Abstract
Purpose
Current strategies implementing drug-eluting polymer stent coatings fail to fully address the lasting effects of endothelial suppression which ultimately result in delayed reendothelialization and thrombogenic complications. The present study investigates the in vitro hemocompatibility of all-trans retinoic acid–loaded poly(1,8-octanediol-co-citrate) coatings (AtRA-POC coatings) for advanced intravascular stent technology. The ability of these materials to support endothelial restoration via migration and proliferation while inhibiting smooth muscle cell growth is also explored.
Methods
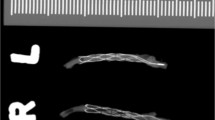
Using in vitro models, the hemocompatibility of AtRA-loaded POC-coated cobalt chromium (CoCr) vascular stents was evaluated in terms of platelet and inflammatory activity. Platelet activity was quantified by platelet adhesion and platelet activation, further supported by SEM visualization. Inflammatory activity was quantified by the production of proinflammatory cytokines by THP1 monocytes. Lastly, in vitro wound healing and 5-ethynyl-2′-deoxyuridine (EdU) and PicoGreen DNA assays were used in quantitating endothelial and smooth muscle cell migration and proliferation.
Results
Experimental examinations of platelet adhesion and activation demonstrate significant reductions in the platelet response to POC-coated AtRA-loaded stents when compared to bare CoCr stents. Such findings reveal AtRA-POC coatings to have significantly improved hemocompatibility compared to that of bare metal stents and at least as good as that of POC alone. Similarly, in reference to LPS-stimulated controls, human monocyte-like THP1 cells in culture with AtRA-POC-CoCr stents for 24 h showed reduced detection of proinflammatory cytokines, comparable to that of bare CoCr and untreated controls. This result supports AtRA-POC coatings as possessing limited immunological potential. Observations from in vitro endothelial and smooth muscle cell investigations demonstrate the ability of the drug AtRA to allow cell processes involved in restoration of the endothelium while inhibiting smooth muscle cell processes.
Conclusion
This study demonstrates AtRA-loaded POC coatings are hemocompatible and noninflammatory, and provide a promising strategy in enhancing vascular stent techniques and clinical integration. Possessing hemocompatibility and immunological compatibility that is at least as good as bare metal stents as clinical standards supports the use of AtRA-POC coatings for vascular applications. Additionally, selectively reducing smooth muscle cell proliferation while supporting endothelial cell proliferation and migration further demonstrates the potential of these materials in significantly improving the state of vascular stent technology in the area of stent thrombosis and neointimal hyperplasia.
Lay Summary
Hemocompatibility and support of endothelial cell functions are essential for advancing drug-eluting stent technology. Since vascular stents will be directly in contact with blood, the materials used for these devices must be compatible with blood components and associated cells to prevent clotting and proinflammatory events. Additionally, ideal strategies must support the restoration of surrounding vascular tissue which becomes damaged during stent implantation and is at the crux of addressing the current challenges of drug-eluting stent approaches. Thus, the present study investigates the in vitro hemocompatibility and effects on endothelial healing of all-trans retinoic acid–loaded poly(1,8-octanediol-co-citrate) coatings for advanced intravascular stent technology.









Similar content being viewed by others
Data availability
Data available upon request.
Code Availability
Not applicable.
References
Gossart A, Letourneur D, Gand A, Regnault V, Ben Mlouka MA, Cosette P, Pauthe E, Ollivier V, Santerre JP. Mitigation of monocyte driven thrombosis on cobalt chrome surfaces in contact with whole blood by thin film polar/hydrophobic/ionic polyurethane coatings. Biomaterials. 2019;217:119306.
Marti A. Cobalt-base alloys used in bone surgery. Injury. 2000;31:D18–21.
Ollivier V, Roques C, Receveur N, Gratz M, Feldman L, Letourneur D, Gachet C, Mangin PH, Jandrot-Perrus M. Bioreactivity of stent material: activation of platelets, coagulation, leukocytes and endothelial cell dysfunction in vitro. Platelets. 2016;28(6):529–39.
Thiruppathi E, Larson MK, Mani G. Surface modification of CoCr alloy using varying concentrations of phosphoric and phosphonoacetic acids: albumin and fibrinogen adsorption, platelet adhesion, activation, and aggregation studies. Langmuir. 2014;31(1):358–70.
Buccheri D, Piraino D, Andolina G, Cortese B. Understanding and managing in-stent restenosis: a review of clinical data, from pathogenesis to treatment. J Thorac Dis. 2016;8(10):E1150–62.
Stevens JR, Zamani A, Osborne JIA, Zamani R, Akrami M. Critical evaluation of stents in coronary angioplasty: a systematic review. Biomed Eng Online. 2021;20(1):46–46.
Marx SO, Totary-Jain H, Marks AR. Vascular smooth muscle cell proliferation in restenosis. Circ Cardiovasc Interv. 2011;4(1):104–11.
Moses JW, Leon MB, Popma JJ, Fitzgerald PJ, Holmes DR, O’Shaughnessy C, Caputo RP, Kereiakes DJ, Williams DO, Teirstein PS, Jaeger JL, Kuntz RE. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003;349(14):1315–23.
Stone GW, Ellis SG, Cox DA, Hermiller J, O’Shaughnessy C, Mann JT, Turco M, Caputo R, Bergin P, Greenberg J, Popma JJ, Russell ME. A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N Engl J Med. 2004;350(3):221–31.
Kounis NG, Koniari I, Roumeliotis A, Tsigkas G, Soufras G, Grapsas N, Davlouros P, Hahalis G. Thrombotic responses to coronary stents, bioresorbable scaffolds and the Kounis hypersensitivity-associated acute thrombotic syndrome. J Thorac Dis. 2017;9(4):1155–64.
Schubert SY, Benarroch A, Ostvang J, Edelman ER. Regulation of endothelial cell proliferation by primary monocytes. Arterioscler Thromb Vasc Biol. 2008;28(1):97–104.
Vieira-de-Abreu A, Campbell RA, Weyrich AS, Zimmerman GA. Platelets: versatile effector cells in hemostasis, inflammation, and the immune continuum. Semin Immunopathol. 2012;34(1):5–30.
Weber M, Steinle H, Golombek S, Hann L, Schlensak C, Wendel HP, Avci-Adali M. Blood-contacting biomaterials: in vitro evaluation of the hemocompatibility. Front Bioeng Biotechnol. 2018;6:99–99.
Motlagh D, Allen J, Hoshi R, Yang J, Lui K, Ameer G. Hemocompatibility evaluation of poly(diol citrate)in vitro for vascular tissue engineering. J Biomed Mater Res, Part A. 2007;82A(4):907–16.
Zailani MZ, Ismail AF, Sheikh Abdul Kadir SH, Othman MHD, Goh PS, Hasbullah H, Abdullah MS, Ng BC, Kamal F. Hemocompatibility evaluation of poly(1,8-octanediol citrate) blend polyethersulfone membranes. J Biomed Mater Res Part A. 2017;105(5):1510–20.
Yang J, Webb AR, Pickerill SJ, Hageman G, Ameer GA. Synthesis and evaluation of poly(diol citrate) biodegradable elastomers. Biomaterials. 2006;27(9):1889–98.
Allen J, Khan S, Lapidos KA, Ameer G, Toward engineering a human neoendothelium with circulating progenitor cells. STEM CELLS. p. N/A-N/A.; 2009
Tran RT, Yang J, Ameer GA. Citrate-based biomaterials and their applications in regenerative engineering. Annu Rev Mater Res. 2015;45:277–310.
Yang J, Webb AR, Ameer GA. Novel citric acid-based biodegradable elastomers for tissue engineering. Adv Mater. 2004;16(6):511–6.
Johst U, Betsch A, Wiskirchen J, Schöber W, Vonthein R, Rinkert N, Kehlbach R, Claussen CD, Duda SH. All-trans and 9-cis retinoid acids inhibit proliferation, migration, and synthesis of extracellular matrix of human vascular smooth muscle cells by inducing differentiation in vitro. J Cardiovasc Pharmacol. 2003;41(4):526–35.
Sugawara A. Effects of retinoids on vasculatures. J Endocrinol Thyroid Res, 2017; 2(3).
Zhang J, Deng B, Jiang X, Cai M, Liu N, Zhang S, Tan Y, Huang G, Jin W, Liu B, Liu S. All-trans-retinoic acid suppresses neointimal hyperplasia and inhibits vascular smooth muscle cell proliferation and migration via activation of AMPK signaling pathway. Front Pharmacol. 2019;10:485–485.
Axel DI, Frigge A, Dittmann J, Runge H, Spyridopoulos I, Riessen R, Viebahn R, Karsch KR. All-trans retinoic acid regulates proliferation, migration, differentiation, and extracellular matrix turnover of human arterial smooth muscle cells. Cardiovasc Res. 2001;49(4):851–62.
Leville CD, Dassow MS, Seabrook GR, Jean-Claude JM, Towne JB, Cambria RA. All-trans-retinoic acid decreases vein graft intimal hyperplasia and matrix metalloproteinase activity in vivo. J Surg Res. 2000;90(2):183–90.
Bouriez D, Giraud J, Gronnier C, Varon C. Efficiency of all-trans retinoic acid on gastric cancer: a narrative literature review. Int J Mol Sci. 2018;19(11).
Giuli MV, Hanieh PN, Giuliani E, Rinaldi F, Marianecci C, Screpanti I, Checquolo S, Carafa M. Current trends in ATRA delivery for cancer therapy. Pharmaceutics, 2020;12(8).
Maeda Y, Yamaguchi T, Hijikata Y, Tanaka M, Hirase C, Takai S, Morita Y, Sano T, Miyatake J, Tatsumi Y, Kanamaru A. Clinical efficacy of all-trans retinoic acid for treating adult T cell leukemia. J Cancer Res Clin Oncol. 2008;134(6):673–7.
Nijhof IS, Groen RW, Lokhorst HM, van Kessel B, Bloem AC, van Velzen J, de Jong-Korlaar R, Yuan H, Noort WA, Klein SK, Martens AC, Doshi P, Sasser K, Mutis T, van de Donk NW. Upregulation of CD38 expression on multiple myeloma cells by all-trans retinoic acid improves the efficacy of daratumumab. Leukemia. 2015;29(10):2039–49.
Xia L, Li R, Wang Y, Lin Z, Zheng J, Li X, Lu Q, Zhang J, Jin H, Fu L, Zhang X, Liu Y, Yang S, Xiao F, Gao XH. Efficacy, safety, and cost-effectiveness of all-trans retinoic acid/clobetasol propionate compound ointment in the treatment of mild to moderate psoriasis vulgaris: a randomized, single-blind, multicenter clinical trial. Dermatol Ther. 2018;31(5):e12632.
Gregory EK, Webb A, Vercammen JM, Kelly ME, Akar B, van Lith R, Bahnson EM, Jiang W, Ameer GA, Kibbe MR. Inhibiting intimal hyperplasia in prosthetic vascular grafts via immobilized all-trans retinoic acid. J Control Release. 2018;274:69–80.
Gregory EK, Webb AR, Vercammen JM, Flynn ME, Ameer GA, Kibbe MR. Periadventitial atRA citrate-based polyester membranes reduce neointimal hyperplasia and restenosis after carotid injury in rats. Am J Physiol Heart Circ Physiol. 2014;307(10):H1419–29.
Jones T, Zhang B, Major S, Webb A. All-trans retinoic acid eluting poly(diol citrate) wafers for treatment of glioblastoma. J Biomed Mater Res B Appl Biomater. 2020;108(3):619–28.
Foley JH, Conway EM. Cross talk pathways between coagulation and inflammation. Circ Res. 2016;118(9):1392–408.
Grunkemeier JM, Tsai WB, Horbett TA. Hemocompatibility of treated polystyrene substrates: contact activation, platelet adhesion, and procoagulant activity of adherent platelets. J Biomed Mater Res. 1998;41(4):657–70.
Motlagh D, Yang J, Lui KY, Webb AR, Ameer GA. Hemocompatibility evaluation of poly(glycerol-sebacate) in vitro for vascular tissue engineering. Biomaterials. 2006;27(24):4315–24.
Axel DI, Kunert W, Göggelmann C, Oberhoff M, Herdeg C, Küttner A, Wild DH, Brehm BR, Riessen R, Köveker G, Karsch KR. Paclitaxel inhibits arterial smooth muscle cell proliferation and migration in vitro and in vivo using local drug delivery. Circulation. 1997;96(2):636–45.
Wakino S, Kintscher U, Kim S, Jackson S, Yin F, Nagpal S, Chandraratna RA, Hsueh WA, Law RE. Retinoids inhibit proliferation of human coronary smooth muscle cells by modulating cell cycle regulators. Arterioscler Thromb Vasc Biol. 2001;21(5):746–51.
Wijeyeratne YD, Heptinstall S. Anti-platelet therapy: ADP receptor antagonists. Br J Clin Pharmacol. 2011;72(4):647–57.
Sondeen JL, de Guzman R, Amy Polykratis I, Dale Prince M, Hernandez O, Cap AP, Dubick MA. Comparison between human and porcine thromboelastograph parameters in response to ex-vivo changes to platelets, plasma, and red blood cells. Blood Coagul Fibrinolysis. 2013;24(8):818–29.
Vollmar B, Slotta JE, Nickels RM, Wenzel E, Menger MD. Comparative analysis of platelet isolation techniques for the in vivo study of the microcirculation. Microcirculation. 2003;10(2):143–52.
von Brühl M-L, Stark K, Steinhart A, Chandraratne S, Konrad I, Lorenz M, Khandoga A, Tirniceriu A, Coletti R, Köllnberger M, Byrne RA, Laitinen I, Walch A, Brill A, Pfeiler S, Manukyan D, Braun S, Lange P, Riegger J, Ware J, Eckart A, Haidari S, Rudelius M, Schulz C, Echtler K, Brinkmann V, Schwaiger M, Preissner KT, Wagner DD, Mackman N, Engelmann B, Massberg S. Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo. J Exp Med. 2012;209(4):819–35.
Swystun LL, Liaw PC. The role of leukocytes in thrombosis. Blood. 2016;128(6):753–62.
Busnelli M, Froio A, Bacci ML, Giunti M, Cerrito MG, Giovannoni R, Forni M, Gentilini F, Scagliarini A, Deleo G, Benatti C, Leone BE, Biasi GM, Lavitrano M. Pathogenetic role of hypercholesterolemia in a novel preclinical model of vascular injury in pigs. Atherosclerosis. 2009;207(2):384–90.
Farb A, Weber DK, Kolodgie FD, Burke AP, Virmani R. Morphological predictors of restenosis after coronary stenting in humans. Circulation. 2002;105(25):2974–80.
Eppihimer MJ, Sushkova N, Grimsby JL, Efimova N, Kai W, Larson S, Forsyth B, Huibregtse BA, Dawkins KD, Wilson GJ, Granada JF. Impact of stent surface on thrombogenicity and vascular healing. Circ Cardiovasc Interv. 2013;6(4):370–7.
Pesarini G, Amoruso A, Ferrero V, Bardelli C, Fresu LG, Perobelli L, Scappini P, De Luca G, Brunelleschi S, Vassanelli C, Ribichini F. Cytokines release inhibition from activated monocytes, and reduction of in-stent neointimal growth in humans. Atherosclerosis. 2010;211(1):242–8.
Inoue T, Croce K, Morooka T, Sakuma M, Node K, Simon DI. Vascular inflammation and repair: implications for re-endothelialization, restenosis, and stent thrombosis. JACC Cardiovasc Interv. 2011;4(10):1057–66.
Shimaya Y, Shimada M, Shutto Y, Fujita T, Murakami R, Nakamura N, Yamabe H, Okumura K. Thrombin stimulates synthesis of macrophage colony-stimulating factor, granulocyte-macrophage colony-stimulating factor and granulocyte colony-stimulating factor by human proximal tubular epithelial cells in culture. Nephron extra. 2012;2(1):1–8.
Chanput W, Mes JJ, Wichers HJ. THP-1 cell line: an in vitro cell model for immune modulation approach. Int Immunopharmacol. 2014;23(1):37–45.
Schutte RJ, Parisi-Amon A, Reichert WM. Cytokine profiling using monocytes/macrophages cultured on common biomaterials with a range of surface chemistries. J Biomed Mater Res, Part A. 2009;88(1):128–39.
Cornelissen A, Vogt FJ. The effects of stenting on coronary endothelium from a molecular biological view: time for improvement? J Cell Mol Med. 2019;23(1):39–46.
Finn AV, Joner M, Nakazawa G, Kolodgie F, Newell J, John MC, Gold HK, Virmani R. Pathological correlates of late drug-eluting stent thrombosis. Circulation. 2007;115(18):2435–41.
Evans CE, Iruela-Arispe ML, Zhao Y-Y. Mechanisms of endothelial regeneration and vascular repair and their application to regenerative medicine. Am J Pathol. 2021;191(1):52–65.
Wang X, Fang F, Ni Y, Yu H, Ma J, Deng L, Li C, Shen Y, Liu X. The combined contribution of vascular endothelial cell migration and adhesion to stent re-endothelialization. Front Cell Dev Biol. 2021;9:641382–641382.
Zhang M, Malik AB, Rehman J. Endothelial progenitor cells and vascular repair. Curr Opin Hematol. 2014;21(3):224–8.
Hayashi S-I, Yamamoto A, You F, Yamashita K, Ikegame Y, Tawada M, Yoshimori T, Shimizu S, Nakashima S. The stent-eluting drugs sirolimus and paclitaxel suppress healing of the endothelium by induction of autophagy. Am J Pathol. 2009;175(5):2226–34.
Ammann KR, DeCook KJ, Li M, Slepian MJ. Migration versus proliferation as contributor to in vitro wound healing of vascular endothelial and smooth muscle cells. Exp Cell Res. 2019;376(1):58–66.
Rodriguez-Garcia B, Bureau C, Barakat AI. eG coated stents exhibit enhanced endothelial wound healing characteristics. Cardiovasc Eng Technol. 2021.
Saito A, Sugawara A, Uruno A, Kudo M, Kagechika H, Sato Y, Owada Y, Kondo H, Sato M, Kurabayashi M, Imaizumi M, Tsuchiya S, Ito S. All-trans retinoic acid induces in vitro angiogenesis via retinoic acid receptor: possible involvement of paracrine effects of endogenous vascular endothelial growth factor signaling. Endocrinology. 2007;148(3):1412–23.
Li H, Zhang LJ, Chen BH, Zhou X, Su K, Shi WT, Wu JZ, Yu H, Wei L. Inhibitory effect of paclitaxel on endothelial cell adhesion and migration. Pharmacology. 2010;85(3):136–45.
Funding
This work was funded by the National Institutes of Health R01, grant number R01HL130493.
Author information
Authors and Affiliations
Contributions
Project conceptualization: Antonio Webb and Josephine Allen; formal analysis and investigation: Heather Ursino, Bisheng Zhang, and Christopher Ludtka; writing—original draft preparation: Heather Ursino and Josephine Allen; writing—review and editing: all authors; funding acquisitions: Antonio Webb and Josephine Allen; supervision: Antonio Webb and Josephine Allen.
Corresponding author
Ethics declarations
Ethics Approval
The study includes experimentation with porcine whole-blood components. All animal procedures to collect whole blood were performed in accordance with the Institutional Animal Care and Use Committee (IACUC) and the University of Florida’s Animal Care Services (ACS) and policies.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
Author Josephine Allen holds a position on the editorial board of the Regenerative Engineering and Translational Medicine journal. The other authors have no relevant financial or nonfinancial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Future Works
Future studies may incorporate flow parameters and signals of relevant surrounding cell types to better replicate in situ conditions for improved translatability to clinical applications. Other variables like injury severity, drug dosage, and further stent surface characterization may also be explored due to known complexities involving these parameters.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ursino, H., Zhang, B., Ludtka, C. et al. Hemocompatibility of All-trans Retinoic Acid–Loaded Citrate Polymer Coatings for Vascular Stents. Regen. Eng. Transl. Med. 8, 579–592 (2022). https://doi.org/10.1007/s40883-022-00257-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40883-022-00257-y