Abstract
Purpose
Identifying the effective treatments for diseases has been a critical issue in daily clinical practice, especially for Alzheimer’s dementia (AD). Abundant evidence showed that non-invasive brain stimulation (NIBS) has the potential to slow or reverse cognitive function decline. Among them, the transcranial Direct Current Stimulation (tDCS) would be relatively safe for patients with AD. The purpose of this study was to review the relevant articles to explore the mechanism and effect of tDCS and other NIBS in AD treatment.
Methods
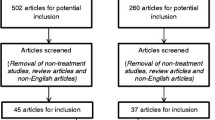
All the reported works were retrieved from two databases (i.e., PubMed and Google Scholar) by using the keywords “NIBS” and “AD”. The mechanisms and effects of different NIBS applied in AD, including transcranial ultrasound stimulation (TUS), transcranial near-infrared (tNIR) light therapy, transcranial magnetic stimulation (TMS), and transcranial electric stimulation (TES) were reviewed.
Results
The positive effects of TUS and tNIR on AD were supported by a few small samples and uncontrolled pilot studies. tDCS and repetitive TMS have been often used in an attempt to improve the cognition in people with brain disorders. Both the tDCS and TMS have benefits in AD by introducing long-term potentiation like change in synaptic strength. The reports showed that tDCS could be more safe, convenient, affordable, and well-tolerated method among all applications for AD treatment.
Conclusion
In this review, it was shown that all the NIBS have positive effects on AD treatment. But, however, tDCS showed the great potential in improving the cognition of AD.
Similar content being viewed by others
1 Introduction
1.1 Needs for the Therapeutic Strategies of AD
Alzheimer’s disease (AD) is the most common type of dementia including 60%–80% of all dementia cases [1]. However, the current medications for AD are either limited to efficacies in the progression of AD or complicated with serious side effects [2,3,4,5]. AD is generally considered to be associated with the amyloid cascade hypothesis which can initiate the downstream brain atrophy and cognitive decline [6,7,8]. Recently the US Food and Drug Administration (FDA) approved the uses of both Aducanumab and Lecanemab, were monoclonal IgG1 antibodies targeting the aggregated forms of amyloid β (Aβ) [9]. However, there is no persuasive evidence to support the approval of aducanumab as the validity from the studies is uncertain [10, 11]. It was studied that these two drugs could lower the brain Aβ burden but could cause the most common side effect, amyloid-related imaging abnormality (ARIA), which includes brain edema and hemorrhage. [12]. The ARIA might also lead to new signs and symptoms including headache, worsening confusion, dizziness, visual disturbances, nausea, and seizures [12]. However, it requires to find the alternative or complementary therapeutic strategies for AD due the controversies of drug therapy for AD.
1.2 Transcranial Direct Current Stimulation (tDCS) and Other Non-invasive Brain Stimulation (NIBS) in AD
The hypothesis of pathogenesis of AD is that the abnormal Aβ plaque deposition and hyperphosphorylation of intra-neuronal tau protein lead to mitochondrial dysfunction, inflammatory damage, synaptic failure, depletion of neurotrophin, deficit of neurotransmitters, vascular injury, and neuronal loss [6,7,8]. The synaptic dysfunction of AD contributed by the Aβ oligomers would induce excess calcium entry into the neurons via N-methyl-D-aspartate receptors (NMDARs) [13]. Consequently, the synaptic plasticity regulation mechanisms such as metaplasticity are altered before the loss of synapse. Long-term potentiation (LTP) and Long-term potentiation (LTD) are two main forms of synaptic plasticity which are involved in learning and memory [14]. The soluble oligomers of Aβ would induce a significant reduction of LTP by facilitating LTD induction [15]. Thus, the conditions that promote LTD, i.e., following excessive Aβ load in the early-onset forms of the disease, can lead to loss of synapses. Additionally,, the promoting LTP can represent a protective mechanism in order to preserve the synaptic plasticity and brain connectivity [16].
NIBS refers to those techniques that act on brain physiology without the need for surgical procedures involving the electrode implantation, such as deep brain stimulation, direct cortical stimulation, or epidural stimulation techniques [17]. It can be used to decrease the inflammation, increase the cerebral blood flow, modulate the activity of neurotrophic factors or neural excitability, and enhance the cortical function by facilitating LTP or reducing LTD, and thus would offer a potential means to slow or reverse the cognitive decline [18,19,20,21,22]. Numerous evidences support the use of NIBS techniques as tools for enhancing the cognitive function in healthy subjects and as therapeutic agents for patients with neurocognitive disorder [23,24,25].
According to the power sources, the techniques of NIBS include transcranial ultrasound stimulation (TUS), transcranial near-infrared (tNIR) light therapy, transcranial magnetic stimulation (TMS), and transcranial electric stimulation (TES) (Fig. 1). tDCS is a common type of TES. It is a simple, safe, convenient, affordable, and well-tolerated method that has been tested to modify the cognition of healthy participants and mitigate the cognitive symptoms in AD for two decades. [21, 26,27,28]. The tDCS and repetitive TMS (rTMS)-induced cognitive enhancement have been studied much more than the same effects produced by TUS and tNIR. [17].
The aim of this study was to systematically review the related articles to explore the effect of tDCS and other non-invasive brain stimulation (NIBS) in AD. The characteristics and mechanisms of each NIBS device applied to AD were discussed.
2 NIBS Techniques in AD
2.1 Transcranial Ultrasound Stimulation (TUS) in AD
Ultrasound is a mechanical wave with a frequency above the human hearing range, from 20 kHz to 1 GHz. It travels with alternating compression and rarefaction, by transmitting energy through molecular movements. The high-intensity ultrasounds use ultrasound intensities > 3W/cm2 and low-intensity ultrasounds (LIU) with < 3W/cm2 [29]. High-intensity focused ultrasound is used to cause the significant tissue heating for therapeutic ablations, whereas LIU produces mechanical effects on tissues that do not cause the heating or damage. Beyond direct effects on electrical activity, LIU has been shown to modulate the activity of neurotrophic factors that could produce the secondary effects on neural activity and plasticity [18]. In TUS stimulation, the transcranial focused ultrasound (tFUS) transmits LIU into the brain non-invasively and focuses on deep brain regions [30].
TUS stimulation treatment of various durations was associated with different beneficial effects against Aβ and tau-induced toxicity and structural damage in the brains of AD transgenic mouse models [31,32,33]. TUS has provided some solid evidence for its beneficial effects on brain plasticity and function as well as neuronal circuit integrity in experimental animal studies [31]. However, no clinical evidence has been provided on the mitigation of neurotoxicity after ultrasound treatment in humans [31]. At the clinical level, three studies have reported the alterations in brain networks after ultrasound therapy in AD patients [34,35,36]. These three pilot studies were performed with quite small patients and in an uncontrolled design.
2.2 Transcranial Near-Infrared (tNIR) Light Therapy in AD
Low-power tNIR light-emitting diodes illuminate the light that is outside of the visible spectrum of human eyes but can efficiently penetrate the scalp, skull, and meninges to reach the brain parenchyma [37, 38]. It was proposed that mitochondrial dysfunction, inadequate supplies of adenosine triphosphate (ATP), and oxidative stress were contributory factors in AD [39]. This near-infrared photon absorption by cytochrome C oxidase might dissociate the inhibitory nitric oxide, unit IV of the mitochondrial respiratory chain, and thereby allowing the respiration to resume to be unhindered and to increase the ATP synthesis. The tNIR light could prove valuable for AD therapeutics by targeting the mitochondria, increasing ATP in proteasomes for ubiquitination of misfolded proteins, decreasing inflammation and even antibacterial and anti-viral effects [40,41,42,43].
So far, there has been a limited number of clinical trials that have used tNIR to treat the patients with AD. Two pilot studies demonstrated the safety and positive cognitive improvements in small sample size of patients with dementia [44, 45]. Very small sample or fuzzy number of AD in these two studies made no clear evidence of efficacy in cognition of AD.
2.3 Transcranial Magnetic Stimulation (TMS) in AD
TMS is a stimulation method in which a changing magnetic field is used to cause the electric current that can modulate the neuronal activity in an area of interest in the brain, with a powerful, rapidly fluctuating, handheld electromagnet [46]. These currents cause direct axonal excitation or trans-synaptic activation of neurons, depending on the excitability properties of the neural structure and their orientation in the magnetic field-induced electric field. It pulses at a specified frequency and intensity, and the repetitive TMS (rTMS), can induce changes in brain excitability that can persist for some time after the period of stimulation [47].
Both high- and low-frequency rTMS significantly modulated the widespread brain activity [48]. The LTP induced by high-frequency magnetic stimulation (100 Hz), and related synaptic enhancement have been reported in animal studies following 10 and 20 Hz magnetic stimulation [22, 49, 50]. This, strongly support the potential mechanisms of rTMS benefits in AD by LTP -like changes in synaptic strength. After low-frequency magnetic stimulation, the GABAergic synthesizing enzymes and transporters increase, as well, after high-frequency stimulation, the number of immunocytochemically identified inhibitory cells decreases [51,52,53]. With respect to the clinical effects of stimulation, low-frequency rTMS protocols were known to result into the cortical suppression and inhibition, whereas the high-frequency stimulation would increase the cortical facilitation and excitability [51,52,53,54].
In AD, several small pilot studies have shown promising results by using rTMS protocols to improve the global cognition or language function [55,56,57]. A recent meta-analysis supported the beneficial effect of rTMS on cognitive functions in patients with AD [58]. A similar result was reported by a study with eight articles focusing on rTMS treatment of AD and suggested the potentiality for the improvement in cognitive measures after rTMS treatments. But, the results did not clearly show whether rTMS was significantly more effective than sham [59].
2.4 Transcranial Electric Stimulation (TES) in AD
TES is the way that two or more electrodes are applied to a person's scalp, by using electrical currents to penetrate the scalp and pass through the brain cortex to alter the brain function [60]. The Polarizing effects evoked by the electric fields (EFs) can be categorized as (1) “suprathreshold” stimulation—directly triggering the neuronal action potentials; (2) “subthreshold” stimulation—primarily exert modulatory effects on ongoing neuronal activity and excitability [17, 61]. In the electrical NIBS techniques, the group of suprathreshold stimulation (that primarily induce the activity of neurons) includes high-intensity short-pulse TES, electroconvulsive therapy (ECT), and electro-anesthesia. The group of subthreshold stimulation includes the forms of low-intensity (e.g., few mA) and sustained (e.g., minutes) TES, such as transcranial alternating current stimulation (tACS), and transcranial random noise stimulation (tRNS), and tDCS [17, 62]. The suprathreshold techniques ultimately affect the behavior by modulation of endogenous networks, whereas the subthreshold techniques can influence the firing in the active system [63, 64]. The electric field intensities produced in the brain by suprathreshold techniques are often two orders of magnitude above the subthreshold, allowing for the triggering of action potentials [17]. It is a reasonable inference that adverse effects are less in subthreshold than that of in suprathreshold electrical stimulation.
In the suprathreshold technique, high-intensity short-pulse TES, electro-anesthesia, and ECT were not investigated for the therapeutic application of AD because of side effects, such as seizure, cardiac arrhythmia, hemodynamic changes, or impaired cognitive function [65,66,67,68,69].
In the subthreshold electrical technique, three different waveforms of the currents are applied to induce the EF: (1) tDCS: the applied current is constant over time; (2) tACS: the current is rapidly alternated at a specific frequency (1–45 Hz), in a sinusoidal wave, to entrain cortical oscillations; and (3) tRNS: a whit-noise band-limited waveform (frequent spectrum 0.6–640 Hz) with full-band current spectrum is applied to boost the endogenous rhythms by means of stochastic resonance. [70, 71] (Fig. 2). The depolarization or hyperpolarization is below the spike threshold. They do not induce the massive synchronized discharge of action potentials as TMS do. They all share the same approach with respect to the electrode montage and in all cases, the duration of stimulation is typically 10–30 min with a peak current of 1–2 mA [72].
This schematic diagram illustrates different subthreshold TES waveforms. Left: The tDCS waveform displays both the anodal (green) and cathodal (dash green) electrodes, which must remain active simultaneously throughout the stimulation process. The current is ramped up (10 s) to the desired current intensity and when said intensity is reached the current intensity is held at that level for the duration of stimulation. The ramped off is also 10 s usually. Middle: The tACS waveform illustrates the characteristic pattern of oscillatory current delivery between the electrodes. Right: tRNS is similar to tACS in using alternating current. The tRNS waveform demonstrates the application of generalized random noise current intensity during the stimulation process
The applied tACS current altering the transmembrane potential of neurons entrains the neuronal firing from a large number of underlying neurons to the exogenous frequency but did not alter the neuronal excitability [73]. In general, the synchronous oscillations of high frequency, such as the gamma band of electroencephalography, represent a highly organized form of brain activity. tACS is an appealing approach with the evidence of abnormal brain oscillations in AD [74]. Alteration in spontaneous oscillatory activity can be accomplished with tACS, which in the main frequency bands of physiological brain activity does not induce the plasticity [75].
The tRNS is a subtype of tACS that involves the application of random noise oscillations above selected brain regions to modulate the cortical plasticity. It can induce the mechanisms of temporal summation of neural activity due to the reason that the time constant of a neuron is long enough to allow the sum of two or more stimuli in a close temporal sequence [76]. The effects of tRNS were also explained by the increase of neuronal excitability via stochastic resonance. Whereas the weak neural signal detection in the central nervous system was enhanced when noise was added [77]. Although there have not been any published reports investigating the potential therapeutic benefit of tRNS in AD, it has been shown to improve the fluid intelligence in healthy adults when paired with adaptive cognitive training [78]. A study proposed that the usage of tACS allowed modulating the brain oscillations and in turn influences the cognitive processes, by demonstrating the causal link between the two [79]. However, there has little evidence been collected with respect to tACS in addressing the gamma oscillatory activity in AD based on evidence from animal models, whereas no study has so far employed tRNS in AD [80, 81].
2.5 tDCS in AD
2.5.1 Neurophysiological Mechanism of tDCS
To date, the majority of studies on subthreshold electrical techniques in AD have been conducted by using tDCS. At the neuronal level, the primary neurophysiological mechanism of tDCS action of the cerebral cortex is assumed based on modulating spontaneous neuronal network activity through polarization of the resting membrane potential [27, 82, 83]. As the weak current of tDCS flows inward the brain, it depolarizes the soma, or cell body of neurons near the anodal electrode by bringing them closer to their thresholds for firing an action potential, whereas the ionic gradients near the cathode have the opposite effect [84,85,86]. The induced extracellular voltages are not uniform across the neurons but changed depending on the cellular compartment [87, 88]. The weak EFs perpendicular to the main orientation of neurons do not polarize the somatic membrane significantly but may still influence the functions [89]. Membrane potential at the soma is linear with EF intensity along the primary neural axis for weak, subthreshold EFs [88]. The effect on membrane polarization affects potentially every aspect of neuronal, electrical, and synaptic activity. The changes in neuronal excitability are reflected in both spontaneous firing rates and responsiveness to afferent synaptic inputs [89,90,91]. Furthermore, the increased excitability of local neurons by anodal stimulation is assumed to increase the blood flow around the stimulation site, and induce subsequent metabolic changes among neurons [92].
The other physiological mechanism of tDCS in the changes of the low-frequency long-range network connectivity patterns observed as resting state networks are reflected in modulation of local, higher-frequency activity, particularly in the gamma frequency band [93]. The decrease in local GABA by tDCS and increase in firing rates lead to an increase in local gamma-band oscillatory activity, which will lead to an increase in functional connectivity in highly connected regions [94]. tDCS leads to an increase in gamma activity has been supported by the study of magnetoencephalography [95].
2.5.2 Biochemical Mechanism of tDCS
In biochemical mechanism of tDCS on neural circuits, EF of tDCS modifies the variety of neurotransmitter systems in synaptic microenvironment. The anodal tDCS may enhance the excitatory synaptic transmissions by changing the balance between glutamate and GABA activities, with enhancing the effect on glutamatergic neurons by reducing GABA activity [94, 96,97,98,99,100,101,102]. In the tDCS induced membrane depolarizing or hyperpolarizing effects on glutamatergic synapses, tDCS enhances or reduces calcium influx via NMDARs and voltage-gated calcium channels. The enzyme cascades are active as the alteration of intra-neuronal calcium. These insert glutamatergic α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPA receptor) into or remove them from the subsynaptic membrane, by strengthening or weakening the synaptic connections [94]. The amount of intracellular calcium controls the induction of both LTP and LTD, if excitability-enhancing LTP or excitability-diminishing LTD takes place. Anodal tDCS presumably induces high calcium concentration which will result into LTP, whereas cathodal tDCS induces low calcium concentration, which will result into LTD. tDCS induces long-term neuromodulation.
The other contributing factors to the neuromodulatory action include changes in brain-derived neurotrophic factor (BDNF) expression. The tropomyosin-receptor kinase (Trk) receptors, a family of growth factor receptors, may also be attracted to the synapse in anodal tDCS [103]. The presence of calcium ion influx increases the release of BDNF into the synaptic cleft [104]. Postsynaptic Trk receptor induces later phase LTP and favors the opening of NMDA receptors, which also promotes later phase LTP, whereas the opposite is involved in cathodal tDCS, promoting the later phase LTD [105, 106].
The effects of tDCS may also involve other factors and the regulation of various neurotransmitters, such as GABA, dopamine, acetylcholine, serotonin, adrenaline and noradrenaline [96, 99, 107,108,109,110]. These neural events are considered to improve the psychiatric symptoms and the cognitive function [83, 111].
Human studies proved the benefit of tDCS on cognitive function in AD [28, 112, 113]. However, there were inconsistent results suggesting that the tDCS showed no significant effect on the performance of the face-name association task or verbal memory function [114, 115]. Nevertheless, the review of the past 18 research reports and the meta-analysis results of tDCS on AD cognitive function still hold the conclusion that tDCS has a positive effect [113, 116].
In summary, the mechanism and benefits of all current studies on AD with various NIBS are shown in Table 1.
3 Discussion
3.1 Benefits and Limitations of TUS, tNIR, and tACS
Although the predominance of small, heterogeneous, proof-of-principle studies precludes definitive conclusions from past studies, NIBS remains an active area of investigation for the treatment of AD and may play a useful role in future multimodality treatment approaches that are likely to be required in AD [59]. tFUS applies acoustic energy to highly specific intracranial areas, including both cortical and deep brain regions, with good spatial specificity and significant depth penetration [36]. It may have the potential to serve as a novel NIBS tool for the treatment of AD. It can be suggested that for clinical TUS brain stimulation, the current techniques and certified systems (such as the pulse frequency, the delivery mode, and the ultrasonic energy) have to be developed and further studies are required to understand its therapeutic mechanism, safety, and efficacy [36].
tNIR light therapy is a relatively new approach to photo-biomodulation for treating brain disorders and possibly for enhancing the cognitive function in dementia [117]. There are only few evidences to date for the tNIR producing the direct neural activity and there have not been any studies that have shown that tNIR induces LTP or LTD in ex vivo brain slices [17].
A recent FDA review for approval of a commercial TMS system for the treatment of AD suggested that current evidence fails to demonstrate a clinically meaningful TMS benefit in AD [51]. One of the limitations of TMS for AD treatment is that the insufficient number of patients are included in those studies. The other is that most of these studies have stimulated the brain regions on the DLPFC, and therefore, the non-significant rTMS effects of other brain regions should be interpreted with caution. Also, the effective treatment of rTMS for AD still needs to be developed.
There are two issues that have questioned the effect of tACS on cognition. First is whether the brain oscillations reflect a fundamental mechanism in cortical information processing or just an epiphenomenon is still unresolved [79]. The second is the simultaneous measurement of EEG, magnetic (magnetoencephalographic), or imaging (blood-oxygen-level dependent) signals during tACS was not feasible due to strong artifacts [118]. The retinal phosphene perception during tACS in a wide frequency range (6–70 Hz) is a side effect of specifically tACS [119].
3.2 Comparison of TMS and tDCS
TMS and tDCS have been often used in an attempt to improve the cognition in people with brain disorders. However, a major limitation across TMS and tDCS studies lies in the difficulty of comparing their efficacy due to the high variability observed across the study protocols [59, 120]. On the study protocol, tDCS has the advantage of being easier to use in double-blind or sham-controlled studies and easier to apply concurrently with behavioral tasks. In comparison with rTMS, tDCS is a low-cost technique, with portability and potential for home application, easy application, and practically fewer adverse effect. The human trials showed that the use of conventional tDCS protocols in human trials (≤ 40 min, ≤ 4 mA, ≤ 7.2 Coulombs) has not produced any reports of a serious adverse effect or irreversible injury [121]. However, current rTMS are not designed for at-home use. The TMS devices are always large, heavy and usually set up on a cart. Their size can be as a large microwave or mini fridge. Unlike tDCS, the head position needs to be fixed as rTMS is ongoing. This is hard for those with dementia with BPSD. In general, low-intensity electrical stimulation such as tDCS, is to induce non-painful (pre-pain) sensations. In contrast, rTMS may produce twitching in the scalp, temporary tinnitus, dizziness, or scalp pain. These may subside almost immediately after a session has been completed. The most serious side effect of rTMS is the potential for seizures, though the risk of TMS-related seizures is < 1% overall [122]. The comparisons of tDCS and rTMS are listed in Table 2.
3.3 tDCS- An Affordable Intervention Tool for AD
The positive or negative efficacy of tDCS on AD is under debate from the past studies, review, and meta-analysis research, respectively [23, 28, 112, 114, 115, 123,124,125,126,127]. The conflict results may be due to the reason that these studies reporting the data from case studies or small samples and there is a very different evaluation criteria, number and length of stimulation sessions, intensity and type of stimulation, target area, and type of sham stimulation between various studies. The results of tDCS in AD to date should be considered preliminary and further investigations are still required for detailed analysis. Also, further research is needed to explore under what circumstances the tDCS may be beneficial in AD [23].
Animal studies showed that the tDCS effectively improved the cognition, spatial learning and memory performance, alleviated Aβ burden and had a protective effect on neurons [128, 129]. The direct current stimulation in animal studies revealed that the long-lasting effects are protein synthesis-dependent and accompanied by modifications of intracellular cAMP [27]. It can modulate the cortical function by inducing the long-term after-effects on cortical excitability and neuronal plasticity [27, 130]. This brings about facilitatory or inhibitory effects, by broadly mirroring the workings of LTP and LTD [20, 21]. Studies showed that tDCS can modulate focally the rCBF and can be used to increase the oxygen availability or to facilitate the elimination of “neurotoxic” substances in degenerative disorders [92]. tDCS is assumed to be the reasonable therapeutic instruments since it alters (i) neuronal activity and (ii) human CBF, (iii) it has synaptic and non-synaptic after-effects (iv), it can modify neurotransmitters polarity-dependently, (v) it can alter oscillatory brain activity and the functional connectivity patterns in the brain [131]. In overall the possible mechanism of tDCS effect on AD is as shown in Fig. 3. tDCS modulates the synaptic environment and calcium reflux, influences the protein synthesis and BDNF release, modulates the LTP and LTD, and subsequently influences the regional cerebral blood flow and functional connectivity. These may play a major role for improving the declined cognition that induced by the misfolding and aggression of toxic Aβ. Thus, tDCS is a selectable tool for studying the effects of cognitive function in AD.
4 Conclusion
All the NIBS methods witnessed the potential to be applied in the treatment of AD. Then, it is suggested that the tDCS can be used as a therapeutic instrument in AD since it causes changes in neuronal activity, blood flow to the brain, osmotic brain activity, communicative patterns of the brain, synaptic and non-synaptic effects, and neural modulation in AD.
Data Availability
Not applicable.
References
DeTure, M. A., & Dickson, D. W. (2019). The neuropathological diagnosis of Alzheimer’s disease. Molecular Neurodegeneration, 14(1), 32. https://doi.org/10.1186/s13024-019-0333-5
Tan, C. C., Yu, J. T., Wang, H. F., Tan, M. S., Meng, X. F., Wang, C., Jiang, T., Zhu, X. C., & Tan, L. (2014). Efficacy and safety of donepezil, galantamine, rivastigmine, and memantine for the treatment of Alzheimer’s disease: a systematic review and meta-analysis. J Alzheimer’s Disease, 41(2), 615–631. https://doi.org/10.3233/JAD-132690
Zemek, F., Drtinova, L., Nepovimova, E., Sepsova, V., Korabecny, J., Klimes, J., & Kuca, K. (2014). Outcomes of Alzheimer’s disease therapy with acetylcholinesterase inhibitors and memantine. Expert Opinion on Drug Safety, 13(6), 759–774. https://doi.org/10.1517/14740338.2014.914168
Sharma, K. (2019). Cholinesterase inhibitors as Alzheimer’s therapeutics (Review). Molecular Medicine Reports, 20(2), 1479–1487. https://doi.org/10.3892/mmr.2019.10374
Avgerinos, K. I., Ferrucci, L., & Kapogiannis, D. (2021). Effects of monoclonal antibodies against amyloid-β on clinical and biomarker outcomes and adverse event risks: A systematic review and meta-analysis of phase III RCTs in Alzheimer’s disease. Ageing Research Reviews, 68, 101339.
Querfurth, H. W., & LaFerla, F. M. (2010). Alzheimer’s disease. New England Journal Medicine, 362(4), 329–344. https://doi.org/10.1056/NEJMra0909142
Lasagna-Reeves, C. A., Castillo-Carranza, D. L., Sengupta, U., Clos, A. L., Jackson, G. R., & Kayed, R. (2011). Tau oligomers impair memory and induce synaptic and mitochondrial dysfunction in wild-type mice. Molecular Neurodegeneration, 6, 39. https://doi.org/10.1186/1750-1326-6-39
Pooler, A. M., Polydoro, M., Wegmann, S., Nicholls, S. B., Spires-Jones, T. L., & Hyman, B. T. (2013). Propagation of tau pathology in Alzheimer’s disease: identification of novel therapeutic targets. Alzheimer’s Research & Therapy, 5(5), 49. https://doi.org/10.1186/alzrt214
Söderberg, L., Johannesson, M., Nygren, P., Laudon, H., Eriksson, F., Osswald, G., Möller, C., & Lannfelt, L. (2023). Lecanemab, aducanumab, and gantenerumab—binding profiles to different forms of amyloid-beta might explain efficacy and side effects in clinical trials for Alzheimer’s disease. Neurotherapeutics, 20(1), 195–206. https://doi.org/10.1007/s13311-022-01308-6
Schneider, L. (2020). A resurrection of aducanumab for Alzheimer’s disease. The Lancet Neurology, 19(2), 111–112. https://doi.org/10.1016/S1474-4422(19)30480-6
Alexander, G. C., Emerson, S., & Kesselheim, A. S. (2021). Evaluation of aducanumab for Alzheimer disease: Scientific evidence and regulatory review involving efficacy, safety, and futility. JAMA, 325(17), 1717–1718. https://doi.org/10.1001/jama.2021.3854
Withington, C. G., & Turner, R. S. (2022). Amyloid-related imaging abnormalities with anti-amyloid antibodies for the treatment of dementia due to Alzheimer’s disease. Front Neurology, 13, 862369. https://doi.org/10.3389/fneur.2022.862369.eCollection
Kodis, E. J., Choi, S., Swanson, E., Ferreira, G., & Bloom, G. S. (2018). N-methyl-D-aspartate receptor-mediated calcium influx connects amyloid-β oligomers to ectopic neuronal cell cycle reentry in Alzheimer’s disease. Alzheimer’s Dementia, 10, 1302–1312. https://doi.org/10.1016/j.jalz.2018.05.017
Malenka, R. C., & Bear, M. F. (2004). LTP and LTD. Neuron, 44(1), 5–21. https://doi.org/10.1016/j.neuron.2004.09.012
Peineau, S., Rabiant, K., Pierrefiche, O., & Potier, B. (2018). Synaptic plasticity moudation by circulating peptides and metaplasticity: Involvement in Alzheimer’s disease. Pharmacological Research, 30, 385–401. https://doi.org/10.1016/j.phrs.2018.01.018
Mango, D., Saidi, A., Cisale, G. Y., Feligioni, M., Corbo, M., & Nisticò, R. (2019). Targeting synaptic plasticity in experimental models of Alzheimer’s disease. Frontiers in Pharmacology, 10, 778. https://doi.org/10.3389/fphar.2019.00778
Giordano, J., Bikson, M., Kappenman, E. S., Clark, V. P., Coslett, H. B., Hamblin, M. R., Hamilton, R., Jankord, R., Kozumbo, W. J., McKinley, R. A., Nitsche, M. A., Reilly, J. P., Richardson, J., Wurzman, R., & Calabrese, E. (2017). Mechanisms and effects of transcranial direct current stimulation. Dose Response, 15(1), 1559325816685467. https://doi.org/10.1177/1559325816685467
Tufail, Y., Matyushov, A., Baldwin, N., Tauchmann, M. L., Georges, J., Yoshihiro, A., Tillery, S. I. H., & Tyler, W. J. (2010). Transcranial pulsed ultrasound stimulates intact brain circuits. Neuron, 66(5), 681–694. https://doi.org/10.1016/j.neuron.2010.05.008
Hamblin, M. R. (2019). Photobiomodulation for Alzheimer’s disease: Has the light dawned? Photonics, 6(3), 77. https://doi.org/10.3390/photonics6030077
Dayan, E., Censor, N., Buch, E. R., Sandrini, M., & Cohen, L. G. (2013). Noninvasive brain stimulation: from physiology to network dynamics and back. Nature Neuroscience, 16(7), 838–844. https://doi.org/10.1038/nn.3422
Birba, A., Ibáñez, A., Sedeño, L., Ferrari, J., García, A. M., & Zimerman, M. (2017). Non-invasive brain stimulation: A New strategy in mild cognitive impairment? Frontiers in Aging Neuroscience, 9, 16. https://doi.org/10.3389/fnagi.2017.00016
Vlachos, A., Müller-Dahlhaus, F., Rosskopp, J., Lenz, M., Ziemann, U., & Deller, T. (2012). Repetitive magnetic stimulation induces functional and structural plasticity of excitatory postsynapses in mouse organotypic hippocampal slice cultures. The Journal of Neuroscience, 32(48), 17514–17523. https://doi.org/10.1523/JNEUROSCI.0409-12.2012
Holczer, A., Németh, V. L., Vékony, T., Vécsei, L., Klivényi, P., & Must, A. (2020). Non-invasive brain stimulation in Alzheimer’s disease and mild cognitive impairment-a state-of-the-art review on methodological characteristics and stimulation parameters. Frontiers in Human Neuroscience, 14, 179. https://doi.org/10.3389/fnhum.2020.00179
Vacas, S. M., Stella, F., Loureiro, J. C., do Simões Couto, F., Oliveira-Maia, A. J., & Forlenza, O. V. (2019). Noninvasive brain stimulation for behavioural and psychological symptoms of dementia: A systematic review and meta-analysis. International Journal of Geriatric Psychiatry, 34(9), 1336–1345. https://doi.org/10.1002/gps.5003
Begemann, M. J., Brand, B. A., Ćurčić-Blake, B., Aleman, A., & Sommer, I. E. (2020). Efficacy of non-invasive brain stimulation on cognitive functioning in brain disorders: A meta-analysis. Psychological Medicine, 50(15), 2465–2486. https://doi.org/10.1017/S0033291720003670
Nitsche, M. A., Liebetanz, D., Lang, N., Antal, A., Tergau, F., & Paulus, W. (2003). Safety criteria for transcranial direct current stimulation (tDCS) in human. Clinical Neurophysiology, 114(11), 2220–2. https://doi.org/10.1016/s1388-2457(03)00235-9
Nitsche, M. A., Cohen, L. G., Wassermann, E. M., Priori, A., Lang, N., Antal, A., Paulus, W., Hummel, F., Boggio, P. S., Fregni, F., & Pascual-Leone, A. (2008). Transcranial direct current stimulation: State of the art 2008. Brain Stimulation, 1(3), 206–223. https://doi.org/10.1016/j.brs.2008.06.004
Khedr, E. M., Gamal, N. F., El-Fetoh, N. A., Khalifa, H., Ahmed, E. M., Ali, A. M., Noaman, M., El-Baki, A. A., & Karim, A. A. (2014). A double-blind randomized clinical trial on the efficacy of cortical direct current stimulation for the treatment of Alzheimer’s disease. Frontiers in Aging Neuroscience, 6, 275. https://doi.org/10.3389/fnagi.2014.00275
Chávez-Martínez, A., Reyes-Villagrana, R. A., Rentería-Monterrubio, A. L., Sánchez-Vega, R., Tirado-Gallegos, J. M., & Bolivar-Jacobo, N. A. (2020). Low and high-intensity ultrasound in dairy products: applications and effects on physicochemical and microbiological quality. Foods, 9(11), 1688. https://doi.org/10.3390/foods9111688
Meng, Y., Hynynen, K., & Lipsman, N. (2021). Applications of focused ultrasound in the brain: from thermoablation to drug delivery. Nature Reviews Neurology, 17(1), 7–22. https://doi.org/10.1038/s41582-020-00418-z
Monteiro, F., Sotiropoulos, I., Carvalho, Ó., Sousa, N., & Silva, F. S. (2021). Multi-mechanical waves against Alzheimer’s disease pathology: a systematic review. Translational Neurodegeneration, 10(1), 36. https://doi.org/10.1186/s40035-021-00256-z
Lee, Y., Choi, Y., Park, E. J., Kwon, S., Kim, H., Lee, J. Y., & Lee, D. S. (2020). Improvement of glymphatic–lymphatic drainage of beta—amyloid by focused ultrasound in Alzheimer ’ s disease model. Scientific Reports, 10(1), 16144. https://doi.org/10.1038/s41598-020-73151-8
Shen, Y., Hua, L., Yeh, C.-K.C., Shen, L., Ying, M., Zhang, Z., Liu, G., Li, S., Chen, S., Chen, X., & Yang, X. (2020). Ultrasound with microbubbles improves memory, ameliorates pathology and modulates hippocampal proteomic changes in a triple transgenic mouse model of alzheimer’s disease. Theranostics, 10(25), 11794–11819. https://doi.org/10.7150/thno.44152
Meng, Y., MacIntosh, B. J., Shirzadi, Z., Kiss, A., Bethune, A., Heyn, C., Mithani, K., Hamani, C., Black, S. E., Hynynen, K., & Lipsman, N. (2019). Resting state functional connectivity changes after MR-guided focused ultrasound mediated blood–brain barrier opening in patients with Alzheimer’s disease. Neuroimage, 200, 275–280. https://doi.org/10.1016/j.neuroimage.2019.06.060
Beisteiner, R., Matt, E., Fan, C., Baldysiak, H., Schönfeld, M., Philippi Novak, T., Amini, A., Aslan, T., Reinecke, R., Lehrner, J., Weber, A., Reime, U., Goldenstedt, C., Marlinghaus, E., Hallett, M., & Lohse-Busch, H. (2019). Transcranial pulse stimulation with ultrasound in Alzheimer’s disease—a new navigated focal brain therapy. Advanced Science, 7(3), 1902583. https://doi.org/10.1002/advs.201902583
Jeong, H., Im, J., Park, J., Na, S. H., Lee, W., Yoo, S. S., Song, I. U., & Chung, Y. A. (2021). A pilot clinical study of low-intensity transcranial focused ultrasound in Alzheimer’s disease. Ultrasonography, 40(4), 512–519. https://doi.org/10.14366/usg.20138
Tedford, C. E., DeLapp, S., Jacques, S., & Anders, J. (2015). Quantitative analysis of transcranial and intraparenchymal light penetration in human cadaver brain tissue. Lasers in Surgery and Medicine, 47(4), 312–322. https://doi.org/10.1002/lsm.22343
Pitzschke, A., Lovisa, B., Seydoux, O., Zellweger, M., Pfleiderer, M., Tardy, Y., & Wagnières, G. (2015). Red and NIR light dosimetry in the human deep brain. Physics in Medicine and Biology, 60(7), 2921–2937. https://doi.org/10.1088/0031-9155/60/7/2921
Swerdlow, R. H., Burns, J. M., & Khan, S. M. (2014). The Alzheimer’s disease mitochondrial cascade hypothesis: Progress and perspectives. Biochimica et Biophysica Acta (BBA)—Molecular Basis of Disease, 1842(8), 1219–1231. https://doi.org/10.1016/j.bbadis.2013.09.010
Hamblin, M. R., & Demidova, T. N. (2006). Mechanisms of Low Level Light Therapy. Proceedings of SPIE—The International Society for Optical Engineering, 6140, 614001–12. https://doi.org/10.1117/12.646294
Passarella, S., & Karu, T. (2014). Absorption of monochromatic and narrow band radiation in the visible and near IR by both mitochondrial and non-mitochondrial photoacceptors results in photobiomodulation. Journal of Photochemistry and Photobiology B: Biology, 140, 344–358. https://doi.org/10.1016/j.jphotobiol.2014.07.021
Lane, N. (2006). Cell biology: Power games. Nature, 443(7114), 901–3. https://doi.org/10.1038/443901a
Poyton, R. O., & Ball, K. A. (2011). Therapeutic photobiomodulation: Nitric oxide and a novel function of mitochondrial cytochrome c oxidase. Discovery Medicine, 11(57), 154–159.
Nizamutdinov, D., Qi, X., Berman, M. H., Dougal, G., Dayawansa, S., Wu, E., Yi, S. S., Stevens, A. B., & Huang, J. H. (2021). Transcranial near infrared light stimulations improve cognition in patients with dementia. Aging and disease, 12(4), 954–963. https://doi.org/10.14336/AD.2021.0229
Berman, M. H., Halper, J. P., Nichols, T. W., Jarrett, H., Lundy, A., & Huang, J. H. (2017). Photobiomodulation with near infrared light helmet in a pilot, placebo controlled clinical trial in dementia patients testing memory and cognition. Journal of Neurology and Neuroscience, 8(1), 176. https://doi.org/10.21767/2171-6625.1000176
Kobayashi, M., & Pascual-Leone, A. (2003). Transcranial magnetic stimulation in neurology. The Lancet Neurology, 2(3), 145–156. https://doi.org/10.1016/s1474-4422(03)00321-1
Klomjai, W., Katz, R., & Lackmy-Vallée, A. (2015). Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS). Annals of Physical and Rehabilitation Medicine, 58(4), 208–213. https://doi.org/10.1016/j.rehab.2015.05.005
Wang, J., Deng, X. P., Wu, Y. Y., Li, X. L., Feng, Z. J., Wang, H. X., Jing, Y., Zhao, N., Zang, Y. F., & Zhang, J. (2020). High-frequency rTMS of the Motor cortex modulates cerebellar and widespread activity as revealed by SVM. Frontiers in Neuroscience, 19(14), 186. https://doi.org/10.3389/fnins.2020.00186
Tokay, T., Holl, N., Kirschstein, T., Zschorlich, V., & Köhling, R. (2009). Highfrequency magnetic stimulation induces long-term potentiation in rat hippocampal slices. Neuroscience Letters, 461, 150–154. https://doi.org/10.1016/j.neulet.2009.06.032
Banerjee, J., Sorrell, M. E., Celnik, P. A., & Pelled, G. (2017). Immediate effects of repetitive magnetic stimulation on single cortical pyramidal neurons. PloS one, 12(1), e0170528. https://doi.org/10.1371/journal.pone.0170528
Weiler, M., Stieger, K. C., Long, J. M., & Rapp, P. R. (2020). Transcranial magnetic stimulation in Alzheimer’s disease: Are we ready? eNeuro, 7(1), ENEURO.0235-192019. https://doi.org/10.1523/ENEURO.0235-19.2019
Lenz, M., Galanis, C., Müller-Dahlhaus, F., Opitz, A., Wierenga, C. J., Szabó, G., Ziemann, U., Deller, T., Funke, K., & Vlachos, A. (2016). Repetitive magnetic stimulation induces plasticity of inhibitory synapses. Nature Communications, 7, 10020. https://doi.org/10.1038/ncomms10020
Jazmati, D., Neubacher, U., & Funke, K. (2018). Neuropeptide Y as a possible homeostatic element for changes in cortical excitability induced by repetitive transcranial magnetic stimulation. Brain Stimulation, 11(4), 797–805. https://doi.org/10.1016/j.brs.2018.02.017
Huang, Y. Z., Edwards, M. J., Rounis, E., Bhatia, K. P., & Rothwell, J. C. (2005). Theta burst stimulation of the human motor cortex. Neuron, 45(2), 201–206. https://doi.org/10.1016/j.neuron.2004.12.033
Rabey, J. M., Dobronevsky, E., Aichenbaum, S., Gonen, O., Marton, R. G., & Khaigrekht, M. (2013). Repetitive transcranial magnetic stimulation combined with cognitive training is a safe and effective modality for the treatment of Alzheimer’s disease: a randomized, double-blind study. Journal of Neural Transmission (Vienna), 120(5), 813–819. https://doi.org/10.1007/s00702-012-0902-z
Bentwich, J., Dobronevsky, E., Aichenbaum, S., Shorer, R., Peretz, R., Khaigrekht, M., Marton, R. G., & Rabey, J. M. (2011). Beneficial effect of repetitive transcranial magnetic stimulation combined with cognitive training for the treatment of Alzheimer’s disease: a proof of concept study. Journal of Neural Transmission, 118(3), 463–71. https://doi.org/10.1007/s00702-010-0578-1
Cotelli, M., Manenti, R., Cappa, S. F., Zanetti, O., & Miniussi, C. (2008). Transcranial magnetic stimulation improves naming in Alzheimer disease patients at different stages of cognitive decline. European Journal of Neurology, 15(12), 1286–1292. https://doi.org/10.1111/j.1468-1331.2008.02202.x
Chou, Y. H., Ton That, V., & Sundman, M. (2020). A systematic review and meta-analysis of rTMS effects on cognitive enhancement in mild cognitive impairment and Alzheimer’s disease. Neurobiology of Aging, 86, 1–10. https://doi.org/10.1016/j.neurobiolaging.2019.08.020
Buss, S. S., Fried, P. J., & Pascual-Leone, A. (2019). Therapeutic noninvasive brain stimulation in Alzheimer’s disease and related dementias. Current Opinion in Neurology, 32(2), 292–304. https://doi.org/10.1097/WCO.0000000000000669
Reed, T., & Cohen, Kadosh R. (2018). Transcranial electrical stimulation (tES) mechanisms and its effects on cortical excitability and connectivity. Journal of Inherited Metabolic Disease, 41(6), 1123–30. https://doi.org/10.1007/s10545-018-0181-4
Radman, T., Ramos, R. L., Brumberg, J. C., & Bikson, M. (2009). Role of cortical cell type and morphology in subthreshold and suprathreshold uniform electric field stimulation in vitro. Brain Stimulation, 2(4), 215-228.e1. https://doi.org/10.1016/j.brs.2009.03.007
Kubanek, J. (2018). Neuromodulation with transcranial focused ultrasound. Neurosurgical Focus, 44(2), E14. https://doi.org/10.3171/2017.11.FOCUS17621
Brunoni, A. R., Teng, C. T., Correa, C., Imamura, M., Brasil-Neto, J. P., Boechat, R., Rosa, M., Caramelli, P., Cohen, R., Del Porto, J. A., Boggio, P. S., & Fregni, F. (2010). Neuromodulation approaches for the treatment of major depression: challenges and recommendations from a working group meeting. Arquivos de Neuro-Psiquiatria, 68(3), 433–51. https://doi.org/10.1590/s0004-282x2010000300021
Reato, D., Rahman, A., Bikson, M., & Parra, L. C. (2010). Low-intensity electrical stimulation affects network dynamics by modulating population rate and spike timing. The Journal of Neuroscience, 30(45), 15067–79. https://doi.org/10.1523/JNEUROSCI.2059-10.2010
Macdonald, D. B. (2002). Safety of intraoperative transcranial electrical stimulation motor evoked potential monitoring. Journal of Clinical Neurophysiology, 19(5), 416–429. https://doi.org/10.1097/00004691-200210000-00005
Francis, J., & Dingley, J. (2015). Electroanaesthesia–from torpedo fish to TENS. Anaesthesia, 70(1), 93–103. https://doi.org/10.1111/anae.12887
Nordanskog, P., Larsson, M. R., Larsson, E. M., & Johanson, A. (2014). Hippocampal volume in relation to clinical and cognitive outcome after electroconvulsive therapy in depression. Acta Psychiatrica Scandinavica, 129(4), 303–311. https://doi.org/10.1111/acps.12150
O’Connor, M., Lebowitz, B. K., Ly, J., Panizzon, M. S., Elkin-Frankston, S., Dey, S., Bloomingdale, K., Thall, M., & Pearlman, C. (2008). A dissociation between anterograde and retrograde amnesia after treatment with electroconvulsive therapy: A naturalistic investigation. The Journal of ECT, 24(2), 146–151. https://doi.org/10.1097/YCT.0b013e318158792f
McClintock, S. M., Choi, J., Deng, Z.-D., Appelbaum, L. G., Krystal, A. D., & Lisanby, S. H. (2014). Multifactorial determinants of the neurocognitive effects of electroconvulsive therapy. The Journal of ECT, 30, 165–176. https://doi.org/10.1097/YCT.0000000000000137
Antal, A., & Herrmann, C. S. (2016). Transcranial alternating current and random noise stimulation: Possible mechanisms. Neural Plasticity, 2016, 3616807.
Gebodh, N., Esmaeilpour, Z., Adair, D., Schestattsky, P., Fregni, F., & Bikson, M. (2019). Transcranial direct current stimulation -among technologies for low-intensity transcranial electrical stimulation: Classification, history, and terminology. Practical Guide to Transcranial Direct Current Stimulation Book Chap, 1, 3–44.
Guleyupoglu, B., Schestatsky, P., Edwards, D., Fregni, F., & Bikson, M. (2013). Classification of methods in transcranial electrical stimulation (tES) and evolving strategy from historical approaches to contemporary innovations. Journal of Neuroscience Methods, 219(2), 297–311. https://doi.org/10.1016/j.jneumeth.2013.07.016
Battleday, R. M., Muller, T., Clayton, M. S., & Cohen, Kadosh R. (2014). Mapping the mechanisms of transcranial alternating current stimulation: A pathway from network effects to cognition. Frontiers in Psychiatry, 5, 162. https://doi.org/10.3389/fpsyt.2014.00162
Babiloni, C., Lizio, R., Marzano, N., Capotosto, P., Soricelli, A., Triggiani, A. I., Cordone, S., Gesualdo, L., & Del Percio, C. (2016). Brain neural synchronization and functional coupling in Alzheimer’s disease as revealed by resting state EEG rhythms. International Journal of Psychophysiology, 103, 88–102.
Reinhart, R. M., Cosman, J. D., Fukuda, K., & Woodman, G. F. (2017). Using transcranial direct-current stimulation (tDCS) to understand cognitive processing. Attention, Perception, & Psychophysics, 79(1), 3–23. https://doi.org/10.3758/s13414-016-1224-2
Fertonani, A., Pirulli, C., & Miniussi, C. (2011). Random noise stimulation improves neuroplasticity in perceptual learning. The Journal of Neuroscience, 31(43), 15416–23. https://doi.org/10.1523/JNEUROSCI.2002-11.2011
Miniussi, C., Harris, J. A., & Ruzzoli, M. (2013). Modelling non-invasive brain stimulation in cognitive neuroscience. Neuroscience & Biobehavioral Reviews, 37(8), 1702–1712. https://doi.org/10.1016/j.neubiorev.2013.06.014
Brem, A.-K., Almquist, J.N.-F., Mansfield, K., Plessow, F., Sella, F., Santarnecchi, E., Orhan, U., McKanna, J., Pavel, M., Mathan, S., Yeung, N., Pascual-Leone, A., Kadosh, R. C., Honeywell SHARP Team authors. (2018). Modulating fluid intelligence performance through combined cognitive training and brain stimulation. Neuropsychologia, 118(Pt A), 107–114. https://doi.org/10.1016/j.neuropsychologia.2018.04.008
Herrmann, C. S., Rache, S., Neuling, T., & Strüber, D. (2013). Transcranial alternating current stimulation: A review of the underlying mechanisms and modulation of cognitive processes. Frontiers in Human Neuroscience, 7, 279. https://doi.org/10.3389/fnhum.2013.00279
Dhaynaut, M., Pascual-Leone, A., Santarnecchi, E., & Fakhri, G. E. (2020). Effects of modulating gamma oscillations via 40 Hz transcranial alternating current stimulation (tACS) on Tau PET imaging in mild to moderate Alzheimer’s Disease. Journal of Nuclear Medicine, 61, 340–340.
Menardi, A., Rossi, S., Koch, G., Hampel, H., Vergallo, A., Nitsche, M. A., Stern, Y., Borroni, B., Cappa, S. F., Cotelli, M., Ruffini, G., El-Fakhri, G., Rossini, P. M., Dickerson, B., Antal, A., Babiloni, C., Lefaucheur, J. P., Dubois, B., Deco, G., … Santarnecchi, E. (2022). Toward noninvasive brain stimulation 2.0 in Alzheimer’s disease. Ageing Research Reviews, 75, 101555. https://doi.org/10.1016/j.arr.2021.101555
Priori, A., Hallett, M., & Rothwell, J. C. (2009). Repetitive transcranial magnetic stimulation or transcranial direct current stimulation? Brain Stimulation, 2(4), 241–245. https://doi.org/10.1016/j.brs.2009.02.004
Yamada, Y., & Sumiyoshi, T. (2021). Neurobiological mechanisms of transcranial direct current stimulation for psychiatric disorders; Neurophysiological, chemical, and anatomical considerations. Frontiers in Human Neuroscience, 15, 631838. https://doi.org/10.3389/fnhum.2021.631838
Cambiaghi, M., Velikova, S., Gonzalez-Rosa, J. J., Cursi, M., Comi, G., & Leocani, L. (2010). Brain transcranial direct current stimulation modulates motor excitability in mice. European Journal of Neuroscience, 31(4), 704–709. https://doi.org/10.1111/j.1460-9568.2010.07092.x
Kabakov, A. Y., Muller, P. A., Pascual-Leone, A., Jensen, F. E., & Rotenberg, A. (2012). Contribution of axonal orientation to pathway-dependent modulation of excitatory transmission by direct current stimulation in isolated rat hippocampus. Journal of Neurophysiology, 107(7), 1881–1889. https://doi.org/10.1152/jn.00715.2011
Jackson, M. P., Rahman, A., Lafon, B., Kronberg, G., Ling, D., Parra, L. C., & Bikson, M. (2016). Animal models of transcranial direct current stimulation: Methods and mechanisms. Clinical Neurophysiology, 127(11), 3425–3454. https://doi.org/10.1016/j.clinph.2016.08.016
Jefferys, J. G. (1981). Influence of electric fields on the excitability of granule cells in Guinea-pig hippocampal slices. The Journal of Physiology, 319, 143–152. https://doi.org/10.1113/jphysiol.1981.sp013897
Chan, C. Y., Hounsgaard, J., & Nicholson, C. (1988). Effects of electric fields on transmembrane potential and excitability of turtle cerebellar Purkinje cells in vitro. The Journal of Physiology, 402, 751–771. https://doi.org/10.1113/jphysiol.1988.sp017232
Bikson, M., Inoue, M., Akiyama, H., Deans, J. K., Fox, J. E., Miyakawa, H., & Jefferys, J. G. (2004). Effects of uniform extracellular DC electric fields on excitability in rat hippocampal slices in vitro. The Journal of Physiology, 557(Pt 1), 175–190. https://doi.org/10.1113/jphysiol.2003.055772
Creutzfeldt, O. D., Fromm, G. H., & Kapp, H. (1962). Influence of transcortical d-c currents on cortical neuronal activity. Experimental Neurology, 5, 436–452. https://doi.org/10.1016/0014-4886(62)90056-0
Bindman, L. J., Lippold, O. C., & Redfearn, J. W. (1964). The action of brief polarizing currents on the cerebral cortex of the rat (1) during current flow and (2) in the production of long-lasting after-effects. The Journal of Physiology, 172(3), 369–382. https://doi.org/10.1113/jphysiol.1964.sp007425
Merzagora, A. C., Foffani, G., Panyavin, I., Mordillo-Mateos, L., Aguilar, J., Onaral, B., & Oliviero, A. (2010). Prefrontal hemodynamic changes produced by anodal direct current stimulation. Neuroimage, 49(3), 2304–10. https://doi.org/10.1016/j.neuroimage.2009.10.044
Cabral, J., Hugues, E., Sporns, O., & Deco, G. (2011). Role of local network oscillations in resting-state functional connectivity. Neuroimage, 57(1), 130–139. https://doi.org/10.1016/j.neuroimage.2011.04.010
Stagg, C. J., Antal, A., & Nitsche, M. A. (2018). Physiology of transcranial direct current stimulation. The Journal of ECT, 34(3), 144–152. https://doi.org/10.1097/YCT.0000000000000510
Venkatakrishnan, A., Contreras-Vidal, J. L., Sandrini, M., & Cohen, L. G. (2011). Independent component analysis of resting brain activity reveals transient modulation of local cortical processing by transcranial direct current stimulation. Annual International Conference of the IEEE Engineering in Medicine and Biology Society. https://doi.org/10.1109/IEMBS.2011.6091998
Clark, V. P., Coffman, B. A., Trumbo, M. C., & Gasparovic, C. (2011). Transcranial direct current stimulation (tDCS) produces localized and specific alterations in neurochemistry: A 1H magnetic resonance spectroscopy study. Neuroscience Letters, 500(1), 67–71. https://doi.org/10.1016/j.neulet.2011.05.244
Stagg, C. J., Bachtiar, V., Amadi, U., Gudberg, C. A., Ilie, A. S., Sampaio-Baptista, C., O’Shea, J., Woolrich, M., Smith, S. M., Filippini, N., Near, J., & Johansen-Berg, H. (2014). Local GABA concentration is related to network-level resting functional connectivity. elife, 3, e01465. https://doi.org/10.7554/eLife.01465
Bachtiar, V., Near, J., Johansen-Berg, H., & Stagg, C. J. (2015). Modulation of GABA and resting state functional connectivity by transcranial direct current stimulation. eLife, 4, e08789. https://doi.org/10.7554/eLife.08789
Hunter, M. A., Coffman, B. A., Gasparovic, C., Calhoun, V. D., Trumbo, M. C., & Clark, V. P. (2015). Baseline effects of transcranial direct current stimulation on glutamatergic neurotransmission and large-scale network connectivity. Brain Research, 1594, 92–107. https://doi.org/10.1016/j.brainres.2014.09.066
Nitsche, M. A., Jaussi, W., Liebetanz, D., Lang, N., Tergau, F., & Paulus, W. (2004). Consolidation of human motor cortical neuroplasticity by D-cycloserine. Neuropsychopharmacology, 29(8), 1573–1578. https://doi.org/10.1038/sj.npp.1300517
Joundi, R. A., Jenkinson, N., Brittain, J. S., Aziz, T. Z., & Brown, P. (2012). Driving oscillatory activity in the human cortex enhances motor performance. Current Biology, 22(5), 403–407. https://doi.org/10.1016/j.cub.2012.01.024
Moisa, M., Polania, R., Grueschow, M., & Ruff, C. C. (2016). Brain network mechanisms underlying motor enhancement by transcranial entrainment of gamma oscillations. The Journal of Neuroscience, 36(47), 12053–12065. https://doi.org/10.1523/JNEUROSCI.2044-16.2016
Mccaig, C. D., Sangster, L., & Stewart, R. (2000). Neurotrophins enhance electric field-directed growth cone guidance and directed nerve branching. Developmental Dynamics, 217(3), 299–308.
Neal, A. P., & Guilarte, T. R. (2010). Molecular neurobiology of lead (Pb(2+)): Effects on synaptic function. Molecular Neurobiology, 42(3), 151–60. https://doi.org/10.1007/s12035-010-8146-0
Minichiello, L. (2009). TrkB signalling pathways in LTP and learning. Nature Reviews Neuroscience, 10(12), 850–860. https://doi.org/10.1038/nrn2738
Pelletier, S. J., & Cicchetti, F. (2014). Cellular and molecular mechanisms of action of transcranial direct current stimulation: evidence from in vitro and in vivo models. International Journal of Neuropsychopharmacology, 18(2), pyu047. https://doi.org/10.1093/ijnp/pyu047
Nitsche, M. A., Lampe, C., Antal, A., Liebetanz, D., Lang, N., Tergau, F., & Paulus, W. (2006). Dopaminergic modulation of long-lasting direct current-induced cortical excitability changes in the human motor cortex. European Journal of Neuroscience, 23(6), 1651–1657. https://doi.org/10.1111/j.1460-9568.2006.04676.x
Nitsche, M. A., Kuo, M. F., Karrasch, R., Wächter, B., Liebetanz, D., & Paulus, W. (2009). Serotonin affects transcranial direct current-induced neuroplasticity in humans. Biological Psychiatry, 66(5), 503–508. https://doi.org/10.1016/j.biopsych.2009.03.022
Polanía, R., Paulus, W., Antal, A., & Nitsche, M. A. (2011). Introducing graph theory to track for neuroplastic alterations in the resting human brain: A transcranial direct current stimulation study. Neuroimage, 54(3), 2287–96. https://doi.org/10.1016/j.neuroimage.2010.09.085
Fonteneau, C., Redoute, J., Haesebaert, F., Le Bars, D., Costes, N., Suaud-Chagny, M. F., & Brunelin, J. (2018). Frontal transcranial direct current stimulation induces dopamine release in the ventral striatum in human. Cerebral Cortex, 28(7), 2636–2646. https://doi.org/10.1093/cercor/bhy093
Fukai, M., Bunai, T., Hirosawa, T., Kikuchi, M., Ito, S., Minabe, Y., & Ouchi, Y. (2019). Endogenous dopamine release under transcranial direct-current stimulation governs enhanced attention: a study with positron emission tomography. Translational Psychiatry, 9(1), 115. https://doi.org/10.1038/s41398-019-0443-4
Ferrucci, R., Mameli, F., Guidi, I., Mrakic-Sposta, S., Vergari, M., Marceglia, S., Cogiamanian, F., Barbieri, S., Scarpini, E., & Priori, A. (2008). Transcranial direct current stimulation improves recognitionmemory in Alzheimer’s disease. Neurology, 71(7), 493–8. https://doi.org/10.1212/01.wnl.0000317060.43722.a3
Hsu, W. Y., Ku, Y., Zanto, T. P., & Gazzaley, A. (2015). Effects of noninvasive brain stimulation on cognitive function in healthy aging and Alzheimer’s disease: A systematic review and meta-analysis. Neurobiology of Aging, 36(8), 2348–2359. https://doi.org/10.1016/j.neurobiolaging.2015.04.016
Cotelli, M., Manenti, R., Brambilla, M., Petesi, M., Rosini, S., Ferrari, C., Zanetti, O., & Miniussi, C. (2014). Anodal tDCS during face-name associations memory training in Alzheimer’s patients. Frontiers in Aging Neuroscience, 6, 38. https://doi.org/10.3389/fnagi.2014.00038
Bystad, M., Grønli, O., Rasmussen, I. D., Gundersen, N., Nordvang, L., Wang-Iversen, H., & Aslaksen, P. M. (2016). Transcranial direct current stimulation as a memory enhancer in patients with Alzheimer’s disease: A randomized, placebo-controlled trial. Alzheimer’s Research & Therapy, 8(1), 13. https://doi.org/10.1186/s13195-016-0180-3
Elder, G. J., & Taylor, J. P. (2014). Transcranial magnetic stimulation and transcranial direct current stimulation: Treatments for cognitive and neuropsychiatric symptoms in the neurodegenerative dementias? Alzheimer’s Research & Therapy, 6(9), 74. https://doi.org/10.1186/s13195-014-0074-1
Naeser, M. A., & Hamblin, M. R. (2011). Potential for transcranial laser or LED therapy to treat stroke, traumatic brain injury, and neurodegenerative disease. Photomedicine and Laser Surgery, 29(7), 443–446. https://doi.org/10.1089/pho.2011.9908
Vöröslakos, M., Takeuchi, Y., Brinyiczki, K., Zombori, T., Oliva, A., Fernández-Ruiz, A., Kozák, G., Kincses, Z. T., Iványi, B., Buzsáki, G., & Berényi, A. (2018). Direct effects of transcranial electric stimulation on brain circuits in rats and humans. Nature Communications, 9(1), 483. https://doi.org/10.1038/s41467-018-02928-3
Antal, A., Grossman, N., & Paulus, W. (2021). Basic Mechanisms of Transcranial Alternating Current and Random Noise Stimulation. In A. R. Brunoni, M. A. Nitsche, & C. K. LooBook (Eds.), Transcranial Direct Current Stimulation in Neuropsychiatric Disorders Clinical Principles and Management (2nd ed., pp. 21–28). Cham: Springer.
Teselink, J., Bawa, K. K., Koo, G. K., Sankhe, K., Liu, C. S., Rapoport, M., Oh, P., Marzolini, S., Gallagher, D., Swardfager, W., Herrmann, N., & Lanctôt, K. L. (2021). Efficacy of non-invasive brain stimulation on global cognition and neuropsychiatric symptoms in Alzheimer’s disease and mild cognitive impairment: A meta-analysis and systematic review. Ageing Research Reviews, 72, 101499. https://doi.org/10.1016/j.arr.2021.101499
Bikson, M., Grossman, P., Thomas, C., Zannou, A. L., Jiang, J., Adnan, T., Mourdoukoutas, A. P., Kronberg, G., Truong, D., Boggio, P., Brunoni, A. R., Charvet, L., Fregni, F., Fritsch, B., Gillick, B., Hamilton, R. H., Hampstead, B. M., Jankord, R., Kirton, A., … Woods, A. J. (2016). Safety of transcranial direct current stimulation: Evidence based update 2016. Brain Stimulation, 9(5), 641–661. https://doi.org/10.1016/j.brs.2016.06.004
Stultz, D. J., Osburn, S., Burns, T., Pawlowska-Wajswol, S., & Walton, R. (2020). Transcranial magnetic stimulation (TMS) safety with respect to seizures: A literature review. Neuropsychiatric Disease and Treatment, 16, 2989–3000. https://doi.org/10.2147/NDT.S276635
Cai, M., Guo, Z., Xing, G., Peng, H., Zhou, L., Chen, H., McClure, M. A., He, L., Xiong, L., He, B., Du, F., & Mu, Q. (2019). Transcranial direct current stimulation improves cognitive function in mild to moderate Alzheimer disease: A meta-analysis. Alzheimer Disease & Associated Disorders, 33(2), 170–178. https://doi.org/10.1097/WAD.0000000000000304
Boggio, P. S., Khoury, L. P., Martins, D. C., Martins, O. E., de Macedo, E. C., & Fregni, F. (2009). Temporal cortex direct current stimulation enhances performance on a visual recognition memory task in Alzheimer disease. Journal of Neurology, Neurosurgery & Psychiatry, 80(4), 444–7. https://doi.org/10.1136/jnnp.2007.141853
Boggio, P. S., Ferrucci, R., Mameli, F., Martins, D., Martins, O., Vergari, M., Tadini, L., Scarpini, E., Fregni, F., & Priori, A. (2012). Prolonged visual memory enhancement after direct current stimulation in Alzheimer’s disease. Brain Stimulation, 5(3), 223–230. https://doi.org/10.1016/j.brs.2011.06.006
Marceglia, S., Mrakic-Sposta, S., Rosa, M., Ferrucci, R., Mameli, F., Vergari, M., Arlotti, M., Ruggiero, F., Scarpini, E., Galimberti, D., Barbieri, S., & Priori, A. (2016). Transcranial Direct current stimulation modulates cortical neuronal activity in Alzheimer’s disease. Frontiers in Neuroscience, 10, 134. https://doi.org/10.3389/fnins.2016.00134
Suemoto, C. K., Apolinario, D., Nakamura-Palacios, E. M., Lopes, L., Leite, R. E., Sales, M. C., Nitrini, R., Brucki, S. M., Morillo, L. S., Magaldi, R. M., & Fregni, F. (2014). Effects of a non-focal plasticity protocol on apathy in moderate Alzheimer’s disease: A randomized, double-blind, sham-controlled trial. Brain Stimulation, 7(2), 308–313. https://doi.org/10.1016/j.brs.2013.10.003
Yang, W. J., Wen, H. Z., Zhou, L. X., Luo, Y. P., Hou, W. S., Wang, X., & Tian, X. L. (2019). After-effects of repetitive anodal transcranial direct current stimulation on learning and memory in a rat model of Alzheimer’s disease. Neurobiology of Learning and Memory, 161, 37–45. https://doi.org/10.1016/j.nlm.2019.02.002
Luo, Y., Yang, W., Li, N., Yang, X., Zhu, B., Wang, C., Hou, W., Wang, X., Wen, H., & Tian, X. (2020). Anodal transcranial direct current stimulation can improve spatial learning and memory and attenuate Aβ42 burden at the early stage of Alzheimer’s disease in APP/PS1 transgenic mice. Frontiers in Aging Neuroscience, 13(12), 134. https://doi.org/10.3389/fnagi.2020.00134
Karim, A. A., Kammer, T., Lotze, M., Nitsche, M. A., Godde, B., Hinterberger, T., Cohen, L., & Birbaumer, N. (2004). Effects of TMS and tDCS on the physiological regulation of cortical excitability in a brain-computer interface. Biomedizinische Technik, 49(1), 55–57.
Hansen, N. (2012). Action mechanisms of transcranial direct current stimulation in Alzheimer’s disease and memory loss. Frontiers in Psychiatry, 3, 48. https://doi.org/10.3389/fpsyt.2012.00048
Acknowledgements
The authors wish to thank Prof. Kang-Ping Lin, Prof. Dong-Her Shih, Prof. Chou-Ching Lin and Dr. Min-Wei Huang for reviewing this paper. We thank I-Chun Hung, Hsiu Hua Wang, Liang Chao Huang and Li-Hui Wang for their excellent technical assistance extended for this study. We also thank Munusamy Thirumavalavan for his correction of English syntax errors.
Funding
The study was supported by research grants from Ministry of Science and Technology and Tainan hospital, Ministry of Health and Welfare, Taiwan.
Author information
Authors and Affiliations
Contributions
Development of research ideas and design: CSMW and KSC. Data extraction: CSMW and WHC. Drafting of the manuscript: CSMW, KSC, YKY and KSC. All authors contributed to the development of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflict of interest.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent to Publish
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, C.SM., Chang, WH., Yang, YK. et al. Comparing Transcranial Direct Current Stimulation (tDCS) with Other Non-Invasive Brain Stimulation (NIBS) in the Treatment of Alzheimer’s Disease: A Literature Review. J. Med. Biol. Eng. 43, 362–375 (2023). https://doi.org/10.1007/s40846-023-00810-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-023-00810-2