Abstract
Purpose
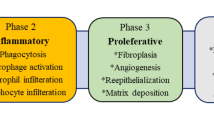
Wound healing is a biological process that plays an important role in tissue recovery and reconstruction of damaged tissues. Although there are several advances in the area of wound healing, chronic wounds still continue as one of the major threats in individuals suffering from long term injuries. At present, natural components that are derived from natural resources have been studied for their efficacy in treating chronic wounds. They have been reported to have unique properties such as biocompatibility, biodegradability, and low immunogenicity making them suitable candidates for wound treatment.
Methods
The review investigated the use of natural products as wound dressing materials for treating acute and chronic wounds.
Results
An ideal wound dressing material should promote quick wound recovery and attempt to restore day-to-day activities of individual’s suffering from chronic wounds. Recently, biomaterials are being widely used for medical purposes because of their biodegradable and non-toxic features. They have shown great promise in treating different types of wounds and for achieving efficient tissue repair.
Conclusion
Natural biomaterials derived from natural resources are well-researched and reviewed for their effectiveness in treating chronic wounds and to understand how they could speed up the healing process. The study of natural biomaterials used as wound dressings has drawn particular interest due to their propensity to stimulate the growth of new tissues. A variety of naturally-occurring polymers, including gelatin, alginate, silk, chitosan, elastin, pectin, and fibrin, have a major role in expediting the healing of wounds.
Lay Summary
Wound is an injury that results from the damage caused by an external or internal rupture in the human tissues or organs. Wound dressing materials that are prepared using natural resources are beneficial in treating acute and chronic wounds.
Graphical Abstract
Schematic representation showing the different forms of wound dressing materials that can fabricated using natural polymers.






Similar content being viewed by others
References
Boateng J, Catanzano O. Advanced therapeutic dressings for effective wound healing—a review. J Pharm Sci. 2015:3653–80. https://doi.org/10.1002/jps.24610.
Bowler PG, Duerden BI, Armstrong DG. Wound microbiology and associated approaches to wound management. Clin microbiol rev. 2001;14:244–69. https://doi.org/10.1128/CMR.14.2.244-269.20.
Davenport M, Dickinson LE. Engineered biomaterials for chronic wound healing. Chronic Wounds, Wound Dress Wound Heal. 2018:51–74. https://doi.org/10.1007/15695_2017_92.
Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care. 2015;4:560–82. https://doi.org/10.1089/wound.2015.0635.
Frigg A, Pagenstert G, Schäfer D, Valderrabano V, Hintermann B. Recurrence and prevention of diabetic foot ulcers after total contact casting. Foot Ankle Int. 2007;28:64–9. https://doi.org/10.3113/FAI.2007.0012.
Sathyaraj WV, Prabakaran L, Bhoopathy J, Dharmalingam S, Karthikeyan R, Atchudan R. Therapeutic efficacy of polymeric biomaterials in treating diabetic wounds—an upcoming wound healing technology. Polymers. 2023;15:5–1205.
Matter MT, Probst S, Läuchli S, Herrmann IK. Uniting drug and delivery: metal oxide hybrid nanotherapeutics for skin wound care. Pharmaceutics. 2020:12. https://doi.org/10.3390/pharmaceutics12080780.
Krzyszczyk P, Schloss R, Palmer A, Berthiaume F. The role of macrophages in acute and chronic wound healing and interventions to promote pro-wound healing phenotypes. Front Physiol. 2018;9:419. https://doi.org/10.3389/fphys.2018.00419.
Schultz GS, Chin GA, Moldawer L, Diegelmann RF. Principles of wound healing. In: Fitridge R, Thompson M, editors. Mechanisms of Vascular Disease: A Reference Book for Vascular Specialists. Adelaide (AU): University of Adelaide Press. https://www.ncbi.nlm.nih.gov/pubmed/30485016.
Cañedo-Dorantes L. Cañedo-Ayala M. Skin acute wound healing: a comprehensive review. Int J Inflam. 2019;2019:3706315. https://doi.org/10.1155/2019/3706315.
Bhoopathy J, Dharmalingam S, Sathyaraj WV, Rajendran S, Rymbai S, Senthil R, Atchudan R. Sericin/human placenta-derived extracellular matrix scaffolds for cutaneous wound treatment—preparation, characterization, in vitro and in vivo analyses. Pharmaceutics. 2023;15: 2:362.
Jayavardhini B, Pravin YR, Kumar C, Murugesan R, Vedakumari SW. Graphene oxide impregnated sericin/collagen scaffolds–fabrication and characterization. Mater Lett. 2022;15:307–131060.
Vedakumari WS, Ayaz N, Karthick AS, Senthil R, Sastry TP. Quercetin impregnated chitosan–fibrin composite scaffolds as potential wound dressing materials—fabrication, characterization and in vivo analysis. Eur J Pharm Sci. 2017;97:106–12.
Rymbai S, Jayavardhini B, Kumar C, Lokesh P, Pravin YR, Vedakumari SW. Effect of quercetin incorporated silk sericin/gelatin scaffolds in wound healing. Chettinad Health City Med J. 9(1)
Soubhagya AS, Moorthi A, Prabaharan M. Preparation and characterization of chitosan/pectin/ZnO porous films for wound healing. Int J Biol Macromol. 2020;157:135–45. https://doi.org/10.1016/j.ijbiomac.2020.04.156.
Maeda M, Kadota K, Kajihara M, Sano A, Fujioka K. Sustained release of human growth hormone (hGH) from collagen film and evaluation of effect on wound healing in db/db mice. J Control Release. 2001;77:261–72. https://doi.org/10.1016/S0168-3659(01)00512-0.
Gopinath D, Ahmed MR, Gomathi K, Chitra K, Sehgal PK, Jayakumar R. Dermal wound healing processes with curcumin incorporated collagen films. Biomater. 2004;25:1911–7. https://doi.org/10.1016/S0142-9612(03)00625-2.
Deepachitra R, Ramnath V, Sastry TP. Graphene oxide incorporated collagen–fibrin biofilm as a wound dressing material. RSC Adv. 2014;4:62717–27. https://doi.org/10.3390/ma12101628.
Feng A, Borrelli M, Meyer-ter-Vehn T, Reichl S, Schrader S, Geerling G. Epithelial wound healing on keratin film, amniotic membrane and polystyrene in vitro. Curr Eye Res. 2014;39:561–70. https://doi.org/10.3109/02713683.2013.853804.
Tanabe T, Okitsu N, Tachibana A, Yamauchi K. Preparation and characterization of keratin–chitosan composite film. Biomater. 2002;23:817–25. https://doi.org/10.1016/S0142-9612(01)00187-9.
Shah A, Ali Buabeid M, Arafa E-SA, Hussain I, Li L, Murtaza G. The wound healing and antibacterial potential of triple-component nanocomposite (chitosan-silver-sericin) films loaded with moxifloxacin. Int J Pharm. 2019;564:22–38. https://doi.org/10.1016/j.ijpharm.2019.04.046.
Pei HN, Chen XG, Li Y, Zhou HY. Characterization and ornidazole release in vitro of a novel composite film prepared with chitosan/poly (vinyl alcohol)/alginate. J Biomed Mater Res A. 2008;85:566–72. https://doi.org/10.1002/jbm.a.31223.
Tyeb S, Kumar N, Kumar A, Verma V. Flexible agar-sericin hydrogel film dressing for chronic wounds. Carbohydr Polym. 2018;200:572–82. https://doi.org/10.1016/j.carbpol.2018.08.030.
Siqueira P, Siqueira É, de Lima AE, Siqueira G, Pinzón-Garcia AD, Lopes AP, et al. Three-dimensional stable alginate-nanocellulose gels for biomedical applications: towards tunable mechanical properties and cell growing. Nanomater. 2019:9. https://doi.org/10.3390/nano9010078.
Ehterami A, Salehi M, Farzamfar S, Samadian H, Vaez A, Ghorbani S, et al. Chitosan/alginate hydrogels containing Alpha-tocopherol for wound healing in rat model. J Drug Deliv Sci Technol. 2019;51:204–13. https://doi.org/10.1016/j.jddst.2019.02.032.
Shihara M, Nakanishi K, Ono K, Sato M, Kikuchi M, Saito Y, et al. Photocrosslinkable chitosan as a dressing for wound occlusion and accelerator in healing process. Biomater. 2002;23:833–40. https://doi.org/10.1016/S0142-9612(01)00189-2.
Ribeiro MP, Espiga A, Silva D, Baptista P, Henriques J, Ferreira C, et al. Development of a new chitosan hydrogel for wound dressing. Wound Repair Regen. 2009;17:817–24. https://doi.org/10.1111/j.1524-475X.2009.00538.x.
Moraes PR, Saska S, Barud H, Lima LR, Martins VD, Plepis AM, et al. Bacterial cellulose/collagen hydrogel for wound healing. Mater Res. 2016;19:106–16. https://doi.org/10.1590/1980-5373-MR-2015-0249.
Zhang X, Yin Z, Guo Y, Huang H, Zhou J, Wang L, et al. A facile and large-scale synthesis of a PVA/chitosan/collagen hydrogel for wound healing. New J Chem. 2020;44:20776–84. https://doi.org/10.1039/D0NJ04016A.
Giusto G, Vercelli C, Comino F, Caramello V, Tursi M, Gandini M. A new, easy-to-make pectin-honey hydrogel enhances wound healing in rats. BMC Complement Altern Med. 2017;17:266. https://doi.org/10.1186/s12906-017-1769-1.
Kim J, Lee C-M. Wound healing potential of a polyvinyl alcohol-blended pectin hydrogel containing Hippophae rahmnoides L. extract in a rat model. Int J Biol Macromol. 2017;99:586–93. https://doi.org/10.1016/j.ijbiomac.2017.03.014.
Noorjahan SE, Sastry TP. An in vivo study of hydrogels based on physiologically clotted fibrin-gelatin composites as wound-dressing materials. J Biomed Mater Res B Appl Biomater. 2004;71:305–12. https://doi.org/10.1002/jbm.b.30094.
Gil J, Natesan S, Li J, Valdes J, Harding A, Solis M, et al. A PEGylated fibrin hydrogel-based antimicrobial wound dressing controls infection without impeding wound healing. Int Wound J. 2017;14:1248–57. https://doi.org/10.1111/iwj.12791.
Park M, Shin HK, Kim B-S, Kim MJ, Kim I-S, Park B-Y, et al. Effect of discarded keratin-based bio composite hydrogels on the wound healing process in vivo. Mater Sci Eng C Mater Biol Appl. 2015;55:88–94. https://doi.org/10.1016/j.msec.2015.03.033.
Kumaran P, Gupta A, Sharma S. Synthesis of wound-healing keratin hydrogels using chicken feathers proteins and its properties. Int J Pharm Pharm Sci. 2017;9(171) https://doi.org/10.22159/IJPPS.2017V9I2.15620.
Xue R, Liu Y, Zhang Q, Liang C, Qin H, Liu P, et al. Shape changes and interaction mechanism of Escherichia coli cells treated with sericin and use of a sericin-based hydrogel for wound healing. Appl Environ Microbiol. 2016;82:4663–72. https://doi.org/10.1128/AEM.00643-16.
Verma J, Kanoujia J, Parashar P, Tripathi CB, Saraf SA. Wound healing applications of sericin/chitosan-capped silver nanoparticles incorporated hydrogel. Drug Deliv Transl Res. 2017;7:77–88. https://doi.org/10.1007/s13346-016-0322-y.
Baptista-Silva S, Bernardes BG, Borges S, Rodrigues I, Fernandes R, Gomes-Guerreiro S, Pinto MT, Pintado M, Soares R, Costa R, Oliveira AL. Exploring silk sericin for diabetic wounds: an in situ-forming hydrogel to protect against oxidative stress and improve tissue healing and regeneration. Biomol. 2022;8(12):801.
Gallardo-Rivera R, de Los Ángeles Aguilar-Santamaría M, Silva-Bermúdez P, García-López J, Tecante A, Velasquillo C, et al. Polyelectrolyte complex of Aloe vera, chitosan, and alginate produced fibroblast and lymphocyte viabilities and migration. Carbohydr Polym. 2018;192:84–94. https://doi.org/10.1016/j.carbpol.2018.03.044.
Alemdaroğlu C, Değim Z, Celebi N, Zor F, Oztürk S, Erdoğan D. An investigation on burns wound healing in rats with chitosan gel formulation containing epidermal growth factor. Burns. 2006;32:319–27. https://doi.org/10.1016/j.burns.2005.10.015.
Değim Z, Celebi N, Sayan H, Babül A, Erdoğan D, Take G. An investigation on skin wound healing in mice with a taurine-chitosan gel formulation. Amino Acids. 2002;22:187–98. https://doi.org/10.1007/s007260200007.
Jridi M, Bardaa S, Moalla D, Rebaii T, Souissi N, Sahnoun Z, Nasri M. Microstructure, rheological and wound healing properties of collagen-based gel from cuttlefish skin. Int J Biol Macromol. 2015;77:369–74.
Ersel M, Uyanikgil Y, Karbek Akarca F, Ozcete E, Altunci YA, Karabey F, et al. Effects of silk sericin on incision wound healing in a dorsal skin flap wound healing rat model. Med Sci Monit. 2016;22:1064–78. https://doi.org/10.12659/MSM.897981.
Yang M, Wang Y, Tao G, Cai R, Wang P, Liu L, et al. Fabrication of sericin/agrose gel loaded lysozyme and its potential in wound dressing application. Nanomater. 2018:8. https://doi.org/10.3390/nano8040235.
Ureña-Benavides EE, Brown PJ, Kitchens CL. Effect of jet stretch and particle load on cellulose nanocrystal-alginate nanocomposite fibers. Langmuir. 2010;26:14263–70. https://doi.org/10.1021/la102216v.
Abdel-Mohsen AM, Frankova J, Abdel-Rahman RM, Salem AA, Sahffie NM, Kubena I, et al. Chitosan-glucan complex hollow fibers reinforced collagen wound dressing embedded with aloe vera. II. Multifunctional properties to promote cutaneous wound healing. Int J Pharm. 2020;582:119349. https://doi.org/10.1016/j.ijpharm.2020.119349.
Sapru S, Das S, Mandal M, Ghosh AK, Kundu SC. Prospects of nonmulberry silk protein sericin-based nanofibrous matrices for wound healing – in vitro and in vivo investigations. Acta Biomater. 2018;78:137–50.
Zhao R, Li X, Sun B, Tong Y, Jiang Z, Wang C. Nitrofurazone-loaded electrospun PLLA/sericin-based dual-layer fiber mats for wound dressing applications. RSC Adv. 2015;5:16940–9. https://doi.org/10.1039/C4RA16208K.
Boateng J, Burgos-Amador R, Okeke O, Pawar H. Composite alginate and gelatin based bio-polymeric wafers containing silver sulfadiazine for wound healing. Int J Biol Macromol. 2015;79:63–71. https://doi.org/10.1016/j.ijbiomac.2015.04.048.
Ahmed A, Getti G, Boateng J. Ciprofloxacin-loaded calcium alginate wafers prepared by freeze-drying technique for potential healing of chronic diabetic foot ulcers. Drug Deliv Transl Res. 2018;8:1751–68. https://doi.org/10.1007/s13346-017-0445-9.
Moura LIF, Dias AMA, Leal EC, Carvalho L, de Sousa HC, Carvalho E. Chitosan-based dressings loaded with neurotensin--an efficient strategy to improve early diabetic wound healing. Acta Biomater. 2014;10:843–57. https://doi.org/10.1016/j.actbio.2013.09.040.
Afewerki S, Sheikhi A, Kannan S, Ahadian S, Khademhosseini A. Gelatin-polysaccharide composite scaffolds for 3D cell culture and tissue engineering: towards natural therapeutics. Bioeng Transl Med. 2019;4:96–115. https://doi.org/10.1002/btm2.10124.
Duconseille A, Astruc T, Quintana N, Meersman F, Sante-Lhoutellier V. Gelatin structure and composition linked to hard capsule dissolution: a review. Food Hydrocolloids. 2015:360–76. https://doi.org/10.1016/j.foodhyd.2014.06.006.
Kang H-W, Tabata Y, Ikada Y. Fabrication of porous gelatin scaffolds for tissue engineering. Biomater. 1999:1339–44. https://doi.org/10.1016/s0142-9612(99)00036-8.
Chen H, Guo L, Wicks J, Ling C, Zhao X, Yan Y, et al. Quickly promoting angiogenesis by using a DFO-loaded photo-crosslinked gelatin hydrogel for diabetic skin regeneration. J Mater Chem B Mater Biol Med. 2016;4:3770–81. https://doi.org/10.1039/c6tb00065g.
Zheng Y, Yuan W, Liu H, Huang S, Bian L, Guo R. Injectable supramolecular gelatin hydrogel loading of resveratrol and histatin-1 for burn wound therapy. Biomater Sci. 2020;8:4810–20. https://doi.org/10.1039/d0bm00391c.
Varaprasad K, Jayaramudu T, Kanikireddy V, Toro C, Sadiku ER. Alginate-based composite materials for wound dressing application: a mini review. Carbohydr Polym. 2020;236:116025. https://doi.org/10.1016/j.carbpol.2020.116025.
Lee KY, Mooney DJ. Alginate: properties and biomedical applications. Prog Polym Sci. 2012;37:106–26. https://doi.org/10.1016/j.progpolymsci.2011.06.003.
Goh CH, Heng PWS, Chan LW. Alginates as a useful natural polymer for microencapsulation and therapeutic applications. Carbo Polym. 2012:1–12. https://doi.org/10.1016/j.carbpol.2011.11.012.
Sun J, Tan H. Alginate-based biomaterials for regenerative medicine applications. Materials. 2013;6:1285–309. https://doi.org/10.3390/ma6041285.
Karri VVSR, Karri VVS, Kuppusamy G, Talluri SV, Mannemala SS, Kollipara R, et al. Curcumin loaded chitosan nanoparticles impregnated into collagen-alginate scaffolds for diabetic wound healing. Int J Bio Macromol. 2016:1519–29. https://doi.org/10.1016/j.ijbiomac.2016.05.038.
Mndlovu H, du Toit LC, Kumar P, Marimuthu T, Kondiah PPD, Choonara YE, et al. Development of a fluid-absorptive alginate-chitosan bioplatform for potential application as a wound dressing. Carbohydr Polym. 2019;222:114988. https://doi.org/10.1016/j.carbpol.2019.114988.
Sarika PR, James NR. Polyelectrolyte complex nanoparticles from cationised gelatin and sodium alginate for curcumin delivery. Carbohydr Polym. 2016;148:354–61. https://doi.org/10.1016/j.carbpol.2016.04.073.
Shankar S, Kasapis S, Rhim J-W. Alginate-based nanocomposite films reinforced with halloysite nanotubes functionalized by alkali treatment and zinc oxide nanoparticles. Int J Biol Macromol. 2018;118:1824–32. https://doi.org/10.1016/j.ijbiomac.2018.07.026.
Altman GH, Diaz F, Jakuba C, Calabro T, Horan RL, Chen J, et al. Silk-based biomaterials. Biomaterials. 2003:401–16. https://doi.org/10.1016/s0142-9612(02)00353-8.
Park YR, Sultan MT, Park HJ, Lee JM, Ju HW, Lee OJ, et al. NF-κB signaling is key in the wound healing processes of silk fibroin. Acta Biomater. 2018;67:183–95. https://doi.org/10.1016/j.actbio.2017.12.006.
Hasatsri S, Yamdech R, Chanvorachote P, Aramwit P. Physical and biological assessments of the innovative bilayered wound dressing made of silk and gelatin for clinical applications. J Biomater Appl. 2015;29:1304–13. https://doi.org/10.1177/0885328214559138.
Navone SE, Pascucci L, Dossena M, Ferri A, Invernici G, Acerbi F, et al. Decellularized silk fibroin scaffold primed with adipose mesenchymal stromal cells improves wound healing in diabetic mice. Stem Cell Res The. 2014;5:7. https://doi.org/10.1186/scrt396.
Tao G, Cai R, Wang Y, Liu L, Zuo H, Zhao P, Umar A, Mao C, Xia Q, He H. Bioinspired design of AgNPs embedded silk sericin-based sponges for efficiently combating bacteria and promoting wound healing. Mater Design. 2019;15(180):107940. https://doi.org/10.1016/j.matdes.2019.107940.
Aramwit P, Sangcakul A. The effects of sericin cream on wound healing in rats. Biosci Biotechnol Biochem. 2007;71(10):2473–7. https://doi.org/10.1271/bbb.70243.
Ersel M, Uyanikgil Y, Akarca FK, Ozcete E, Altunci YA, Karabey F, et al. Effects of silk sericin on incision wound healing in a dorsal skin flap wound healing rat model. Med Sci Monitor. 2016:1064–78. https://doi.org/10.12659/msm.897981.
Arango MC, Osorio YM, Osorno JB, Parra SB, Alvarez-López C. Effect of ethanol post-treatments over sericin scaffolds for tissue engineering applications. J Polym Environ. 2022;9:1–2. https://doi.org/10.1007/s10924-022-02647-3.
Siritienthong T, Ratanavaraporn J, Aramwit P. Development of ethyl alcohol-precipitated silk sericin/polyvinyl alcohol scaffolds for accelerated healing of full-thickness wounds. Int J Pharm. 2012;439:175–86. https://doi.org/10.1016/j.ijpharm.2012.09.043.
Patil PP, Reagan MR, Bohara RA. Silk fibroin and silk-based biomaterial derivatives for ideal wound dressings. Int Journal Biol Macromol. 2020;1(164):4613–27. https://doi.org/10.1016/j.ijbiomac.2020.08.041.
Vasconcelos A, Gomes AC, Cavaco-Paulo A. Novel silk fibroin/elastin wound dressings. Acta Biomater. 2012;8:3049–60. https://doi.org/10.1016/j.actbio.2012.04.035.
Sivashankari PR, Moorthi A, Abudhahir KM, Prabaharan M. Preparation and characterization of three-dimensional scaffolds based on hydroxypropyl chitosan-graft-graphene oxide. Int J biol macromol. 2018;110:522–30.
Jayakumar R, Reis RL, Mano JF. Chemistry and applications of phosphorylated chitin and chitosan. E-polymer 2006 [cited 2023 Jan 5];6. Available from: https://www.degruyter.com/document/doi/10.1515/epoly.2006.6.1.447/html.
Patrulea V, Ostafe V, Borchard G, Jordan O. Chitosan as a starting material for wound healing applications. Eur J Pharm Biopharm. 2015;97:417–26. https://doi.org/10.1016/j.ejpb.2015.08.004.
Shehabeldine AM, Salem SS, Ali OM, Abd-Elsalam KA, Elkady FM, Hashem AH. Multifunctional silver nanoparticles based on chitosan: antibacterial, antibiofilm, antifungal, antioxidant, and wound-healing activities. J Fungi. 2022;8(6):612. https://doi.org/10.3390/jof8060612.
Jayakumar R, Menon D, Manzoor K, Nair SV, Tamura H. Biomedical applications of chitin and chitosan-based nanomaterials—a short review. Carbohydr Polym. 2010;82:227–32.
Li X-F, Feng X-Q, Yang S, Fu G-Q, Wang T-P, Su Z-X. Chitosan kills Escherichia coli through damage to be of cell membrane mechanism. Carbohydr Polym. 2010;79:493–9.
Kaygusuz H, Torlak E, Akın-Evingür G, Özen İ, von Klitzing R, Erim FB. Antimicrobial cerium ion-chitosan crosslinked alginate biopolymer films: a novel and potential wound dressing. Int J Biol Macromol. 2017;105:1161–5. https://doi.org/10.1016/j.ijbiomac.2017.07.144.
Ma Y, Xin L, Tan H, Fan M, Li J, Jia Y, Ling Z, Chen Y, Hu X. Chitosan membrane dressings toughened by glycerol to load antibacterial drugs for wound healing. Mater Sci Eng C. 2017;1(81):522–31. https://doi.org/10.1016/j.msec.2017.08.052.
Pereira RF, Barrias CC, Bártolo PJ, Granja PL. Cell-instructive pectin hydrogels crosslinked via thiol-norbornene photo-click chemistry for skin tissue engineering. Acta Biomater. 2018;66:282–93. https://doi.org/10.1016/j.actbio.2017.11.016.
Marras-Marquez T, Peña J, Veiga-Ochoa MD. Robust and versatile pectin-based drug delivery systems. Int J Phar. 2015;479:265–76. https://doi.org/10.1016/j.ijpharm.2014.12.045.
Valle KZM, Saucedo Acuña RA, Ríos Arana JV, Lobo N, Rodriguez C, Cuevas-Gonzalez JC, et al. Natural film based on pectin and allantoin for wound healing: obtaining, characterization, and rat model. Biomed Res Int. 2020;2020:6897497. https://doi.org/10.1155/2020/6897497.
Andriotis EG, Eleftheriadis GK, Karavasili C, Fatouros DG. Development of bio-active patches based on pectin for the treatment of ulcers and wounds using 3D-bioprinting technology. Pharmaceutics. 2020;12 https://doi.org/10.3390/pharmaceutics12010056.
Almine JF, Bax DV, Mithieux SM, Nivison-Smith L, Rnjak J, Waterhouse A, et al. Elastin-based materials. Chem Soc Rev. 2010;39:3371–9. https://doi.org/10.1039/b919452p.
Rodríguez-Cabello JC, González de Torre I, Ibañez-Fonseca A, Alonso M. Bioactive scaffolds based on elastin-like materials for wound healing. Adv Drug Deliv Re. 2018;129:118–33. https://doi.org/10.1016/j.addr.2018.03.003.
Baumann L, Bernstein EF, Weiss AS, Bates D, Humphrey S, Silberberg M, Daniels R. Clinical relevance of elastin in the structure and function of skin. In: Aesthetic Surgery Journal Open Forum 2021 Sep (Vol. 3, No. 3, p. ojab019). US: Oxford University Press. https://doi.org/10.1093/asjof/ojab019.
Kawabata S, Kanda N, Hirasawa Y, Noda K, Matsuura Y, Suzuki S, Kawai K. The utility of silk-elastin hydrogel as a new material for wound healing. Plast Reconstr Surg– Glob Open. 2018;6(5) https://doi.org/10.1097/GOX.0000000000001778.
Rouse JG, Van Dyke ME. A review of keratin-based biomaterials for biomedical applications. Mater Mol Diversity Preserv Int. 2010;3:999–1014.
Yıldız A, Kara AA, Acartürk F. Peptide-protein based nanofibers in pharmaceutical and biomedical applications. Int J Biol Macromol. 2020;148:1084–97. https://doi.org/10.1016/j.ijbiomac.2019.12.275.
Esparza Y, Ullah A, Wu J. Molecular mechanism and characterization of self-assembly of feather keratin gelation. Int J Biol Macromol. 2018;107:290–6. https://doi.org/10.1016/j.ijbiomac.2017.08.168.
Hill P, Brantley H, Van Dyke M. Some properties of keratin biomaterials: kerateines. Biomaterials. 2010;31:585–93. https://doi.org/10.1016/j.biomaterials.2009.09.076.
Vakilian S, Jamshidi-adegani F, Al-Shidhani S, Anwar MU, Al-Harrasi R, Al-Wahaibi N, et al. A Keratin-based biomaterial as a promising dresser for skin wound healing. Wound Med. 2019;25:100155.
Funding
The author Weslen Vedakumari Sathyaraj acknowledges the funding support received from Chettinad Academy of Research and Education under CARE Seed Research Grant – Ref. No. 004/Regr./AR-Research/2022-03.
Author information
Authors and Affiliations
Contributions
Writing—original draft: Jayavardhini Bhoopathy and Lokesh Prabakaran
Formal analysis: Ramadoss Karthikeyan and Rethinam Senthil
Conceptualization and supervision: Weslen Vedakumari Sathyaraj
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhoopathy, J., Prabakaran, L., Sathyaraj, W.V. et al. A Comprehensive Review on Natural Therapeutics for Wound Treatment. Regen. Eng. Transl. Med. 10, 34–45 (2024). https://doi.org/10.1007/s40883-023-00314-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40883-023-00314-0