Abstract
Introduction
The PrismRA® test identifies rheumatoid arthritis (RA) patients who are unlikely to respond to anti-tumor necrosis factor (anti-TNF) therapies. This study evaluated the clinical and financial outcomes of incorporating PrismRA into routine clinical care of RA patients.
Methods
A decision-analytic model was created to evaluate clinical and economic outcomes in the 12-month period following first biologic treatment. Two treatment strategies were compared: (1) observed clinical decision-making based on a 175-patient cohort receiving an anti-TNF therapy as their first biologic after failure of conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) and (2) modeled clinical decision-making of the same population using PrismRA results to inform first-line biologic treatment choice. Modeled costs include biologic drug pharmacy, non-biologic pharmacy, and total medical costs. The odds of inadequate response to anti-TNF therapies and various components of patient care were calculated based on PrismRA results.
Results
Identifying predicted inadequate responders to anti-TNF therapies resulted in a modeled 38% increase in ACR50 response to first-line biologic therapies. The fraction of patients who achieved an ACR50 response to any therapy (TNFi and others) within the 12-month period was 33% higher in the PrismRA-stratified population than in the unstratified population (59 vs. 44%, respectively). When therapy prescriptions were modeled according to PrismRA results, cost savings were modeled for all financial variables: overall costs (4% decreased total, 19% decreased on ineffective treatments), total biologic drug pharmacy (4% total, 23% ineffective), non-biologic pharmacy (2% total, 19% ineffective), and medical costs (6% total, 19% ineffective). Female sex was the clinical metric that showed the greatest association with inadequate response to anti-TNF therapies (odds ratio 2.42, 95% confidence interval 1.20, 4.88).
Conclusions
If PrismRA is implemented into routine clinical care as modeled, predicting which RA patients will have an inadequate response to anti-TNF therapies could save > $7 million in overall ineffective healthcare costs per 1000 patients tested and increase targeted DMARD response rates in RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Anti-tumor necrosis factor (Anti-TNF) therapies are expensive and represent a significant financial burden to the healthcare system; however, two-thirds of rheumatoid arthritis (RA) patients do not adequately respond to anti-TNF therapies, and instead experience prolonged pain, continued inflammation, and often require a higher dose of steroids. |
PrismRA® is a molecular signature test that uses precision medicine to accurately predict inadequate response to anti-TNF therapies in RA patients initiating targeted therapy after failing conventional synthetic disease-modifying antirheumatic drugs (DMARDs). |
The study modeled the stratification of RA patients by PrismRA® into responders and inadequate responders to anti-TNF therapies and evaluated the impact on financial and clinical outcomes. |
What has been learned from the study? |
Response to first-line targeted DMARDs, defined as ACR50, improved from 30% in the unstratified patient cohort to over 40% in the stratified patient cohort, which resulted in cost savings per patient, reduced overall spend by 4%, and reduced ineffective biologic treatment spend by 19%. |
If PrismRA® is incorporated into the clinical care of RA patients as modeled, understanding which patients will have an inadequate response to anti-TNF therapies could save more than $7 million in ineffective healthcare expenditures for every 1000 patients tested and increase observed response rates not only for those predicted inadequate responders, but for all RA patients who are starting a biologic or targeted therapy for the first time. |
Introduction
Initial treatment of rheumatoid arthritis (RA) involves conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) such as methotrexate, hydroxychloroquine, leflunomide, and sulfasalazine. For the 60% of RA patients who fail to achieve treatment guideline targets of low disease activity (LDA) or remission with csDMARDs [1, 2], there are a number of biologic and targeted therapies that have been approved by regulatory agencies in the United States (US) and abroad. These therapies include tumor necrosis factor-alpha inhibitors (anti-TNF), T cell co-stimulation modulators, Janus kinase inhibitors (JAK), interleukin-6 (IL-6) inhibitors, interleukin-1 (IL-1) inhibitors, and B cell inhibitors. However, nearly 90% of first-line biologics received by patients with RA are an anti-TNF therapy [3, 4]. Two-thirds of such patients receiving an anti-TNF therapy as their first biologic treatment will fail to satisfy the ACR50 criteria within 6 months [5]. Thus, a patient and rheumatologist typically must go through multiple trial-and-error attempts prior to improvement in disease activity. This process often entails continued disease progression manifesting as progressive joint damage, prolonged pain, persistent inflammation, increased use of corticosteroids, patient frustration, and significant expenditures without results [6]. Proactive identification of patients who will not respond to anti-TNF therapies would allow prompt redirection to alternative therapeutics and provide a patient a greater opportunity to rapidly reach treatment targets.
Precision medicine in rheumatology is enabling customized treatment approaches and care of RA patients [7,8,9,10,11,12,13,14,15]. Currently, there is no tool for rheumatologists to predict which drug is most likely to result in a patient achieving treat-to-target goals of LDA or remission. A test called PrismRA integrates molecular features detected in whole blood with clinical metrics to identify a signature of inadequate response to anti-TNF therapy, before the start of first-line targeted or biologic treatment [16]. PrismRA was validated using prospectively collected data from biologic-naïve patients who did not reach their treatment targets while being treated with csDMARDs and were determined to be candidates for biologic therapy initiation [16].
This study evaluated the financial and clinical outcomes of incorporating the PrismRA molecular signature test into the clinical care of patients with RA. First, a decision-analytic model using ACR50 as the threshold of response evaluated the cost savings resulting from implementation of the PrismRA test. Second, the clinical utility of PrismRA was demonstrated as the results of this test were associated with a higher likelihood of an inadequate response to anti-TNF therapies than the entire population of RA patients about to be started on their first biologic agent.
Methods
Patient Population
The 175-patient cohort has been described previously [16, 17]. Briefly, prospectively collected data from biologic-naïve patients with RA enrolled in the Consortium of Rheumatology Researchers of North America (CORRONA) Comparative Effectiveness Registry to Study Therapies for Arthritis and Inflammatory Conditions (CERTAIN) [17] study were used to validate the biomarkers identifying inadequate response to anti-TNF therapies [16]. Patients in this study had moderate to high disease activity at enrollment and were starting a biologic agent. This analysis included only patients who were biologic-naïve at enrollment, had not reached their treatment targets while being treated with csDMARD, and were starting an anti-TNF therapy. The previous studies described were conducted in accordance with the Helsinki Declaration. Institutional Review Board or Ethics Committee approvals and patient consent were obtained prior to sample collection and study participation. Biological samples and detailed clinical metrics were collected at baseline prior to initiation of anti-TNF therapy as well as at 3 and 6 months of treatment, as described previously [17]. A 29-patient subset of individuals who were ≥ 65 years old was evaluated separately.
Evaluation of Response to Anti-TNF Therapy
Response at 6 months following anti-TNF therapy initiation was defined by ACR50: ≥ 50% improvement in 28 tender joint count, ≥ 50% improvement in 28 swollen joint count, and ≥ 50% improvement in at least three out of five clinical variables [Health Assessment Questionnaire disability index (HAQ-DI), patient pain assessment, patient global assessment, physician global assessment, and C-reactive protein level (CRP)] [18]. The PrismRA development was described previously [16]; the underlying biomarker panel predicts the likelihood of inadequate response to anti-TNF therapies by evaluating ten single nucleotide polymorphisms, eight transcripts, sex, body mass index, C-reactive protein, anti-cyclic citrullinated protein, and patient global assessment. The fraction of patients who achieved European League Against Rheumatism (EULAR) good response (improvement in Disease Activity Score in 28 joints [DAS28]-CRP > 1.2 relative to baseline), and LDA and remission were assessed for DAS28-CRP (LDA = 2.4–2.9; remission ≤ 2.4).
Statistical Analyses
Odds ratios (ORs) were used to represent the strength of association between the clinical metrics and failure to achieve an ACR50 response while taking anti-TNF therapies. ORs and confidence intervals (CIs) were calculated as previously described [19, 20]. Analyses were performed using Python 3.7.6 (https://www.python.org) and R 3.6.1 (https://www.r-project.org). Patients were subdivided based on sex (male or female); BMI [underweight (< 18.5 kg/m2), average (≥ 18.5 to < 25.0 kg/m2), overweight (≥ 25.0 to < 30.0 kg/m2) and obese (≥ 30.0 kg/m2)], age (by decade); and tobacco smoking history (never, previous, or current). Continuous variables [number of tender joints, number of swollen joints and Clinical Disease Activity Index (CDAI)], are represented as box plots for ACR50 responders and inadequate responders and indicate the interquartile range, median and all scatter points.
Model Building
The methodology and training set of patient data was as previously described for the development of PrismRA [16]. Briefly, Random Forest from Scikit-learn [21,22,23] was used to build drug response classification models using baseline clinical metrics.
Decision-Analytic Model
A decision-analytic model compared two treatment strategies within a 12-month period from the start of the first biologic therapy, which were (1) observed clinical decision-making based on the CORRONA CERTAIN cohort and (2) modeled clinical decision-making on the same cohort based on stratification by the results of PrismRA. The most common disease improvement target evaluated in clinical trials involving RA patients is ACR20, which represents a 20% improvement in a standard set of clinical measures relative to baseline [18]. However, the more stringent metric of ACR50, representing a 50% improvement from baseline, more closely corresponds to changes to disease measures that reflect a patient reaching remission or LDA [24]. Hence, we used the ACR50 endpoint for our decision-making model, which assumes that patients who do not achieve ACR50 after 6 months of treatment will switch to a different biologic or targeted therapy.
For the first strategy, patients who followed a standard-of-care approach were evaluated using real-world data from the CERTAIN study for prescription rates. Patients in this cohort were prescribed an anti-TNF therapy (etanercept, adalimumab, infliximab, golimumab, certolizumab pegol) as first-line biologic treatment following inadequate response to csDMARD therapies. Patients were classified as responders or inadequate responders based on their real-world 6-month ACR50 outcomes. For patients classified as a responder, the model continued the assigned medication for another 6 months. For patients classified as inadequate responders, the model assigned the patient to a second-line treatment of either a different anti-TNF therapy or a different mechanism of action (MOA) (abatacept, rituximab, tocilizumab, tofacitinib) according to prescription patterns observed in the CERTAIN study. Published ACR50 response rates at 6 months to second-line therapies were used to assign the proportion of patients who achieved an ACR50 response. The average response rate for second-line alternative MOA therapies was obtained from published randomized control trials (Table S2) [5]. A weighted average of response rates was used from the longitudinal assessment of the patients: 60% of patients were assigned an anti-TNF therapy with a 16% ACR50 response rate and 40% of patients were assigned other MOA therapies with an average 26% ACR50 response rate (Table S3).
For the second strategy, the model determined anti-TNF response or anti-TNF inadequate response based on the PrismRA result using published performance metrics [16]. Patients who were predicted inadequate responders to anti-TNF therapies by PrismRA were diverted to another MOA therapy. Those patients who were not predicted to be inadequate responders by PrismRA were assigned an anti-TNF therapy. ACR50 response rates at 6 months were modeled using published efficacy metrics from randomized control trials (Table S2) [5]. Patients on anti-TNF therapy who achieved an ACR50 clinical response remained on that same anti-TNF therapy in the model. Patients who did not achieve an ACR50 response to first-line anti-TNF therapy were assigned another MOA therapy. Patients diverted from anti-TNF therapies and assigned an alternative MOA in the model were assumed to achieve response rates consistent with published studies (Table S2) [5]. Patients who did not achieve ACR50 response at 6 months according to the model were assigned a second MOA that differed from their first selection.
The modeled costs obtained from published studies [25,26,27] were assigned in three categories: (1) biologic pharmacy, (2) non-biologic pharmacy, and (3) total medical cost. Biologic pharmacy cost was determined from the payer perspective and calculated as total costs in 6-month intervals (Table S4). Total biologic costs included the total biologic drug and associated administration costs, based on actual drug utilization and drug administration [25]. Total medical cost included inpatient hospitalizations, joint replacement surgeries, infections, cardiovascular events, emergency department encounters, outpatient visits, physician office visits, rheumatologist office visits, physical/occupational therapy, durable medical equipment, and imaging such as radiographs, magnetic resonance imaging, and other types of imaging [26]. Non-biologic pharmacy costs included expenses related to outpatient pharmacy fills, with the exception of fills for biologic drugs (Table S5) [26]. A separate analysis evaluating individuals ≥ 65 years old was also carried out as described above.
Results
Patient Characteristics
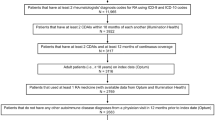
A total of 175 biologic-naïve RA patients from the CERTAIN study [17] who were about to receive an anti-TNF therapy as their first biologic were included in this study (Table 1). The fraction of patients who failed to achieve an observed ACR50 threshold in response to anti-TNF therapies was 69.7% (122/175). The study used a PrismRA score at or above 11.8 to define a group that would have a high or very high likelihood of inadequate response to anti-TNF therapies (Fig. 1 and Table S6) [16]. Of the 175 patients, 61 were correctly predicted as being inadequate responders while seven patients who achieved an ACR50 response were mis-classified as inadequate responders. The observed ACR50 response rate to anti-TNF therapies for those individuals who lacked a molecular signature of inadequate response was greater than that of the unstratified patient population (43% [46/107] vs. 30% [53/175]) [16].
PrismRA result. Biologic-naïve RA patients are stratified by PrismRA results: < 9.4 means a signal of inadequate response to TNF inhibitors is absent, at or above 9.4 is a moderate signal of inadequate response associated with ≥ 85% likelihood of inadequate response, ≥ 11.5 is a high signal of inadequate response associated with ≥ 90% likelihood of inadequate response, and ≥ 16.6 is a very high signal of inadequate response associated with ≥ 95% likelihood of inadequate response. In the decision-analytic model in this study, patients with ≥ 90% likelihood of inadequate response to anti-TNF therapies (PrismRA result ≥ 11.8) were defined as predicted inadequate responders
In the validation cohort, 29 RA patients were ≥ 65 years old and used to reflect PrismRA results for patients who are eligible for Medicare in the US. Among these individuals, PrismRA results for predicted inadequate responders had a positive predictive value (PPV) of 100% (95% CI 80–100) and a specificity of 100% (95% CI 60–100).
Patients who were predicted by PrismRA to have a molecular signature consistent with a moderate, high, or very high likelihood of inadequate response to anti-TNF therapies were not only less likely to achieve an ACR50 improvement in disease activity, but they were less likely to achieve LDA and remission, and were likely to have more swollen and tender joints following treatment (Fig. 2 and Tables S7, S8). Furthermore, a smaller proportion of the predicted inadequate responders achieved a EULAR good response than those identified as predicted responders (Fig. 2b). This suggests that although PrismRA was developed using ACR50 as the response measure, patients lacking the molecular signature of inadequate response to anti-TNF therapies achieved greater improvements in the signs and symptoms of RA by other widely used assessments.
Predicted inadequate responders are less likely to achieve LDA or remission. a Patients were stratified according to their PrismRA scores (none, low, moderate, and high signals of inadequate response to TNF inhibitors). a The fraction of patients in each group that achieved LDA or remission was determined using DAS28-CRP (LDA = 2.4–2.9; remission ≤ 2.4). b Predicted inadequate responders had a lower likelihood of achieving a EULAR good response (improvement > 1.2 in DAS28-CRP and a final DAS28-CRP ≤ 2.4). c DAS28-CRP, tender 28-joint counts, swollen 28-joint counts and CDAI scores at baseline and 6 months of anti-TNF therapy in the unstratified and PrismRA stratified patient populations. Box plots indicate the interquartile range, median, 95% confidence interval, and outliers
PrismRA Test Results are a Better Indicator of Inadequate Response to Anti-TNF Therapies than Current Clinical Metrics
Several baseline clinical variables have been associated with a lower response rate to anti-TNF therapies, including female sex, elevated BMI, and active tobacco smoking history [28, 29]. In order to compare these predictors to PrismRA, patients were re-evaluated after first being subdivided based on sex (male or female), BMI (average, overweight or obese), and age (by decade). In this cohort of patients, the odds of failing to achieve an ACR50 response was influenced by elevated BMI and female sex, but not age (Fig. 3a–c). To demonstrate that PrismRA is more predictive of inadequate response to anti-TNF therapies than current clinical baseline assessments and therefore an important advancement in the treatment of RA patients, the odds of achieving an ACR50 response was evaluated for clinical metrics. ORs and corresponding 95% CIs were used to represent the strength of association between the clinical metrics and inadequate response to anti-TNF therapies as defined by ACR50 (Table S9).
The percentage of inadequate anti-TNF therapy responders in relation to clinical metrics. For each clinical metric, the percentage of patients who inadequately respond to anti-TNF therapies (ACR50 criteria) is indicated at 6 months. The number of patients assessed in each category is reported below the category label. Clinical metrics evaluated include a sex, b BMI, c age, and d active tobacco smoking history. The OR and CI for female sex, obese BMI (≥ 30 kg/m2), age under 50 years old, and tobacco smoke exposure (current and previous) are indicated
A BMI corresponding to overweight (≥ 25 to < 30 kg/m2) or obese (≥ 30 kg/m2) correlates with a decreased response rate to anti-TNF therapies [29, 30] and BMI is included in the PrismRA biomarker panel [16]. Active cigarette smoking when biologic treatment is initiated is associated with a lower therapeutic response to anti-TNF therapies [28, 31]. However, evaluation of the validation cohort by active tobacco smoking history (never smoked, previous smoker, current smoker) revealed little influence on the response rate to anti-TNF therapies as assessed by ACR50 (Fig. 3d).
To assess whether clinical metrics were more predictive of inadequate response to anti-TNF therapies in combination, multivariate models were built using clinical metrics with the same machine learning approach and patient data as was used to develop the PrismRA molecular signature test [16]. Integrating only the clinical metrics resulted in a multivariate model with an OR of inadequate response of 1.34 (CI 0.67–2.34) for the training set data. The odds of a patient not responding to an anti-TNF therapy is nearly 6.6 times higher when that patient has a molecular signature consistent with inadequate response to anti-TNF therapies (OR 6.57; CI 2.75–15.70) [16]. Therefore, by integrating molecular gene expression data derived from patient blood with clinical variables, the PrismRA molecular signature test is a better predictor of inadequate response to anti-TNF therapies than baseline clinical metrics alone.
PrismRA Improved the Overall Response Rate for All First-Line Targeted Therapies
A decision-analytic model was created to systematically compile and evaluate the clinical and economic outcomes of PrismRA over a 12-month period from the start of the first biologic therapy (Fig. 4). This model compared two treatment strategies: (1) the standard-of-care clinical decision for 175 biologic-naïve patients who were prescribed an anti-TNF therapy as their first biologic, as documented in the CERTAIN comparative effectiveness study and modeled for which MOA was used after initial failure of the first anti-TNF therapy and (2) modeling of clinical decision-making in the same 175-patient population based on stratification of the first biologic using the PrismRA test.
Decision-analytic model comparing two treatment strategies within a 12-month period from the start of the first biologic therapy. A decision-analytic model compared two treatment strategies within a 12-month period from the start of the first biologic therapy. The strategies are a observed clinical decision-making based on a 175-patient biologic-naïve RA patient cohort receiving an anti-TNF therapy as the first biologic after failure of csDMARDs and b a clinical decision-making model of the same population using PrismRA prediction of inadequate response to anti-TNF therapies to stratify the first-line biologic. ACR50 responses were modeled at 6 and 12 months post-therapy initiation. Inadequate response is defined as a failure to achieve an ACR50 response. The percentages of the patients directed through each arm of the modeled strategy are indicated. The second targeted therapy was modeled as 60% to a second anti-TNF therapy and 40% to an alternative MOA (a biologic or targeted therapy other than a TNF inhibitor)
In the first treatment strategy, 70% (122/175) of patients did not achieve an ACR50 response at 6 months. These patients were re-assigned by the model to a second-line targeted therapy (60% second anti-TNF therapy, 40% alternative MOA). ACR50 response rates for second-line treatments at 12 months predicted a 20% ACR50 response rate (24/122 patients). The 30% of patients (53) who achieved an ACR50 response to their first anti-TNF therapy were assumed by the model to continue the same anti-TNF therapy for the entire 12-month period. Therefore, 44% (77/175) of the 175-patient cohort (53 first-line plus 24 second-line responders) were predicted to achieve an ACR50 response to a biologic or targeted therapy at 12-months.
In the second strategy, the same clinical modeling was applied to the same population after initial stratification of the first biologic using results of the PrismRA test. The 68 predicted inadequate responders (38.9%; 68/175) were assigned by the model another MOA, of which 27 (39.6%; 27/68) achieved an ACR50 response within 6 months. The 107 patients (61.1%; 107/175) who were not deselected by PrismRA were assigned an anti-TNF therapy, of which 46 (43.0%; 46/107) achieved an ACR50 response. The 61 anti-TNF therapy first-line patients who did not achieve an ACR50 response at 6 months (57.0%; 61/107) were assigned another MOA as second-line therapy, of which an additional 16 individuals (26.2%; 16/61) achieved an ACR50 response. Therefore, 57% of the 175-patient cohort (73 first-line therapy responders and 26 second-line therapy responders) were predicted to achieve an ACR50 response to a biologic or targeted therapy within the first 12-months of treatment. This response rate is consistent with typical 12-month ACR50 response rates reported in clinical trials (approximately 40–60%) [32,33,34,35,36,37].
Unlike other published findings [26], this PrismRA-stratified cohort did not show an increase in drug administration for patients who achieved response. There was no statistical difference in cumulative dosage in patients who were responders and inadequate responders. There was a slight escalation of dose in infliximab among inadequate responders, but this information was not integrated into the model.
Comparing both strategies, there was a 38% relative increase in observed response rate to first-line biologic therapies in the PrismRA-stratified population: 42% (73/175) versus 30% (53/175) in the unstratified patient population. Furthermore, an additional 15% of the original 175 patients (59% vs 44%; relative increase 33%) achieved an ACR50 response to any therapy within the 12-month period when stratified using PrismRA results.
Cost Savings Result From Redirection of Predicted Anti-TNF Inadequate Responders to Alternative First-Line Targeted Therapies
In addition to response rates, the decision-analytic model evaluated the costs of treatment for both strategies. The categories included biologic pharmacy, non-biologic pharmacy, and medical costs. The total cost for each category was reported along with the sub-category for ineffective treatment, defined as costs associated with patients who did not achieve an ACR50 response during the 12-month period.
For the first strategy (standard-of-care), biologic pharmacy was $6,684,216 ($4,179,592 ineffective), non-biologic pharmacy was $336,036 ($225,410 ineffective), and total medical costs were $1,956,878 ($1,462,966 ineffective). Hence, the overall total spend for the first strategy was $8,977,130 of which $5,867,969 (65%) was spent on patients who did not reach ACR50 within the 12-month period.
For the second strategy involving PrismRA stratification, biologic pharmacy was $6,391,856 ($3,213,121 ineffective), non-biologic pharmacy was $328,106 ($182,031 ineffective), and total medical costs were $1,833,602 ($1,181,429 ineffective). Hence, the overall total spend for this cohort of patients was $8,553,564, of which $4,576,581 (54%) was spent on patients who did not reach ACR50 within the 12-month period.
Consequently, PrismRA stratification yielded a 5% decrease in overall costs and 22% decrease in ineffective costs for the first 12 months after initiation of biologic therapy (Fig. 5). Cost savings were modeled for all three financial outcomes evaluated: total biologic drug pharmacy (4% total, 23% ineffective), non-biologic pharmacy (2% total, 19% ineffective) and total medical costs (6% total, 19% ineffective). This equated to savings of $7379 in overall ineffective costs per patient. Similar cost savings were observed when only those patients in the Medicare-eligible population were evaluated (≥ 65 years old, n = 29): 7% decrease in overall costs, 25% decrease for ineffective treatments), and savings of $6668 in ineffective costs per Medicare-eligible patient were observed. Therefore, stratification of the RA patient population using the PrismRA test resulted in cost savings in all aspects of medical care.
Decision-analytic model estimated reduction in ineffective treatment costs within a 12-month period. The cost of non-biologic pharmacy (orange), total medical cost (green), and biologic drug pharmacy (blue) is shown for the RA patient populations modeled by the two treatment strategies of the decision-analytic model. Ineffective treatment costs are indicated by the hashed pattern in the same color for each category. Data for a the entire 175-patient cohort and b the Medicare-eligible patient subcohort (≥ 65 years old) are shown
Discussion
Identifying anti-TNF therapy inadequate responders could yield significant direct cost savings to the healthcare system in terms of both total spend and ineffective treatment spend for biologic drugs, non-biologic drugs, and total medical cost spend. Modeling the impact of patient stratification in the 175-patient cohort using the PrismRA test lowered the fraction of costs spent on ineffective treatments by 18% (65% [5,867,969/8,977,130] vs. 54% ineffective [4,576,581/8,553,564]) in the unstratified population. Substantial cost savings were also observed in the subset of patients who are Medicare-eligible.
An analysis of 2006–2010 Medicare data revealed that of the 579,474 RA patients for whom data were available, 14,244 biologic-naïve individuals initiated an anti-TNF therapy [38]. Inferring anti-TNF therapy effectiveness based on claims data showing adherence to the therapy, the study reported that 72–77% of these biologic-naïve RA patients had an inadequate response to the anti-TNF therapies [38], similar to the overall inadequate response rates reported for this drug class. Modeling the performance of PrismRA in this ≥ 65 population, PrismRA stratification could have helped rheumatologists direct more than 5000 predicted anti-TNF inadequate responders to alternative therapies, thereby helping RA patients reach their treatment targets faster.
The PrismRA molecular signature test identifies RA patients who are predicted to be inadequate responders to anti-TNF therapies. It stratifies patients based on their unique disease biology, thereby enabling personalized therapy selection. A molecular signature is a combination of biological features, including RNA and protein, that capture an individual’s genetic makeup and reflect a patient’s distinctive disease biology. Some patients who are not identified as inadequate responders will still fail to have an adequate response to anti-TNF therapy for reasons that are unrelated to their molecular signature, such as the development of neutralizing anti-drug antibodies. Development of such antibodies has been reported for all anti-TNF therapies [39]. Patients identified as inadequate responders to anti-TNF therapies could be started on an alternative drug class approved as a first-line targeted DMARD to which they would have a better likelihood of reaching their treatment targets, while avoiding unnecessary TNF-cycling through a drug class that is predicted to provide minimal, if any, therapeutic benefit. Additionally, the remaining patient population not characterized as inadequate responders would also experience a higher observed response rate to anti-TNF therapies, thereby raising the overall first-line targeted therapy response rate in RA. Hence, stratification by PrismRA can raise the overall response rate to first-line biologic therapy in RA patients who have failed csDMARDs.
Many studies have reported algorithms and biomarkers that predict inadequate response to anti-TNF therapies [21, 40,41,42,43,44,45,46,47,48,49,50,51]. However, none of these models have been widely incorporated into the clinical care of RA patients. PrismRA captures a molecular signature of inadequate response to anti-TNF therapies that is not revealed by any other baseline clinical measurement (Table S9). The odds of a patient failing an anti-TNF therapy is nearly 6.6 times higher when that patient has a PrismRA inadequate response signature (OR 6.57; CI of 2.75–15.70) [16] over those patients who lack that signature. A previous study reported obesity as the strongest predictor of worse clinical outcomes in RA, defined as failure to achieve remission [29]. However, in the patient cohort discussed herein, female sex was the clinical metric that showed the greatest association with inadequate response to anti-TNF therapies. This difference highlights the importance of integrating multiple aspects of disease biology into a molecular signature that predicts inadequate response to targeted therapies across patient cohorts.
This study has the following limitations: (1) a sensitivity analysis was not performed on the model, (2) the cost savings model assumes that clinicians will change management of the patient when the patient does not respond to a medication within 6 months; however, retrospective data reveal that many inadequate responders to medications are kept on the same drug for longer periods of time, up to 18 months [52], (3) the model assumes that clinicians will prescribe with full adherence to the PrismRA test results, diverting patients who are not likely to respond to anti-TNF therapies to another MOA therapy, even though rheumatologists may be limited in doing so based on patient preference or payer formularies, and (4) the cost of PrismRA was not included in the model. Additionally, reported cost savings will depend on the price difference between the anti-TNF therapies and alternative MOA therapies used, which will differ based on formulary policies and use of biosimilars [53,54,55].
Under the treat-to-target strategy of managing RA, the timing and selection of treatment need to be carefully considered because these factors impact the probability of a patient reaching remission or LDA. Initiating effective treatment within 6–12 months of symptom onset can prevent permanent functional debilitation associated with damage of joints [56]. Additionally, response rates of first-line biologic therapies are higher for patients failing to reach treatment targets with methotrexate than for those patients who also have inadequately responded to an anti-TNF therapy [57]. Therefore, there is an urgent need for precision medicine tools that can identify which patients will not benefit from these advanced biologic and targeted therapies.
Conclusions
In 2018, healthcare spending in the U.S. reached 17.7% of gross domestic product at $3.6 trillion, the equivalent of $11,172 per person (https://www.cms.gov). In 2003, arthritis and rheumatologic conditions cost the US economy an estimated $81 billion in direct costs and $47 billion in indirect costs [58]. These expenditures have not yielded commensurate improvements in clinical outcomes [59, 60]. Precision medicine and biomarker-guided treatment represent a necessary step in advancing the clinical effectiveness and cost savings of all medications including targeted treatments for RA patients.
References
Emery P, Horton S, Dumitru RB, et al. Pragmatic randomised controlled trial of very early etanercept and MTX versus MTX with delayed etanercept in RA: the VEDERA trial. Ann Rheum Dis. 2020;79:464–71.
Bijlsma JWJ, Welsing PMJ, Woodworth TG, et al. Early rheumatoid arthritis treated with tocilizumab, methotrexate, or their combination (U-Act-Early): a multicentre, randomised, double-blind, double-dummy, strategy trial. Lancet. 2016;388(10042):343–55.
Jin Y, Desai RJ, Liu J, et al. Factors associated with initial or subsequent choice of biologic disease-modifying antirheumatic drugs for treatment of rheumatoid arthritis. Arthritis Res Ther. 2017;19(1):159.
Curtis JR, Zhang J, Xie F, et al. Use of oral and subcutaneous methotrexate in rheumatoid arthritis patients in the United States. Arthritis Care Res (Hoboken). 2014;66(11):1604–11.
Rein P, Mueller RB. Treatment with biologicals in rheumatoid arthritis: an overview. Rheumatol Ther. 2017;4(2):247–61.
Kvien TK. Epidemiology and burden of illness of rheumatoid arthritis. Pharmacoeconomics. 2004;22(2 Suppl 1):1–12.
Ma MHY, Defranoux N, Li W, et al. A multi-biomarker disease activity score can predict sustained remission in rheumatoid arthritis. Arthritis Res Ther. 2020;22(1):158.
Curtis JR, van der Helm-van Mil AH, Knevel R, et al. Validation of a novel multibiomarker test to assess rheumatoid arthritis disease activity. Arthritis Care Res (Hoboken). 2012;64(12):1794–803.
Shi J, Knevel R, Suwannalai P, et al. Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage. Proc Natl Acad Sci USA. 2011;108(42):17372–7.
Dervieux T, Furst D, Lein DO, et al. Pharmacogenetic and metabolite measurements are associated with clinical status in patients with rheumatoid arthritis treated with methotrexate: results of a multicentred cross sectional observational study. Ann Rheum Dis. 2005;64(8):1180–5.
Dervieux T, Greenstein N, Kremer J. Pharmacogenomic and metabolic biomarkers in the folate pathway and their association with methotrexate effects during dosage escalation in rheumatoid arthritis. Arthritis Rheum. 2006;54(10):3095–103.
Jilani AA, Mackworth-Young CG. The role of citrullinated protein antibodies in predicting erosive disease in rheumatoid arthritis: a systematic literature review and meta-analysis. Int J Rheumatol. 2015;2015:728610.
Humby F, Lewis M, Ramamoorthi N, et al. Synovial cellular and molecular signatures stratify clinical response to csDMARD therapy and predict radiographic progression in early rheumatoid arthritis patients. Ann Rheum Dis. 2019;78(6):761–72.
Wijbrandts CA, Tak PP. Prediction of response to targeted treatment in rheumatoid arthritis. Mayo Clin Proc. 2017;92(7):1129–43.
Johnson KJ, Sanchez HN, Schoenbrunner N. Defining response to TNF-inhibitors in rheumatoid arthritis: the negative impact of anti-TNF cycling and the need for a personalized medicine approach to identify primary non-responders. Clin Rheumatol. 2019;38(11):2967–76.
Johanna MTW, Asher A, Alex J, et al. Clinical validation of a blood-based predictive test for stratification of response to anti-TNF therapies in rheumatoid arthritis patients. Netw Syst Med. 2020;3(1):91–104.
Pappas DA, Kremer JM, Reed G, et al. Design characteristics of the CORRONA CERTAIN study: a comparative effectiveness study of biologic agents for rheumatoid arthritis patients. BMC Musculoskelet Disord. 2014;15:113.
Felson DT, Anderson JJ, Boers M, et al. American College of Rheumatology. Preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheum. 1995;38(6):727–35.
Szumilas M. Explaining odds ratios. J Can Acad Child Adolesc Psychiatry. 2010;19(3):227–9.
Sperandei S. Understanding logistic regression analysis. Biochem Med (Zagreb). 2014;24(1):12–8.
Bienkowska JR, Dalgin GS, Batliwalla F, et al. Convergent Random Forest predictor: methodology for predicting drug response from genome-scale data applied to anti-TNF response. Genomics. 2009;94(6):423–32.
Breiman L. Random forest. Mach Learn. 2001;45(1):5–32.
Pedregosa F, Varoquaux G, Gramfort A, Michel V, Thirion B, Grisel O, Blondel M, Prettenhofer P, Weiss R, Dubourg V, Vanderplas J. Scikit-learn: machine learning in Python. J Mach Learn Res. 2011;2012(12):2825–30.
Pokharel G, Deardon R, Barnabe C, et al. Joint estimation of remission and response for methotrexate-based DMARD options in rheumatoid arthritis: a bivariate network meta-analysis. ACR Open Rheumatol. 2019;1(8):471–9.
Gu T, Shah N, Deshpande G, et al. Comparing biologic cost per treated patient across indications among adult US managed care patients: a retrospective cohort study. Drugs Real World Outcomes. 2016;3(4):369–81.
Grabner M, Boytsov NN, Huang Q, et al. Costs associated with failure to respond to treatment among patients with rheumatoid arthritis initiating TNFi therapy: a retrospective claims analysis. Arthritis Res Ther. 2017;19(1):92.
Review IfCaE. A look at targeted immune modulators for rheumatoid arthritis. 2017. https://icer-review.org/wp-content/uploads/2017/04/NECEPAC_RA_RAAG_040717.pdf. Accessed 9 Apr 2020.
Hyrich KL, Watson KD, Silman AJ, et al. Predictors of response to anti-TNF-alpha therapy among patients with rheumatoid arthritis: results from the British Society for Rheumatology Biologics Register. Rheumatology (Oxford). 2006;45(12):1558–655.
Levitsky A, Brismar K, Hafstrom I, et al. Obesity is a strong predictor of worse clinical outcomes and treatment responses in early rheumatoid arthritis: results from the SWEFOT trial. RMD Open. 2017;3(2):e000458.
Singh S, Facciorusso A, Singh AG, et al. Obesity and response to anti-tumor necrosis factor-alpha agents in patients with select immune-mediated inflammatory diseases: a systematic review and meta-analysis. PLoS ONE. 2018;13(5):e0195123.
Abhishek A, Butt S, Gadsby K, et al. Anti-TNF-alpha agents are less effective for the treatment of rheumatoid arthritis in current smokers. J Clin Rheumatol. 2010;16(1):15–8.
Weinblatt ME, Schiff M, Valente R, et al. Head-to-head comparison of subcutaneous abatacept versus adalimumab for rheumatoid arthritis: findings of a phase IIIb, multinational, prospective, randomized study. Arthritis Rheum. 2013;65(1):28–38.
Isaacs JD, Salih A, Sheeran T, et al. Efficacy and safety of subcutaneous tocilizumab in rheumatoid arthritis over 1 year: a UK real-world, open-label study. Rheumatol Adv Pract. 2019;3(1):rkz010.
Keystone E, Heijde D, Mason D Jr, et al. Certolizumab pegol plus methotrexate is significantly more effective than placebo plus methotrexate in active rheumatoid arthritis: findings of a fifty-two-week, phase III, multicenter, randomized, double-blind, placebo-controlled, parallel-group study. Arthritis Rheum. 2008;58(11):3319–29.
Emery P, Burmester GR, Bykerk VP, et al. Evaluating drug-free remission with abatacept in early rheumatoid arthritis: results from the phase 3b, multicentre, randomised, active-controlled AVERT study of 24 months, with a 12-month, double-blind treatment period. Ann Rheum Dis. 2015;74(1):19–26.
Emery P, Bingham CO 3rd, Burmester GR, et al. Certolizumab pegol in combination with dose-optimised methotrexate in DMARD-naive patients with early, active rheumatoid arthritis with poor prognostic factors: 1-year results from C-EARLY, a randomised, double-blind, placebo-controlled phase III study. Ann Rheum Dis. 2017;76(1):96–104.
Breedveld FC, Weisman MH, Kavanaugh AF, et al. The PREMIER study: a multicenter, randomized, double-blind clinical trial of combination therapy with adalimumab plus methotrexate versus methotrexate alone or adalimumab alone in patients with early, aggressive rheumatoid arthritis who had not had previous methotrexate treatment. Arthritis Rheum. 2006;54(1):26–37.
Yun H, Xie F, Delzell E, et al. The comparative effectiveness of biologics among older adults and disabled rheumatoid arthritis patients in the Medicare population. Br J Clin Pharmacol. 2015;80(6):1447–57.
Thomas SS, Borazan N, Barroso N, et al. Comparative immunogenicity of TNF inhibitors: impact on clinical efficacy and tolerability in the management of autoimmune diseases. A systematic review and meta-analysis. BioDrugs. 2015;29(4):241–58.
Julia A, Erra A, Palacio C, et al. An eight-gene blood expression profile predicts the response to infliximab in rheumatoid arthritis. PLoS ONE. 2009;4(10):e7556.
Lequerre T, Gauthier-Jauneau AC, Bansard C, et al. Gene profiling in white blood cells predicts infliximab responsiveness in rheumatoid arthritis. Arthritis Res Ther. 2006;8(4):R105.
Sekiguchi N, Kawauchi S, Furuya T, et al. Messenger ribonucleic acid expression profile in peripheral blood cells from RA patients following treatment with an anti-TNF-alpha monoclonal antibody, infliximab. Rheumatology (Oxford). 2008;47(6):780–8.
Stuhlmuller B, Haupl T, Hernandez MM, et al. CD11c as a transcriptional biomarker to predict response to anti-TNF monotherapy with adalimumab in patients with rheumatoid arthritis. Clin Pharmacol Ther. 2010;87(3):311–21.
van Baarsen LG, Wijbrandts CA, Rustenburg F, et al. Regulation of IFN response gene activity during infliximab treatment in rheumatoid arthritis is associated with clinical response to treatment. Arthritis Res Ther. 2010;12(1):R11.
Koczan D, Drynda S, Hecker M, et al. Molecular discrimination of responders and nonresponders to anti-TNF alpha therapy in rheumatoid arthritis by etanercept. Arthritis Res Ther. 2008;10(3):R50.
Nerviani A, Di Cicco M, Mahto A, et al. A pauci-immune synovial pathotype predicts inadequate response to TNFalpha-blockade in rheumatoid arthritis patients. Front Immunol. 2020;11:845.
Nguyen MVC, Baillet A, Romand X, et al. Prealbumin, platelet factor 4 and S100A12 combination at baseline predicts good response to TNF alpha inhibitors in rheumatoid arthritis. Jt Bone Spine. 2019;86(2):195–201.
Thomson TM, Lescarbeau RM, Drubin DA, et al. Blood-based identification of non-responders to anti-TNF therapy in rheumatoid arthritis. BMC Med Genom. 2015;8:26.
Folkersen L, Brynedal B, Diaz-Gallo LM, et al. Integration of known DNA, RNA and protein biomarkers provides prediction of anti-TNF response in rheumatoid arthritis: results from the COMBINE study. Mol Med. 2016;22:322–8.
Ortea I, Roschitzki B, Ovalles JG, et al. Discovery of serum proteomic biomarkers for prediction of response to infliximab (a monoclonal anti-TNF antibody) treatment in rheumatoid arthritis: an exploratory analysis. J Proteomics. 2012;77:372–82.
Blaschke S, Rinke K, Maring M, et al. Haptoglobin-alpha1, -alpha2, vitamin D-binding protein and apolipoprotein C-III as predictors of etanercept drug response in rheumatoid arthritis. Arthritis Res Ther. 2015;17:45.
Acar M, Juneja P, Handel M. Treatment persistence of subcutaneous TNF inhibitors among Australian patients with immune-mediated rheumatic disease (IMRD). Open Access Rheumatol. 2018;10:151–60.
Mehr SR, Brook RA. Factors influencing the economics of biosimilars in the US. J Med Econ. 2017;20(12):1268–71.
Huskamp HA, Epstein AM, Blumenthal D. The impact of a national prescription drug formulary on prices, market share, and spending: lessons for Medicare? Health Aff (Millwood). 2003;22(3):149–58.
Parrish RH. Lecture 2-What Is a Formulary, Anyway? (Or the Cliff Notes Version of Drug Stewardship and Expense Control). Pharmacy (Basel). 2018;6(3):69.
Burgers LE, Raza K, van der Helm-van Mil AH. Window of opportunity in rheumatoid arthritis—definitions and supporting evidence: from old to new perspectives. RMD Open. 2019;5(1):e000870.
Rendas-Baum R, Wallenstein GV, Koncz T, et al. Evaluating the efficacy of sequential biologic therapies for rheumatoid arthritis patients with an inadequate response to tumor necrosis factor-alpha inhibitors. Arthritis Res Ther. 2011;13(1):R25.
Yelin E, Murphy L, Cisternas MG, et al. Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997. Arthritis Rheum. 2007;56(5):1397–407.
Bentley TG, Effros RM, Palar K, et al. Waste in the U.S. Health care system: a conceptual framework. Milbank Q. 2008;86(4):629–59.
Hussey PS, Wertheimer S, Mehrotra A. The association between health care quality and cost: a systematic review. Ann Intern Med. 2013;158(1):27–34.
Weinblatt ME, Keystone EC, Furst DE, et al. Adalimumab, a fully human anti-tumor necrosis factor alpha monoclonal antibody, for the treatment of rheumatoid arthritis in patients taking concomitant methotrexate: the ARMADA trial. Arthritis Rheum. 2003;48(1):35–45.
Keystone EC, Kavanaugh AF, Sharp JT, et al. Radiographic, clinical, and functional outcomes of treatment with adalimumab (a human anti-tumor necrosis factor monoclonal antibody) in patients with active rheumatoid arthritis receiving concomitant methotrexate therapy: a randomized, placebo-controlled, 52-week trial. Arthritis Rheum. 2004;50(5):1400–11.
Keystone E, Landewe R, van Vollenhoven R, et al. Long-term safety and efficacy of certolizumab pegol in combination with methotrexate in the treatment of rheumatoid arthritis: 5-year results from the RAPID 1 trial and open-label extension. Ann Rheum Dis. 2014;73(12):2094–100.
Smolen J, Landewe RB, Mease P, et al. Efficacy and safety of certolizumab pegol plus methotrexate in active rheumatoid arthritis: the RAPID 2 study. A randomised controlled trial. Ann Rheum Dis. 2009;68(6):797–804.
Moreland LW, Schiff MH, Baumgartner SW, et al. Etanercept therapy in rheumatoid arthritis. A randomized, controlled trial. Ann Intern Med. 1999;130(6):478–86.
Kay J, Matteson EL, Dasgupta B, et al. Golimumab in patients with active rheumatoid arthritis despite treatment with methotrexate: a randomized, double-blind, placebo-controlled, dose-ranging study. Arthritis Rheum. 2008;58(4):964–75.
Keystone EC, Genovese MC, Klareskog L, et al. Golimumab, a human antibody to tumour necrosis factor alpha given by monthly subcutaneous injections, in active rheumatoid arthritis despite methotrexate therapy: the GO-FORWARD Study. Ann Rheum Dis. 2009;68(6):789–96.
Maini R, St Clair EW, Breedveld F, et al. Infliximab (chimeric anti-tumour necrosis factor alpha monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving concomitant methotrexate: a randomised phase III trial. ATTRACT Study Group. Lancet. 1999;354(9194):1932–9.
Abe T, Takeuchi T, Miyasaka N, et al. A multicenter, double-blind, randomized, placebo-controlled trial of infliximab combined with low dose methotrexate in Japanese patients with rheumatoid arthritis. J Rheumatol. 2006;33(1):37–44.
Kremer JM, Russell AS, Emery P, et al. Long-term safety, efficacy and inhibition of radiographic progression with abatacept treatment in patients with rheumatoid arthritis and an inadequate response to methotrexate: 3-year results from the AIM trial. Ann Rheum Dis. 2011;70(10):1826–30.
Kremer JM, Dougados M, Emery P, et al. Treatment of rheumatoid arthritis with the selective costimulation modulator abatacept: twelve-month results of a phase iib, double-blind, randomized, placebo-controlled trial. Arthritis Rheum. 2005;52(8):2263–71.
Edwards JC, Szczepanski L, Szechinski J, et al. Efficacy of B-cell-targeted therapy with rituximab in patients with rheumatoid arthritis. N Engl J Med. 2004;350(25):2572–81.
Emery P, Fleischmann R, Filipowicz-Sosnowska A, et al. The efficacy and safety of rituximab in patients with active rheumatoid arthritis despite methotrexate treatment: results of a phase IIB randomized, double-blind, placebo-controlled, dose-ranging trial. Arthritis Rheum. 2006;54(5):1390–400.
Smolen JS, Beaulieu A, Rubbert-Roth A, et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double-blind, placebo-controlled, randomised trial. Lancet. 2008;371(9617):987–97.
Maini RN, Taylor PC, Szechinski J, et al. Double-blind randomized controlled clinical trial of the interleukin-6 receptor antagonist, tocilizumab, in European patients with rheumatoid arthritis who had an incomplete response to methotrexate. Arthritis Rheum. 2006;54(9):2817–29.
van der Heijde D, Strand V, Tanaka Y, et al. Tofacitinib in combination with methotrexate in patients with rheumatoid arthritis: clinical efficacy, radiographic, and safety outcomes from a twenty-four-month, Phase III Study. Arthritis Rheumatol. 2019;71(6):878–91.
Keystone EC, Taylor PC, Drescher E, et al. Safety and efficacy of baricitinib at 24 weeks in patients with rheumatoid arthritis who have had an inadequate response to methotrexate. Ann Rheum Dis. 2015;74(2):333–40.
Smolen JS, Kay J, Doyle MK, et al. Golimumab in patients with active rheumatoid arthritis after treatment with tumour necrosis factor alpha inhibitors (GO-AFTER study): a multicentre, randomised, double-blind, placebo-controlled, phase III trial. Lancet. 2009;374(9685):210–21.
Genovese MC, Schiff M, Luggen M, et al. Long-term safety and efficacy of abatacept through 5 years of treatment in patients with rheumatoid arthritis and an inadequate response to tumor necrosis factor inhibitor therapy. J Rheumatol. 2012;39(8):1546–54.
Emery P, Deodhar A, Rigby WF, et al. Efficacy and safety of different doses and retreatment of rituximab: a randomised, placebo-controlled trial in patients who are biological naive with active rheumatoid arthritis and an inadequate response to methotrexate (Study Evaluating Rituximab's Efficacy in MTX iNadequate rEsponders (SERENE)). Ann Rheum Dis. 2010;69(9):1629–35.
Emery P, Keystone E, Tony HP, et al. IL-6 receptor inhibition with tocilizumab improves treatment outcomes in patients with rheumatoid arthritis refractory to anti-tumour necrosis factor biologicals: results from a 24-week multicentre randomised placebo-controlled trial. Ann Rheum Dis. 2008;67(11):1516–23.
Burmester GR, Blanco R, Charles-Schoeman C, et al. Tofacitinib (CP-690,550) in combination with methotrexate in patients with active rheumatoid arthritis with an inadequate response to tumour necrosis factor inhibitors: a randomised phase 3 trial. Lancet. 2013;381(9865):451–60.
Acknowledgements
The authors would like to thank all the patients, physicians, and physician staff who have participated in the CORRONA CERTAIN substudy.
Funding
All work was funded by and the journal Rapid Service Fee was paid for by Scipher Medicine Corporation.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Lixia Zhang, Anna Jeter, and Johanna B. Withers are all full-time employees of and have stock ownership in Scipher Medicine Corporation. Martin J. Bergman is a shareholder of Johnson & Johnson; has received fees as a consultant from AbbVie, Amgen, AstraZeneca, BMS, Genentech/Roche, Gilead, Janssen, Merck, Novartis, Pfizer, Regeneron, Sandoz, Sanofi; and has served as a speaker for AbbVie, Amgen, AstraZeneca, Gilead, Novartis, Regeneron, Sanofi. Alan J. Kivitz is a shareholder of Amgen, Gilead Sciences, Inc., GlaxoSmithKline, Novartis, Pfizer and Sanofi; has received fees as a consultant from AbbVie, Boehringer Ingelheim, Flexion, Gilead Sciences, Inc., Janssen, Pfizer, Regeneron, Sanofi and SUN Pharma Advanced Research; and has served as a speaker for AbbVie, Celgene, Flexion, Genzyme, Horizon, Merck, Novartis, Pfizer, Regeneron, Sanofi, and UCB. Dimitrios A. Pappas and Joel M. Kremer are employees and shareholders of CORRONA, LLC. Martin Scipher Medicine and PrismRA are trademarks of Scipher Medicine Corporation. The PrismRA predictive model is proprietary to Scipher Medicine Corporation.
Compliance with Ethics Guidelines
The previous studies described were conducted in accordance with the Helsinki Declaration. Institutional Review Board or Ethics Committee approvals and patient consent were obtained prior to sample collection and study participation.
Data Availability
All data generated during this study are included in this published article or as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to: https://doi.org/10.6084/m9.figshare.12728597.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bergman, M.J., Kivitz, A.J., Pappas, D.A. et al. Clinical Utility and Cost Savings in Predicting Inadequate Response to Anti-TNF Therapies in Rheumatoid Arthritis. Rheumatol Ther 7, 775–792 (2020). https://doi.org/10.1007/s40744-020-00226-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-020-00226-3