Abstract
Systemic corticosteroids (CSs), a keystone in pulmonology, are drugs with strong antiinflammatory activity. They are cheap, easily available, and accessible, but with common and serious side effects. Moreover, the use of exogenous CSs may suppress the hypothalamic–pituitary–adrenal (HPA) axis, predisposing to adrenal insufficiency. Safe CS treatment is a challenge of pharmacological research. This narrative review examined the indications of CSs in some respiratory diseases, analyzing what types, dosages, and length of treatment are required as the dosage and duration of CS treatments need to be minimized. Chronic maintenance treatments with CSs are associated with poor prognosis, but they are still prescribed in patients with severe asthma, Chronic obstructive pulmonary disease (COPD), and interstitial lung diseases. When CS discontinuation is not possible, all efforts should be made to achieve clinically meaningful reductions. Guidelines suggest the use of methylprednisolone at a dose of 20–40 mg/day or equivalent for up to 10 days in subjects with COVID-19 pneumonia (but not other respiratory viral diseases) and respiratory failure, exacerbations of asthma, and COPD. Some guidelines suggest that CS treatment shorter than 10–14 days can be abruptly stopped, strictly monitoring subjects with unexplained symptoms after CS withdrawal, who should promptly be tested for adrenal insufficiency (AI) and eventually treated. CSs are often used in severe community-acquired pneumonia associated with markedly increased serum inflammation markers, in acute respiratory distress syndrome (ARDS), in septic shock unresponsive to hydro-saline replenishment and vasopressors, and acute exacerbations of interstitial lung diseases. As these cases often require higher doses and longer duration of CS treatment, CS tapering should be gradual and, when useful, supported by an evaluation of HPA axis function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cortisol, the main glucocorticoid hormone, has strong antiinflammatory activity. The antiinflammatory activity of cortisol, and its more powerful synthetic derivatives, is often utilized in medicine. |
Systemic corticosteroid drugs have common and serious side effects. These adverse effects are not only due to direct toxicity but may also be related to withdrawal. In fact, exogenous use of corticosteroid interferes with the function of the HPA axis, and may suppress the endogenous production of cortisol, predisposing patients experiencing abrupt interruption of the drug to adrenal insufficiency. |
Systemic corticosteroid drugs are effective, cheap, easily available, and accessible. Their use remains common in several respiratory diseases, such as COVID-19 pneumonia, severe community-acquired pneumonia, ARDS, septic shock, some interstitial lung diseases, COPD, and asthma and their exacerbations. |
Guideline recommendations on systemic corticosteroid use in respiratory medicine show some discrepancies, with unclear chapters, and are often updated. New knowledge and alternative therapeutic options also make their extensive implementation difficult in real life. Effective and safe treatment with corticosteroids is a challenge and forces clinicians to continuously review and balance the risks and benefits of treatment. |
This review aims to update current indications to systemic corticosteroid use in respiratory medicine, including choice of drug, dosage, timing, and duration of treatment and tapering strategy. |
There is increasing evidence suggesting limiting as much as possible the use of systemic corticosteroids. When complete discontinuation of corticosteroids is not possible, all efforts should be made to achieve clinically meaningful reductions. Meanwhile, monitoring the patient carefully to detect early side effects and to treat accordingly is always required. |
Introduction
The adrenal cortex produces several corticosteroid hormones, including mineralocorticoids (i.e., aldosterone) involved in fluid and electrolyte balance, and glucocorticoids (hereafter, CSs) that are involved in the maintenance of homeostasis, also exerting ant-inflammatory activities. This last property is commonly utilized in medicine. A US retrospective cohort study that enrolled more than a million subjects revealed that 21% received a CS treatment within the last year [1]. Respiratory diseases accounted for a substantial part of total CS prescriptions. Unfortunately, CS use is associated with common and severe adverse effects (Table 1).
Our aim is to define the minimally effective dose of CSs in respiratory medicine. We searched for the following key terms in PubMed and Google Scholar databases from inception to December 2022: glucocorticoid, steroid, corticosteroid, dexamethasone, betamethasone, hydrocortisone, cortisol, methylprednisolone, prednisone AND ARDS, sepsis, respiratory viral infections, influenza, SARS, MERS, COVID-19, SARS-CoV-2, CAP, COPD, asthma, fibrosis, interstitial lung disease, chronic bronchitis, emphysema, exacerbation. This paper is a qualitative review including randomized controlled trials (RCTs), observational studies, meta-analyses, and guidelines in this field. We performed no statistical analysis and report evidence in a descriptive way. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
CS and Adrenal Insufficiency
Several synthetic CSs have been developed for pharmacological use. They have higher antiinflammatory potency and lower mineralocorticoid activity than cortisol, the main endogenous hormone, as presented in Table 2 [2]. The antiinflammatory properties of CSs are used as maintenance treatment to manage several respiratory diseases, such as sarcoidosis, some interstitial lung diseases (ILDs) and difficult-to-control asthma. More often, CSs are used as bursts for some days to treat exacerbations or acute respiratory events.
A primary care UK study in which over 24,000 subjects receiving CSs (and matched controls) were followed-up over time demonstrated a direct relationship between adverse events and CS exposure, with substantial increases in risk seen above a cumulative dose of 1000 mg prednisone or equivalent [3]. A population-based cohort analysis evaluated the incidence of three major adverse effects that the use of CSs may provoke in users. Most subjects (70%) had received only one course of CSs per year, with a median prednisone equivalent daily dose of 20 mg/day for 6 days. There was a statistically significant increase in the rate of sepsis [incidence rate ratio (IRR): 3.77], venous thromboembolism (IRR: 3.11), and fracture (IRR: 1.96) in the CS users versus non-CS users within the first 30 days of treatment [1]. These data show that not only prolonged treatments, but even short courses of CSs may be associated with common and severe adverse events.
Not only treatments with CSs may give side effects, but also their abrupt interruption. In fact, endogenous CS production is regulated by the hypothalamic–pituitary–adrenal (HPA) axis, where adrenocorticotrophic hormone (ACTH) and corticotrophin releasing (CTR) factor promote cortisol delivery and circulating cortisol exerts negative feedback on ACTH and CTR production. Exogenous CSs suppress ACTH and CTR production and may interfere with release of endogenous CSs, leading to adrenal insufficiency (AI). AI may be severe or even life threatening and is often associated with nonspecific symptoms, such as fatigue, hypotension, hyponatremia, nausea, vomiting, diarrhoea, abdominal pain, anorexia/weight loss, headache, fever, myalgia, arthralgia, or psychiatric symptoms. The daily cortisol production is approximately 20 mg in adults, but this increases during stressful conditions [4], which explains why clinically relevant AI is more common in acute conditions.
In their meta-analysis estimating percentages of subjects with AI after treatment with CSs for various conditions, Broersen [5] et al. found, stratifying by doses, percentages of patients with AI from 2.4% (95% CI 0.6–9.3) for doses equivalent to < 10 mg prednisone per day to 21.5% (95% CI 12.0–35.5) for > 20 mg prednisone per day; stratifying by treatment duration AI was found from 1.4% (95% CI 0.3–7.4) for treatments < 28 day to 27.4% (95% CI 17.7–39.8) for > 1 year. The same study observed that some subjects meeting laboratory diagnosis of AI reported symptoms and only some patients showed AI for a certain cumulative CS dosage. Most subjects showed a full recovery within 2 weeks, but others required longer times, showing that the time of recovery from AI after CS withdrawal is unpredictable.
Several laboratory tests have been proposed to assess HPA axis function and AI. Serum cortisol measurements at 9 a.m. is commonly considered the gold standard for AI assessment and may exclude or confirm its presence. Each laboratory should define its own methods and normal ranges of measurement, but a 9 a.m. serum cortisol level < 80–100 nmol/L (< 3–5 mcg/dL) is the usual cut-off value indicating AI. In contrast, a 9 a.m. serum cortisol > 350–500 nmol/L (> 20 mcg/dL) excludes AI. Values falling between the selected thresholds are generally considered as indeterminate and may be resolved by the corticotropin (short Synacthen®, Cortrosyn®) stimulation test. This test assesses the integrity of the HPA axis based on peak response after ACTH injection. A single dose (250 μg) of synthetic ACTH is usually administered at 9 a.m.; blood samples are drawn immediately before the test and at 30 min after the injection to assess the rise in serum cortisol. An attenuated or absent increase in response to direct stimulation by supra-physiologic ACTH indicates adrenal gland atrophy [4]. Noteworthily, the test for AI available in clinical practice has a high sensitivity rather than a high specificity, and the number of false positive tests is not negligible. It has been suggested that the low-dose (0.5–1 mcg) synthetic ACTH stimulation test may be more sensitive than the supra-physiologic 250 mcg test in the suspicion of secondary AI, but this test remains the preferred assessment for screening of secondary AI [4].
COVID-19 and Other Viral Respiratory Infections
At the onset of the pandemic, there was disagreement on the usefulness of CS therapy in subjects with COVID-19 pneumonia. Over time, many severe forms were attributed to an inflammatory cytokine storm and CS use could have the potential to decrease upregulated inflammatory responses. The RECOVERY study [5] has shown the role of CSs in severe COVID-19. This trial enrolled 6425 (mean age 66 years, 56% with comorbidities) hospitalized patients with COVID-19; 2104 subjects were given dexamethasone 6 mg orally or intravenously once daily for up to 10 days or until discharged and 4321 subjects were randomized to receive usual therapy. The group treated with dexamethasone showed a significantly lower mortality (at 28 days, primary outcome of the study) than the control arm (22.9% versus 25.7%; RR 0.83; 95% CI 0.75–0.93; P < 0.001). In the analysis prespecified for subgroups, the reduction of the mortality rate in the arm treated with dexamethasone was observed both in the subgroup of subjects with oxygen supplementation (23.3% versus 26.2%; RR 0.82; 95% CI 0.72–0.94) and, above all, in those on invasive mechanical ventilation (29.3% versus 41.4%; RR 0.64; 95% CI 0.51–0.81), but not in the subgroup of subjects not receiving any oxygen supplementation (17.8% versus 14.0%; RR 1.19; 95% CI 0.91–1.55).Other subgroup analyses showed significant advantage only when dexamethasone was introduced in subjects with onset of symptoms for more than 8 days, aged less than 70 years, and in males, confirming the need of personalizing treatment. It has been shown that initial pulse dose (1 g methylprednisolone boluses for 3 consecutive days in addition to dexamethasone [6]), higher doses, and longer duration [7] of CS treatment did not improve outcomes. Table 3 presents the guideline recommendations [8,9,10,11,12,13] for CS use in subjects with COVID-19 requiring at least oxygen therapy. The guidelines also highlight that, if dexamethasone is unavailable, equivalent daily doses of alternative CSs may be used [10].
The 2018 IDSA guidelines for the management of influenza do not recommend add-on therapy with CSs for the treatment of suspected or confirmed seasonal influenza, influenza-associated pneumonia, or respiratory failure, unless clinically indicated for other reasons (e.g., exacerbation of asthma, COPD, refractory septic shock). A recent study has confirmed that CS administration increased the occurrence of nosocomial infections and mortality in patients with seasonal/mixed seasonal flu. In addition, the use of CSs in subjects with influenza may be associated with a prolonged viral spread [14].
ARDS
Acute respiratory distress syndrome (ARDS) is a common cause of respiratory failure and death in critically ill subjects and is defined as an acute diffuse inflammatory lung injury manifesting as acute severe hypoxemia, bilateral lung infiltrates, and noncardiogenic pulmonary edema. The PaO2/FiO2 ratio is usually used to distinguish mild (200 < PaO2/FiO2 ≤ 300 mmHg), moderate (100 < PaO2/FiO2 ≤ 200 mmHg), and severe ARDS (PaO2/FiO2 ≤ 100 mmHg).
An extensive meta-analysis of 18 randomized controlled trials [15] including 2826 adult subjects with ARDS (all invasively ventilated) of any etiology confirmed that the use of CSs reduced hospital mortality (RR 0.82; 95% CI 0.72–0.95). Subgroup analysis showed that subjects receiving a longer course of CS (> 7 days) had higher success rates, while no significant benefit in hospital mortality was observed with late administration (> 7 days of onset of ARDS) of CSs (RR 0.52; 95% 0.11–2.52). A meta-analysis [16] found that the use of methylprednisolone (RR = 0.70; 95% CI 0.56–0.88; P < 0.01), and cortisol (RR = 0.79; 95% CI: 0.63–0.98; P = 0.03) was also associated with reduction of 28 day mortality. Another meta-analysis observed that CS treatments longer than 7 days and low dosage (≤ 2 mg/kg methylprednisolone per day) were significantly associated with decreased mortality in adult ARDS patients [18]. The results of meta-analyses may be prone to publication bias, but the largest randomized controlled trial to date, the DEXA-ARDS [19], enrolling 277 subjects with moderate-to-severe ARDS, confirmed that early administration of dexamethasone 20 mg once daily from day 1 to day 5, and 10 mg once daily from day 6 to day 10, reduced the duration of mechanical ventilation at 28 days (between-group difference 4.8 days, 95% CI 2.6–7.0 days; P < 0·0001) and mortality at 60 days (21% versus 36%; 95% CI −25.9 to −4.9; P = 0·0047). Current recommendations for CS use in ARDS are reported in Table 4 [20,21,22,23]. The optimal dose and the duration of CS regimens in ARDS needs to be further studied. This is a very important issue because large and prolonged doses of CS may be associated with severe adverse events, such as neuropathy and myopathy, commonly observed in subjects admitted in critical conditions and responsible for increased length of hospital stays and mortality. CSs should be weaned slowly (6 − 14 days) and not abruptly as deterioration may occur from the development of a reconstituted inflammatory response. Meduri et al. [2] have proposed a regimen protocol, reported in the Supplementary file 1.
Sepsis and Septic Shock
Sepsis is defined as a life-threatening host response to an infection that can culminate in shock, (multi)organ failure (including ARDS), and death. In about 15% of subjects, sepsis evolves into septic shock. In-hospital mortality of septic shock ranges from 30% to 50%. Although evaluated in several randomized controlled trials, the safety and efficacy of CSs remain controversial [24]. There is a wide heterogeneity between the studies and conclusions are supported with low or very low certainty of evidence. Most researchers agree that the use of CSs reduces the duration of shock, ventilator use, and intensive care unit (ICU) stay [24]. CSs should only be used as adjuvant therapy for septic shock unresponsive to hydro-saline replenishment and vasopressors. If CSs are used, guidelines recommend cortisol for at least 3 days; in most cases CSs can be stopped after cessation of vasopressors. Most trials evaluated intravenous cortisol (200 mg continuously or 60 mg in bolus four times per day), finding no evidence of variation in effect, even when modifying the type of CS used. There is no clear consensus on whether CSs should be tapered or if abrupt withdrawal is appropriate, but larger randomized controlled trials did not use a tapering strategy and found no difference in shock recurrence [24].
Interstitial Lung Diseases
Interstitial lung diseases (ILDs) are a heterogeneous family of pulmonary disorders with diffuse lung fibrosing lesions. Idiopathic pulmonary fibrosis (IPF), the most common ILD, has a rapidly progressive course associated with deteriorating quality of life and poor prognosis [25]. Although the natural history of ILDs other than IPF varies, a significant percentage of subjects with these diseases, approximately one-third of the total, also show rapid progression [26]. During the disease course, many subjects with these diseases experience acute exacerbations, characterized by a sudden decline in lung function and quality of life with an increase in lung ground glass opacities and/or consolidation, not related to heart failure and/or pulmonary embolism. Acute exacerbations are associated with worsening prognosis in subjects with ILDs [25, 26]. Despite the lack of strong evidence supporting the use of CSs in acute exacerbations, their use is common practice. An international survey on exacerbation of subjects with IPF including 509 pulmonologists from 66 countries has supported its use, recommending a pulse dose of 500–1000 mg of methylprednisolone intravenously for the first 3 days, followed by oral prednisone 1 mg/kg once daily for an average of 13 weeks [27]. A retrospective cohort study of 89 patients with ILD (56 with IPF and 33 with non-IPF ILD) with acute exacerbation used a similar treatment protocol with CSs. On the seventh day from starting treatment, an High resolution Chest Tomography (HRCT) was repeated, and prednisone was tapered for 4–6 weeks if there were radiological improvements; if no radiological and/or clinical improvements were seen, the CS was discontinued. The 1 year transplant-free survival was 20% in IPF subjects and 52% in non-IPF patients [28]. Although gradual tapering of CS is a common practice to manage exacerbations of subjects with ILDs, there is no consensus on the best tapering strategy. Early tapering was defined as a reduction in CS maintenance dose of > 10% within 2 weeks of admission, regardless of the pulse approach. In a retrospective Japanese study in subjects treated for exacerbation of IPF, Anan et al. [29] found that early CS dose tapering was associated with a favorable outcome (90 day mortality). By contrast, another retrospective single-center cohort study reported that a high total CS dose in the first 30 days was associated with fewer relapses of exacerbations compared with a low total dose [30].
Community-Acquired Pneumonias
Community acquired pneumonias (CAPs) are common and serious acute events, often of bacterial etiology. CAP mortality remains high even if early and appropriate antimicrobial therapy is administered, supporting the hypothesis that prognosis depends not only on the virulence and bacterial load of the agent, but also on the reaction of the host. The use of CSs may accelerate symptom resolution and time to clinical stability in subjects with severe CAP, but their ultimate effect is still undetermined. Studies evaluating the role of CSs have low certainty of evidence and included populations with CAP of various severity and the use of different CS regimens. In Table 5 we have reported guideline recommendations on CS use as adjuvant treatment in subjects with CAP [31,32,33,34,35]. British Thoracic Society (BTS) [31] and American Thoracic Society (ATS)/Infectious Diseases Society of America (IDSA) guidelines [34] do not routinely recommend the use of CSs in the absence of respiratory comorbidities, such as asthma or COPD. The South African guidelines [33] support the use of CSs in adults with severe CAP requiring ICU admission unless the suspicion of influenza, tuberculosis, or a recent (within the previous 3 months) history of gastrointestinal bleeding.
Two recent large randomized controlled trials including subjects with severe CAP have also found contrasting results. The ESCAPe trial [36], including 586 patients (33% receiving mechanical ventilation at the time of randomization), did not show any difference in 60 day mortality with CSs (adjusted odds ratio 0.90, 95% CI 0.57–1.40). By contrast, in a French study [37] including 795 adults, there was a significantly lower mortality (at 28 days, primary outcome of the study) in the active group (intravenous cortisol 200 mg daily for either 4 or 8 days as determined by clinical improvement, followed by tapering for a total of 8 or 14 days) versus the placebo arm (absolute difference, −5.6%; 95% CI −9.6% to −1.7%; P = 0.006). The use of CSs has been advocated in subjects with CAP who have septic shock and/or a high inflammatory response such as C-reactive protein (serum C-reactive protein (CRP)) values > 15 mg/dL at admission and the need for invasive mechanical ventilation. Prednisone 50 mg for 5–7 days without tapering is the most studied regimen, but the optimal duration of treatment and the right way of discontinuing it (tapering or not) has not yet been standardized.
COPD
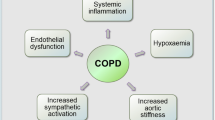
Chronic obstructive pulmonary disease (COPD) is a heterogeneous lung condition characterized by chronic respiratory symptoms and persistent airflow obstruction. The course of COPD may be punctuated by acute events, defined exacerbations, that negatively impact on health status, rates of hospitalization, and disease progression (3762) . Systemic CSs are commonly used in acute exacerbations of COPD due to their effectiveness in shortening the recovery time and reducing the risk of early relapse and treatment failure (3762). As presented in Table 6, guidelines recommend the use of CSs for the management of exacerbations in COPD patients [38,39,40,41,42,43,44]. The best time for first CS administration is undefined, but probably the earlier the better. Apart from Thoracic Society of Australia and New Zealand (TSANZ) guidelines, which recommend tapering for treatments longer than 14 days, there is no clear indication if abrupt withdrawal is appropriate, but larger RCTs organized in the absence of a tapering strategy found no difference in recurrences. Intriguingly, a recent prospective, randomized, open-label trial has evaluated a personalized approach in CS dosage (providing a starting daily dose > 60 mg for many included subjects) versus the standard regimen (40 mg daily dose of prednisolone or equivalent) in 248 in-hospital patients with COPD exacerbation using some factors, such as Anthonisen type exacerbation, COPD Assessment Test score, previous CS dose in the last exacerbation, inflammatory markers (C-reactive protein and eosinophils), results of blood gas analysis, and weight. Failure of therapy occurred in 28% of the personalized-dose group compared with 49% in the fixed-dose arm (relative risk, 0.40; 95% CI 0.24–0.68; P < 0.001) [45].
Another approach to reduce the cumulative dose of CS for managing exacerbations is driven by blood eosinophil counts. The open, multicenter CORTICO-COP RCT including 318 subjects hospitalized for exacerbations that, after administering a first dose of 80 mg methylprednisolone intravenously on day 1, randomized half of participants to a scheme of 37.5 mg prednisolone per day for 4 days, while the other arm provided such administration only on days in which eosinophil counts were > 300/mcl. There was a significant reduction in the cumulative CS total dose in the eosinophil count-led group (P < 0.0001), but no differences were found between the two groups in hospital stay, mortality, or treatment failure at 30 days [46]. Some practical difficulties persist for the routine use of blood eosinophil counts to drive CS treatment of COPD exacerbations. Firstly, variations in blood eosinophil counts may occur in hourly samples, used drugs, and exercise or food habits. Secondly, it may be not easy to take a daily blood sample at home. Finally, there is no full agreement on the threshold of blood eosinophil count driving CS treatment.
Asthma
Asthma is a highly prevalent syndrome of chronic airway inflammation, variability in respiratory symptoms, and expiratory airflow limitation. The goal of asthma management is to achieve disease stability, defined as good symptom control and reduced risk of exacerbations. Guidelines stratify asthma in five progressive steps based on treatment intensity [47]. Inhaled corticosteroids (ICSs), at different dosages, eventually associated with one or more controllers, are the cornerstone of asthma control. Approximately 5–10% of patients with asthma have a disease defined as severe, which is uncontrolled despite good adherence with high-dose ICS (see Table 2) plus controllers, or that worsens when high-dose ICS treatment is decreased. Prolonged use of CSs has long been the mainstay of treatment for chronic severe asthma, but their use is currently considered as a last option when control is not achieved with standard care [47]. Despite this recommendation, the occurrence of chronic CS treatment is relatively common in real life. A retrospective Korean study among adults with asthma followed by specialists found that 2.1% of the study population had CS-dependent asthma [48]. A similar percentage of patients with uncontrolled asthma using regular CSs was also observed across five countries in the ISAR study [49]. The use of biologics as an add-on therapy is now the standard of care for subjects with severe asthma, despite the use of high-dose ICS plus controllers [47]. Biologics often permit the cessation of CSs; when complete CS discontinuation is not possible, clinically meaningful reductions can be achieved. Some recent trials [50] have formally utilized adrenal function testing as part of the CS reduction protocol, introducing an algorithm (a simplified form is displayed in Fig. 1) for safer withdrawal of CSs.
Suggested protocol of withdrawal, also including hypothalamic–pituitary–adrenal (HPA) axis function following prolonged corticosteroid treatment (modified from ref. [50])
Patients with asthma sometimes suffer from exacerbations that may be life-threatening and cause a further decline in quality of life and lung function [47]. A severe exacerbation is defined as acute worsening of asthma requiring a burst of CSs, an emergency visit, and/or hospitalization. CSs are effective for treating asthma exacerbations [47]. Guidelines recommend a 5–7 day course of prednisolone in all but mildest exacerbations, as reported in Table 7 [47, 52,53,54,55,56,57]. Tapering is usually not recommended, but prompt administration (within 1 h) is required.
Severe exacerbations are observed in any stage of asthma, but are more common in subjects with severe asthma, CS-dependent disease, and history of previous exacerbations [47]. A German study observed that approximately 7–15% of subjects at GINA steps 1–4 and 35% at step 5 treatment received at least one burst of CSs annually [58]. A nationwide cohort study in France reported that 59% of patients with severe asthma were treated with bursts of CSs, with an average frequency of 3.3 courses per patient per year [59]. An Australian report observed that about 25% of patients with asthma were prescribed CS doses > 1000 mg of prednisolone equivalent over a 5 year period [60].
Conclusions
CSs are very effective, affordable (they are cheap), and highly accessible (sometimes as over-the-counter products) with global availability, but there is increasing evidence that their use, even for short-burst treatments, can give common and severe adverse effects Noteworthy, there is no clear relationship between cumulative dosage of CS therapy and adverse effects. Possibly age, comorbidities, and individual susceptibility are relevant variables that can influence CS toxicity. Nevertheless, effective and safe treatment with CSs is a challenge, largely recognized by patients and physicians, which forces clinicians to continuously review and balance the risks and benefits of treatment. Discontinuation or minimization of cumulative doses should always be attempted [61]. In a consensus statement, a reduction in prednisolone of at least 5 mg (2.5 mg if the starting dose was ≤ 10 mg/day) per day was considered as clinically meaningful [8]. Recent studies are increasing our knowledge on HPA axis function and the risk of its suppression after CS treatment. Meanwhile, carefully monitoring the patient to detect early abnormalities (i.e., fluid retention, hyperglycemia, increase in blood pressure) and accordingly treat them is always required. We have tried to give indications on the minimally effective dosage of CS treatment in adults for the most common respiratory diseases, also including (when available) timing of starting schedule, type of drug, duration, and dose tapering. Future research should select patients who are most likely to show a benefit of CS treatment, and personalized dosages driven by clinical and laboratory biomarkers. When oral administration is feasible, intravenous or intramuscular use does not offer any advantage over oral CS therapy. Although some molecules are preferentially used in studies, there is no direct head-to-head comparison of different CSs. At the moment, there are few (if any) clinical reasons to prefer a certain CS, although available molecules differ in relative potencies, pharmacodynamics, and pharmacokinetics. Queries remain open, not only on the choice of the CS, but also on the dosing, timing, and duration of treatment [17, 51].
References
Waljee AK, Rogers MA, Lin P, et al. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ. 2017;357:j1415. https://doi.org/10.1136/bmj.j1415.
Meduri GU, Annane D, Confalonieri M, et al. Pharmacological principles guiding prolonged glucocorticoid treatment in ARDS. Intensive Care Med. 2020;46(12):2284–96.
Price DB, Trudo F, Voorham J, et al. Adverse outcomes from initiation of systemic corticosteroids for asthma: long-term observational study. J Asthma Allergy. 2018;11:193–204.
Society for Endocrinology. Society position statements: use of synthetic ACTH (Synacthen) in patients with a history of asthma. 2020. https: www.endocrinology.org/clinical-practice/clinical-guidance/society-position-statements/. Accessed 31 December2022.
Broersen LH, Pereira AM, Jørgensen JO, Dekkers OM. Adrenal insufficiency in corticosteroids use: systematic review and meta-analysis. J Clin Endocrinol Metab. 2015;100:2171–80. https://doi.org/10.1210/jc.2015-1218.
Horby P, Lim WS, Emberson JR, for the RECOVERY Collaborative Group, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;25:693–704. https://doi.org/10.1056/NEJMoa2021436.
Salvarani C, Massari M, Costantini M, et al. Intravenous methylprednisolone pulses in hospitalised patients with severe COVID-19 pneumonia, a double-blind, randomised, placebo-controlled trial. Eur Respir J. 2022. https://doi.org/10.1183/13993003.00025-2022.
Salton F, Confalonieri P, Centanni S, et al. Prolonged higher dose methylprednisolone vs. conventional dexamethasone in COVID-19 pneumonia: a randomised controlled trial (MEDEAS). Eur Respir J. 2022. https://doi.org/10.1183/13993003.01514-2022.
World Health Organization. Corticosteroids for COVID-19: Living guidance 2 September 2020. https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-Corticosteroids-2020.1. Accessed 15 Jan 2023.
Roche N, Crichton ML, Goeminne PC, et al. Update June 2022: management of hospitalised adults with coronavirus disease 2019 (COVID-19): a European Respiratory Society living guideline. Eur Respir J. 2022;60(2):2200803. https://doi.org/10.1183/13993003.00803-2022. (PMID: 35710264).
EMA. https://www.ema.europa.eu/en/news/ema-endorses-use-dexamethasone-covid-19-patients-oxygen-mechanical-ventilation. Accessed 15 Jan 2023.
IDSA. https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/#nullCOVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. Accessed 15 Jan 2023.
National Institutes of Health. COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. https://www.covid19treatmentguidelines.nih.gov/. Accessed 15 Jan 2023.
Uyeki TM, Bernstein HH, Bradley JS, et al. Clinical practice guidelines by the infectious diseases society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenza. Clin Infect Dis. 2019;68(6):e1–47. https://doi.org/10.1093/cid/ciy866.
Chaudhuri D, Sasaki K, Karkar A, et al. Corticosteroids in COVID-19 and non-COVID-19 ARDS: a systematic review and meta-analysis. Intensive Care Med. 2021;47(5):521–37.
Lin P, Zhao Y, Li X, et al. Decreased mortality in acute respiratory distress syndrome patients treated with corticosteroids: an updated meta-analysis of randomised clinical trials with trial sequential analysis. Crit Care. 2021;25(1):122. https://doi.org/10.1186/s13054-021-03546-0. (PMID: 33771216).
Chang X, Li S, Fu Y, et al. Safety and efficacy of corticosteroids in ARDS patients: a systematic review and meta-analysis of RCT data. Respir Res. 2022;23(1):301. https://doi.org/10.1186/s12931-022-02186-4. (PMID: 36333729).
Villar J, Ferrando C, Martınez D, et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med. 2020;8(3):267–76. https://doi.org/10.1016/S2213-2600(19)30417-5.
Annane D, Pastores SM, Rochwerg B, et al. Guidelines for the diagnosis and management of critical illness-related corticosteroid insufficiency (CIRCI) in critically ill patients (Part I): society of critical care medicine (SCCM) and European Society of Intensive Care Medicine (ESICM) 2017. Intensive Care Med. 2017;43(12):1751–63. https://doi.org/10.1007/s00134-017-4919-5.
Griffiths MJ, McAuley DF, Perkins GD, et al. Guidelines on the management of acute respiratory distress syndrome. BMJ Open Respir Res. 2019;6: e000420.
Papazian L, Aubron C, Brochard L, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019;9(1):69. https://doi.org/10.1186/s13613-019-0540-9. (PMID: 31197492).
Tasaka S, Ohshimo S, Takeuchi M, on behalf of the ARDS Clinical Practice Guideline 2021 committee from the Japanese Society of Intensive Care Medicine, the Japanese Respiratory Society, and the Japanese Society of Respiratory Care Medicine, et al. ARDS clinical practice guideline 2021. J Intensive Care. 2022;10(1):32. https://doi.org/10.1186/s40560-022-00615-6. (PMID: 35799288).
Liang H, Song H, Zhai R, et al. Corticosteroids for treating sepsis in adult patients: a systematic review and meta-analysis. Front Immunol. 2021;12:709155. https://doi.org/10.3389/fimmu.2021.709155. (PMID: 34484209).
Raghu G, Remy-Jardin M, Richeldi L, et al. Idiopathic pulmonary fibrosis (an update) and progressive pulmonary fibrosis in adults: an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2022;205(9):e18–47. https://doi.org/10.1164/rccm.202202-0399ST. (PMID: 35486072).
Nasser M, Larrieu S, Si-Mohamed S, et al. Progressive fibrosing interstitial lung disease: a clinical cohort (the PROGRESS® study). Eur Respir J. 2021;57(2):2002718. https://doi.org/10.1183/13993003.02718-2020. (PMID: 32943410).
Kreuter M, Polke M, Walsh SLF, et al. Acute exacerbation of idiopathic pulmonary fibrosis: international survey and call for harmonisation. Eur Respir J. 2020;55:1901760. https://doi.org/10.1183/13993003.01760-2019.
Adams CJ, Chohan K, Rozenberg D, et al. Feasibility and outcomes of a standardized management protocol for acute exacerbation of interstitial lung disease. Lung. 2021;199(4):379–87. https://doi.org/10.1007/s00408-021-00463-5. (PMID: 34347146).
Anan K, Kataoka Y, Ichikado K, et al. Early corticosteroid dose tapering in patients with acute exacerbation of idiopathic pulmonary fibrosis. Respir Res. 2022;23(1):291. https://doi.org/10.1186/s12931-022-02195-3. (PMID: 36289512).
Yamazaki R, Nishiyama O, Saeki S, et al. Initial therapeutic dose of corticosteroid for an acute exacerbation of IPF is associated with subsequent early recurrence of another exacerbation. Sci Rep. 2021;11:5782.
Lim WS, Baudouin SV, George RC, Pneumonia Guidelines Committee of the BTS Standards of Care Committee, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64(Suppl 3):iii1-55. https://doi.org/10.1136/thx.2009.121434.
Menéndez R, Torres A, Asp J, et al. Community-Acquired Pneumonia. New Guidelines of the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) Neumología adquirida en la comunidad. Nueva normativa de la Sociedad Española de Neumología y Cirugía Torácica (SEPAR). Arch Bronconeumol. 2010;46(10):543–58.
Boyles TH, Brink A, Calligaro GL, et al. South African guideline for the management of community-acquired pneumonia in adults. J Thorac Dis. 2017;9:1469–502.
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia an Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45–67. https://doi.org/10.1164/rccm.201908-1581ST. (PMID: 31573350).
Martin-Loeches I, Torres A, Nagavci B, et al. ERS/ESICM/ESCMID/ALAT guidelines for the management of severe community-acquired pneumonia. Eur Respir J. 2023;61(4):2200735. https://doi.org/10.1183/13993003.00735-2022. (PMID: 37012080).
Meduri GU, Shih MC, Bridges L, on behalf of the ESCAPe Study Group, et al. Low-dose methylprednisolone treatment in critically ill patients with severe community-acquired pneumonia. Intensive Care Med. 2022;48(8):1009–23. https://doi.org/10.1007/s00134-022-06684-3. (PMID: 35723686).
Dequin PF, Meziani F, Quenot JP, on behalf of the CRICS-TriGGERSep Network, et al. Hydrocortisone in severe community-acquired pneumonia. N Engl J Med. 2023. https://doi.org/10.1056/NEJMoa2215145. (PMID: 36942789).
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease. Updated 2023. http://www.goldcopd.org/uploads/users/files/GOLD_Report.pdf. Accessed 12 Jan 2023
Wedzicha JA, Miravitlles M, Hurst JR, et al. Management of COPD exacerbations: an ERS/ATS guideline. Eur Respir J. 2017;49:1600791.
NICE. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Evidence reviews for the length of corticosteroid use during exacerbations NICE guideline NG115 2019. https://www.nice.org.uk/guidance/ng115/evidence/j-length-of-corticosteroid-use-during-exacerbations-pdf-237699674965. Accessed 12 Jan 2023.
Canadian Respiratory Guidelines. COPD action plan. https://cts-sct.ca/wp-content/uploads/2019/03/5491_THOR_COPDActionPlanUpdate_2019_Editable_Eng_v2.pdf. Accessed 12 Jan 2023.
Japanese Respiratory Society. Guidelines for the Diagnosis and Treatment of COPD. 3rd edition. 2010. http://www.jrs.or.jp/uploads/uploads/files/photos/765.pdf 61. Accessed 12 Jan 2023.
Thoracic Society of Australia and New Zealand. The COPD-X plan. http://copdx.org.au/copd-x-plan/. Accessed 12 Jan 2023.
Miravitlles M, Calle M, Molina J, for the Spanish Guideline for COPD (GesEPOC), et al. Spanish COPD guidelines (GesEPOC) 2021: updated pharmacological treatment of stable COPD. Arch Bronconeumol. 2022;58:T69–81.
Li L, Zhao N, Ma X, et al. Personalized variable vs fixed-dose systemic corticosteroid therapy in hospitalized patients with acute exacerbations of COPD: a prospective, multicenter, randomized, open-label clinical trial. Chest. 2021;160(5):1660–9. https://doi.org/10.1016/j.chest.2021.05.024. (PMID: 34023318).
Sivapalan P, Lapperre TS, Janner J, et al. Eosinophil-guided corticosteroid therapy in patients admitted to hospital with COPD exacerbation (CORTICO-COP): a multicentre, randomised, controlled, open-label, non-inferiority trial. Lancet Respir Med. 2019;7(8):699–709.
Global Initiative for Asthma. Global strategy for asthma management and prevention. Available from https://ginasthma.org/wp-content/uploads/2021/04/GINA-2021-MainReport_FINAL_21_04_28-WMS.pdf. Accessed 24 Jan 2023
Kwon JW, Kim MA, Sim DW, on behalf of the Korean Academy of Asthma, Allergy, and Clinical Immunology (KAAACI), the Working Group on Severe Asthma, et al. Prescription patterns of oral corticosteroids for asthma treatment and related asthma phenotypes in University Hospitals in Korea. Allergy Asthma Immunol Res. 2022;14(3):300–13. https://doi.org/10.4168/aair.2022.14.3.300. (PMID: 35557495).
Wang E, Wechsler ME, Tran TN, et al. Characterization of severe asthma worldwide: data from the International Severe Asthma Registry. Chest. 2020;157(4):790–804.
Menzies-Gow A, Gurnell M, Heaney LG, et al. Oral corticosteroid elimination via a personalised reduction algorithm in adults with severe, eosinophilic asthma treated with benralizumab (PONENTE): a multicentre, open-label, single-arm study. Lancet Respir Med. 2022;10(1):47–58. https://doi.org/10.1016/S2213-2600(21)00352-0. (PMID: 34619104).
Menzies-Gow A, Gurnell M, Heaney LG, et al. Adrenal function recovery after durable oral corticosteroid sparing with benralizumab in the PONENTE study. Eur Respir J. 2022;60:2103226. https://doi.org/10.1183/13993003.03226-2021.
Rothe T, Spagnolo P, Bridevaux PO, et al. Diagnosis and management of asthma—the Swiss Guidelines. Respiration. 2018;95(5):364–80. https://doi.org/10.1159/000486797. (PMID: 29614508).
Paton J, White J, Annandale J, et al. British guideline on the management of asthma. London: British Thoracic Society and Scottish Intercollegiate Guideline Network; 2019.
Ramsahai JM, Hansbro PM, Wark PAB. Mechanisms and management of asthma exacerbations. Am J Respir Crit Care Med. 2019;199(4):423–32. https://doi.org/10.1164/rccm.201810-1931CI. (PMID: 30562041).
Nakamura Y, Tamaoki J, Nagase H, on behalf of the Japanese Society of Allergology, et al. Japanese guidelines for adult asthma 2020. Allergol Int. 2020;69(4):519–48. https://doi.org/10.1016/j.alit.2020.08.001. (PMID: 32893125).
NHLBI Asthma Management Guidelines: Focused Updates 2020. https://www.nhlbi.nih.gov/health-topics/asthma-management-guidelines-2020-updates. Accessed 23 Jan 2023.
Blakey J, Chung LP, McDonald VM, et al. Oral corticosteroids stewardship for asthma in adults and adolescents: A position paper from the Thoracic Society of Australia and New Zealand. Respirology. 2021;26(12):1112–30. https://doi.org/10.1111/resp.14147. (PMID: 34587348).
Nan C, Schmidt O, Lindner R, et al. German regional variation of acute and high oral corticosteroid use for asthma. J Asthma. 2022;59(4):791–800. https://doi.org/10.1080/02770903.2021.1878532. (PMID: 33492176).
Bourdin A, Fabry-Vendrand C, Ostinelli J, et al. The burden of severe asthma in France: a case–control study using a medical claims database. J Allergy Clin Immunol Pract. 2019;7:1477–87.
Hew M, McDonald VM, Bardin PG, et al. Cumulative dispensing of high oral corticosteroid doses for treating asthma in Australia. Med J Aust. 2020;213(7):316–20. https://doi.org/10.5694/mja2.50758.
Suehs C, Menzies-Gow A, Price D, et al. Expert consensus on the tapering of oral corticosteroids for the treatment of asthma: a Delphi study. Am J Respir Crit Care Med. 2020;203:871. https://doi.org/10.1164/rccm.202007-27210.
Gallagher NE, Hanratty CE, Humbert M, et al. Biomarker-based corticosteroid adjustment in severe asthma: a modified Delphi consensus. ERJ Open Res. 2018;4(4):00081–2018. https://doi.org/10.1183/23120541.00081-2018. (PMID: 30538996).
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contribution
All named authors contributed equally to the final paper, including study conception and design, review of the searched literature, and drafting of the manuscript. All authors contributed to the revision and approved the final version.
Disclosures
Andrea S. Melani, Sara Croce, Lucia Cassai, Giusy Montuori, Gaia Fabbri, Maddalena Messina, Magda Viani and Elena Bargagli have nothing to disclose
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Melani, A.S., Croce, S., Cassai, L. et al. Systemic Corticosteroids for Treating Respiratory Diseases: Less Is Better, but… When and How Is It Possible in Real Life?. Pulm Ther 9, 329–344 (2023). https://doi.org/10.1007/s41030-023-00227-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-023-00227-x