Abstract
Purpose
The true aggressive behavior of oral cavity BSCC compared to SCC has been debated, and the study of disturbances in cell cycle proteins may help understand the biological behavior in both variants. The aim of this study was to investigate the p53 and p16 status in 32 SCC and 16 BSCC of oral cavity.
Methods
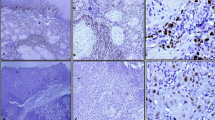
Immunohistochemistry was used to assess these proteins’ status. The association between p53 and p16 with clinico-pathological features and prognostic value were evaluated.
Results
A high prevalence of p53 disruption was observed in both variants (84.4% of 32—SCC and 81.2% of 16—BSCC; p = 0.78). The BSCC showed a higher prevalence of high p16 expression (86.7% of 15) when compared to SCC (61.3% of 31); however, this difference did not reach statistical significance (p = 0.08). In the SCC variant, cases with high p16 expression showed a lower overall survival. Protein p53 showed association with tobacco use, but with no other clinico-pathological features.
Conclusions
Our results suggest that p53 and p16 cell cycle disruptions are common findings in oral cavity SCC, as well as in BSCC. A higher prevalence of p16 overexpression in oral BSCC cases may be related to carcinogenesis process.


Similar content being viewed by others
References
Zini A, Czerninski R, Sgan-Cohen HD (2010) Oral cancer over four decades: epidemiology, trends, histology, and survival by anatomical sites. J Oral Pathol Med 39:299–305
Ralli M, Singh S, Yadav SP, Sharma N, Verma R, Sen R (2016) Assessment and clinicopathological correlation of p16 expression in head and neck squamous cell carcinoma. J Cancer Res Ther 12:232–237
de Sampaio Góes FC, Oliveira DT, Dorta RG, Nishimoto IN, Landman G, Kowalski LP (2004) Prognoses of oral basaloid squamous cell carcinoma and squamous cell carcinoma: a comparison. Arch Otolaryngol Head Neck Surg 130:83–86
Fritsch VA, Lentsch EJ (2014) Basaloid squamous cell carcinoma of the larynx: analysis of 145 cases with comparison to conventional squamous cell carcinoma. Head Neck 36:164–170
Jayasooriya PR, Tilakaratne WM, Mendis BR, Lombardi T (2013) A literature review on oral basaloid squamous cell carcinomas, with special emphasis on etiology. Ann Diagn Pathol 17:547–551
Pereira CH, Morais MO, Martins AF, Soares MQ, de Alencar RC, Batista AC et al (2016) Expression of adhesion proteins (E-cadherin and β-catenin) and cell proliferation (Ki-67) at the invasive tumor front in conventional oral squamous cell and basaloid squamous cell carcinomas. Arch Oral Biol 61:8–15
Bellizzi AM, Woodford RL, Moskaluk CA, Jones DR, Kozower BD, Stelow EB (2009) Basaloid squamous cell carcinoma of the esophagus: assessment for high-risk human papillomavirus and related molecular markers. Am J Surg Pathol 33:1608–1614
Chernock RD, Lewis JS Jr, Zhang Q, El-Mofty SK (2010) Human papillomavirus-positive basaloid squamous cell carcinomas of the upper aerodigestive tract: a distinct clinicopathologic and molecular subtype of basaloid squamous cell carcinoma. Hum Pathol 41:1016–1023
Jacobi C, Ayx I, Fritsche K, Piontek G, Hoffmann D, Weirich G et al (2015) Potential impact of human papillomavirus on survival of basaloid squamous carcinoma of the head and neck. Oncotarget 6:3462–3470
Califano J, van der Riet P, Westra W, Nawroz H, Clayman G, Piantadosi S et al (1996) Genetic progression model for head and neck cancer: implications for field cancerization. Can Res 56:2488–2492
Reshmi S, Gollin S (2005) Chromosomal instability in oral cancer cells. J Dent Res 84:107–117
Fischer NW, Prodeus A, Malkin D, Gariépy J (2016) p53 oligomerization status modulates cell fate decisions between growth, arrest and apoptosis. Cell Cycle 15:3210–3219
Karpathiou G, Monaya A, Forest F, Froudarakis M, Casteillo F, Dumollard J et al (2016) p16 and p53 expression status in head and neck squamous cell carcinoma: a correlation with histological, histoprognostic and clinical parameters. Pathology 48:341–348
Suh Y, Amelio I, Guerrero Urbano T, Tavassoli M (2014) Clinical update on cancer: molecular oncology of head and neck cancer. Cell Death Dis. https://doi.org/10.1038/cddis.2013.548
Shah NG, Trivedi TI, Tankshali RA, Goswami JV, Jetly DH, Shukla SN et al (2009) Prognostic significance of molecular markers in oral squamous cell carcinoma: a multivariate analysis. Head Neck 31:1544–1556
Vallonthaiel AG, Singh MK, Dinda AK, Kakkar A, Thakar A, Das SN (2016) Expression of cell cycle-associated proteins p53, pRb, p16, p27, and correlation with survival: a comparative study on oral squamous cell carcinoma and verrucous carcinoma. Appl Immunohistochem Mol Morphol 24:193–200
Yuen PW, Chow V, Choy J, Lam KY, Ho WK, Wei WI (2001) The clinicopathologic significance of p53 and p21 expression in the surgical management of lingual squamous cell carcinoma. Am J Clin Pathol 116:240–245
Mane DR, Kale AD, Angadi P, Hallikerimath S (2013) Expression of cytokeratin subtypes: MMP-9, p53, and αSMA to differentiate basaloid squamous cell carcinoma from other basaloid tumors of the oral cavity. Appl Immunohistochem Mol Morphol 21:431–443
Sampaio-Góes FC, Oliveira DT, Dorta RG, Nonogaki S, Landman G, Nishimoto I et al (2005) Expression of PCNA, p53, BAX, and Bcl-X in oral poorly differentiated and basaloid squamous cell carcinoma: relationships with prognosis. Head Neck 27:982–989
Romagosa C, Simonetti S, López-Vicente L, Mazo A, Lleonart ME, Castellvi J et al (2011) p16Ink4a overexpression in cancer: a tumor suppressor gene associated with senescence and high-grade tumors. Oncogene 30:2087–2097
Satgunaseelan L, Virk SA, Lum T, Gao K, Clark JR, Gupta R (2016) p16 expression independent of human papillomavirus is associated with lower stage and longer disease-free survival in oral cavity squamous cell carcinoma. Pathology 48:441–448
Zhao N, Ang MK, Yin XY, Patel MR, Fritchie K, Thorne L et al (2012) Different cellular p16(INK4a) localisation may signal different survival outcomes in head and neck cancer. Br J Cancer 107:482–490
Chernock RD, Wang X, Gao G, Lewis JS Jr, Zhang Q, Thorstad WL et al (2013) Detection and significance of human papillomavirus, CDKN2A(p16) and CDKN1A(p21) expression in squamous cell carcinoma of the larynx. Mod Pathol 26:223–231
Cho KJ, Su J, Kim SB, Lee SW, Choi SH, Nam SY et al (2017) Basaloid squamous cell carcinoma of the head and neck: subclassification into basal, ductal, and mixed subtypes based on comparison of clinico-pathologic features and expression of p53, cyclin D1, epidermal growth factor receptor, p16, and human papillomavirus. J Pathol Transl Med. https://doi.org/10.4132/jptm.2017.03.03
Begum S, Westra WH (2008) Basaloid squamous cell carcinoma of the head and neck is a mixed variant that can be further resolved by HPV status. Am J Surg Pathol 32:1044–1050
Baba Y, Ishimoto T, Harada K, Kosumi K, Murata A, Miyake K et al (2015) Molecular characteristics of basaloid squamous cell carcinoma of the esophagus: analysis of KRAS, BRAF, and PIK3CA mutations and LINE-1 methylation. Ann Surg Oncol 22:3659–3665
Imamhasan A, Mitomi H, Saito T, Hayashi T, Takahasi M, Kajiyama Y et al (2012) Immunohistochemical and oncogenetic analysis of the esophageal basaloid squamous cell carcinoma in comparison with conventional squamous cell carcinomas. Hum Pathol 43:2012–2023
Solomon MC, Vidyasagar MS, Fernandes D, Guddattu V, Mathew M, Shergill AK et al (2016) The prognostic implication of the expression of EGFR, p53, cyclin D1, Bcl-2 and p16 in primary locally advanced oral squamous cell carcinoma cases: a tissue microarray study. Med Oncol 33:138
Gonzalez JC, Cepeda LG, Yanez SB, Cornejo A, Estevez AM, Huerta E (2016) p53 and p16 in oral epithelial dysplasia and oral squamous cell carcinoma: a study of 208 cases. Indian J Pathol Microbiol 59:153–158
Rodríguez Tojo MJ, García Cano FJ, Infante Sánchez JC, Velázquez Fernández E, Aguirre Urízar JM (2005) Immunoexpression of p53, Ki-67, and E-cadherin in basaloid squamous cell carcinoma of the larynx. Clin Transl Oncol 7:110–114
Nylander K, Dabelsteen E, Hall PA (2000) The p53 molecule and its prognostic role in squamous cell carcinoma of the head and neck. J Oral Pathol Med 29:413–425
Cohen ER, Reis IM, Gomez C, Pereira L, Freiser ME, Hoosien G et al (2017) Immunohistochemistry analysis of CD44, EGFR, and p16 in oral cavity and oropharyngeal squamous cell carcinoma. Otolaryngol Head Neck Surg. https://doi.org/10.1177/0194599817700371
Begum S, Gillison ML, Ansari-Lari MA, Shah K, Westra WH (2003) Detection of human papillomavirus in cervical lymph nodes: a highly effective strategy for localizing site of tumor origin. Clin Cancer Res 9(17):6469–6475
Klaes R, Friedrich T, Spitkovsky D, Ridder R, Rudy W, Petry U et al (2001) Overexpression of p16(INK4A) as a specific marker for dysplastic and neoplastic epithelial cells of the cervix uteri. Int J Cancer 92(2):276–284
Sano T, Oyama T, Kashiwabara K, Fukuda T, Nakajima T (1998) Expression status of p16 protein is associated with human papillomavirus oncogenic potential in cervical and genital lesions. Am J Pathol 153(6):1741–1748
Gröbe A, Hanken H, Kluwe L, Schöllchen M, Tribius S, Pohlenz P et al (2013) Immunohistochemical analysis of p16 expression, HPV infection and its prognostic utility of oral squamous cell carcinoma. J Oral Pathol Med 42:676–681
Friederich RE, Sperber C, Jäkel T, Röser K, Löning T (2010) Basaloid lesions of oral squamous epithelial cells and their association with HPV infection and P16 expression. Anticancer Res 30:1605–1612
Chung CH, Gillison ML (2009) Human papillomavirus in head and neck cancer: its role in pathogenesis and clinical implications. Clin Cancer Res 15:6758–6762
Sedghizadeh PP, Billington WD, Paxton D, Ebeed R, Mahabady S, Clark GT et al (2016) Is p16-positive oropharyngeal squamous cell carcinoma associated with favorable prognosis? A systematic review and meta-analysis. Oral Oncol 54:15–27
Sritippho T, Pongsiriwet S, Lertprasertsuke N, Buddhachat K, Sastraruji T, Iamaroon A (2016) p16—a possible surrogate marker for high-risk human papillomaviruses in oral cancer? Asian Pac J Cancer Prev 17:4049–4057
Upile NS, Shaw RJ, Jones TM, Goodyear P, Liloglou T, Risk JM et al (2014) Squamous cell carcinoma of the head and neck outside the oropharynx is rarely human papillomavirus related. Laryngoscope 124(12):2739–2744
Ambrosch P, Schlott T, Hilmes D, Ruschenburg I (2001) p16 alterations and retinoblastoma protein expression in squamous cell carcinoma and neighboring dysplasia from the upper aerodigestive tract. Virchows Arch 438:343–349
Schmitt CA, Fridman JS, Yang M, Lee S, Baranov E, Hoffman RM et al (2002) A senescence program controlled by p53 and p16INK4a contributes to the outcome of cancer therapy. Cell 109:335–346
Acknowledgements
The authors acknowledge the Foundation for Research Support in the State of Goiás for the financial support (FAPEG Grant No. 201201270020063).
Funding
Financial support was provided by the Foundation for Research Support in the State of Goiás (FAPEG Grant No. 201201270020063).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Informed consent
Due to the retrospective nature of this study, formal consent of each participant was not required.
Ethical approval
This research was approved by the Federal University of Goiás Research Ethics Committee (Protocol 22/2013).
Rights and permissions
About this article
Cite this article
Martins, A.F.L., Pereira, C.H., Morais, M.O. et al. p53 and p16 expression in oral cavity squamous cell and basaloid squamous cell carcinoma. Oral Cancer 2, 7–17 (2018). https://doi.org/10.1007/s41548-018-0004-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41548-018-0004-1