Abstract
Purpose
This study investigated the effects of insertion speed of dental implants on their stability.
Methods
Dental implants were inserted at speeds of 4, 10, 20, and 30 rpm, respectively, into artificial bones of two different bone qualities; namely, good bone (GB) and poor bone (PB). Therefore, the four insertion speeds and two bone qualities totaled eight groups, with five specimens per group. During the insertion process, the maximum insertion torque value (ITV) was measured, along with two stability parameters: periotest value (PTV) and initial stability quotient (ISQ).
Results
Dental implants in the GB group exhibited better stability than those in the PB group (p < 0.001). Significant differences in ITVs were observed among the four insertion speeds in both the GB and PB groups (p = 0.004 and p = 0.034, respectively). In general, the higher the insertion speed, the lower the ITV; in particular, the ITVs for implants inserted at 4 rpm were higher than those measured at 20 and 30 rpm (p = 0.008). However, regardless of the bone quality, the PTVs did not differ significantly among the four insertion speeds (p = 0.066). In both the GB and PB groups, the ISQs differed significantly differences among the four insertion speeds (p = 0.016 and p = 0.004, respectively).
Conclusion
The stability parameters measured for dental implants in the GB group were all higher than those measured in the PB group. In general, a higher insertion speed resulted in a lower ITV value. The PTV did not differ significantly, while the ISQ differed significantly among the four insertion speeds.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Caries, periodontal diseases, infection, and trauma can cause root and alveolar resorption of permanent teeth. These conditions can result in tooth avulsion or even the need for tooth extraction [1]. One treatment for tooth loss is dental implant surgery. Osseointegration is the key factor in determining the success of dental implant surgery, and the initial stability of an implant is a good indicator of osseointegration effectiveness [2,3,4,5,6]. Osteointegration refers to the natural bonding between the implant and the alveolar bone. Cancellous bone calcified on the implant surface increases the contact area, gradually allowing it to withstand occlusal force [7]. A literature review reported that the primary stability of an implant is commonly used to predict the effect of osseointegration, in which high primary stability indicated a high likelihood of surgery success. Monje et al. [8] noted that since primary stability is measured immediately following implantation, it can also be referred to as mechanical stability. The insertion torque value (ITV), initial stability quotient (ISQ), and implant stability parameter (periotest value, PTV), can be used as indicators of stability. Furthermore, implant survival and marginal alveolar bone loss around the implant can also be used for assessment [9]. In other words, the primary stability of the implant contributes to the success of subsequent osseointegration, thereby facilitating long-term success. Before performing dental implant surgery, biomechanical considerations are also required to increase the primary stability after insertion. These biomechanical considerations include bone quality, bone volume, and implant length and diameter, which affect the stress distribution of an implant. Moreover, different bone qualities, including density and texture, are encountered during dental implantation. The jaw bone can be categorized into types 1–4 according to bone density [10], with types 2 and 3 generally considered the most favorable for osseointegration. Anterior mandibles are typically the densest, while posterior maxillae are the most porous [11]. However, when inserting an implant from the alveolar crest to the target depth, the bone density and type also change gradually. Bone volume and quantity are also important. The larger the bone volume, the greater the implant length and diameter. Longer and wider implants can increase the amount of bone interfacing with the implant, resulting in the ability to withstand a greater mechanical load [12].
Previous studies have reported on the relationship between implant insertion speed and torque [7, 13, 14]. Sumer et al. [15] investigated the heat generated during implant insertion, concluding that manual implant insertion at speeds of 30 and 50 rpm generated lower heat compared to insertion at 100 rpm. Di Stefano et al. [16] inserted implants into artificial bones at a constant speed of 35 rpm and explored the feasibility of using the insertion torque-depth curve as the basis for determining the primary stability of the implant. The authors concluded that the torque-depth curve integral provided a reliable assessment of primary stability and showed greater sensitivity to density variations compared to other known parameters used to assess primary stability. Yamaguchi et al. [17] examined the effects of implant design on primary stability, measured the maximum insertion torque, and plotted the torque-time curves for implants inserted at 15 rpm with a 500 g load into artificial bones. The authors observed a maximum torque value in the torque-time curves during implant insertion. Previous studies reported a wide range of implant insertion speeds, from 4 to 100 rpm. However, the manufacturers determine insertion speed according to ASTM F543 when testing dental implants. This standard specifies that dental implants must be inserted at a speed of 4 rpm or greater [18]. This implant insertion speed is significantly slower than the 20–25 rpm typically used by clinicians. In general, dental implants are inserted at a speed set by the implant manufacturer. O’Sullivan et al. [19] suggested that the same slow insertion speed should be adopted for Mk IV implants under profuse sterile saline irrigation. Osseocare's dental handpiece, on the other hand, allows the operator to choose either fast or slow speeds for implant insertion [when the foot pedal is activated, the handpiece shaft rotates at the selected speed (high or low) until the maximum insertion torque is reached, at which point the unit shuts off]. Thus, the implant insertion speed is generally set by the implant or dental handpiece manufacturers. However, no study has reported the effects of insertion speed on implant stability.
Few studies have examined insertion speed [7, 13, 14]. Studies on speed generally focused on the effects of pre-drilled holes on temperature [20]. Several studies examined the effect of drilling speed in pre-drilled holes on subsequent implant stability [21, 22]. However, there are no common consensuses on the appropriate speed at which the dental implants should be inserted into the bone [7, 13, 14]. Several studies have investigated the effects of insertion speed on stability, based on screws for general material testing, including orthodontic miniscrews, and abutment screws [7, 13, 14]. However, none of these studies have evaluated the effects of implant insertion speed on the primary implant stability from a biomechanical perspective. Furthermore, the effects of insertion speed on implant stability are unclear. Thus, the present study investigated the effects of the insertion speed of dental implants on their stability.
2 Materials and Methods
2.1 Preparation of the Artificial Bone and Dental Implant Components
This study used Nobel Biocare’s Groovy Speedy, which provides a thread taper root form that resembles natural roots and is currently the most common form of root. The experiments used dental implants (Branemark Systems NobelSpeedy Groovy, Nobel Biocare AB, Gothenburg, Sweden) measuring 4.0 × 11.5 mm (diameter × length), similar to those commonly used in clinical practice (Fig. 1). Human alveolar bones are divided into the outer dense cortical bone and the inner cancellous bone with a trabecular structure. The present study used solid and cellular rigid polyurethane materials to simulate cortical (model 3401) and cancellous bones, respectively. Patient bone quality and quantity are also biomechanical conditions that should be evaluated before dental implant surgery. To this end, artificial bones (Pacific Research Laboratories, Vashon, Washington, USA) of two different qualities were selected to simulate good and poor bone types (GB and PB, respectively). Specifically, the artificial bone used to simulate GB was cancellous bone with an elastic modulus of 137 MPa and an upper layer cortical bone thickness of 2.5 mm, and an elastic modulus of 16.7 GPa. The artificial bone used to simulate the PB included cancellous bone with an elastic modulus of 12.4 MPa and the upper layer cortical bone with a thickness of 1.0 mm and an elastic modulus of 16.7 GPa (Fig. 1).
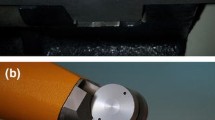
2.2 Four Insertion Speeds of Dental Implant
To ensure the dental implant was inserted into the artificial bone specimen at a vertical angle, a precision drilling machine was used to prepare pre-drilled holes 12.5 mm in length and 4 mm in diameter. As the bottom of the implant is flat, the bottom of the drill is pointed to drill into the bone. Therefore, the extra tip of the drill was approximately 1 mm longer than the implant. The dental implant was inserted using a torque-rotation machine. With a digital torque meter (TQ-8800, Lutron Electronic Enterprise, Taipei, Taiwan), torque values within the range of 0–150 N·cm can be measured with a resolution of 0.1 N·cm. This digital torque meter can be connected to a computer, record synchronous torque-time or torque-depth data, plot torque-time or torque-depth curves, and present the primary stability of a dental implant based on its maximum insertion torque value (ITV) (Fig. 2).
In this study, the implant insertion speeds were divided into four groups: (1) the insertion speed commonly used in the laboratory, i.e., 4 rpm, inserted using a torque rotation machine. The experimental design applied an axial force of 1.14 kg according to the ASTM F543 standard. (2–4) Insertion speeds commonly used by clinical dentists; i.e., 10, 20, and 30 rpm, inserted using an OsseoSet™ 300 Dental Surgical Unit (Nobel Biocare AB, Gothenburg, Sweden) with a resolution of 1 N·cm.
2.3 Measuring the ISQ and PTV of the Dental Implant
Following the insertion of the dental implant into the artificial bone, the other two stability parameters (PTV and ISQ) were measured using a clamp to secure the artificial bone in place. Upon implant insertion, the PTV was measured using a periotest device (Medizintechnik Gulden, Bensheim, Germany). The implant and abutment were fastened with the abutment screw before measurement. During each measurement, the distance and the angle between the periotest device and the abutment were also fixed. The lower the PTV, the better the implant stability. As the dental implant lacks the periodontal ligament of a natural tooth, the range of values measured is smaller and lower than those in natural teeth, resulting in poor sensitivity. Therefore, the angle and position at which the tapping head hits the abutment and the height of the abutment must be fixed so that these variables do not affect the measurement. In the present study, the artificial bone specimen was first placed in the clamp to control the tapping head to consistently hit the abutment at the same position and angle, thereby reducing errors (Fig. 3).
Next, the ISQ was measured using an Osstell ISQ™ (Osstell AB, Gothenborg, Sweden) wireless resonance frequency analyzer. A transducer (smart peg) was installed on top of the implant. The higher the ISQ, the better the implant stability. For measurement, the artificial bone was first fixed to the special fixture. The smart peg was then attached to the upper part of the implant instead of the abutment. In the present study, the ISQ values were recorded in artificial bone specimens of varying qualities to assess dental implant stability (Fig. 4).
2.4 Statistical Analysis
Dental implants were inserted into artificial bones of two different quality types at four different insertion speeds, resulting in eight sample groups. As there were only five samples per group, nonparametric statistical analysis was applied. First, Mann–Whitney U tests were used to assess the differences in stability of implants inserted into two bones of different qualities. Next, Kruskal–Wallis tests were used to determine the differences in stability of implants inserted at four different speeds. Post hoc pairwise comparisons were conducted using Mann–Whitney exact tests with Bonferroni adjustment. The significance level was set at 0.00833 (0.05/6). The statistical analysis was performed using IBM SPSS Statistics for Windows, version 19.0 (IBM Corp., Armonk, NY, USA).
3 Results
3.1 Insertion Speed Affects the Initial Stability of Dental Implants in the GB Groups
Effects of bone quality on implant stability parameters ITV, PTV, and ISQ: differences in the medians of ITV, PTV, and ISQ were observed between different bone quality groups. The stability values measured for implants in the GB group were higher than those measured in the PB group, the difference being statistically significant (p < 0.001).
As for the effects of the four insertion speeds on ITV, PTV, and ISQ in the good bone groups, there was no consistent pattern observed for these three parameters. The effects on each stability parameter were therefore discussed separately. The implant stability parameter ITV was significantly different among the four insertion speeds (p = 0.004). In general, a higher insertion speed would result in a lower ITV. In particular, ITVs measured for implants inserted at 4 rpm were higher than those inserted at 20 and 30 rpm (p = 0.008), and ITVs measured for implants inserted at 10 rpm were higher than those inserted at 30 rpm (p = 0.008). However, the implant stability parameter PTV did not differ significantly among the four insertion speeds (p = 0.066). Nonetheless, significant differences were observed in the implant stability parameter ISQ among the four insertion speeds (p = 0.016). In particular, ISQs measured for implants inserted at 4 rpm were lower than those inserted at 10 and 20 rpm (p = 0.008), but no significant difference was observed between ISQs for implants inserted at 4 and 30 rpm. Also, there were no significant differences between ISQs for implants inserted at 10, 20, and 30 rpm (Table 1).
The torque-time curves for dental implants inserted into the GB group at four different insertion speeds are presented in Fig. 5. All four insertion speeds showed rapid increases in torque at the beginning of the experiment, evidenced by the relatively steep slopes on the torque-time plots, as the implants encountered greater resistance upon insertion into the artificial cortical bone compared to the cancellous bone. Because the cortical bone has a dense structure, even when the counterbore drill was expanded into the cortical bone layer of the artificial bone, releasing pressure around the implant neck, the contact point with the cortical bone at approximately 1/3 of the lower part of the implant may still cause a rapid increase in torque. Once the insertion depth reached the cylinder portion of the implant at approximately more than two-thirds of the implant depth, the increase in torque slowed, with smaller slopes in the torque-time curves. The torque slowly increased until the entire implant was inserted.
3.2 Insertion Speed Affects the Initial Stability of Dental Implants in the PB Group
Similarly, when inserting implants into artificial bones with poor quality, the four insertion speeds showed no consistent pattern in their effects on the implant stability parameters (ITV, PTV, and ISQ).
ITV differed significantly among the four insertion speeds (p = 0.034). The ITVs for implants inserted at 4 rpm were higher than those inserted at 10, 20, and 30 rpm (p = 0.008); while the ITVs for implants inserted at 10, 20, and 30 rpm did not differ significantly (p > 0.05). The PTV did not differ significantly among the four insertion speeds (p = 0.066). However, the ISQ differed significantly among the four insertion speeds (p = 0.004), with higher values for implants inserted at 4 and 10 rpm compared to those inserted at 30 rpm (p = 0.008) (Table 2).
The torque-time curves for dental implants inserted into the PB group at four different insertion speeds are presented in Fig. 6. All four insertion speeds showed rapid torque increases at the beginning of the experiment, similar to the observations in the GB group. As the cortical bone is thinner in this group, the steep-slope part (time) of the torque curves is shortened as the implant passes relatively quickly through the cortical bone layer.
4 Discussion
A previous review showed that the primary stability of an implant is commonly used to predict the effect of osseointegration, in which high primary stability indicates a high likelihood of surgery success [8]. While many studies have explored factors affecting the primary stability of implants, few have investigated the effects of insertion speed on implant stability. The insertion speeds of implants in previous studies ranged widely, from 4 to 100 rpm [7, 15]. However, in their research and development process, the manufacturers of dental implants determine the insertion speed according to ASTM F543. The standard specifies that dental implants must be inserted at a speed of 4 rpm or greater [18]. This speed is significantly slower than the 20–30 rpm speed typically used by clinicians. Clinicians usually set the insertion speed according to the specifications of the implant or dental handpiece manufacturers. However, there is no discussion regarding the effects of insertion speed on implant stability. Several studies have investigated the effects of insertion speed on stability based on the examination of screws for general material testing, including orthodontic miniscrews, and abutment screws [7, 13, 14]. However, none of these studies discussed the effects of implant insertion speed on primary stability from a biomechanical perspective. The present study is the first to investigate the impact of different insertion speeds on implant stability using artificial bones. The results showed that, regardless of the bone quality, the faster the insertion speed, the smaller the torque. The clinical contribution of this study is that, if the dental handpiece manufacturer offers the option, a slow speed should be selected to ensure sufficient maximum insertion torque.
Previous studies have assessed the effect of primary stability on the surgical success rates of dental implants [8]. In their systematic review, Monje et al. [8] discussed the relationship between primary and secondary stability of dental implants. Primary stability is measured immediately following implantation, while secondary stability (also called biological stability) is measured after osseointegration. The authors showed that primary and secondary stability were highly correlated; i.e., the primary stability of an implant contributed to the subsequent success of osseointegration. Al-Sabbagh et al. [23] discussed the correlation between a primary implant stability and osseointegration. They noted that good primary stability relies on the mechanical friction between the implant surface and surrounding bone with an absence of mobility in the osteotomy site immediately after implant placement. The systematic review by Quesada-García et al. reported on the stability of implants using resonance frequency analysis. They reported that the clinical assessment of osseointegration was based on mechanical stability rather than histological criteria, based on primary stability (absence of mobility in the bone bed after implant insertion) and secondary stability (bone formation and remodeling at the implant-bone interface). Bassir et al. assessed the differences between early dental implant placement and other implant methods. The primary and secondary outcomes were implant failure and marginal bone level, respectively. The authors found that the marginal bone loss associated with early implant placement was significantly lower than that associated with immediate implant placement; thus, so the surgical outcome was more favorable than immediate implant placement. Therefore, the degree of marginal bone loss affected the implant stability and the quality of the surrounding bone, ultimately altering the implant's long-term stability.
The present study used artificial cortical bones of varying thicknesses and artificial cancellous bones of varying porosities to simulate jawbones with two different qualities. However, as artificial bone lacks blood supply, osseointegration cannot be assessed. Nevertheless, artificial bone offers sample consistency and is easier to obtain. Additionally, the ASTM F-1839 standard states that artificial foam bone is “… an ideal material for comparative testing of bones screws and other medical devices and instruments” [24]. Kim et al. [25] assessed implant stability based on ISQ values measured through resonance frequency analysis. They also examined the effects of combining different densities of trabecular layers and varying thicknesses of cortical bone layers on implant stability in artificial bones. They noted the challenges of evaluating implant stability in human alveolar bones and distinguishing between control and experimental groups under controlled conditions. Previous studies have also demonstrated the usefulness of artificial bone blocks to simulate cortical and trabecular bone conditions. Miyamoto et al. [26] reported mean cortical thicknesses of 2.22 ± 0.47 mm for the mandible and 1.49 ± 0.34 mm for the maxilla. Tabassum et al. [27] used a trabecular bone density of 0.48 g/cm3 and cortical bone thicknesses ranging from 0 to 2.5 mm to examine the effects of cortical bone thickness on the primary stability of implants inserted into polyurethane foam blocks (Sawbones). To mimic the cortical layer, on top of these blocks short-fiber-filled epoxy sheets were attached with a thickness varying from 0 to 2.5 mm. Hsu et al. [12] assessed the effects of bone-implant contact ratio and bone quality on primary implant stability, recommending the use of bone models with a cellular structure to mimic the human cancellous bone structure, as the two share a similar architecture. The results of the present study also suggested that bone models with a cellular structure are superior for elucidating the importance of primary implant stability because their architecture is similar to that of cancellous bone. Therefore, this study used artificial bones in its experiments.
Previous studies have examined the effects of bone quality on implant survival rates [8]. Schnitmann et al. [28] tracked 137 dental implants for 30 months, reporting success rates of 100% in the anterior mandible, 92.4% in the posterior mandible, 93.75% in the anterior maxilla, and 78.26% in the posterior maxilla. These results are consistent with Lekholom and Zarb’s classification of bone quality, which validated the reference value of this classification system. Jaffin et al. [29]compared 1,054 Branemark implants following dental implant surgery. Five years of tracking revealed that bone quality was the most critical factor affecting surgery outcomes. Based on Lekholom and Zarb’s bone classification, only 101 implants were implanted in type 4 bones; however, 36 implants in this group were extracted without osseointegration, accounting for 55% of the 65 failures across all four groups. Asma'a et al. [30] compared alveolar bone quality by computed tomography based on Lekholom and Zarb’classification system, with consistent results, which validated the reference value of this classification system. The authors also assessed cancellous bone density by computed tomography. Based on the differences in grayscale values, for the same cortical bone thickness for types 2 and 3, distinct subclassifications were derived from differences in cancellous bone density. At present, the general conclusion is that mandible quality is higher than maxilla quality, and density in the anterior portion is greater than that in the posterior portion. The present study used artificial bones of two different qualities. The results indicated positive correlations between jawbone quality and implant stability regardless of the insertion speed. Currently, three clinical methods are used to measure dental implant stability, namely: the maximum ITV, ISQ converted from resonance frequency analysis, and PTV measured using a periotest device. Among them, the maximum ITV is measured at the time of dental implant placement. The torque generated during implant insertion into the alveolar bone is measured, and can only be performed once at the time of surgery. Theoretically, the greater the ITV, the better the primary implant stability. In a systematic review of 37 articles, Monje et al. [8] assessed the reliability and feasibility and respective deficiencies of various methods for measuring implant stability, including the periotest in instrument vibration analysis, the ISQ obtained by resonance frequency analysis, and the insertion or reverse torque obtained by torque tests. Regarding implant insertion torque, a higher insertion torque leads to higher implant survival, with a high degree of reliability in terms of judging implant stability. To compare the correlation between implant stabilities measured by two non-invasive techniques, namely the periotest and the resonance frequency analysis, Kocak-Buyukdere et al. [31] measured 54 clinically stable implants on the day of dental implant surgery and 4 weeks later. They found that both measuring techniques are applicable in the assessment of implant stability. This study, however, found that the median values of ITV, PTV, and ISQ differed according to bone quality. The stability values measured for implants in the GB group were significantly higher than those measured in the PB group. The ISQ values in the GB and PB groups were 70–77 and 52–58, respectively. Atsumi et al. [32] reported that ISQ values in a specific range could be used to simulate different bone conditions, in which values < 50 may indicate a subsequent implant failure and values > 65 generally indicate surgical success. The ISQ range in the present study (70–77) was higher than the value of 65 suggested by Atsumi et al. [32]. This indicates that good bone quality contributes to increased surgical success rates; thus, the ISQ range in the present study was reasonable. Chakrapaniet al. [33] reported that the PTV range corresponds to mobility categories. This classification is based on the four degrees of tooth mobility described by Miller, from grade 0 to grade 3. A PTV value of − 8 to + 9 corresponds to grade 0, while a value of + 10 to + 19 corresponds to grade 1. The PTV range in the GB in the present study (0.6–2.5) corresponded to grade 0 mobility. The PTV range in the PB group (11.2–17.3) corresponded to grade 1 mobility. Thus, good bone quality reduced implant mobility. Accordingly, the PTV values in the present study were within reasonable ranges.
Previous studies on dental implant primary stability and insertion speed mostly focused on the effects of pre-drilling speed on implant primary stability during the preparation of pre-drilled holes [21, 22]. The general belief is that when preparing such holes, the drilling speed cannot exceed 47 rpm; otherwise, osteonecrosis will occur, preventing the implant from osseointegration. Several studies have explored the effects of drilling speed in preparing pre-drill holes on subsequent implant stability. Romanos et al. [21] prepared pre-drilled holes using two speeds in 240 artificial bones; half in artificial GB and PB, respectively. The authors then inserted three different brands of dental implants and measured the ISQ values. According to their statistical analysis, when implants from Group C (Eztetic-Zimmer, 3.1/11.5 mm) were implanted in artificial bones with GB, high ISQ was achieved for pre-drilled holes prepared with a lower drilling speed; when implants from Group A (NobelActive, 3.0/11.5 mm)were implanted in artificial bones with PB, high ISQ was achieved by preparing the pre-drilled hole with a higher drilling speed. No other significant differences were observed in the remaining groups. Thus, the authors concluded that the drilling speed should be adjusted according to the bone quality to achieve higher implant stability. Seo et al. [22] prepared predrill holes at 50, 800, and 1200 rpm in the right and left mandibles of six dogs and then inserted implants. The authors then measured the primary stability ISQ and the proportion of new bone formation after sectioning to assess early bone healing. Two weeks and 1 month later, the implant stability differed significantly among the three drilling speeds, with the greatest difference between 50 and 1200 rpm and the best biological response at 1200 rpm. However, previous studies primarily focused on the effects of drilling speed on dental implant stability, particularly whether the heat generated while preparing the pre-drilled hole would result in poor bone healing. Studies on the effects of insertion speed on stability are relatively limited.
Few studies have examined the effect of implant insertion speed on implant stability. Nassar et al. [14] reported that the torque-tension on the thread was affected by tightening speed. With repeated tightening and loosening, the coefficient of friction of sliding surfaces increased for tightening speeds < 30 rpm. That study focused on insertion speed in the context of testing general industrial thread materials. In this study, regardless of bone quality, a higher insertion speed resulted in lower torque. In the GB group, the ITVs of implants inserted at 4 rpm were higher than those inserted at 20 and 30 rpm, while those inserted at 10 rpm were higher than those inserted at 30 rpm. In the PB group, the ITVs of implants inserted at 4 rpm were higher than those inserted at 10, 20, and 30 rpm. These results are consistent with those reported by Bulaqi et al. [13] that increasing the tightening speed also reduces the coefficient of friction, both of which resulted in reduced conical torque. Their study investigated the effects of insertion speed and coefficient of friction on the preload of an abutment screw using the finite element method. From the bottom up, the abutment was divided into three regions: a thread zone, a conical zone, and a wrench zone for applying insertion torque through rotation. Their study evaluated different insertion methods to prevent screw loosening. To achieve the recommended torque in the experiments, speeds of 15–30 rpm were used to insert the abutment screws. To achieve the recommended torque in this single-step simulation, angular displacement was applied to the head of the abutment screw at tightening speeds of 15–30 rpm under different frictional conditions. However, Whang et al. [7] examined the effects of insertion speed on insertion torque and found no statistically significant difference in peak insertion torque for 6-mm orthodontic miniscrews inserted at 4 or 8 rpm. The authors tested six commercially available orthodontic miniscrews, only one of which was subjected to insertion experiments with varying speeds. Thus, insertion speed was not the focus of their study. One explanation for the lack of statistical differences could be that all set speeds were < 10 rpm. This low speed is unlikely to show significant differences. Furthermore, orthodontic miniscrews are usually inserted by orthodontists using a screwdriver, so the speed will not be too fast. By comparison, the present study employed insertion speeds of 4–30 rpm and recorded torque-time curves to provide a more comprehensive understanding of the effects of insertion speed on torque. The ITV but not PTV differed significantly according to insertion speed. This may be because the ITV represents the torque generated during insertion, whereas the PTV represents the degree of contact between the dental implant and the surrounding bone as well as its mobility. These results suggest that different insertion speeds do not significantly alter the level of contact between the bone and the implant but do alter the torque produced. Therefore, further research is needed. ISQ differed significantly according to insertion speed. In the GB group, the ISQs for implants inserted at 4 rpm were lower than those inserted at 10 and 20 rpm but did not differ significantly between implants inserted at 4 and 30 rpm. The ISQs for implants inserted at 10, 20, and 30 rpm also did not differ significantly. In the PB group, the ISQs for implants inserted at 4 and 10 rpm were higher than those inserted at 30 rpm. The clinical contribution of this study is that, if a dental handpiece manufacturer offers the option of inserting an implant at fast or slow speeds, a slow speed should be selected to ensure sufficient maximum insertion torque. This finding is consistent with that reported by O'Sullivan et al., who noted that the Osseocare dental handpiece provides fast and slow speeds for the insertion of implants to achieve the desired maximum insertion torque. The Osseocare unit allows the operator to select preset maximum insertion torque values. When the foot pedal is activated, the handpiece shaft rotates at the selected speed (high or low) until the maximum insertion torque is reached, at which point the unit shuts off.
This study plotted four torque-time curves with different insertion speeds for each of the two bone quality groups. Regardless of GB or PB, the insertion torques of the four insertion speeds increased rapidly at the beginning of the curve, resulting in steep slopes that corresponded to the resistance experienced by the implant upon insertion into the artificial cortical bone. Stefano et al. [16]also plotted torque-depth curves but observed a uniform increase. This difference could be due to their use of polyurethane foam blocks of different densities to simulate the human alveolar bones, without solid material to simulate the cortical bones. They only used a single-layer structure, which could explain the stable slope of the curve. The artificial bones used in this study should be more similar to real bones.
This study has several limitations. Obtaining fresh cadaveric bones and minimizing the effects of varying bone samples can be challenging. Therefore, based on previous research, the experiments were performed on artificial bones. To represent jawbones of two different qualities, artificial cancellous bones of different porosities were combined with artificial cortical bones of different thicknesses. However, only two types of artificial bones cannot adequately simulate the four types (types 1–4) of jaw bone qualities classified by bone density in previous studies. The addition of artificial cancellous bones with different porosities and artificial cortical bones with different thicknesses will allow more accurate comparisons with the classification criteria. In addition, this study used only one brand and model of dental implants. Finally, this study was conducted in vitro solely from a biomechanical perspective without considering other biological reactions. Therefore, additional animal trials and clinical validations are required.
5 Conclusion
Despite the limitations of this study, the results showed that both bone quality and insertion speed affected implant stability. The three stability parameters (ITV, PTV, and ISQ) measured for dental implants in the GB group were all higher than those measured in the PB group. The ITV differed significantly among the four insertion speeds, and a lower insertion speed would result in a higher ITV. Both bone quality groups showed higher ITVs for implants inserted at 4 rpm compared to those inserted at 20 and 30 rpm. Additionally, the ISQ differed significantly among the four insertion speeds, with differing effects between the GB and PB groups. Finally, the PTV did not differ significantly among the four insertion speeds.
Data Availability
The data sets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Kinane, D. F., Stathopoulou, P. G., & Papapanou, P. N. (2017). Periodontal diseases. Nature Reviews Disease Primers, 3, 1–14.
Hsu, J.-T., Wu, A.Y.-J., Fuh, L.-J., & Huang, H.-L. (2017). Effects of implant length and 3D bone-to-implant contact on initial stabilities of dental implant: A microcomputed tomography study. BMC Oral Health, 17, 1–8.
Javed, F., Ahmed, H. B., Crespi, R., & Romanos, G. E. (2013). Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interventional Medicine and Applied Science, 5, 162–167.
Jokar, H., Rouhi, G., & Abolfathi, N. (2020). The effects of splinting on the initial stability and displacement pattern of periodontio-integrated dental implants: A finite element investigation. Journal of Medical and Biological Engineering, 40, 719–726.
Karnik, N., Bhadri, K., Bora, U., Joshi, S., & Dhatrak, P. (2021). A Mathematical model for biomechanical evaluation of micro-motion in dental prosthetics using vibroacoustic RFA. Journal of Medical and Biological Engineering, 41, 571–580.
Cui, Q., Wang, R., Faller, L.-M., Kan, T., Jiang, X., Zhu, F., Zhu, W., & Liu, Y. (2022). Temperature field in bone during robotic dental implant drilling: theoretical models and in vitro experiments. Journal of Medical and Biological Engineering, 42, 253–262.
Whang, C., Bister, D., & Sherriff, M. (2011). An in vitro investigation of peak insertion torque values of six commercially available mini-implants. The European Journal of Orthodontics, 33, 660–666.
Monje, A., Ravidà, A., Wang, H.-L., Helms, J. A., & Brunski, J. B. (2019). Relationship between primary/mechanical and secondary/biological implant stability. International Journal of Oral & Maxillofacial Implants, 34, s7–s23.
Yun, H.-J., Park, J.-C., Yun, J.-H., Jung, U.-W., Kim, C.-S., Choi, S.-H., & Cho, K.-S. (2011). A short-term clinical study of marginal bone level change around microthreaded and platform-switched implants. Journal of Periodontal & Implant Science, 41, 211–217.
Alghamdi, H. S. (2018). Methods to improve osseointegration of dental implants in low quality (type-IV) bone: An overview. Journal of Functional Biomaterials, 9, 7.
Fuh, L. J., Huang, H. L., Chen, C. S., Fu, K. L., Shen, Y. W., Tu, M. G., Shen, W. C., & Hsu, J. T. (2010). Variations in bone density at dental implant sites in different regions of the jawbone. Journal of Oral Rehabilitation, 37, 346–351.
Hsu, J.-T., Huang, H.-L., Chang, C.-H., Tsai, M.-T., Hung, W.-C., & Fuh, L.-J. (2013). Relationship of three-dimensional bone-to-implant contact to primary implant stability and peri-implant bone strain in immediate loading: microcomputed tomographic and in vitro analyses. International Journal of Oral & Maxillofacial Implants, 28, 367–374.
Bulaqi, H. A., Mashhadi, M. M., Geramipanah, F., Safari, H., & Paknejad, M. (2015). Effect of the coefficient of friction and tightening speed on the preload induced at the dental implant complex with the finite element method. The Journal of Prosthetic Dentistry, 113, 405–411.
Nassar, S. A., Ganeshmurthy, S., Ranganathan, R. M., & Barber, G. C. (2007). Effect of tightening speed on the torque-tension and wear pattern in bolted connections. Journal of Pressure Vessel Technology, 129, 426–440.
Sumer, M., Keskiner, I., Mercan, U., Misir, F., & Cankaya, S. (2014). Assessment of heat generation during implant insertion. The Journal of Prosthetic Dentistry, 112, 522–525.
Di Stefano, D. A., Arosio, P., Gastaldi, G., & Gherlone, E. (2018). The insertion torque-depth curve integral as a measure of implant primary stability: An in vitro study on polyurethane foam blocks. The Journal of Prosthetic Dentistry, 120, 706–714.
Yamaguchi, Y., Shiota, M., Munakata, M., Kasugai, S., & Ozeki, M. (2015). Effect of implant design on primary stability using torque-time curves in artificial bone. International Journal of Implant Dentistry, 1, 1–7.
A F543–17, American Society for Testing and Materials, (2008). ASTM F543–17 standard specification and test methods for metallic medical bone screws. American Society for Testing and Materials, West Conshohocken
O’Sullivan, D., Sennerby, L., Jagger, D., & Meredith, N. (2004). A comparison of two methods of enhancing implant primary stability. Clinical Implant Dentistry and Related Research, 6, 48–57.
Mihali, S. G., Canjau, S., Cernescu, A., Bortun, C. M., Wang, H.-L., & Bratu, E. (2018). Effects of a short drilling implant protocol on osteotomy site temperature and drill torque. Implant Dentistry, 27, 63–68.
Romanos, G. E., Ciornei, G., Jucan, A., Malmstrom, H., & Gupta, B. (2014). In vitro assessment of primary stability of Straumann® implant designs. Clinical Implant Dentistry and Related Research, 16, 89–95.
Seo, D.-U., Kim, S.-G., Oh, J.-S., & Lim, S.-C. (2017). Comparative study on early osseointegration of implants according to various drilling speeds in the mandible of dogs. Implant Dentistry, 26, 841–847.
Al-Sabbagh, M., Eldomiaty, W., & Khabbaz, Y. (2019). Can osseointegration be achieved without primary stability? Dental Clinics, 63, 461–473.
A F1839–08, American Society for Testing and Materials, (2008). ASTM F1839–08 standard specification for rigid polyurethane foam for use as a standard material for testing orthopedic devices and instruments. American Society for Testing and Materials, West Conshohocken
Kim, D.-S., Lee, W.-J., Choi, S.-C., Lee, S.-S., Heo, M.-S., Huh, K.-H., Kim, T.-I., & Yi, W.-J. (2014). Comparison of dental implant stabilities by impact response and resonance frequencies using artificial bone. Medical Engineering & Physics, 36, 715–720.
Miyamoto, I., Tsuboi, Y., Wada, E., Suwa, H., & Iizuka, T. (2005). Influence of cortical bone thickness and implant length on implant stability at the time of surgery—Clinical, prospective, biomechanical, and imaging study. Bone, 37, 776–780.
Tabassum, A., Meijer, G. J., Wolke, J. G., & Jansen, J. A. (2010). Influence of surgical technique and surface roughness on the primary stability of an implant in artificial bone with different cortical thickness: A laboratory study. Clinical Oral Implants Research, 21, 213–220.
Schnitman, P., Rubenstein, J., Woehrle, P., DaSilva, J., & Koch, G. (1988). Implants for partial edentulism. The International Journal of Oral Implantology Implantologist, 5, 33–35.
Jaffin, R. A., & Berman, C. L. (1991). The excessive loss of Branemark fixtures in type IV bone: A 5-year analysis. Journal of Periodontology., 62, 2–4.
Asma’a, A. (2021). Comparative study of the accuracy of CBCT implant site measurements using different software programs. The Saudi Dental Journal, 33, 355–361.
Kocak-Buyukdere, A., & Kayabay, G. (2021). Measurement of dental implant stability by two different techniques. Nigerian Journal of Clinical Practice, 24, 973.
Atsumi, M., Park, S.-H., & Wang, H.-L. (2007). Methods used to assess implant stability: current status. International Journal of Oral & Maxillofacial Implants, 22, 743–754.
Chakrapani, S., Goutham, M., Krishnamohan, T., Anuparthy, S., Tadiboina, N., & Rambha, S. (2015). Periotest values: Its reproducibility, accuracy, and variability with hormonal influence. Contemporary Clinical Dentistry, 6, 12.
Funding
This research was supported by China Medical University, Taiwan (CMU110-S-05).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or personal relationships with people or organizations that could be considered inappropriate for conducting this study.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hsu, YY., Tsai, MT., Huang, HL. et al. Insertion Speed Affects the Initial Stability of Dental Implants. J. Med. Biol. Eng. 42, 516–525 (2022). https://doi.org/10.1007/s40846-022-00742-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-022-00742-3