Abstract
Introduction
Developmental theories recognize that there is a progression of competence over time. However, despite growing interest in the developmental trajectories of medical students, little research exists that longitudinally documents their gains across domains. Our goal was to track students’ perceived competence over time and to identify different patterns across competencies.
Method
At the end of each of their four academic years, four successive cohorts of Harvard Medical School (HMS) students were surveyed to indicate how much they had learned in each of 28 areas. Nineteen items mapped onto the six competency areas defined by the Accreditation Council for Graduate Medical Education (ACGME) and competency cluster scores were calculated for each.
Results
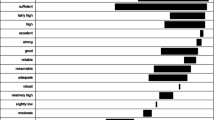
Medical knowledge, patient care, and systems-based practice increased significantly each year from the prior year’s baseline, with the other competencies demonstrating less consistent patterns of growth. At the end of year 1, interpersonal skills, problem-based learning and improvement, and professionalism were rated highest. By the end of year 4, interpersonal skills remained the most highly rated, and systems-based practice, which grew considerably from years 1 to 4, was still rated lowest.
Conclusions
Medical education results in a progressive trajectory of overall competence, with increases, some small and some large, found for every domain for every year. However, the six domains start from differing baselines and progress at different rates over students’ undergraduate careers.

Similar content being viewed by others
References
Lowry BN, Vansaghi LM, Rigler SK, Stites SW. Applying the milestones in an internal medicine residency program curriculum: a foundation for outcome-based learner assessment under the next accreditation system. Acad Med. 2013;88:1665–9.
AAgaard E, Kane GC, Conforti L, Hood S, Caverzagie KJ, Smith C, et al. Early feedback on the use of the internal medicine milestones in assessment of resident performance. J Grad Med Educ. 2013;5:433–8.
Lurie SJ. History and practice of competency-based assessment. Med Educ. 2012;46:49–57.
Carraccio CL, Englander R. From Flexner to competencies: reflections on a decade and the journey ahead. Acad Med. 2013;88:1067–73.
Ten Cate O, Billett S. Competency-based medical education: origins, perspectives and potentialities. Med Educ. 2014;48:325–32.
Hauer KE, Kohlwes K, Cornett P, Hollander H, Ten Cate O, Ranji SR, et al. Identifying entrustable professional activities in internal medicine training. J Grad Med Educ. 2013;5:54–9.
Teherani A, Chen HC. The next steps in competency-based medical education: milestones, entrustable professional activities and observable practice activities. J Gen Intern Med. 2014;29:1090–2.
van Loon KA, Driessen EW, Teunissen PW, Scheele F. Experiences with EPAs, potential benefits and pitfalls. Med Teach. 2014;36:698–702.
Handfield-Jones R, Mann K, Challis M, Hobma S, Klass D, McManus I, et al. Linking assessment to learning: a new route to quality assurance in medical practice. Med Educ. 2002;36:949–56.
Newton BW, Barber L, Clardy J, Cleveland E, O’Sullivan P. Is there hardening of the heart during medical school? Acad Med. 2008;83:244–9.
Krupat E, Pelletier S, Alexander EK, Hirsh D, Ogur B, Schwartzstein R. Can changes in the principal clinical year prevent the erosion of students’ patient-centered beliefs? Acad Med. 2009;84:582–6.
Freeman A, Van der Vleuten C, Nouns Z, Ricketts C. Progress testing internationally. Med Teach. 2010;32:451–5.
Schuwirth LW, van der Vleuten CP. The use of progress testing. Perspect Med Educ. 2012;1:24–30.
Makoul G, Winter RJ. The student perception survey: a tool for assessing medical school curricula. Acad Med. 1997;72:410–1.
Makoul G, Curry RH, Thompson JA. Gauging the outcomes of change in a new medical curriculum: students’ perceptions of progress toward educational goals. Acad Med. 2000;75:S102–5.
Accreditation Council on General Medical Education. Core competencies definitions. http://www.gahec.org/CME/Liasions/0%29ACGME%20Core%20Competencies%20Definitions.htm. Accessed 2 Sept 2015.
Teunissen PW, Stapel DA, Scheele F, Scherpbier AJ, Boor K, van Diemen-Steenvoorde JA, et al. The influence of context on residents’ evaluations: effects of priming on clinical judgment and affect. Adv Health Sci Educ Theory Pract. 2009;14:23–41.
Yeates P, Cardell J, Byrne G, Eva KW. Relatively speaking: contrast effects influence assessors’ scores and narrative feedback. Med Educ. 2015;49:909–19.
Ma HK, Min C, Neville A, Eva K. How good is good? Students and assessors’ perceptions of qualitative markers of performance. Teach Learn Med. 2013;25:15–23.
Tweed M, Thompson-Fawcett M, Wilkinson T. Decision-making bias in assessment: the effect of aggregating objective information and anecdote. Med Teach. 2013;35:832–7.
Blanch-Hartigan D. Medical students’ self-assessment of performance: results from three meta-analyses. Patient Educ Couns. 2011;84:3–9.
Groves RM, Peytcheva E. The impact of nonresponse rates on nonresponse bias: a meta-analysis. Public Opin Q. 2008;72:167–89.
Davern M. Nonresponse rates are a problematic indicator of nonresponse bias in survey research. Health Serv Res. 2013;48:905–12.
Johnson TP, Wislar JS. Response rates and nonresponse errors in surveys. JAMA. 2012;307:1805–6.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krupat, E., Pelletier, S.R. The Development of Medical Student Competence: Tracking Its Trajectory Over Time. Med.Sci.Educ. 26, 61–67 (2016). https://doi.org/10.1007/s40670-015-0190-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-015-0190-y