Abstract
Background
Single-pass batch dialysis (SBD) is a well-established system for treatment of end-stage renal disease. However, little evidence is available on sustained low-efficiency extended dialysis (SLED) performed with SBD in patients with acute kidney injury (AKI) in the intensive care unit (ICU).
Methods
All SLED-SBD sessions conducted on AKI patients in nine ICUs between March and June 2010 were retrospectively analyzed regarding the achieved metabolic and fluid control. Logistic regression was performed to identify the risk factors associated with hypotension and clotting during the sessions.
Results
Data from 106 patients and 421 sessions were analyzed. Patients were 54.2 ± 17.0 years old, 51 % males, and the main AKI cause was sepsis (68 %); 80 % of patients needed mechanical ventilation and 55 % vasoactive drugs. Hospital mortality was 62 %. The median session time was 360 min [interquartile range (IQR) 300–360] and prescribed ultrafiltration was 1500 ml (IQR 800–2000). In 272 sessions (65 %) no complications were recorded. No heparin was used in 269/421 procedures (64 %) and system clotting occurred in 63 sessions (15 %). Risk factors for clotting were sepsis [odds ratio (OR) 2.32 (1.31–4.11), p = 0.004], no anticoagulation [OR 2.94 (1.47–5.91), p = 0.002] and the prescribed time (hours) [OR 1.14 (1.05–1.24), p = 0.001]. Hypotension occurred in 25 % of procedures and no independent risk factors were identified by logistic regression. Adequate metabolic and fluid balance was achieved during SLED sessions. Median blood urea decreased from 107 to 63 mg/dl (p < 0.001), potassium from 4.1 to 3.9 mEq/l (p < 0.001), and increased bicarbonate (from 21.4 to 23.5 mEq/l, p < 0.001). Median fluid balance during session days ranged from +1300 to −20 ml/24 h (p < 0.001).
Conclusions
SLED-SBD was associated with a low incidence of clotting despite frequent use of saline flush, and achieved a satisfactory hemodynamic stability and reasonable metabolic and fluid control in critically-ill AKI patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) affects up to 30 % of intensive care unit (ICU) patients with approximately 5–10 % of them requiring renal replacement therapy (RRT) [1, 2]. The usual RRT methods for treating these patients are continuous renal replacement therapy (CRRT) or intermittent hemodialysis (IHD). Both methods have advantages and disadvantages: CRRT allows hemodynamic stability and great fluid removal but is expensive and time consuming. On the other hand, IHD is cheaper and faster but induces hypotension in 20–30 % of these patients. [3] In the last 10 years, hybrid therapies such as sustained low-efficiency extended dialysis (SLED) have emerged as attractive alternatives, able to provide satisfactory metabolic control at low complication rates and reduced anticoagulation demand [4–7].
Single-pass batch dialysis (SBD), formerly used for end-stage renal disease treatment [5, 8–10], has also been used in AKI patients as SLED therapy due to its characteristics: user friendliness, use of ultrapure dialysate, and no need of water purification on the spot [8–12]. Pilot studies on SLED using SBD (SLED-SBD) in ICU AKI patients [7, 13] found few episodes of hypotension or clotting and adequate urea removal. However, the complications and metabolic control of SBD have not been studied in a large cohort of critically ill patients. Thus, the aim of this study was to evaluate the complications and metabolic control of SLED-SBD in ICU AKI patients.
Methods
We retrospectively analyzed all dialysis sessions performed with SBD in critically ill patients from March to June 2010. All patients were at nine clinical or surgical ICUs, comprising 110 beds of a general university hospital (Central Institute of Hospital das Clínicas, School of Medicine, University of São Paulo, Brazil). The Research Ethics Committee (CAPPesq project number 0485/11) approved the study and waived informed consent, considering the observational nature of the study.
Patients
We included AKI patients aged over 17 years who underwent at least one SLED-SBD. We excluded patients with serious electrolytic disorders who could not receive a standard dialysate, those with a baseline serum creatinine (SCr) ≥ 3.5 mg/dl, and renal transplant recipients. We also excluded patients performing exclusively classical hemodialysis (CHD) or CRRT. All patients with norepinephrine dosage ≥0.2 mcg/kg/min or refractory hypotension precluding SLED procedures performed CRRT.
AKI was diagnosed by an increase in SCr 1.5-fold (≥50 %) or 0.3 mg/dl relative to its reference value, according to the Acute Kidney Injury Network (AKIN) criteria [14]. Reference SCr was considered the value at hospital admission or the minimum value achieved during hospitalization. A reference SCr > 1.5 mg/dl was indicative of previous renal dysfunction.
We collected the following patient data: age, gender, type of ICU (clinical or surgical), etiology of renal injury (sepsis, ischemia, nephrotoxicity, or urinary obstruction), and need for vasoactive drugs and mechanical ventilation during the sessions. For each SLED session the occurrence of complications such as hypotension and/or clotting were analyzed as well as the achieved metabolic and fluid control.
Dialysis procedures
All dialysis procedures in the ICUs were prescribed by the same group of nephrologists. The procedure was initiated by a nephrology-specialized nurse and then handled by ICU nurses.
SLED was performed with a SBD machine (Genius®, Fresenius Medical Care, Bad Homburg, Germany) at a blood flow rate (QA) of 180–300 ml/min using high-flux polysulfone filters (FX 60 or FX 80, Fresenius Medical Care, Bad Homburg, Germany). The dialysate flow was always equal to the QA. In the SBD device, the dialysate is stored in an air-free 90-l glass container (batch system). The standard dialysate compositions were as follows: sodium 138 mEq/l; bicarbonate 35 mEq/l; calcium 2.5 or 3.5 mg/dl; chloride 106 mEq/l; magnesium 1.0 mEq/l; potassium 2 or 3 mEq/l.
We recorded the following characteristics of the procedure: the ICU shift when the procedure started (1st shift from 6:00 AM to 12:00 AM; 2nd: from 12:00 AM to 6:00 PM and 3rd: from 6:00 PM to 6:00 AM), type of anticoagulant (non-fractionated heparin or saline flush), length of the session (prescribed and achieved), QA and ultrafiltration (UF) (prescribed and achieved), the mean arterial pressure at start, and the minimum systolic and diastolic arterial pressure registered during the session. Also, the site of the vascular access (femoral, jugular or subclavian) was recorded. The vascular access was provided via an intravenous catheter with 11.5 F, length 16 or 20 cm, Arrow International (Mahurkar, Covidien, USA) or Eagle Flow (Health Line Corp., Salt Lake city, UT, USA). CHD was defined as hemodialysis procedure up to 4 h and SLED sessions with duration ≥6 h.
Complications
We assessed the complications related to the patients or the procedures. Hypotension was defined as a mean arterial pressure (MAP) less than 65 mmHg or the need to introduce or increase vasoactive drugs during the session. Other serious complications such as arrhythmias, seizures and the introduction of ventilator support were also recorded. Malfunctioning catheter was defined as lines reversion or any reduction of prescribed blood flow during a session. Clotting was defined as the coagulation of lines and/or filters resulting in SLED interruption.
Clinical/laboratory parameters and metabolic control
Urinary volume and fluid balance of each patient on the day before and after each SLED session were assessed. The following ICU routine serum laboratory exams were analyzed at each day of SLED therapy: sodium, lactate, total calcium, phosphate, hemoglobin, platelet count, and standard prothrombin time. These exams are usually collected daily in the early morning as a routine in all ICUs. For each patient, the mean blood urea concentration (arithmetic mean value of daily blood urea measurements during the period under SLED) was calculated. Bicarbonate, potassium and blood urea values on the day when the session started were compared to those values obtained the day after the end of the session. These parameters were used to assess metabolic control.
Statistics
Variables were expressed as median (25th–75th interquartile) for continuous variables and as frequencies and percentage for categorical variables. Comparisons among groups were made with Chi Square test, Mann–Whitney test or Student t test as appropriated. A multiple logistic regression using the backward stepwise method was performed to identify the factors associated with the most frequent complications: hypotension and clotting. The Hosmer–Lemeshow test was employed to evaluate the fit of the model. The results of logistic regression are presented as odds ratio (OR) with lower and upper 95 % confidence interval (CI). Data were analyzed with Program SPSS for Windows, version 18.0 (Chicago, IL, USA). All tests were two-tailed. For all comparisons, p < 0.05 was considered significant.
Results
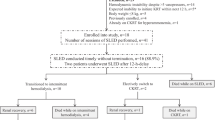
During the study period, 1750 patients were admitted to the ICUs and 257 of these patients underwent RRT during ICU stay. A total of 151 patients performed SBD hemodialysis and we analyzed data from 421 sessions conducted in 106 AKI patients who fulfilled the eligibility criteria. SLED was the initial RRT method for 72 patients (68 %); 48 patients (45 %) underwent only this method. The other 58 (55 %) changed the method during hospitalization: 34 patients (32 %) were transferred from CRRT to SLED; 11 (10 %) were transferred from SLED to CRRT, and 13 (12 %) were transferred from SLED to CHD (Fig. 1).
Flowchart of study population. ICU intensive care unit, RRT renal replacement therapy, CHD classic hemodialysis, SLED slow efficiency extended dialysis, CRRT continuous renal replacement therapy, SBD single-pass batch dialysis, CKD chronic kidney disease, AKI acute kidney injury, SCr serum creatinine
Patients and RRT characteristics
Patients were 54.2 ± 17.0 years old, 49 (51 %) were male; 64 patients (60 %) were in a surgical ICU and the main AKI cause was sepsis in 72 (68 %), ischemia in 47 (44 %) and nephrotoxicity in 14 (13 %). Baseline SCr was 1.11 mg/dl (0.79–1.61) and previous renal dysfunction was present in 37 patients (35 %). During ICU stay, 85 patients (80 %) needed mechanical ventilation, 58 (55 %) received vasoactive drugs, and hospital mortality was 62 % (Table 1).
Each patient underwent 2.0 (1.0–5.0) SLED sessions in 4.0 (1.0–9.0) days of therapy. Median achieved session time was 360 min (300–360); 316 sessions (75.1 %) achieved at least 360 min. Achieved blood/dialysate flow was 250 (200–300) ml/min, prescribed UF was 250 ml/h (160–333). ICU shift distribution of RRT was: 1st shift 190 procedures (45.1 %), 2nd shift 140 (33.2 %), and 3rd shift 84 (20 %). The sites of venous access were jugular in 55 % of the sessions, femoral in 36 % and subclavian in 5 %. Saline flushing was used as anticoagulant in 269 sessions (63.9 %). The most frequent contraindications for heparin use were thrombocytopenia (platelet count below 100,000/mm3) and active bleeding, observed in 176 (39.6 %) and 74 (17.5 %) of the procedures, respectively.
Complications of dialysis sessions
In 272 sessions (65 %), there were no complications. The occurrence of serious complications was extremely rare: in three (0.7 %) sessions, cardiac arrhythmia was observed and only one death was related to procedure (Table 2).
Clotting was observed in 63 sessions (15 %). In 50 of them (82 %), only saline flushing had been used as anticoagulant. Clotting was more frequently observed in patients with sepsis (p = 0.01), in sessions with increased duration [360 (300–360) vs. 330 (260–360) min, p < 0.001] and less frequently observed with the use of heparin (p = 0.001). Malfunctioning catheter was observed in 95 (22.8 %) sessions (inducing the need for QA reduction in 7.8 %), but was not related to clotting (p = 0.12). Sessions with clotting were not associated with prothrombin time (p = 0.13), hemoglobin value (p = 0.23), platelet count (p = 0.19) or vascular access site (p = 0.99). Also, hypotension did not induce more frequent clotting (16 vs. 13 %, p = 0.32). A multiple logistic regression was performed in order to identify the factors associated with clotting. The final model is shown in Table 3.
Hypotension was observed in 103 sessions (25 %). In all but five of these sessions, pre-session MAP was <65 mmHg. Hypotension was associated with higher pre-session levels of lactate (22 [16–32] vs. 18 [13–24] mmol/l, p = 0.01) and lower standard prothrombin time [1.2 (1.0–1.4) vs. 1.3 (1.1–1.5), p = 0.01] as shown in Table 2. Also, hypotension was more frequent in clinical than in surgical ICUs (26 vs. 17 %, p = 0.03). Multiple logistic regressions were performed to identify the factors associated with hypotension. However, a good model was not obtained. There were no differences in rate of complications (p = 0.42 for clotting and p = 0.87 for hypotension) among the three ICU shifts, as shown in Table 2.
We analyzed the subgroup of procedures with an achieved time <6 h. The ultrafiltration per hour obtained was lower in the group <6 h (200 vs. 250 ml/h, p < 0.01), but the incidence of hypotension was similar to that of the group >6 h (29 vs. 23 %, p = 0.16). There were no differences between the groups regarding presence of sepsis (70 vs. 72 %, p = 0.74) or type of ICU (p = 0.57), as shown in Table 4.
Metabolic control/adequacy
The main biochemical blood tests before the SBD sessions were SCr 1.10 (0.79–1.65) mg/dl, urea 107 (77–141) mg/dl, sodium 141 (138–147) mEq/l, potassium 4.3 (3.9–4.9) mEq/l, chloride 107 (103–115) mEq/l, total calcium 4.6 (4.3–5.0) mg/dl, phosphate 5.0 (4.0–6.0) mg/dl, bicarbonate 18.9 (14.9–21.3) mEq/l, lactate 21 (13.0–32.0) mg/dl, platelet count 192 (86–280) × 103/mm3, hemoglobin 8.9 (7.4–10.2) g/dl and international normalized ratio (INR) 1.3 (1.1–1.6).
SBD provided a satisfactory metabolic control. In the period in which patients were under SLED therapy, mean blood urea was 93 (69–115) mg/dl. Blood test parameters were significantly improved after SLED completion: urea from 107 to 63 mg/dl; serum potassium (from 4.1 to 3.9 mEq/l, p < 0.001) and bicarbonate (from 21.4 to 23.5 mEq/l, p < 0.001). Serum phosphorus after the procedure was 3.9 (2.9–4.9) mg/dl. Hypophosphatemia occurred in 100 (23.7 %) procedures.
The prescribed session time was totally achieved in 75 % of procedures and prescribed UF was achieved in 72 % of procedures. The sessions induced a reduction in the fluid balance from 1300 to −20 ml (p < 0.001). Hypotension induced lower achieved UF [250 (166–354) vs. 166 ml/h (0–333), p = 0.001] and increased post-session fluid balance [+305 (−420 to +1274) vs. −158 (−743 to +771) ml/24 h, p = 0.01]. Clotting tended to be associated to lower delivered UF [216 (83–354) vs. 250 ml/h (166–354), p = 0.07], but had no effect on fluid balance (p = 0.18).
Discussion
There is renewed interest in prolonged or extended dialysis modalities for critically ill patients with AKI in the ICU [15]. Advantages of SLED are associated with hemodynamic stability, flexible treatment schedules and reduced costs [4–13, 16]. In the present study, 71 % of all hemodialysis procedures performed in ICUs used SBD. SLED combines the advantages of CRRT and IHD [4, 5, 17], emerging as a suitable bridge when switching from CRRT to IHD, as occurred in 34 patients (32 %) of our study.
Fluid overload is considered to be an important risk factor for mortality, delayed diagnosis of AKI, increased length of ICU and hospital stay, as well as pulmonary and surgical complications in AKI patients [18, 19]. Kielstein et al. [13] demonstrated similar a UF volume per session comparing 20 patients with 11.7 h of SLED therapy vs. 23.3 h of CRRT (2.9 v. 3.2 l, respectively, p = NS). In our study, we obtained a median UF of 1.5 l per 6 h of SLED, suggesting that this RRT method must be considered when fluid removal in critically-ill AKI patients is necessary.
In the ICU, heparin anticoagulation is frequently contraindicated due to its complications and it has been avoided in up to 75 % of patients [20]. In the current study, no anticoagulation was used in 64 % of procedures, and the clotting incidence was 15 %. Clotting was more frequently observed in patients with sepsis. SBD has no drip chambers and blood lines have no contact with air, possibly determining lower thrombogenic activity. Other studies with SBD have used a lower dose of heparin, with similar results. Kielstein et al. [13] employed 500 IU in bolus before continuous infusion, and Schneider et al. [12] prescribed reduced infusion volumes (250 ml/h).
Increased session duration was associated with clotting in some [7, 13, 23] but not all [23] studies. Lonnemann et al. [7] performed 20 sessions of 18 h length, all of the procedures with heparin. Despite a lower dosage, no clotting was observed. Kielstein et al. [13] assessed 20 patients submitted to 12-h SBD sessions, demonstrating no coagulation events, but heparin was used in all procedures. In more power-sized studies, the incidence of clotting was higher. Kumar et al. [22] evaluated 367 treatment-days, 70 % of them with heparin, and incidence of clotting was 22.9 %. Marshall et al. [5] performed 145 treatments of 12 h length with anticoagulation and showed clotting in 20 %.
In dialysis with shorter duration, anticoagulation can be withheld, especially in patients with higher bleeding risk or contraindication to heparin. Berbece et al. [20] studied 165 treatments of 8 h duration, 65 % of them with saline flushing, and showed clotting in 17 % with heparin and in 27 % with saline flushing. Moreover, some studies showed a comparable incidence of clotting in longer treatments. Albino et al. [24] evaluated 195 sessions of 6 or 10 h length, 66 % of them with saline flushing, and observed a low overall incidence of clotting (14.9 %), without difference between the groups (11 vs. 18 %, respectively, p = 0.72).
Anticoagulation with sodium citrate has also been employed in SLED [12, 25]. Morgera et al. [26] studied 21 patients in each arm (citrate vs. heparin) and showed similar filter efficacy by clotting score, but the clotting incidence was not described. Schneider et al. [12] showed that anticoagulation with citrate alone was more effective than with heparin alone (19 vs. 36 %). Clark et al. [27] employed a regional citrate anticoagulation (RCA) protocol in 30 patients, with calcium chloride infused to the patient and adjusted as in a continuous procedure. Filter clotting, early termination of procedure and bleeding were not reported. Furthermore, hypernatremia, alkalosis and excess citrate were not observed, but hypocalcaemia occurred due to higher dialysate flow and calcium-free baths.
Fiaccadori et al. [28] studied 807 sessions in 116 patients, developing an excellent RCA protocol with low-cost citrate formulations (ACD-A), no need to routinely use systemic calcium administration and easier laboratory monitoring to avoid citrate accumulation. The dialysate contained 1.25 mmol/l of calcium, and calcium gluconate 10 % infusion was started at 5 ml/h when serum Ca fell below 0.9 mmol/l. Only 5 % of patients presented major bleeding, intravenous calcium infusions were needed in 3 % of sessions and irreversible clotting occurred in 2 %. No citrate accumulation was observed, and even patients with higher Model For End-Stage Liver Disease (MELD) scores (>25) maintained citrate levels and activated coagulation times similar to those with lower MELD scores [28, 29].
Nevertheless, in patients at high risk of bleeding, RCA was performed in only 18 % of cases [29]. In our country, citrate use has been hampered by expensive costs of citrate solutions and cumbersome control of calcium levels. To date, there is no published experience using citrate in SLED in our country. Table 5 describes the anticoagulation methods used in studies with SLED.
Satisfactory cardiovascular tolerability is reported in several studies assessing SLED in the ICU setting [5, 13, 19, 23]. We observed hypotension in 25 % of patients, mainly those already with lower MAP at the beginning of the session. Furthermore, only 11 patients had to switch from SLED to CRRT. Schwenger et al. [16] performed a randomized clinical trial comparing 115 patients undergoing 14 h of SLED-SBD with 117 patients undergoing 20 h of CRRT. SLED patients had a lower incidence of hypotension, similar to the patients under CRRT (1.5 ± 1.4 vs. 1.8 ± 1.6 episodes per patient, respectively, p = 0.07).
In general, SLED-SBD seems to be a safe procedure. In our study, some complications were observed in 35 % of the sessions but they were minor and reversible. The frequency of severe complications was very low: in three (0.7 %) sessions the patient presented with cardiac arrhythmia and only one death was related to the dialysis procedure. These results are quite similar to those found by other authors. Ponce et al. [32] retrospectively analyzed 1367 SLED sessions (6–8 h) in 231 ICU patients receiving norepinephrine (mean dosage 0.45 ± 0.16 mcg/kg/min), 92 % under mechanical ventilation, mainly due to sepsis (76 %) and observed serious complications (ventricular tachycardia or increase of norepinephrine dosage >1 mcg/kg/min) in 1.4 % of the procedures. Fiaccadori et al. [25] studied 185 sessions (8–10 h) with prostacyclin in 35 patients, 80 % under mechanical ventilation and 62 % with vasoactive drugs, and observed ventricular tachycardia or refractory hypotension in 2 % of sessions.
This study has several limitations. It is a retrospective study of one tertiary center, and the results may not be applicable to other settings. The efficiency of dialysis was not precisely determined and some relevant variables such as illness severity scores were not recorded, precluding more detailed analysis. The dialysate composition was restricted to three standard solutions in our study, which limits an adequate tailoring to the patient. However, we studied a large number of sessions performed in clinical and surgical ICUs, and we assessed the number and type of complications of SLED-SBD, which has not been previously reported. We also were able to identify the factors associated with clotting.
In conclusion, SLED therapy with SBD is a safe method of RRT in AKI ICU patients, with reduced incidence of clotting and an acceptable risk of hemodynamic instability. Good fluid balance control and satisfactory metabolic control can be achieved and SBD is an attractive alternative for ICU patients who are candidates for SLED therapy.
References
Ricci Z, Ronco C (2008) Dose and efficiency of renal replacement therapy: continuous renal replacement therapy versus intermittent hemodialysis versus slow extended daily dialysis. Crit Care Med 36:S229–S237
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C, Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators (2005) Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294:813–818
Murray P, Hall J (2000) Renal replacement therapy for acute renal failure. Am J Respir Crit Care Med 162:777–781
Kielstein JT, Schiffer M, Hafer C (2010) Back to the future: extended hemodialysis for treatment of acute kidney injury in the intensive care unit. J Nephrol 23(5):494–501
Marshall MR, Golper TA, Shaver MJ, Alam MG, Chatoth DK (2001) Sustained low-efficiency dialysis for critically ill patients requiring renal replacement therapy. Kidney Int 60:777–785
Fliser D, Kielstein JT (2004) A single-pass batch dialysis system: and ideal dialysis method for the patient in intensive care with acute renal failure. Curr Opin Crit Care 10:483–488
Lonnemann G, Floege J, Kliem V, Brunkhorst R, Koch KM (2000) Extended daily veno-venous high-flux haemodialysis in patients with acute renal failure and multiple organ dysfunction syndrome using a single path batch dialysis system. Nephrol Dial Transplant 15:1189–1193
Kleophas W, Backus G (2001) A simplified method for adequate hemodialysis. Blood Purif 19:189–194
Kleophas W, Haastert B, Backus G, Hilgers P, Westhoff A, van Endert G (1998) Long-term experience with an ultrapure individual dialysis fluid with a batch type machine. Nephrol Dial Transplant 13:3118–3125
Fassbinder W (2003) Experience with the Genius hemodialysis system. Kidney Blood Pressure Res 26:96–99
Dhondt AW, Vanholder RC, de Smet RV, Claus SA, Waterloos MA, Glorieux GL, Delanghe JR, Lameire NH (2003) Studies on dialysate mixing in the Genius single-pass batch system for hemodialysis therapy. Kidney Int 63:1540–1547
Schneider M, Liefeldt L, Slowinski T, Peters H, Neumayer HH, Morgera S (2008) Citrate anticoagulation protocol for slow extended hemodialysis with the Genius dialysis system in acute renal failure. Int J Artif Organs 31(1):43–48
Kielstein JT, Kretschmer U, Ernst T, Hafer C, Bahr MJ, Haller H, Fliser D (2004) Efficacy and cardiovascular tolerability of extended dialysis in critically ill patients: a randomized controlled study. Am J Kidney Dis 43(2):342–349
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A (2007) Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11:R31
Fliser D, Kielstein JT (2006) Technology insight: treatment of renal failure in the intensive care unit with extended dialysis. Nat Clin Pract Nephrol 2(1):32–39
Schwenger V, Weigand MA, Hoffman O et al (2012) Sustained low efficiency dialysis using a single-pass batch system in acute kidney injury—a randomized interventional trial: the Renal Replacement Therapy Study in Intensive Care Unit Patients. Crit Care 16(4):R140
Kihara M, Ikeda Y, Shibata K, Masumori S, Fujita H, Ebira H, Toya Y, Takagi N, Shionoiri H, Umemura S (1994) Slow hemodialysis performed during the day in managing renal failure in critically ill patients. Nephron 67:36–41
Labib M, Khalid R, Khan A, Khan S (2013) Volume management in the critically ill patient with acute kidney injury. Crit Care Res Pract 2013:792830. doi:10.1155/2013/792830 (Epub 2013 Feb 7)
Thongprayoon C, Cheungpasitporn W, Srivali N, Ungprasert P, Kittanamongkolchai W, Kashani K (2015) The impact of fluid balance on diagnosis, staging and prediction of mortality in critically ill patients with acute kidney injury. J Nephrol. doi:10.1007/s40620-015-0211-3
Berbece AN, Richardson RMA (2006) Sustained low-efficiency dialysis in the ICU: cost, anticoagulation, and solute removal. Kidney Int 70(5):963–968
Chen S, Ma T (2014) Sustained low efficiency daily diafiltration for diabetic nephropathy patients with acute kidney injury. Med Princ Pract 23:119–124
Kumar VA, Craig M, Depner TA, Yeun JY (2000) Extended daily dialysis: a new approach to renal replacement for acute renal failure in the intensive care unit. Am J Kidney Dis 36:294–300
Fieghen HE, Friedrich JO, Burns KE, Nisembaum R, Adhikari NK, Hladunewich MA, Lapinsky SE, Richardson RM, Wald R (2010) The hemodynamic tolerability and feasibility of sustained low efficiency dialysis in the management of critically ill patients with acute kidney injury. BMC Nephrol 11:32. doi:10.1186/1471-2369-11-32
Albino BB, Balbi AL, Ponce D (2014) Dialysis complications in AKI patients treated with extended daliy dialysis: is the duration of therapy important? Biomed Res Int 2014:153626. doi:10.1155/2014/153626 (Epub 2014 Aug 11)
Fiaccadori E, Maggiore U, Parenti E, Giacosa R, Picetti E, Rotelli C, Tagliavini D, Cabassi A (2007) Sustained low-efficiency dialysis (SLED) with prostaciclin in critically ill patients with acute renal failure. Nephrol Dial Transplant 22:529–537
Morgera S, Scholle C, Melzer C, Slowinski T, Liefeld L, Baumann G, Peters H, Neumayer HH (2004) A simple, safe and effective citrate anticoagulation protocol for the Genius dialysis system in acute renal failure. Nephron Clin Pract 98:c35–c40
Clark JA, Schulman G, Golper T (2008) Safety and efficacy of regional citrate anticoagulation during 8-h sustained low-efficiency dialysis. Clin J Am Soc 3:736–742
Fiaccadori E, Regolisti G, Cademartiri C, Cabassi A, Picetti E, Barbagallo M, Gherli T, Castellano G, Morabito S, Maggiore U (2013) Efficacy and safety of a citrate-based protocol for sustained low-efficiency dialysis in AKI using standard dialysis equipment. Clin J Am Soc Nephrol 8:1670–1678
Fiaccadori E, Pistolesi V, Mariano F, Mancini E, Canepari G, Inguaggiato P, Pozzato M, Morabito S (2015) Regional citrate anticoagulation for renal replacement therapies in patients with acute kidney injury: a position statement of work group “Renal Replacement Therapies in Critically Ill Patients” of Italian Society of Nephrology. J Nephrol 28:151–164
Mariano F, Tedeschi L, Morselli M, Stella M, Triolo G (2010) Normal citratemia and metabolic tolerance of citrate anticoagulation for hemodiafiltration in severe septic shock burn patients. Intensive Care Med 36:1735–1743
Sun Z, Ye H, Shen X, Chao H, Wu X, Yang J (2014) Continuous venovenous hemofiltration versus extended daily hemofiltration in patients with septic acute kidney injury: a retrospective cohort study. Crit Care 18(2):R70. doi:10.1186/cc13827
Ponce D, Abrão JMG, Albino BB, Balbi AL (2013) Extended daily dialysis in acute kidney injury patients: metabolic and fluid control and risk factors for death. PLoS One 8(12):e81697. doi:10.1371/journal.pone.0081697 (eCollection 2013)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
This study was performed in accordance with the Declaration of Helsinki and its amendments. Any information connected with the identity of individual subjects was excluded from the study. The Research Ethics Committee of Hospital das Clínicas (CAPPesq project number 0485/11) approved the study.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Caires, R.A., Abdulkader, R.C.R.M., Costa e Silva, V.T. et al. Sustained low-efficiency extended dialysis (SLED) with single-pass batch system in critically-ill patients with acute kidney injury (AKI). J Nephrol 29, 401–409 (2016). https://doi.org/10.1007/s40620-015-0224-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-015-0224-y