIMT and $9043 AUD for group-based CIMT).
When we assumed that the cost of staff time to deliver CIMT instead of standard therapy was covered by existing resources, this resulted in a large improvement in cost effectiveness, with an ICER of $1505 AUD for both individual (− 81%) and group-based CIMT (− 75%).
The ICER for the best-case scenario model was $245 AUD per additional person gaining a meaningful improvement in their arm function.
3.5 Stochastic Sensitivity Analyses
Stochastic sensitivity analysis found that the bootstrap replications of the baseline ICER fell between $1376.17 AUD per additional person (lower limit of the 95% CI; north-east sector of the cost-effectiveness plane), and − $17,536.41 AUD per additional person (upper limit of the 95% CI; north-west sector of the cost-effectiveness plane) with meaningful change when group and individual therapy were combined (see Fig. 3). The 5.4% fraction of the bootstrap replications falling in the north-west quadrant of the cost-effectiveness plane (incremental cost > 0; incremental effectiveness < 0; negative ICER) suggests that CIMT when delivered with the implementation package may be dominated by usual care.
The CEAC (Fig. 4) displays the probability that CIMT implementation is cost effective at a range of willingness to pay (WTP) thresholds. With a WTP threshold of $1 AUD there is a 0.2% probability that CIMT will be cost effective, while at a $50,000 AUD threshold the probability of CIMT being cost effective is 93.7%. Using hospitalisation costs for stroke with intermediate complexity as further proxies for WTP thresholds, we see that at the average daily cost of admission ($1703 AUD [57]), the probability of CIMT being cost effective is 10%, while at the average total cost of admission ($10,890 AUD [57]), the probability of CIMT being cost effective is 88.4%.
Bootstrapped cost-effectiveness acceptability curve (CEAC) showing probability of CIMT (with individual and group therapy combined) being cost effective at varying willingness-to-pay (WTP) thresholds from 0 to 50,000 per additional person achieving meaningful improvement in arm function. Costs in Australian dollars. CIMT constraint-induced movement therapy
4 Discussion
The implementation package resulted in increased delivery of CIMT in practice, and there were improved arm outcomes for CIMT participants when compared with the outcomes achieved from standard upper limb therapy. Our findings suggest that CIMT programmes have lower delivery costs in the Australian context compared with similar programmes delivered in Canada [27] and the United Kingdom [28], despite these programmes not including implementation support. The Canadian study only estimated therapist costs and used an average therapist pay to calculate costs whilst the United Kingdom study allocated some costs for staff training (up to 20 hours of therapist time per study), average equipment costs (£100 GBP per CIMT participant) and average therapist costs (£40 per therapist per hour) (UK results are based on 2005/06 prices).
While there is no established threshold to determine value for money in relation to arm function, the ICERs for individual ($8052 AUD) CIMT and to a lesser extent group-based CIMT ($6045 AUD) could be considered poor value for money when planning to deliver the CIMT implementation package and introducing CIMT into routine practice, and there is a 5% chance that it could be more expensive and less effective. However, our best-case scenario was developed based on realistic targets consistent with benchmarking literature [54] and reflective of clinical practice in the real world, and suggests that when therapists, within their existing roles, are supported to achieve best-practice rates of CIMT uptake (80%) and arm outcomes, the cost per person achieving meaningful improvement reduces significantly to $245 AUD. This suggests that supporting best-practice implementation of CIMT in the Australian health care system is achievable and may represent good value for money when compared with standard care, particularly when the average daily cost of a stroke hospital admission currently ranges from $1701 to $2106 AUD per day [57].
This study has implications for public health policy managers and health services with regard to resource allocation, which are outlined in the following sections.
4.1 Implications for Clinical Practice
In Australia, the average length of stay within inpatient stroke rehabilitation continues to fall (national average 22 days in 2018 [22] versus 26 days in 2015–2016 [2]). A shorter length of stay results in challenges with allocation of limited resources. Care is often transferred to outpatient rehabilitation where patients usually receive low-intensity individual upper limb therapy, on a weekly or fortnightly basis, for several weeks or months. We found that CIMT delivered as an individual or group-based programme resulted in worthwhile and meaningful improvements in arm function within 2–3 weeks. Our research suggests that around one third of the approximately 40,000 acute care hospitalisations with a principal diagnosis of stroke in Australia annually [58] are eligible for CIMT, and only 11% of eligible stroke survivors receive CIMT during their rehabilitation [59]. This indicates that over 10,000 Australians are missing out on this evidence-based intervention, which our research demonstrates can be successfully implemented in clinical practice [30] and may be cost effective. Considering the cost of CIMT delivery in the context of daily inpatient rehabilitation costs, CIMT is an attractive alternative to standard care. These intensive programmes lead to improvements in arm function in a shorter time, reducing service use and perhaps also reducing informal carer burden, which may improve the cost effectiveness of rehabilitation.
Furthermore, the use of technology for telehealth enables alternative modes of CIMT delivery, with further opportunities to improve cost effectiveness. In the current study, CIMT was predominantly delivered in person, with costs incurred for therapy time and therapist travel for follow-up. CIMT delivered via telehealth may reduce resource demands, improve programme uptake and reach to patients, thereby reducing overall costs. A few studies have demonstrated promising outcomes for arm recovery when CIMT is delivered via telehealth [60, 61] or online platforms [62, 63]. However, these studies have several limitations including small sample sizes and risk of bias associated with the methods used. Therefore, further research is required, evaluating both the efficacy and cost effectiveness of CIMT when delivered via remote methods.
4.2 Implications for Service Delivery and Policy
With investment in implementation support, we have demonstrated that CIMT can be implemented in acute, rehabilitation, inpatient and outpatient settings [30]. The modest cost of the CIMT implementation package, when delivered at scale, provides a model for applying these implementation strategies in practice. Furthermore, the costs associated with supporting CIMT implementation including staff education could be further reduced if CIMT training was provided as a standard part of the curriculum in occupational therapy and physiotherapy training programmes. This would reduce the need for site-specific training and education, with only booster training sessions needed to accommodate staffing changes.
Studies in acute stroke care have suggested that reducing evidence–practice gaps can have positive economic benefits [7]; however, few studies have explored the cost effectiveness of recommended rehabilitation interventions [64,65,66]. Challenges associated with evaluating the cost effectiveness of rehabilitation interventions such as CIMT include the complexity of the intervention and the significant variation in how outcomes are measured across services [67]. In this study, we focused on costing arm recovery. Future economic evaluations of CIMT should use a standardised approach to economic evaluations [64], including the use of measures to evaluate the impact of CIMT on level of disability (e.g. the modified Rankin Scale) [68] and quality of life (e.g. the EQ-5D) [69] in addition to the collection of measures of arm function, the primary area targeted by CIMT. Evaluation that incorporates outcome measures that can be expressed in QALYs would allow cost-utility analysis and comparison with established thresholds for assessment of cost effectiveness [41] and comparison across different interventions and areas of healthcare. Alternatively, discrete choice experiment methods to identify the WTP for gains in arm function would allow a threshold for cost effectiveness to be determined [70].
4.3 Implications for Future Research
Despite a large improvement in the proportion of people offered, then receiving CIMT, about half of the people offered CIMT in this study declined or did not receive a programme. To date, there has been limited research exploring the acceptability of CIMT from the stroke or brain injury survivor’s perspective [71,72,73]. It is well established that when patient preferences for treatment are taken into account, uptake and compliance improves, leading to better health outcomes [74] and improving cost effectiveness. Further research in relation to CIMT implementation should therefore focus on exploring factors that influence the reach and uptake of CIMT by the target population.
4.4 Strengths and Limitations
Our study collected detailed data on the real-world costs associated with CIMT delivery in a public health setting, including staff time and resource use. We measured practice before and after delivery of the CIMT implementation package. Over 1500 files were audited across 10 time points and nine teams. We therefore feel confident that our assumptions within the model for the effectiveness of the CIMT implementation package are an accurate representation of the package’s influence on practice change.
Despite these strengths, there are always some study limitations. We discuss above the limitations of our outcome measure of cost per person with improved arm function. Without a formal WTP threshold there is no clear recommendation regarding the cost effectiveness of CIMT. However, as the first examination of the cost effectiveness of CIMT, this work provides a valuable platform for future research on the cost effectiveness and cost utility of CIMT and other upper-limb therapy approaches.
Economic models represent a simplified version of reality. Several assumptions have been made within the model that may not reflect practice, particularly in relation to standard care estimates. Firstly, the ‘no implementation package’ arm of our decision analytic tree included CIMT delivery outcomes that were collected from the study sites at earlier time points, prior to the introduction of the implementation package. Secondly, participant outcomes used in the standard care group were calculated from the literature, using data collected between 2011 and 2013, and without specific information on eligibility of CIMT available. These estimates therefore may not reflect current standard care. However, as the standard care outcomes used were from a study site where the implementation package was later delivered, we believe they are representative of standard care within the health district.
Another limitation of the study is that we did not test the hypothesis that there may be diminishing returns in the effectiveness of CIMT when CIMT is expanded to a larger patient population during scale up of the implementation package. Whilst expanding scale up of CIMT implementation might result in economies of scale in terms of costs of providing CIMT, scale up of CIMT implementation may also result in changes or reductions in average efficacy of CIMT.
We used a short time horizon within the model, consistent with the duration of a CIMT programme. This may have resulted in truncation of CIMT outcomes or costs, and potentially biased estimates of CIMT cost effectiveness [75].
Due to the small number of people with TBI included within the sample (n = 7, 11%) there is some uncertainty in the results for this patient population. Finally, self-reported data from therapists were used to calculate resource use and time spent completing CIMT activities. Self-reported data may have resulted in under or overestimates of actual time needed to complete CIMT activities.
5 Conclusion
CIMT uptake and delivery improved with implementation support, with observed improvements in arm function for people with stroke and TBI. This economic model demonstrates that with financial investment to support initial implementation and ongoing training, CIMT results in important improvements in arm function for patients. Although it is difficult to say without an established threshold, the ICERs in this study for individual and group therapy may not represent cost-effective intervention. However, the best-case scenario suggests when therapists are supported to provide best-practice CIMT it likely represents good value for money.
References
Australian Institute of Health and Welfare. Stroke and its management in Australia: an update. Canberra: Australian Institute of Health and Welfare. 2013. https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/stroke-management-australia-update/formats.
Australian Institute of Health and Welfare. Australia's health 2018. Canberra: Australian Institute of Health and Welfare. 2018. https://doi.org/10.25816/5ec1e56f25480.
Kwah L, Harvey L, Diong J, Herbert R. Models containing age and NIHSS predict recovery of ambulation and upper limb function six months after stroke: an observational study. J Physiother. 2013;59(3):189–97.
XE.com Inc. Historical rate tables. 2021. https://www.xe.com/currencytables/?from=AUD&date=2021-06-01#table-section.
Access Economics Pty Limited, Victorian Neurotrauma Initiative. The economic cost of spinal cord injury and traumatic brain injury in Australia: Victorian Neurotrauma Initiative. 2009. http://www.tac.vic.gov.au/about-the-tac/research/research/tac-neurotrauma-research/vni/the20economic20cost20of20spinal20cord20injury20and20traumatic20brain20injury20in20australia.pdf.
Tam A, Mac S, Isaranuwatchai W, Bayley M. Cost-effectiveness of a high-intensity rapid access outpatient stroke rehabilitation program. Int J Rehabil Res. 2019;42(1):56–62.
Kim J, Andrew NE, Thrift AG, Bernhardt J, Lindley RI, Cadilhac DA. The potential health and economic impact of improving stroke care standards for Australia. Int J Stroke. 2017;12(8):875–85.
Marquina C, Ademi Z, Zomer E, Ofori-Asenso R, Tate R, Liew D. Cost burden and cost-effective analysis of the Nationwide Implementation of the quality in acute stroke care protocol in Australia. J Stroke Cerebrovasc Dis. 2021;30(8):105931.
Kim J, Easton D, Zhao H, Coote S, Sookram G, Smith K, et al. Economic evaluation of the Melbourne Mobile Stroke Unit. Int J Stroke. 2020;16(4):466–75.
Reeves P, Edmunds K, Levi C, Lin L, Cheng X, Aviv R, et al. Cost-effectiveness of targeted thrombolytic therapy for stroke patients using multi-modal CT compared to usual practice. PLoS ONE. 2018;13(10):e0206203.
Sevick LK, Ghali S, Hill MD, Danthurebandara V, Lorenzetti DL, Noseworthy T, et al. Systematic review of the cost and cost-effectiveness of rapid endovascular therapy for acute ischemic stroke. Stroke. 2017;48(9):2519–26.
Dewey HM, Thrift AG, Mihalopoulos C, Carter R, Macdonell RAL, McNeil JJ, et al. Cost of stroke in Australia from a societal perspective. Stroke. 2001;32(10):2409–16.
Stroke Foundation. Clinical guidelines for stroke management 2017 Melbourne, Australia. 2017. https://informme.org.au/en/Guidelines/Clinical-Guidelines-for-Stroke-Management-2017.
Kwakkel G, Veerbeek JM, van Wegen EE, Wolf SL. Constraint-induced movement therapy after stroke. Lancet Neurol. 2015;14(2):224–34.
Shaw SE, Morris D, Uswatte G, McKay S, Meythaler JM, Taub E. Constraint-induced movement therapy for recovery of upper-limb function following traumatic brain injury. J Rehabil Res Dev. 2005;42(6):769–78.
Page S, Levine P. Forced use after TBI: promoting plasticity and function through practice. Brain Inj. 2003;17(8):675–84.
Cho YW, Jang SH, Lee ZI, Song JC, Lee HK, Lee HY. Effect and appropriate restriction period of constraint-induced movement therapy in hemiparetic patients with brain injury: a brief report. NeuroRehabilitation. 2005;20(2):71–4.
Morris D, Taub E, Mark VW. Constraint-induced movement therapy: characterising the intervention protocol. Eura Medicophys. 2006;42(3):257–68.
Stroke Foundation. Clinical guidelines for stroke management. Melbourne, Australia. 2021. https://informme.org.au/guidelines/clinical-guidelines-for-stroke-management.
Ontario Neurotrauma Foundation. Clinical Practice Guidelines for the Rehabilitation of Adults with Moderate to Severe TBI Ontario, Canada. 2016. https://braininjuryguidelines.org/modtosevere/.
Intercollegiate Stroke Working Party. National clinical guideline for stroke. 5th ed. London: Royal College of Physicians. 2016.
Stroke Foundation. National Stroke Audit-Rehabilitation Services Report 2018. Melbourne, Australia. 2018. https://informme.org.au/media/5omlum0k/rehab_strokeservicesreport_2018.pdf.
Pedlow K, Lennon S, Wilson C. Application of constraint-induced movement therapy in clinical practice: an online survey. Arch Phys Med Rehabil. 2014;95(2):276–82.
Fleet A, Che M, MacKay-Lyons M, MacKenzie D, Page SJ, Eskes G, et al. Examining the use of constraint-induced movement therapy in Canadian neurological occupational and physical therapy. Physiother Can. 2014;66(1):60–71.
Viana R, Teasell R. Barriers to the implementation of constraint-induced movement therapy into practice. Top Stroke Rehabil. 2012;19(2):104–14.
Daniel L, Howard W, Braun D, Page SJ. Opinions of constraint-induced movement therapy among therapists in Southwestern Ohio. Top Stroke Rehabil. 2012;19(3):268–75.
Medical Advisory Secretariat Health Quality Ontario. Constraint-induced movement therapy for rehabilitation of arm dysfunction after stroke in adults: an evidence-based analysis. Ontario Health Technol Assessment Ser. 2011;11(6):1–58.
French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al. A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness. Health Technol Assess. 2008;12(30):iii–117.
Mennemeyer ST, Taub E, Uswatte G, Pearson S. Employment in households with stroke after Constraint-Induced Movement therapy. NeuroRehabilitation. 2006;21(2):157–65.
Christie L, McCluskey A, Lovarini M. Implementation of sustainable publicly funded constraint induced movement therapy (CIMT): The ACTIveARM Project. In: Therapists WFoO, editor. WFOT Congress 2018; Cape Town, South Africa. 2018.
Platz T, Pinkowski C, van Wijck F, Kim I-H, di Bella P, Johnson G. Reliability and validity of arm function assessment with standardized guidelines for the Fugl-Meyer Test, Action Research Arm Test and Box and Block Test: a multicentre study. Clin Rehabil. 2005;19(4):404–11.
Cup EH, Scholte-op-Reimer WJ, Thijssen MC, van Kuyk-Minis MA. Reliability and validity of the Canadian Occupational Performance Measure in stroke patients. Clin Rehabil. 2003;17(4):402–9.
Mathiowetz V, Weber K, Kashman N, Volland G. Adult norms for the nine hole peg test of finger dexterity. Occup Therapy J Res. 1985;5:1.
Mathiowetz V, Volland G, Kashman N, Weber K. Adult norms for the box and blocks test of manual dexterity. Am J Occup Ther. 1985;39(6):386–91.
van der Lee JH, Beckerman H, Knol DL, de Vet HCW, Bouter LM. Clinimetric properties of the Motor Activity Log for the assessment of arm use in hemiparetic patients. Stroke. 2004;35:1410–4.
Lin K, Wu C, Liu J, Chen Y, Hsu C. Constraint-induced therapy versus dose-matched control intervention to improve motor ability, basic/extended daily functions, and quality of life in stroke. Neurorehabil Neural Repair. 2009;23(2):160–5.
Wolf SL, Thompson PA, Winstein CJ, Miller JP, Blanton SR, Nichols-Larsen DS, et al. The EXCITE stroke trial: comparing early and delayed constraint-induced movement therapy. Stroke. 2010;41(10):2309–15.
Dettmers C, Teske U, Hamzei F, Uswatte G, Taub E, Weiller C. Distributed form of constraint-induced movement therapy improves functional outcome and quality of life after stroke. Arch Phys Med Rehabil. 2005;86(2):204–9.
Planning Unit South Western Sydney Local Health District. South West Sydney: our health. In: An in-depth study of the health of the population now and into the future. Liverpool, New South Wales: South Western Sydney Local Health District, South Western Sydney Primary Health Network. 2019.
Australian Government Department of Health. In: The Australian health system. 2019. https://www.health.gov.au/about-us/the-australian-health-system.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes, 4th edition. Oxford: Oxford University Press; 2015.
NSW Ministry of Health. NSW Health Service Professionals (State) Award 2017. Sydney, Australia: Industrial Relations Commission of New South Wales. 2017.
NSW Ministry of Health. NSW Health Service Health Professionals (State) Award 2018. Sydney, Australia: Industrial Relations Commission of New South Wales. 2018.
NSW Ministry of Health. NSW Health Health Employee's (State) Award 2017. Sydney, Australia: Industrial Relations Commission of New South Wales. 2017.
NSW Ministry of Health. NSW Health Health Employees' (State) Award 2018. Sydney, Australia: Industrial Relations Commission of New South Wales. 2018.
NSW Ministry of Health. Increased Rates of Pay and Allowances for Staff in the NSW Health Service—HSU and ASMOF Awards. Sydney, Australia: Industrial Relations Commission of New South Wales. 2018.
NSW Nurses and Midwives' Association. Public Health System Nurses’ and Midwives’ (State) Award 2018. Sydney, Australia: Industrial Relations Commission of New South Wales. 2018.
Lyle RC. A performance test for assessment of upper limb function in physical rehabilitation treatment and research. Int J Rehabil Res. 1981;4(4):483–92.
Lang CE, Edwards DF, Birkenmeier RL, Dromerick AW. Estimating minimal clinically important differences of upper-extremity measures early after stroke. Arch Phys Med Rehabil. 2008;89(9):1693–700.
van der Lee JH, Beckerman H, Lankhorst GJ, Bouter LM. The responsiveness of the Action Research Arm test and the Fugl-Meyer Assessment scale in chronic stroke patients. J Rehabil Med. 2001;33(3):110–3.
Van der Lee JH, De Groot V, Beckerman H, Wagenaar RC, Lankhorst GJ, Bouter LM. The intra- and interrater reliability of the action research arm test: a practical test of upper extremity function in patients with stroke. Arch Phys Med Rehabil. 2001;82(1):14–9.
Vratsistas-Curto A, Sherrington C, McCluskey A. Dosage and predictors of arm practice during inpatient stroke rehabilitation: an inception cohort study. Disabil Rehabil. 2019;2019:1–8.
Vratsistas-Curto A, Sherrington C, McCluskey A. Responsiveness of five measures of arm function in acute stroke rehabilitation. Clin Rehabil. 2018;32(8):1098–107.
Weissman NW, Allison JJ, Kiefe CI, Farmer RM, Weaver MT, Williams OD, et al. Achievable benchmarks of care: the ABCs of benchmarking. J Eval Clin Pract. 1999;5(3):269–81.
Gray A, Clarke PM, Wolstenholme JL, Wordsworth S. Applied methods of cost-effectiveness analysis in healthcare. Oxford: Oxford University Press; 2010.
Black WC. The CE plane: a graphic representation of cost-effectiveness. Med Decis Mak. 1990;10(3):212–4.
Independent Hospital Pricing Authority. National Hospital Cost Data Collection Report: Public Sector, Round 22 (Financial Year 2017-18). 2020. https://www.ihpa.gov.au/publications/national-hospital-cost-data-collection-report-public-sector-round-22-financial-year.
Australian Institute of Health and Welfare. Stroke. Canberra: Australian Institute of Health and Welfare. 2020. https://www.aihw.gov.au/reports/australias-health/stroke.
Stroke Foundation. National stroke audit—rehabilitation services report 2020. Melbourne, Australia. 2020. https://informme.org.au/stroke-data/Rehabilitation-audits.
Light K. Constraint-induced movement therapy: home-training is beneficial and cost effective. Physiotherapy. 2015;101:e873–4.
Pickett TC, Davis SB, Fritz SL, Malcolm MP, Ketterson TU, Light KE, et al. Telehealth and constraint-induced movement therapy (CIMT). Clin Gerontol. 2007;31(1):5–20.
Lum PS, Taub E, Schwandt D, Postman M, Hardin P, Uswatte G. Automated constraint-induced therapy extension (AutoCITE) for movement deficits after stroke. J Rehabil Res Dev. 2004;41(3A):249–58.
Hughes A-M, Meagher C, Burridge J. Arm rehabilitation at home for people with stroke: staying safe: encouraging results from the Co-designed LifeCIT programme. In: Kollak I, editor. Safe at home with assistive technology. Cham: Springer International Publishing; 2017. p. 59–79.
Cadilhac DA, Kim J, Wilson A, Berge E, Patel A, Ali M, et al. Improving economic evaluations in stroke: a report from the ESO Health Economics Working Group. Eur Stroke J. 2020;5(2):84–192.
Brady BK, McGahan L, Skidmore B. Systematic review of economic evidence on stroke rehabilitation services. Int J Technol Assess Health Care. 2005;21(1):15–21.
Treacy D, Howard K, Hayes A, Hassett L, Schurr K, Sherrington C. Two weeks of additional standing balance circuit classes during inpatient rehabilitation are cost saving and effective: an economic evaluation. J Physiother. 2018;64(1):41–7.
Craig LE, Wu O, Bernhardt J, Langhorne P. Approaches to economic evaluations of stroke rehabilitation. Int J Stroke. 2013;9(1):88–100.
Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin scale: implications for Stroke clinical trials. Stroke. 2007;38(3):1091–6.
Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337–43.
Soekhai V, de Bekker-Grob EW, Ellis AR, Vass CM. Discrete choice experiments in health economics: past present and future. Pharmacoeconomics. 2019;37(2):201–26.
Borch IH, Thrane G, Thornquist E. Modified constraint-induced movement therapy early after stroke: participants’ experiences. Eur J Physiother. 2015;17(4):208–14.
Page SJ, Levine P, Sisto S, Bond Q, Johnston M. Stroke patients’ and therapists’ opinions of constraint induced movement therapy. Clin Rehabil. 2002;16(1):55–60.
Morris DM, Shaw SE, Mark VW, Uswatte G, Barman J, Taub E. The influence of neuropsychological characteristics on the use of CI therapy with persons with traumatic brain injury. NeuroRehabilitation. 2006;21(2):131–7.
Shingler SL, Bennett BM, Cramer JA, Towse A, Twelves C, Lloyd AJ. Treatment preference, adherence and outcomes in patients with cancer: literature review and development of a theoretical model. Curr Med Res Opin. 2014;30(11):2329–41.
Haacker M, Hallett TB, Atun R. On time horizons in health economic evaluations. Health Policy Plan. 2020;35(9):1237–43.
Acknowledgements
We thank Angela Vratsistas-Curto for her assistance in confirming standard care estimates used within the model, Joseph Descallar for assistance with ABC benchmarking calculations used within the model, the Occupational Therapy and Physiotherapy departments of Liverpool, Bankstown, Braeside, Campbelltown and Camden Hospitals for participating in the study and the ACTIveARM advisory committee for support throughout the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The project was funded by the New South Wales Ministry of Health Translational Research Grants Scheme (TRGS) (project number 28).
Conflicts of interest
The authors declare no competing interests.
Ethical approval
Ethical approval was provided by the local ethics committee (ethics number HREC/16/LPOOL/419).
Consent to participate and publication
Informed consent was obtained from both therapists and CIMT participants prior to data collection, including consent to publish study findings.
Availability of data and material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability (software application or custom code)
Not applicable.
Authors' contributions
Lauren J. Christie: conceptualisation, data collection, data analysis, funding acquisition, project administration, writing of original draft manuscript, reviewing and editing of final manuscript. Nicola Fearn: conceptualisation, data collection, data analysis, reviewing and editing of final manuscript. Annie McCluskey: conceptualisation, contributions to data analysis, funding acquisition, reviewing and editing of final manuscript. Meryl Lovarini: conceptualisation, contributions to data analysis, funding acquisition, reviewing and editing of final manuscript. Reem Rendell: data collection, reviewing and editing of final manuscript. Alison Pearce: conceptualisation, methodology, data analysis, contributions to original draft manuscript, reviewing and editing of final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Christie, L.J., Fearn, N., McCluskey, A. et al. Cost-Effectiveness of Constraint-Induced Movement Therapy Implementation in Neurorehabilitation: The ACTIveARM Project. PharmacoEconomics Open 6, 437–450 (2022). https://doi.org/10.1007/s41669-022-00323-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-022-00323-9