Abstract
Objective
Volunteerism represents an important mechanism to promote resilience, empathy, and general well-being in medical students, a group that stands to benefit. Medical students report feelings of fatigue, burnout, exhaustion, and stress that correlates with poor academic performance, and significant decline in empathy over the 3rd year of both MD and DO programs. Volunteer motivations have been shown to mediate participant well-being. The relationship between medical student volunteer motivations and specific outcomes during the COVID-19 pandemic has not been addressed.
Methods
We characterized features of medical student volunteers during the COVID-19 pandemic in 2020, including volunteering motivation using the Volunteer Functions Inventory, the types of activities in which they participated, and the physical, psychosocial, and emotional outcomes they experienced following volunteering.
Results
Altruistic and humanitarian values–centric motivation predicts positive volunteering outcomes including increased resilience, ability to deal with disappointment and loss, and ability to cope with the COVID-19 pandemic. Values-centric motivation also increases volunteer empathy independent of educational stage. Values-centric participants were more likely to select volunteering activities with patient contact, which promotes student empathy and resilience. Conversely, career-centric motivation does not predict positive outcomes. These students are more likely to engage in research-oriented activities.
Conclusions
The efficacy of integrating volunteerism into medical school curricula may be limited by professional pressure that manifests as career-oriented motivation. We propose that practical integration should promote altruistic and humanitarian values–centric participant orientation to the volunteering process, which is associated with enhanced recruitment, preservation of empathy, and additional positive volunteering outcomes of interest.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Can the mental and physical health of medical students during periods of crisis be improved through volunteering, and if so, what participant or activity characteristics mediate positive outcomes? Volunteerism is a broadly accessible activity that can improve the mental and physical health of participants [1]. A longitudinal study found that individuals who regularly engaged in volunteering reported high levels of mental well-being [2]. A study of adults greater than 50 years old found that volunteering reduced mortality and improved psychosocial outcomes [3]. Volunteering also increases resilience and empathy [1, 4,5,6,7,8]. These outcomes have led some groups to propose volunteer engagement as a tool to improve overall health and well-being [2, 3, 9].
Despite the generalized benefit of volunteering, motivations for volunteering may differ between individuals due to the complex interplay of socioeconomic, cultural, and biographic factors, among other influences. Motivations of medical service volunteers may be distributed across a variety of personal values [10]. Demographic characteristics including the age of medical volunteers have been found to mediate motivation-dependent volunteering outcomes, including satisfaction and emotional exhaustion [11]. Understanding the motivations of volunteers appears necessary to provide specific insight into participant outcomes.
Medical students stand to benefit from volunteering. They report high levels of fatigue, stress, exhaustion, and burnout [12, 13]. These factors correlate with poor academic performance, and stress among medical students has been found to be higher in students who do not engage in extracurricular activities [12]. A significant decline in empathy in medical students over the 3rd year, specifically in students who do not volunteer, has also been observed. Initiating reflective interventions combats the erosion of empathy in these students [14,15,16,17].
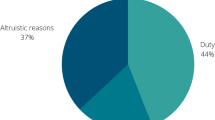
During the onset of the COVID-19 pandemic in the USA in early 2020, medical student groups and faculty at medical institutions nationwide generated volunteering initiatives for medical students to address the critical needs of clinics and communities [18, 19]. For example, students connected with patients or older adults over the phone to help alleviate the effects of social isolation imposed by lockdowns [20,21,22,23,24]. Students engaged in these activities reported high values–based motivations for participation [20]. Students with high prosocial motivation were found to be more likely to volunteer both prior to and during the COVID-19 pandemic [25, 26]. Medical student volunteers during the COVID-19 pandemic report positive outcomes including increased perception of teamwork, communication, and empathy [21]. Medical students experienced common shared obstacles, including tension between personal safety and professional duty (38%), and were often concerned about COVID’s impacts on society (44%) [34]. Prosocial motivation may be a component of student volunteering; student volunteers may be more engaged with their local communities than students who do not volunteer [35]. The choice to volunteer as a medical provider during a crisis may also be due to an individual’s altruistic tendencies, in addition to the desire to impact local spaces [36]. Notably, institutions including the Association of American Medical Colleges emphasize community outreach and volunteerism, promoting these behaviors in medical student populations [37, 38].
Despite the observation that volunteering motivations influence volunteering outcomes, the relationship between specific motivation and volunteering outcomes has yet to be addressed in medical student populations.
The characterization of medical student volunteering motivations and outcomes would provide valuable insight into the differential impact of volunteering on medical student volunteers, providing a roadmap toward effectively integrating volunteerism into the lives of medical students with an intention of combating burnout and preserving empathy. The goal of this study is twofold: (1) to investigate the motivations behind medical student volunteering and (2) to explore the effect of volunteering on medical student well-being during the COVID-19 pandemic.
Materials and Method
IRB Approval
This study was approved and granted a notice of exemption on August 5th, 2020, by the Institutional Review Board at Stony Brook University (IRB# 2020–00,498).
Study Tool
The survey tool consists of three parts. First, we collected general information about the participant and volunteer activities, including volunteering location, volunteering activity, hours volunteered, medical student class year, and prior volunteering experience. Second, we assessed motivations to volunteer with the Volunteer Functions Inventory (VFI), a 30-item validated measurement tool that employs a 7-point Likert scale. Six personal and social functions describe an individual’s motivations to volunteer, which are as follows: protective, values, career, social, understanding, and enhancement motives [27]. Third, we assessed volunteering impact by yes/no binary items on whether volunteering during the COVID-19 epidemic affected physical, psychosocial, or emotional outcomes (PSEOs) [27].
Data Collection
We anonymously surveyed medical students across all class years using the online Qualtrics platform; data were collected over 1 month from August to September 2020. This student cohort included Medical Scientist Training Program (MD/PhD) students. Participants provided informed consent for participation in the study prior to taking the survey. The survey was distributed to a total of 473 students, and 94 students gave at least partial responses (20%). Of these, the 53 complete survey responses from students who had volunteered were used for analysis. The other responses were incomplete.
Data Analysis
Descriptive statistics were used to detail features of our study population and PSEOs of volunteering. We conducted Fisher’s exact tests to assess potential associations between categorical variables and PSEOs of interest (more empathic, more compassionate, better able to deal with disappointment and loss, happier, more resilient, less anxious, and better able to deal with the COVID-19 pandemic). We conducted repeated-measures analysis of variance (ANOVA) followed by Tukey post hoc tests to determine if there were differences in respondents’ VFI subscales and volunteering activity selection. T tests were used to study relationships between VFI subscales and (a) whether volunteering activity involved patient contact, or (b) selected PSEOs. We performed a Spearman’s rho to test the association between VFI subscales and physical improvement (physically healthier, more energetic, better sleep), psychosocial improvement (more empathic, more compassionate, increased purpose, improved relationships), and emotional improvement (better able to deal with disappointment and loss, emotionally healthier, happier, more resilient, more in control, less anxious). The minimum criterion for significance was set at p < 0.05. Statistical analysis was performed using SPSS 27.0 statistical software (IBM Corporation).
Results
Demographics
The study population is a representative cross section of medical student class years at an academic medical center on the east coast. Responses were well distributed across the pre-clerkship/early clinical or clerkship/advanced clinical education stages, the location of volunteering activities, the types of activities respondents engaged in, the time respondents spent volunteering, and the number of volunteering activities individual respondents participated in (Table 1). No statistically significant relationship was observed between the class year of volunteers, the type of volunteering activity, nor the number of hours they volunteered. Most students volunteered for fewer than 100 h; notably, three students volunteered for more than 200 h. Eighty percent of student volunteers had prior volunteering experience, but we did not observe statistically significant differences in either VFI motivations or in the number of hours volunteered between students who had or had not volunteered previously.
Medical Student Volunteer Motivations and Volunteer Activity
Student volunteer motivations, as measured by the VFI, were found to hold statistically significant relationships with the choice of volunteer activities [27]. Volunteer scores on the VFI Career and Understanding subscales were statistically significantly higher in students who selected to be involved in remote volunteering activities over those who participated in in-person volunteering activities (Fig. 1). A statistically significant relationship was also observed between the VFI Career subscale and whether or not students participated in one or more research, patient care, or community support/outreach activities (Fig. 2), but no relationships existed between the other VFI subscales and these variables. Of the five VFI subscales, medical students who volunteered, irrespective of volunteering location, scored highest on the VFI Values subscale, suggesting that students who volunteer are strongly motivated by humanitarian and altruistic values.
Volunteering motivations influence selection of volunteering activity location. ANOVA and post hoc analyses were conducted to explore whether VFI subscale scores impacted the location of volunteering activities selected by medical students. ANOVA (Career): F(2,45) = 3.885, p = 0.028. Tukey HSD: remote v. in-person, p = 0.021. ANOVA (Understanding): F(2,45) = 4.010, p = 0.025. Tukey HSD: remote v. in person, p = 0.019. Significance was calculated at p < 0.05. No other comparisons yielded statistically significant relationships. Data is represented by the mean value for each category plus or minus one standard deviation
Participants with high career motivation select research-oriented volunteering activities. The relationship between VFI Career motivation scores and the types of volunteering activities selected by volunteers was studied using ANOVA and post hoc analyses. ANOVA: F(3,43) = 5.657, p = 0.002. Tukey HSD: research versus patient care, p = 0.039. Tukey HSD: research versus community support/outreach, p = 0.007. Tukey HSD: more than one versus community support/outreach, p = 0.020. Significance was calculated at * = p < 0.05 and ** = p < 0.01. Data is represented by the mean value for each category plus or minus one standard deviation
Volunteering motivations were found to influence selection of activities with patient contact. Classification of whether or not a volunteering activity contained patient contact was independent of whether it was in-person or remote; it was possible to engage in remote activities with patient contact as well as in-person activities without patient contact. Participants who selected activities with patient contact had statistically significantly higher scores on the VFI Values and Understanding subscales (Fig. 3).
Volunteering motivations influence selection of volunteering activities with patient contact. The relationship between VFI subscale scores and whether or not participants selected a volunteering activity with patient contact was studied using independent-samples t tests. VFI values (t(45) = 2.101, p = 0.44) and VFI understanding: (t(45) = 3.048, p = 0.007). Significance was calculated at * = p < 0.05, two-sided. Data is represented by the mean value for each category plus or minus one standard deviation
Medical Student Volunteer Motivation and Physical, Psychosocial, and Emotional Outcomes
Student volunteering motivations were statistically and positively correlated with physical, psychosocial, and emotional improvement, as assessed by Spearman’s rank-order correlations (Table 2). The only VFI subscale that was found to hold no statistically significant relationships to these was the Career subscale.
The relationships between VFI subscales and the individual PSEOs more empathetic, more compassionate, more resilient, more happy, less anxious, better able to deal with disappointment and loss, and better able to handle the COVID-19 pandemic were studied. The VFI Values subscale was significantly and positively associated with an increase in empathy (t(46) = 2.764, p = 0.008), resilience (t(46) = 5.545, p = 0.000), ability to deal with disappointment and loss (t(46) = 3.454, p = 0.001), and ability to cope with the COVID-19 pandemic (t(46) = 2.333, p = 0.024). No statistically significant relationship existed between the Career subscale and any PSEO. Most PSEOs were significantly associated with multiple VFI subscales, suggesting multifactorial influences (Table 2).
Volunteering and Physical, Psychosocial, and Emotional Outcomes
Students who volunteered stated that they felt less anxious (n = 29, 57%), more empathetic (n = 32, 63%), more resilient (n = 35, 67%), more compassionate (n = 41, 80%), better able to cope with the COVID-19 epidemic in NYS (n = 41, 80%), happier (n = 38, 75%), emotionally healthier (n = 39, 77%), and had more purpose (n = 45, 88%). Fewer volunteers reported volunteering improved their physical health (n = 14, 28%), sleep (n = 18, 35%), or ability to deal with disappointment and loss (n = 19, 37%). There was a significant relationship between the PSEO deal with disappointment and loss and class year (Fisher’s exact test, p = 0.010). MS1 (n = 11, 61%) and MSTP GS (n = 3, 60%) students reported that volunteering improved their ability to deal with disappointment and loss, while fewer MS2 (n = 2, 29%), MS3 (n = 1, 7%), and MS4 (n = 2, 33%) students reported a positive effect. Chi-square contributions indicate that the difference is driven largely by MS1 students reporting a greater, and MS3 students reporting a lesser, ability to deal with disappointment and loss than expected. No other statistically significant relationships were observed between PSEOs and class year, nor the number of hours volunteered and PSEOs. However, volunteers who participated in activities with patient contact reported that volunteering made them feel more resilient (p = 0.030, Fisher’s exact test) and more empathetic (p = 0.012, Fisher’s exact test).
The relationship between PSEOs and completion of the clinical clerkship year was examined. MS3 and MS4 students had completed these clerkships (clerkship/advanced clinical), while the MS2 class had begun just over 2 months prior to lockdowns and were included with MS1 and MSTP GS students (pre-clerkship/early clinical). No statistically significant relationships were observed between these groups and the following tested PSEOs: dealing with disappointment and loss, empathy, and compassion.
Discussion
Relationship Between Motivation and PSEOs
Our data indicate that a volunteer’s motivations can enhance or mute the beneficial outcomes of volunteering. Dwyer et al. found that volunteers’ motives could affect satisfaction and contribution to volunteer activities; specifically, VFI values, or the values-centric meaningfulness of the work to the volunteers, were associated with greater volunteer satisfaction [28]. VFI Values scores were positively and significantly associated with increased empathy, resilience, ability to deal with disappointment and loss, and ability to cope with the COVID-19 pandemic. A values-centric participant orientation appears predictive of diverse positive volunteering outcomes. PSEOs were associated with multiple VFI subscales, suggesting that PSEOs are multifactorial with respect to volunteer motivation.
Expressing Altruistic and Humanitarian Values Through Patient Care
Medical student volunteers who are highly motivated to volunteer due to altruistic and humanitarian values (VFI Values) or the desire to gain knowledge, skills, and abilities (VFI Understanding) were more likely to select volunteering activities with patient contact. A systematic review noted that the VFI subscales with the highest scores among volunteers in healthcare settings were VFI Values and Enhancement [29]. A values-centric orientation may be common among medical students who volunteer with patients. Participation in patient contact activity was associated with increased resilience and empathy; these may be desirable outcomes to promote in medical student populations. Clary et al. note that recruitment appeals are most effective when matched with the internal state of volunteers, and Kpanake et al. conclude that broad values-based motivational messaging would be the best way to attract medical volunteers in epidemic response [10, 27]. Orientation of medical students to values-centric motivations may increase participation in patient contact activities, and increase empathy and resilience.
Career-Oriented Motivation
Students who participated in research had higher VFI Career scores than those who participated in community support and outreach or patient care. Similarly, students who participated in remote activities had higher VFI Career scores than those who volunteered in-person or both in-person and remotely. Notably, during the study period, many research activities occurred remotely following COVID-19 restrictions. Thus, high VFI Career scores amongst remote volunteers could be influenced by students who performed research due to “motivation to enhance knowledge in a specific area related to professional and academic development.” [27]. Students motivated to volunteer in order to enhance their career prospects may believe that research achieves this end more so than other experiences. Although it is possible that engagement in a particular activity influenced how a student later perceived their motivations (as measured by the retrospective study tool), these data suggest that a student’s career-oriented motivation influenced their selection of both research-oriented and remote volunteering activities.
Positive Impact on Student Volunteers
Students reported heightened self-perception of empathy, compassion, resilience, and ability to cope with COVID-19 following volunteering. Students also reported that volunteering made them feel happier and emotionally healthier. These results correspond with prior observations that volunteering has a positive impact on the subjective experience of medical students, even under the conditions of stress, uncertainty, and social isolation of the COVID-19 pandemic [26]. Few volunteers reported that volunteering made them feel physically healthier or sleep better. These observations may indicate an inflection point at which the experience of medical student volunteers was affected particularly strongly by the COVID-19 pandemic. For example, it is probable that the perceived health risk of volunteering during a pandemic may have decreased a volunteer’s self-reported physical well-being.
Preserving Student Empathy
We observed no association between students’ educational stage and whether volunteering made them feel more compassionate, empathetic, or resilient. While we measured a change in empathy rather than an absolute value, this result is particularly encouraging given statistically significant declines on empathy scales have been noted for both MD and DO students [14, 15]. Volunteers in diverse contexts have been found to score significantly higher on Empathy Quotient (a 60-question assessment) compared to non-volunteers, and many experienced empathetic concern toward those they were trying to help [7, 8]. Furthermore, Beck et al. examined the impact of service learning on medical students, and found that first-year medical students who volunteered felt that this experience was career reinforcing and allowed them to better understand patient care; the authors believed this experience played a role in developing their professional identities and empathy [30]. Our data indicates that volunteering may increase empathy, compassion, and resilience in students, regardless of educational stage. Volunteering could play a role in preserving empathy amongst students as they move through medical training. We observed that a higher percentage of volunteers who engaged in patient contact reported an increase in empathy, suggesting that the type of volunteer activity might be important in fostering and maintaining empathy amongst medical students. Indeed, Modi et al. report that students who had not volunteered in a student-run free clinic showed a decline in empathy over the course of medical school, while students who had volunteered, even if they had volunteered at the clinic only once, did not show a significant decline [16].
Little Improvement in Dealing with Disappointment and Loss
Only 19 (37%) volunteers felt that volunteering helped them deal with disappointment and loss. It is possible that potential positive effects of volunteering were not enough to overcome the broad array of difficult situations that faced students during this worldwide health crisis. This effect was stratified by year, with MS1s and MSTP GS students reporting a greater ability to deal with disappointment and loss after volunteering than MS2, MS3, and MS4 students. The MS2, MS3, and MS4 class years had participated in clinical clerkships, even if, for the MS2 class, it had been for just over 2 months. This exposure may have connected these students to the experiences of hospital staff more strongly than class years who had not spent significant time in these environments. The effect of specific factors must also be registered; for example, the MS3 class had a particularly low response rate. These students faced unprecedented uncertainty around STEP exam scheduling, the cancelation of away rotations, and how this might affect upcoming residency applications, interviews, and the MATCH.
One limitation of the study is methodological, as self-report items were used to measure PSEOs. Future studies building on these findings should incorporate the use of validated tools (e.g., the Jefferson Scale of Empathy to measure empathy, a volunteering outcome) to further interrogate the association between motivation and volunteer outcomes [31]. Clinical correlates may also be appropriate outcome measures; Jiang et al. found that short-term volunteering did not lead to changes in psychosocial health, with no association found between volunteering and depressive symptoms in older adults [32]. In addition, we note that surveying medical students from a single institution may not be representative of a broader population, that students self-selected to volunteer and complete the survey, and that our survey had a low response rate. Future study could also integrate open-ended questions to assess trends not sufficiently captured by binary or scale-based survey questions.
In conclusion, volunteerism represents an accessible mechanism through which to improve the general well-being of medical students, a group that reports high stress, burnout, and other poor psychosocial, emotional, and physical outcomes. Integrating positive volunteer service into the lives of medical students may contribute to the preservation of empathy. The integration of targeted empathy preservation initiatives has previously been shown to be effective in 3rd year medical student populations [17]. The difficulty of matching into a residency program of a medical specialty of choice is well-appreciated by medical students, and volunteering experience is an important feature of many applications. Over half of U.S. medical residency program directors across all programs cite volunteering experience as an important factor when selecting applicants to interview, which is more than those citing consistency of applicant grades [33]. It is reasonable to conclude that the high career-oriented motivation of students in this study may be influenced by the drive to successfully match. These students opted to engage at significantly high rates in research-oriented activities, and high career motivation was not associated with statistically significant positive outcomes. These observations suggest that minimizing the influence of the competitive environment, or promoting the influence of other motivating factors, may produce more positive outcomes for medical student volunteers. Broad altruistic and humanitarian values–based orientation schema may be effective tools to promote volunteering frameworks associated with positive and protective outcomes, specifically student compassion, resilience, and empathy. Future work may build on this hypothesis to demonstrate the effect of motivational orientation of medical student volunteers prior to engaging in volunteering activities. If such a mechanism holds, it would represent a valuable tool with which to enhance medical student well-being.
Availability of Data and Material
The datasets generated during and/or analyzed during this study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Wilson J, Musick M. The effects of volunteering on the volunteer. Law Contemp Probl. 1999;62(4):141. https://doi.org/10.2307/1192270.
Tabassum F, Mohan J, Smith P. Association of volunteering with mental well-being: a lifecourse analysis of a national population-based longitudinal study in the UK. BMJ Open. 2016;6(8):e011327. https://doi.org/10.1136/bmjopen-2016-011327.
Kim ES, Whillans AV, Lee MT, Chen Y, VanderWeele TJ. Volunteering and subsequent health and well-being in older adults: an outcome-wide longitudinal approach. Am J Prev Med. 2020;59(2):176–86. https://doi.org/10.1016/j.amepre.2020.03.004.
Schwartz CE, Sendor RM. Helping others helps oneself: response shift effects in peer support. Soc Sci Med. 1999;48(11):1563–75. https://doi.org/10.1016/s0277-9536(99)00049-0.
Moll J, Krueger F, Zahn R, Pardini M, de Oliveira-Souza R, Grafman J. Human fronto-mesolimbic networks guide decisions about charitable donation. Proc Natl Acad Sci. 2006;103(42):15623–8. https://doi.org/10.1073/pnas.0604475103.
Park SQ, Kahnt T, Dogan A, Strang S, Fehr E, Tobler PN. A neural link between generosity and happiness. Nat Commun. 2017;8(1):15964. https://doi.org/10.1038/ncomms15964.
Milanovic M. Effects of volunteerism and relationship status on empathy. SURG J. 2012;6(1):5–13. https://doi.org/10.21083/surg.v6i1.198.
Stolinski AM, Ryan CS, Hausmann LRM, Wernli MA. Empathy, guilt, volunteer experiences, and intentions to continue volunteering among buddy volunteers in an AIDS organization. J Appl Biobehav Res. 2007;9(1):1–22. https://doi.org/10.1111/j.1751-9861.2004.tb00089.x.
Post SG. Altruism, happiness, and health: it’s good to be good. Int J Behav Med. 2005;12(2):66–77. https://doi.org/10.1207/s15327558ijbm1202_4.
Kpanake L, Dounamou T, Sorum PC, Mullet E. What motivates individuals to volunteer in Ebola epidemic response? A structural approach in Guinea. Hum Resour Health. 2019;17(1):81. https://doi.org/10.1186/s12960-019-0409-x.
Aranda M, Zappalà S, Topa G. Motivations for volunteerism, satisfaction, and emotional exhaustion: the moderating effect of volunteers’ age. Sustainability. 2019;11(16):4477. https://doi.org/10.3390/su11164477.
Shadid A, Shadid AM, Shadid A, Almutairi FE, Almotairi KE, Aldarwish T, Alzamil O, Alkholaiwi F, Khan SU. Stress, burnout, and associated risk factors in medical students. Cureus. 2020;12(1). https://doi.org/10.7759/cureus.6633.
Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–51. https://doi.org/10.1097/ACM.0000000000000134.
Hojat M, Mangione S, Nasca TJ, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004;38(9):934–41. https://doi.org/10.1111/j.1365-2929.2004.01911.x.
Brown RS. Do students lose empathy in medical school? Pharos. 2017;23.
Modi A, Fascelli M, Daitch Z, Hojat M. Evaluating the relationship between participation in student-run free clinics and changes in empathy in medical students. J Prim Care Community Health. 2017;8(3):122–6. https://doi.org/10.1177/2150131916685199.
Imperato A, Strano-Paul L. Impact of reflection on empathy and emotional intelligence in third-year medical students. Acad Psychiatry. 2021;45:350–3. https://doi.org/10.1007/s40596-020-01371-1.
Rupley D, Grilo SA, Kondragunta S, et al. Mobilization of health professions students during the COVID-19 pandemic. Semin Perinatol. 2020;44(7): 151276. https://doi.org/10.1016/j.semperi.2020.151276.
Soled D, Goel S, Barry D, et al. Medical student mobilization during a crisis: lessons from a COVID-19 medical student response team. Acad Med. 2020;95(9):1384–7. https://doi.org/10.1097/ACM.0000000000003401.
McDonnell EP, Berger RS, Corbett CR, Coppola KM, Brodt‐Ciner ZN. Medical students’ motivations to help older adults during the COVID‐19 pandemic. J Am Geriatr Soc. Published online 5 Mar 2021:jgs.17077. https://doi.org/10.1111/jgs.17077.
Lewis SM, Strano-Paul LA. A COVID Service-learning initiative: emotional support calls for the geriatric population. J Am Geriatr Soc. 2021;69(2):E4-5. https://doi.org/10.1111/jgs.17003.
Office EE, Rodenstein MS, Merchant TS, Pendergrast TR, Lindquist LA. Reducing social isolation of seniors during COVID-19 through medical student telephone contact. J Am Med Dir Assoc. 2020;21(7):948–50. https://doi.org/10.1016/j.jamda.2020.06.003.
van Dyck LI, Wilkins KM, Ouellet J, Ouellet GM, Conroy ML. Combating heightened social isolation of nursing home elders: the telephone outreach in the COVID-19 outbreak program. Am J Geriatr Psychiatry. 2020;28(9):989–92. https://doi.org/10.1016/j.jagp.2020.05.026.
Ayoub P, Chang DD, Hussein N, et al. Medical student mobilization during a pandemic: the Ochsner clinical school response to COVID-19. TOJ. 2020;20(2):146–50. https://doi.org/10.31486/toj.20.0069.
Carlo G, Okun MA, Knight GP, de Guzman MRT. The interplay of traits and motives on volunteering: agreeableness, extraversion and prosocial value motivation. Personality Individ Differ. 2005;38(6):1293–305. https://doi.org/10.1016/j.paid.2004.08.012.
Shi Y, Zhang S, Fan L, Sun T. What motivates medical students to engage in volunteer behavior during the COVID-19 outbreak? A large cross-sectional survey Front Psychol. 2021;11: 569765. https://doi.org/10.3389/fpsyg.2020.569765.
Clary EG, Snyder M, Ridge RD, et al. Understanding and assessing the motivations of volunteers: a functional approach. J Pers Soc Psychol. 1998;74(6):1516–30. https://doi.org/10.1037//0022-3514.74.6.1516.
Dwyer PC, Bono JE, Snyder M, Nov O, Berson Y. Sources of volunteer motivation: transformational leadership and personal motives influence volunteer outcomes: sources of volunteer motivation. Nonprofit Manag Leadersh. 2013;24(2):181–205. https://doi.org/10.1002/nml.21084.
Chacón F, Gutiérrez G, Sauto V. Volunteer functions inventory: a systematic review. Psicothema. 2017;29.3:306–16. https://doi.org/10.7334/psicothema2016.371.
Beck J, Chretien K, Kind T. Professional identity development through service learning: a qualitative study of first-year medical students volunteering at a medical specialty camp. Clin Pediatr (Phila). 2015;54(13):1276–82. https://doi.org/10.1177/0009922815571108.
Hojat M, Mangione S, Nasca TJ, et al. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educ Psychol Measur. 2001;61(2):349–65. https://doi.org/10.1177/00131640121971158.
Jiang D, Warner LM, Chong AM-L, Li T, Wolff JK, Chou K-L. Benefits of volunteering on psychological well-being in older adulthood: evidence from a randomized controlled trial. Aging Mental Health. 2021;25(4):641–9. https://doi.org/10.1080/13607863.2020.1711862.
Results of the 2020 NRMP program director survey. National Resident Matching Program Data Release and Research Committee. 2020. https://mk0nrmp3oyqui6wqfm.kinstacdn.com/wp-content/uploads/2020/08/2020-PD-Survey.pdf. Accessed 28 Apr 2020.
Alkureishi ML, Jaishankar D, Dave S, Tatineni S, Zhu M, Chretien KC, Woodruff JN, Pincavage A, Lee WW. Medical student well-being being research consortium. Impact of the early phase of the COVID-19 pandemic on medical student well-being: a multisite survey. J Gen Intern Med. 2022;37(9):2156–64. https://doi.org/10.1007/s11606-022-07497-2.
Adel FW, Berggren RE, Esterl RM Jr, Ratelle JT. Student-run free clinic volunteers: who they are and what we can learn from them. BMC Med Educ. 2021;21(1):356. https://doi.org/10.1186/s12909-021-02793-7.
Bailey H, Kaplan LJ. Volunteerism during humanitarian crises: a practical guide. Crit Care. 2022;26(1):111. https://doi.org/10.1186/s13054-022-03984-4.
Alberti PM, Sutton KM, Cooper LA, Lane WG, Stephens S, Gourdine MA. Communities, social justice, and academic health centers. Acad Med. 2018;93(1):20–4. https://doi.org/10.1097/ACM.0000000000001678.
The Association of American Medical Colleges. Collaborative student volunteer and service projects. AAMC Resour Libr. 2022. https://www.aamc.org/resource-library/collaborative-student-volunteer-and-service-projects.
Acknowledgements
The authors would like to formally acknowledge the contributions of Dr. Wei-Hsin Lu of Renaissance School of Medicine at Stony Brook University. We thank her for providing guidance and expert insight during all aspects of this research project.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Hannah Phillips, Mansi Chandra, Victoria Ende, Sarah Grosser, Ian Outhwaite, and Rebecca Jennings. Data analysis was performed by Rebecca Jennings. The first draft of the manuscript was contributed to by all authors, and written and revised in significant part by Rebecca Jennings, Hannah Phillips, and Ian Outhwaite. All authors commented on previous versions of the manuscript, and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The Institutional Review Board at Stony Brook University reviewed and approved this study (IRB# 202–00498, initial approval on 8/5/2020).
Consent to Participate
Informed consent was obtained from all participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Phillips, H.E., Jennings, R.B., Outhwaite, I.R. et al. Motivation to Impact: Medical Student Volunteerism in the COVID 19 Pandemic. Med.Sci.Educ. 32, 1149–1157 (2022). https://doi.org/10.1007/s40670-022-01639-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-022-01639-1