Abstract
Purpose
Vitamin D deficiency is related to metabolic disturbances. Indeed, a poor vitamin D status has been usually detected in patients with cardiovascular disease (CVD). However, the relationship between vitamin D and CVD risk factors in young adults remains controversial at present. This study aimed to examine the association between circulating 25-hydroxivitamin D (25(OH)D) and CVD risk factors in young adults.
Methods
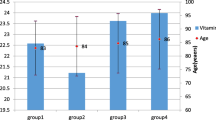
The present cross-sectional study included a cohort of 177 young adults aged 18–25 years old (65% women). 25(OH)D serum concentrations were assessed using a competitive chemiluminescence immunoassay. Fasting CVD risk factors (i.e., body composition, blood pressure, glucose metabolism, lipid profile, liver, and inflammatory markers) were determined by routine methods. A panel of 63 oxylipins and endocannabinoids (eCBs) was also analyzed by targeted metabolomics.
Results
Circulating 25(OH)D concentrations were inversely associated with a wide range of CVD risk factors including anthropometrical (all P ≤ 0.005), body composition (all P ≤ 0.038), glucose metabolism (all P ≤ 0.029), lipid profile (all P < 0.035), liver (all P ≤ 0.011), and pro-inflammatory biomarkers (all P ≤ 0.030). No associations of serum 25(OH)D concentrations were found with pro-inflammatory markers (all P ≥ 0.104), omega-6 and omega-3 oxylipins, nor eCBs concentrations or their analogs (all P ≥ 0.05).
Conclusion
The present findings support the idea that 25(OH)D could be a useful predictor of CVD risk in young individuals.

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding authors on reasonable request.
References
Nitsa A, Toutouza M, Machairas N et al (2018) Vitamin D in cardiovascular disease. Vivo Athens Greece 32:977–981. https://doi.org/10.21873/invivo.11338
Siasos G, Bletsa E, Stampouloglou PK et al (2020) MicroRNAs in cardiovascular disease. Hellenic J Cardiol 61:165–173. https://doi.org/10.1016/j.hjc.2020.03.003
Chooi YC, Ding C, Magkos F (2019) The epidemiology of obesity. Metabolism 92:6–10. https://doi.org/10.1016/j.metabol.2018.09.005
Sunkara A, Raizner A (2019) Supplemental vitamins and minerals for cardiovascular disease prevention and treatment. Methodist DeBakey Cardiovasc J 15:179–184. https://doi.org/10.14797/mdcj-15-3-179
Osuna-Prieto FJ, Martinez-Tellez B, Ortiz-Alvarez L et al (2021) Elevated plasma succinate levels are linked to higher cardiovascular disease risk factors in young adults. Cardiovasc Diabetol 20:151. https://doi.org/10.1186/s12933-021-01333-3
Trejo R, Cross W, Stephenson J, Edward K (2018) Young adults’ knowledge and attitudes towards cardiovascular disease: a systematic review and meta-analysis. J Clin Nurs 27:4245–4256. https://doi.org/10.1111/jocn.14517
Tian X, Chen S, Zuo Y et al (2022) Association of lipid, inflammatory, and metabolic biomarkers with age at onset for incident cardiovascular disease. BMC Med 20:383. https://doi.org/10.1186/s12916-022-02592-x
Latic N, Erben RG (2020) Vitamin D and cardiovascular disease, with emphasis on hypertension, atherosclerosis, and heart failure. Int J Mol Sci 21:6483. https://doi.org/10.3390/ijms21186483
Mozos I, Marginean O (2015) Links between vitamin D deficiency and cardiovascular diseases. BioMed Res Int 2015:109275. https://doi.org/10.1155/2015/109275
García-Bailo B, Jamnik J, Da Costa LA et al (2013) Genetic variation in the vitamin D receptor, plasma 25-hydroxyvitamin D, and biomarkers of cardiometabolic disease in Caucasian young adults. J Nutr Nutr 6:256–267. https://doi.org/10.1159/000354729
Mousa A, Naderpoor N, Teede HJ et al (2015) Vitamin D and cardiometabolic risk factors and diseases. Minerva Endocrinol 40:213–230
Serrano NC, Romero SL, Suárez DP et al (2020) Efficacy of oral Vitamin D supplementation in reducing body mass index and lipid profile in adolescents and young adults in Colombia. Med (Baltim) 99:e21722. https://doi.org/10.1097/MD.0000000000021722
Manson JE, Cook NR, Lee I-M et al (2019) Vitamin D supplements and prevention of cancer and cardiovascular disease. N Engl J Med 380:33–44. https://doi.org/10.1056/NEJMoa1809944
Grant WB, Bhattoa HP, Boucher BJ (2017) Seasonal variations of U.S. mortality rates: roles of solar ultraviolet-B doses, vitamin D, gene expression, and infections. J Steroid Biochem Mol Biol 173:5–12. https://doi.org/10.1016/j.jsbmb.2017.01.003
Grant WB, Boucher BJ (2022) An exploration of how solar radiation affects the seasonal variation of human mortality rates and the seasonal variation in some other common disorders. Nutrients 14:2519. https://doi.org/10.3390/nu14122519
Thompson B, Waterhouse M, English DR et al (2023) Vitamin D supplementation and major cardiovascular events: D-Health randomised controlled trial. BMJ 381:e075230. https://doi.org/10.1136/bmj-2023-075230
Zittermann A, Trummer C, Theiler-Schwetz V et al (2021) Vitamin D and cardiovascular disease: an updated narrative review. Int J Mol Sci 22:2896. https://doi.org/10.3390/ijms22062896
Williams DM, Fraser A, Fraser WD et al (2013) Associations of maternal 25-hydroxyvitamin D in pregnancy with offspring cardiovascular risk factors in childhood and adolescence: findings from the Avon Longitudinal Study of Parents and Children. Heart 99:1849–1856. https://doi.org/10.1136/heartjnl-2013-303678
Boyle VT, Thorstensen EB, Thompson JMD et al (2017) The relationship between maternal 25-hydroxyvitamin D status in pregnancy and childhood adiposity and allergy: an observational study. Int J Obes 41:1755–1760. https://doi.org/10.1038/ijo.2017.182
Tint MT, Chong MF, Aris IM et al (2005) Association between maternal mid-gestation vitamin D status and neonatal abdominal adiposity. Int J Obes 42:1296–1305. https://doi.org/10.1038/s41366-018-0032-2
Black LJ, Burrows S, Lucas RM et al (2016) Serum 25-hydroxyvitamin D concentrations and cardiometabolic risk factors in adolescents and young adults. Br J Nutr 115:1994–2002. https://doi.org/10.1017/S0007114516001185
García-Bailo B, Karmali M, Badawi A, El-Sohemy A (2013) Plasma 25-hydroxyvitamin D, hormonal contraceptive use, and cardiometabolic disease risk in an ethnically diverse population of young adults. J Am Coll Nutr 32:296–306. https://doi.org/10.1080/07315724.2013.826112
Gooding HC, Gidding SS, Moran AE et al (2020) Challenges and opportunities for the prevention and treatment of cardiovascular disease among young adults: report from a national heart, lung, and blood institute working group. J Am Heart Assoc Cardiovasc Cerebrovasc Dis 9:e016115. https://doi.org/10.1161/JAHA.120.016115
Sanchez-Delgado G, Martinez-Tellez B, Olza J et al (2015) Activating brown adipose tissue through exercise (ACTIBATE) in young adults: rationale, design and methodology. Contemp Clin Trials 45:416–425. https://doi.org/10.1016/j.cct.2015.11.004
World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310:2191–2194. https://doi.org/10.1001/jama.2013.281053
Whelton PK, Williams B (2018) The 2018 European Society of Cardiology/European Society of Hypertension and 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines: more similar than different. JAMA 320:1749–1750. https://doi.org/10.1001/jama.2018.16755
Holick MF, Binkley NC, Bischoff-Ferrari HA et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930. https://doi.org/10.1210/jc.2011-0385
Ascaso JF, Romero P, Real JT et al (2001) Insulin resistance quantification by fasting insulin plasma values and HOMA index in a non-diabetic population. Med Clin (Barc) 117:530–533. https://doi.org/10.1016/s0025-7753(01)72168-9
Bedogni G, Bellentani S, Miglioli L et al (2006) The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol 6:33. https://doi.org/10.1186/1471-230X-6-33
Jurado-Fasoli L, Di X, Kohler I et al (2022) Omega-6 and omega-3 oxylipins as potential markers of cardiometabolic risk in young adults. Obesity 30:50–61. https://doi.org/10.1002/oby.23282
Di Zazzo A, Yang W, Coassin M et al (2020) Signaling lipids as diagnostic biomarkers for ocular surface cicatrizing conjunctivitis. J Mol Med Berl Ger 98:751–760. https://doi.org/10.1007/s00109-020-01907-w
Carracher AM, Marathe PH, Close KL (2018) International diabetes federation 2017. J Diabetes 10:353–356. https://doi.org/10.1111/1753-0407.12644
Ortega FB, Lavie CJ, Blair SN (2016) Obesity and cardiovascular disease. Circ Res 118:1752–1770. https://doi.org/10.1161/CIRCRESAHA.115.306883
Lutsey PL, Michos ED (2013) Vitamin D, calcium, and atherosclerotic risk: evidence from serum levels and supplementation studies. Curr Atheroscler Rep 15:293. https://doi.org/10.1007/s11883-012-0293-5
Forney LA, Earnest CP, Henagan TM et al (2014) Vitamin D status, body composition, and fitness measures in college-aged students. J Strength Cond Res 28:814–824. https://doi.org/10.1519/JSC.0b013e3182a35ed0
Lerchbaum E, Trummer C, Theiler-Schwetz V et al (2019) Effects of vitamin D supplementation on body composition and metabolic risk factors in men: a randomized controlled trial. Nutrients 11:1894. https://doi.org/10.3390/nu11081894
Vimaleswaran KS, Berry DJ, Lu C et al (2013) Causal relationship between obesity and vitamin D status: bi-directional mendelian randomization analysis of multiple cohorts. PLoS Med 10:e1001383. https://doi.org/10.1371/journal.pmed.1001383
Li J, Gao Y, Yu T et al (2020) Obesity and leptin influence vitamin D metabolism and action in human marrow stromal cells. J Steroid Biochem Mol Biol 198:105564. https://doi.org/10.1016/j.jsbmb.2019.105564
Roizen JD, Long C, Casella A et al (2019) Obesity decreases hepatic 25-hydroxylase activity causing low serum 25-hydroxyvitamin D. J Bone Miner Res Off J Am Soc Bone Miner Res 34:1068–1073. https://doi.org/10.1002/jbmr.3686
Jean G, Souberbielle JC, Chazot C (2017) Vitamin D in chronic kidney disease and dialysis patients. Nutrients 9:328. https://doi.org/10.3390/nu9040328
Hu X, Ma X, Luo Y et al (2018) Associations of serum fibroblast growth factor 23 levels with obesity and visceral fat accumulation. Clin Nutr 37:223–228. https://doi.org/10.1016/j.clnu.2016.12.010
de la Guía-Galipienso F, Martínez-Ferran M, Vallecillo N et al (2021) Vitamin D and cardiovascular health. Clin Nutr Edinb Scotl 40:2946–2957. https://doi.org/10.1016/j.clnu.2020.12.025
Cheng Q, Boucher BJ, Leung PS (2013) Modulation of hypovitaminosis D-induced islet dysfunction and insulin resistance through direct suppression of the pancreatic islet renin–angiotensin system in mice. Diabetologia 56:553–562. https://doi.org/10.1007/s00125-012-2801-0
Dolinsky DH, Armstrong S, Mangarelli C, Kemper AR (2013) The association between vitamin D and cardiometabolic risk factors in children: a systematic review. Clin Pediatr (Phila) 52:210–223. https://doi.org/10.1177/0009922812470742
Abboud M (2020) Vitamin D supplementation and blood pressure in children and adolescents: a systematic review and meta-analysis. Nutrients 12:E1163. https://doi.org/10.3390/nu12041163
Lips P, Eekhoff M, van Schoor N et al (2017) Vitamin D and type 2 diabetes. J Steroid Biochem Mol Biol 173:280–285. https://doi.org/10.1016/j.jsbmb.2016.11.021
Dominguez EAT, Peñafiel AM, Pedraza AG, Leo EEM (2021) Molecular mechanisms from insulin-mimetic effect of vitamin D: treatment alternative in Type 2 diabetes mellitus. Food Funct 12:6682–6690. https://doi.org/10.1039/D0FO03230A
Benaim C, Cocate PG, de Barros EG et al (2019) Longitudinal association of 25-hydroxyvitamin D with adipokines and markers of glucose metabolism among Brazilian pregnant women. Br J Nutr 121:42–54. https://doi.org/10.1017/S0007114518003057
Jeenduang N, Sangkaew B (2020) The association between serum 25-hydroxyvitamin D concentrations and serum lipids in the Southern Thai population. Arch Med Sci AMS 18:11–17. https://doi.org/10.5114/aoms.2020.101100
Karnchanasorn R, Ou H-Y, Chiu KC (2012) Plasma 25-hydroxyvitamin D levels are favorably associated with β-cell function. Pancreas 41:863–868. https://doi.org/10.1097/MPA.0b013e31823c947c
Kelishadi R, Farajzadegan Z, Bahreynian M (2014) Association between vitamin D status and lipid profile in children and adolescents: a systematic review and meta-analysis. Int J Food Sci Nutr 65:404–410. https://doi.org/10.3109/09637486.2014.886186
Skaaby T, Husemoen LLN, Borglykke A et al (2014) Vitamin D status, liver enzymes, and incident liver disease and mortality: a general population study. Endocrine 47:213–220. https://doi.org/10.1007/s12020-013-0107-8
Kwok RM, Torres DM, Harrison SA (2013) Vitamin D and nonalcoholic fatty liver disease (NAFLD): is it more than just an association? Hepatol Baltim Md 58:1166–1174. https://doi.org/10.1002/hep.26390
Barchetta I, Cimini FA, Chiappetta C et al (2020) Relationship between hepatic and systemic angiopoietin-like 3, hepatic Vitamin D receptor expression and NAFLD in obesity. Liver Int Off J Int Assoc Study Liver 40:2139–2147. https://doi.org/10.1111/liv.14554
Hao Y, Ma X, Luo Y et al (2014) Serum vitamin D is associated with non-alcoholic fatty liver disease in Chinese males with normal weight and liver enzymes. Acta Pharmacol Sin 35:1150–1156. https://doi.org/10.1038/aps.2014.48
Mansur JL, Tajer C, Mariani J et al (2020) Vitamin D high doses supplementation could represent a promising alternative to prevent or treat COVID-19 infection. Clin E Investig En Arterioscler Publicacion Of Soc Espanola Arterioscler 32:267–277. https://doi.org/10.1016/j.arteri.2020.05.003
Sharma S, Kumar A, Choudhary A et al (2020) Neuroprotective role of oral vitamin D supplementation on consciousness and inflammatory biomarkers in determining severity outcome in acute traumatic brain injury patients: a double-blind randomized clinical trial. Clin Drug Investig 40:327–334. https://doi.org/10.1007/s40261-020-00896-5
Subramanian K, Bergman P, Henriques-Normark B (2017) Vitamin D promotes pneumococcal killing and modulates inflammatory responses in primary human neutrophils. J Innate Immun 9:375–386. https://doi.org/10.1159/000455969
Qi G, Yu K, Feng Y et al (2021) 1α,25-dihydroxyvitamin D3 promotes early osteogenic differentiation of PDLSCs and a 12-year follow-up case of early-onset vitamin D deficiency periodontitis. J Steroid Biochem Mol Biol 208:105805. https://doi.org/10.1016/j.jsbmb.2020.105805
Zhang C, Fu S, Zhao M et al (2020) Associations between complement components and vitamin D and the physical activities of daily living among a longevous population in Hainan, China. Front Immunol 11:1543. https://doi.org/10.3389/fimmu.2020.01543
Knuth MM, Stutts WL, Ritter MM et al (2021) Vitamin D deficiency promotes accumulation of bioactive lipids and increased endocannabinoid tone in zebrafish. J Lipid Res 62:100142. https://doi.org/10.1016/j.jlr.2021.100142
Nandi A, Wadhwani N, Joshi SR (2019) Vitamin D deficiency influences fatty acid metabolism. Prostaglandins Leukot Essent Fatty Acids 140:57–63. https://doi.org/10.1016/j.plefa.2018.11.014
Blue MN, Trexler ET, Hirsch KR, Smith-Ryan AE (2019) A profile of body composition, omega-3 and vitamin D in National Football League players. J Sports Med Phys Fitness 59:87–93. https://doi.org/10.23736/S0022-4707.18.08122-7
Schmill MP, Thompson Z, Argueta DA et al (2022) Effects of selective breeding, voluntary exercise, and sex on endocannabinoid levels in the mouse small-intestinal epithelium. Physiol Behav 245:113675. https://doi.org/10.1016/j.physbeh.2021.113675
Guida F, Boccella S, Belardo C et al (2020) Altered gut microbiota and endocannabinoid system tone in vitamin D deficiency-mediated chronic pain. Brain Behav Immun 85:128–141. https://doi.org/10.1016/j.bbi.2019.04.006
Acknowledgements
The authors would like to thank all the participants of this study for their time and effort.
Funding
This study was supported by the Spanish Ministry of Economy and Competitiveness via the Fondo de Investigación Sanitaria del Instituto de Salud Carlos III (PI13/01393), and PTA-12264, Retos de la Sociedad (DEP2016-79512-R), Spain and European Regional Development Funds (ERDF), the Spanish Ministry of Education (FPU18/03357 and FPU19/01609); the Fundación Iberoamericana de Nutrición (FINUT), Spain; the Redes Temáticas de Investigación Cooperativa RETIC (Red SAMID RD16/0022), Spain; the AstraZeneca HealthCare Foundation, the University of Granada Plan Propio de Investigación 2016 – Excellence actions: Unit of Excellence on Exercise and Health (UCEES), the Plan Propio de Investigación 2018 – Programa Contratos-Puente, Spain; the Junta de Andalucía, Consejería de Conocimiento, Investigación y Universidades, the Fundación Alfonso Martin Escudero and by the CIBEROBN, Centro de Investigación Biomédica en Red (CB22/03/00058), Instituto de Salud Carlos III, Ministerio de Ciencia e Innovación and Unión Europea – European Regional Development Fund.
Author information
Authors and Affiliations
Contributions
F.J.A-G: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, software, supervision, validation, visualization, writing—original draft and writing—review and editing; H.V-L: funding acquisition, software, visualization, writing—original draft and writing—review and editing; L.J-F: conceptualization, funding acquisition, investigation, methodology, and writing—review and editing; M.D-M: conceptualization, funding acquisition, investigation, methodology, and writing—review and editing; I.K: investigation, methodology, software, and writing—review and editing; J.R.R: conceptualization, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing—original draft and writing—review and editing.
Corresponding authors
Ethics declarations
Conflict of interest
None declared.
Research involving human participants and/or animals
The study was approved by the University of Granada Ethics Committee on Human Research (no. 924) and by that the Servicio Andaluz de Salud and was following the principles of the latest version of the Declaration of Helsinki [25].
Informed consent
All participants gave their written informed consent to be included before their enrollment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Amaro-Gahete, F.J., Vázquez-Lorente, H., Jurado-Fasoli, L. et al. Low vitamin D levels are linked with increased cardiovascular disease risk in young adults: a sub-study and secondary analyses from the ACTIBATE randomized controlled trial. J Endocrinol Invest (2024). https://doi.org/10.1007/s40618-023-02272-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40618-023-02272-4