Abstract
Purpose
Interval cytoreduction (IC) after a course of neoadjuvant chemotherapy is the preferentially followed management for advanced epithelial ovarian cancers. When planning an interval cytoreduction, it is important to assess the probability of achieving optimal surgery so as to avoid futile laparotomies. Several assessment techniques like CECT of the abdomen and pelvis, tumour marker-based response assessment and diagnostic laparoscopy are being used for this purpose with varying results. In our institute, we evaluated the utility of CA-125 value to predict the possibility of optimal surgery in advanced carcinoma ovary after neoadjuvant chemotherapy (NACT).
Methods
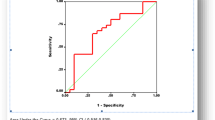
The data of treated advanced epithelial ovarian cancer were collected from the hospital records for the study period between February 2015 and February 2018 (n = 83). The cut-off value and percentage reduction of CA 125 in predicting optimal cytoreduction were analysed by receiver operator curve (ROC). These values were validated prospectively from March 2018 to September 2019 in 60 cases treated during this period. Statistical analysis was performed using SPSS 25.
Results
ROC analysis revealed CA-125 value of 88.5 U/ml (i.e. twice the upper limit of normal value) had sensitivity of 100% and specificity of 94% (AUC = 0.98; P value < 0.001) to predict optimal cytoreduction. Similarly, 90.46% reduction in CA-125 value had a sensitivity of 72% and specificity of 71% (AUC = 0.72; P value = 0.047) to predict optimal IC. In the prospective validation, among those who had post-NACT CA-125 value of less than twice the upper limit of normal value, 98.14% (53 out of 54) had optimal surgery with a P value of 0.0001. Among those with more than 90% reduction in CA 125 value after neoadjuvant chemotherapy 94.8% (55 out of 58) had optimal cytoreduction (P value—0.012).
Conclusion
The post-chemo CA 125 value and percentage reduction of CA 125 after neoadjuvant chemotherapy have high sensitivity and positive predictive value in predicting optimal interval cytoreduction.


Similar content being viewed by others
References
Rauh-Hain J et al. Ovarian cancer screening and early detection in the general population. PubMed - NCBI [Internet]. [cited 2019 Dec 6]. https://www.ncbi.nlm.nih.gov/pubmed/21629494.
Gómez-Hidalgo NR, Martinez-Cannon BA, Nick AM, Lu KH, Sood AK, Coleman RL, et al. Predictors of optimal cytoreduction in patients with newly diagnosed advanced-stage epithelial ovarian cancer: time to incorporate laparoscopic assessment into the standard of care. Gynecol Oncol. 2015;137:553.
Seigel R et al. Cancer Statistics, 2017. PubMed - NCBI [Internet]. [cited 2019 Dec 6]. https://www.ncbi.nlm.nih.gov/pubmed/28055103.
Chang L-C, Huang C-F, Lai M-S, Shen L-J, Wu F-LL, Cheng W-F. Prognostic factors in epithelial ovarian cancer: a population-based study. PLoS ONE. 2018;13(3):e0194993.
Nelson BE et al. Preoperative abdominopelvic computed tomographic prediction of optimal cytoreduction in epithelial ovarian carcinoma. PubMed - NCBI [Internet]. [cited 2020 Jan 21]. https://www.ncbi.nlm.nih.gov/pubmed/8418230.
Ferrandina G, Sallustio G, Fagotti A, Vizzielli G, Paglia A, Cucci E, et al. Role of CT scan-based and clinical evaluation in the preoperative prediction of optimal cytoreduction in advanced ovarian cancer: a prospective trial. Br J Cancer. 2009;101:1066–73.
Fagotti A et al. Introduction of staging laparoscopy in the management of advanced epithelial ovarian, tubal and peritoneal cancer: impact on prognosis in a single. PubMed - NCBI [Internet]. [cited 2020 Jan 21]. https://www.ncbi.nlm.nih.gov/pubmed/23938372.
Rutten MJ, van Meurs HS, van de Vrie R, Gaarenstroom KN, Naaktgeboren CA, van Gorp T, et al. Laparoscopy to predict the result of primary cytoreductive surgery in patients with advanced ovarian cancer: a randomized controlled trial. J Clin Oncol. 2017. https://doi.org/10.1200/jco.2016.69.2962.
Gupta M, Patel SM, Arora R, Tiwari R, Dave P, Desai A, et al. Does preoperative CA-125 cutoff value and percent reduction in CA-125 levels correlate with surgical and survival outcome after neoadjuvant chemotherapy in patients with advanced-stage ovarian cancer? Our experience from a tertiary cancer institute. South Asian J Cancer. 2020;9:30.
Can the preoperative Ca-125 level predict optimal cytoreduction in patients with advanced ovarian carcinoma? A single institution cohort study | Request PDF [Internet]. ResearchGate. [cited 2020 Jan 21]. https://www.researchgate.net/publication/23716664_Can_the_preoperative_Ca-125_level_predict_optimal_cytoreduction_in_patients_with_advanced_ovarian_carcinoma_A_single_institution_cohort_study.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumar, D.S., Noushad, S.N., Anandh, S.M. et al. CA-125 Levels Predict Optimal Surgery in Carcinoma Ovary: A Retrospective Analysis with Prospective Validation. Indian J Gynecol Oncolog 18, 51 (2020). https://doi.org/10.1007/s40944-020-00398-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-020-00398-4