Abstract
Purpose of Review
The degeneration of the intervertebral disc (IVD) is a progressive disease that involves drastic structural and molecular changes due to increased catabolism in the annulus fibrosus (AF) and nucleus pulposus (NP) causing inflammation, and eventually, lower back pain.
Recent Findings
As alternatives to the highly invasive and conservative surgical interventions, more regenerative tissue engineering approaches using biomaterials have been suggested. Natural and synthetic biomaterials are being extensively explored for either separate or collective NP and AF repair, for conferring differing functionalities to the tissue rudiment. The need for biomaterials arises from their potential to provide structural support, pain alleviation, increased anabolism, a carrier for cells and sustained release of therapeutic molecules to target specific signaling pathways or have therapeutic effects of their own.
Summary
Here, we review the biomaterials that have been studied for disc repair where the aim is to reinstate the healthy tissue composition and disc height and restore the function of the disc through regeneration. The complexity of the disc tissue and the information gaps in the disease mechanism still remains a challenge facing a satisfactory tissue engineering strategy for IVD regeneration.

Similar content being viewed by others
References
Ho-Pham LT, Lai TQ, Mai LD, Doan MC, Pham HN, Nguyen TV. Prevalence and pattern of radiographic intervertebral disc degeneration in Vietnamese : a population-based study. Calcif Tissue Int. 2015. https://doi.org/10.1007/s00223-015-9986-4.
Shankar H, Scarlett JA, Abram SE. Anatomy and pathophysiology of intervertebral disc disease. Tech Reg Anesth Pain Manag. 2009;13(2):67–75.
Chou AI, Bansal A, Miller GJ, Nicoll SB. The effect of serial monolayer passaging on the collagen expression profile of outer and inner anulus fibrosus cells. Spine (Phila Pa 1976). 2006;31(17):1875–81.
Francoise M, Abdul AM. Investigation of the laminate structure of lumbar disc anulus fibrosus. Spine (Phila. Pa. 1976). 1990;15(5):402–10.
Maroudas A, Stockwell RA, Nachemson A, Urban J. Factors involved in the nutrition of the human lumbar intervertebral disc: cellularity and diffusion of glucose in vitro. Anatomy. 1975;121(1):113–30.
Urban JP, Roberts S. Development and degeneration of the intervertebral discs. Mol Med Today. 1995;1(7):329–35.
McCann MR, Séguin CA. Notochord cells in intervertebral disc development and degeneration. J Dev Biol. 2016;4(1):1–18.
Wuertz K, Vo N, Kletsas D, Boos N. Inflammatory and catabolic signalling in intervertebral discs: the roles of NF-κB and MAP kinases. Eur Cell Mater. 2012;23:103–20.
Cs-Szabo G, Ragasa-San Juan D, Turumella V, Masuda K, Thonar EJ-MA, An HS. Changes in mRNA and protein levels of proteoglycans of the anulus fibrosus and nucleus pulposus during intervertebral disc degeneration. Spine (Phila. Pa. 1976). 2002;27(20):2212–9.
Le Maitre CL, Pockert A, Buttle DJ, Freemont AJ, Hoyland JA. Matrix synthesis and degradation in human intervertebral disc degeneration. Biochem Soc Trans. 2007;35(Part 4):652–5.
Le Maitre CL, Freemont AJ, Hoyland JA. The role of interleukin-1 in the pathogenesis of human intervertebral disc degeneration. Arthritis Res Ther. Jan. 2005;7(4):R732–45.
Burke JG, Watson RWG, McCormack D, Dowling FE, Walsh MG, Fitzpatrick JM. Intervertebral discs which cause low back pain secrete high levels of proinflammatory mediators. J Bone Joint Surg. 2002;84(2):196–201.
Shamji MF, et al. Proinflammatory cytokine expression profile in degenerated and herniated human intervertebral disc tissues. Arthritis Rheum. 2010;62(7):1974–82.
Altun I. Cytokine profile in degenerated painful intervertebral disc: variability with respect to duration of symptoms and type of disease. Spine J. 2016;16(7):857–61.
Purmessur D, a Walter B, Roughley PJ, Laudier DM, Hecht AC, Iatridis J. A role for TNFα in intervertebral disc degeneration: a non-recoverable catabolic shift. Biochem Biophys Res Commun. 2013;433(1):151–6.
Wang J, Markova D, Anderson DG, Zheng Z, Shapiro IM, Risbud MV. TNF-alfa and IL-1beta promote a disintegrin-like and metalloprotease with thrombospondin type I motif-5-mediated aggrecan degradation through syndecan-4 in intervertebral disc. J Biol Chem. 2011;286(46):39738–49.
Anderson DG, Albert TJ. The molecular basis of intervertebral disk degeneration. Semin Spine Surg. Dec. 2003;15(4):352–60.
Stefanakis M, et al. Annulus fissures are mechanically and chemically conducive to the ingrowth of nerves and blood vessels. Spine (Phila. Pa. 1976). 2012;37(22):1883–91.
García-Cosamalón J, et al. Intervertebral disc, sensory nerves and neurotrophins: who is who in discogenic pain? J Anat. 2010;217(1):1–15.
Iatridis James C, Weidenbaum M, Setton LA, Mow VC. Is the nucleus pulposus a solid or a fluid? Mechanical behaviors of the nucleus pulposus of the human intervertebral disc. Spine (Phila Pa 1976). 1996;21(10):1174–84.
Kushchayev SV, et al. ABCs of the degenerative spine. Insights Imaging. 2018;9:253–74. https://doi.org/10.1007/s13244-017-0584-z.
Borem R, Madeline A, Walters J, Mayo H, Gill S, Mercuri J. Angle-ply biomaterial scaffold for annulus fibrosus repair replicates native tissue mechanical properties, restores spinal kinematics, and supports cell viability. Acta Biomater. 2017;58:254–68.
Zeng Y, et al. Injectable microcryogels reinforced alginate encapsulation of mesenchymal stromal cells for leak-proof delivery and alleviation of canine disc degeneration. Biomaterials. 2015;59:53–65.
Zhou X, et al. Genipin cross-linked type II collagen/chondroitin sulfate composite hydrogel-like cell delivery system induces differentiation of adipose-derived stem cells and regenerates degenerated nucleus pulposus. Acta Biomater. 2018. https://doi.org/10.1016/j.actbio.2018.03.019.
Navaro Y, et al. Matrix stiffness determines the fate of nucleus pulposus–derived stem cells. Biomaterials. 2015;49:68–76.
Frauchiger DA, Tekari A, Wöltje M, Fortunato G, Benneker LM, Gantenbein B. A review of the application of reinforced hydrogels and silk as biomaterials for intervertebral disc repair. Eur Cell Mater. 2017;34:271–90.
Pereira DR, Oliveira JM, Reis RL. Nanocellulose reinforced gellan-gum hydrogels as potential biological substitutes for annulus fibrosus tissue regeneration. Nanomed Nanotechnol Biol Med:2017. https://doi.org/10.1016/j.nano.2017.11.011.
Iu J, Santerre JP, Kandel RA. Towards engineering distinct multi-lamellated outer and inner annulus fibrosus tissues. J Orthop Res. 2017:1–10. https://doi.org/10.1002/jor.23793.
Sloan SR, Galesso D, Secchieri C, Berlin C, Hartl R, Bonassar LJ. Initial investigation of individual and combined annulus fibrosus and nucleus pulposus repair ex vivo. Acta Biomater. 2017;59:192–9.
Pennicooke B, et al. Annulus fibrosus repair using high-density collagen gel. Spine (Phila. Pa. 1976). 2018;43(4):208–15.
Zhu Y, et al. Development of kartogenin-conjugated chitosan–hyaluronic acid hydrogel for nucleus pulposus regeneration. Biomater Sci. 2017;5:784–91.
Gan Y, et al. An interpenetrating network-strengthened and toughened hydrogel that supports cell-based nucleus pulposus regeneration. Biomaterials. 2017;136:12–28.
Tsaryk R, et al. Collagen-low molecular weight hyaluronic acid semi-interpenetrating network loaded with gelatin microspheres for cell and growth factor delivery for nucleus pulposus regeneration. Acta Biomater. 2015;20:10–21.
Sivan SS, et al. Injectable hydrogels with high fixed charge density and swelling pressure for nucleus pulposus repair: biomimetic glycosaminoglycan analogues. Acta Biomater. 2014;10:1124–33.
Antunes JC, et al. Poly (γ-glutamic acid ) and poly (γ-glutamic acid)-based nanocomplexes enhance type II collagen production in intervertebral disc. J Mater Sci Mater Med. 2017;28(6):1–17.
Growney Kalaf EA, Pendyala M, Bledsoe JG, Sell SA. Characterization and restoration of degenerated IVD function with an injectable, in situ gelling alginate hydrogel: an in vitro and ex vivo study. J Mech Behav Biomed Mater. 2017;72:229–40.
Vicente AP-S, et al. Self-healing dynamic hydrogel as injectable shock-absorbing artificial nucleus pulposus. Biomacromolecules. 2017;18:2360–−2370.
Long RG, et al. In vitro and biomechanical screening of polyethylene glycol and poly(trimethylene carbonate) block copolymers for annulus fibrosus repair. J Tissue Eng Regen Med. 2018;12:727–36.
Cruz MA, et al. Cell-seeded adhesive biomaterial for repair of annulus fibrosus defects in intervertebral discs. Tissue Eng:2017. https://doi.org/10.1089/ten.TEA.2017.0334.
Kang R, et al. Cyanoacrylate medical glue application in intervertebral disc annulus defect repair: mechanical and biocompatible evaluation. J Biomed Mater Res Part B. 2017;105B:14–20.
Ma J, et al. A novel electrospun-aligned nanoyarn/three- dimensional porous nanofibrous hybrid scaffold for annulus fibrosus tissue engineering. Int J Nanomedicine. 2018;13:1553–67.
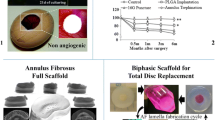
Xin L, Zhang C, Zhong F, Fan S, Wang W, Wang Z. Minimal invasive annulotomy for induction of disc degeneration and implantation of poly (lactic-co-glycolic acid) (PLGA) plugs for annular repair in a rabbit model. Eur J Med Res. 2016;21(7):1–11.
Martin JT, et al. In vivo performance of an acellular disc-like angle ply structure (DAPS) for total disc replacement in a small animal model. J Orthop Res. 2016:1–9. https://doi.org/10.1002/jor.23310.
Siskey R, Ciccarelli L, Lui MKC, Kurtz SM. Are PEEK-on-ceramic bearings an option for total disc arthroplasty? An in vitro tribology study. Clin Orthop Relat Res. 2016;474:2428–40.
O’Brien FJ. Biomaterials & scaffolds for tissue engineering. Mater Today. 2011;14(3):88–95.
Larrañaga A, et al. Antioxidant functionalized polymer capsules to prevent oxidative stress. Acta Biomater. 2017;67:21–31.
Gan Y, et al. A controlled release codelivery system of MSCs encapsulated in dextran/gelatin hydrogel with TGF-B3-loaded nanoparticles for nucleus pulposus regeneration. Stem Cells Int. 9042019:2016.
Bian Z, Sun J. Development of a KLD-12 polypeptide/TGF-β1-tissue scaffold promoting the differentiation of mesenchymal stem cell into nucleus pulposus-like cells for treatment of intervertebral disc degeneration. Int J Clin Exp Pathol. 2015;8(2):1093–103.
Tellegen AR, et al. Intradiscal application of a PCLA–PEG–PCLA hydrogel loaded with celecoxib for the treatment of back pain in canines: what’s in it for humans? J Tissue Eng Regen Med. 2018;12:642–52.
Likhitpanichkul M, et al. Fibrin-genipin annulus fibrosus sealant as a delivery system for anti-TNFα drug. Spine J. 2015;15(2015):2045–54.
Gorth DJ, et al. IL-1ra delivered from poly(lactic-co-glycolic acid) microspheres attenuates IL-1beta mediated degradation of nucleus pulposus in vitro. Arthritis Res Ther. 2012;14(4):R179.
Feng G, et al. Injectable nanofibrous spongy microspheres for NR4A1 plasmid DNA transfection to reverse fibrotic degeneration and support disc regeneration. Biomaterials. 2017;131:86–97.
Fontana G, Thomas D, Collin E, Pandit A. Microgel microenvironment primes adipose-derived stem cells towards an NP cells-like phenotype. Adv Healthc Mater. 2014;3(12):2012–22.
Thorpe AA, et al. Thermally triggered hydrogel injection into bovine intervertebral disc tissue explants induces differentiation of mesenchymal stem cells and restores mechanical function. Acta Biomater. 2017;54:212–26.
Bhunia BK, Kaplan DL, Mandal BB. Silk-based multilayered angle-ply annulus fibrosus construct to recapitulate form and function of the intervertebral disc. Proc Natl Acad Sci. 2018;115(3):477–82.
Xu X, Hu J, Lu H. Histological observation of a gelatin sponge transplant loaded with bone marrow-derived mesenchymal stem cells combined with platelet-rich plasma in repairing an annulus defect. PLoS One. 2017;12(2):1–15.
Frith JE, et al. Effects of bound versus soluble pentosan polysulphate in PEG/HA-based hydrogels tailored for intervertebral disc regeneration. Biomaterials. 2014;35(4):1150–62.
Frith JE, et al. An injectable hydrogel incorporating mesenchymal precursor cells and pentosan polysulphate for intervertebral disc regeneration. Biomaterials. 2013;34(37):9430–40.
Li YY, et al. Delivering mesenchymal stem cells in collagen microsphere carriers to rabbit degenerative disc: reduced risk of osteophyte formation. Tissue Eng A. 2014;20(9–10):1379–91.
Gruber HE, Leslie K, Ingram J, Norton HJ, Hanley EN. Cell-based tissue engineering for the intervertebral disc: in vitro studies of human disc cell gene expression and matrix production within selected cell carriers. Spine J. 2004;4(1):44–55.
Sakai D, Andersson GBJ. Stem cell therapy for intervertebral disc regeneration: obstacles and solutions. Nat Rev Rheumatol. 2015;11(4):243–56.
Helen W, Merry CLR, Blaker JJ, Gough JE. Three-dimensional culture of annulus fibrosus cells within PDLLA/bioglass composite foam scaffolds: assessment of cell attachment , proliferation and extracellular matrix production. Biomaterials. 2007;28:2010–20.
Halloran DO, Grad S, Stoddart M, Dockery P, Alini M, Pandit A. An injectable cross-linked scaffold for nucleus pulposus regeneration. Biomaterials. 2008;29:438–47.
Chang G, Kim HJ, Kaplan D, Vunjak-Novakovic G, Kandel RA. Porous silk scaffolds can be used for tissue engineering annulus fibrosus. Eur Spine J. 2007;16:1848–57.
Collin EC, et al. An injectable vehicle for nucleus pulposus cell-based therapy. Biomaterials. 2011;32:2862–70.
Nerurkar NL, Elliott DM, Mauck RL. Mechanics of oriented electrospun nanofibrous scaffolds for annulus fibrosus tissue engineering. J Orthop Res. 2007:1018–28. https://doi.org/10.1002/jor.
Attia M, Santerre JP, Kandel RA. The response of annulus fibrosus cell to fibronectin-coated nanofibrous polyurethane-anionic dihydroxyoligomer scaffolds. Biomaterials. 2011;32:450–60.
Bhattacharjee M, et al. Oriented lamellar silk fibrous scaffolds to drive cartilage matrix orientation : towards annulus fibrosus tissue engineering. Acta Biomater. 2012;8:3313–25.
Park S, et al. Annulus fibrosus tissue engineering using lamellar silk scaffolds. J Tissue Eng Regen Med. 2012;6(Suppl 3):s24–33.
Omlor GW, et al. Injection of a polymerized hyaluronic acid/collagen hydrogel matrix in an in vivo porcine disc degeneration model. Eur Spine J. 2012;21:1700–8.
Jeong CG, Francisco AT, Niu Z, Mancino RL, Craig SL, Setton LA. Screening of hyaluronic acid-poly(ethylene glycol) composite hydrogels to support intervertebral disc cell biosynthesis using artificial neural network analysis. Acta Biomater. 2014;10:3421–30.
Kazezian Z, Li Z, Alini M, Grad S, Pandit A. Injectable hyaluronic acid down-regulates interferon signaling molecules , IGFBP3 and IFIT3 in the bovine intervertebral disc. Acta Biomater. 2017;52:118–29.
Yu-Chun C, We-Yu S, Shu-Hua Y, Amit G, Feng-Huei L. In situ forming hydrogels composed of oxidized high molecular weight hyaluronic acid and gelatin for nucleus pulposus regeneration. Acta Biomater. 2013;9:5181–93.
Lee H, Hwang C, Kim H, Jeong S. Enhancement of bio-stability and mechanical properties of hyaluronic acid hydrogels by tannic acid treatment. Carbohydr Polym. 2018;186:290–8.
Raspanti M, Caravà E, Sgambato A, Natalello A, Russo L, Cipolla L. The collaggrecan: synthesis and visualization of an artificial proteoglycan. Int J Biol Macromol. 2016;86:65–70.
Yuan D, et al. Regenerative intervertebral disc endplate based on biomimetic three-dimensional scaffolds. Spine (Phila. Pa. 1976). 2017;42(5):E260–6.
Li Z, et al. Heterodimeric BMP-2/7 for nucleus pulposus regeneration — In vitro and ex vivo studies. J Orthop Res. 2017:51–60. https://doi.org/10.1002/jor.23351.
Paglia DN, Singh H, Karukonda T, Drissi H, Moss IL. PDGF-BB delays degeneration of the intervertebral discs in a rabbit preclinical model. Spine. 2016;41(8):E449–58.
Teixeira GQ, et al. A degenerative/proinflammatory intervertebral disc organ culture: an ex vivo model for anti-inflammatory drug and cell therapy. Tissue Eng Part C. 2016;22(1):8–19.
Ahn J, et al. Transplantation of human Wharton’s jelly-derived mesenchymal stem cells highly expressing TGFβ receptors in a rabbit model of disc degeneration. Stem Cell Res Ther. 2015;6(190):1–13.
Pan Z, et al. Therapeutic effects of gefitinib-encapsulated thermosensitive injectable hydrogel in intervertebral disc degeneration. Biomaterials. 2018;160:56–68.
Costa J, Silva-correia J, Pinto V, Morais S, Miguel J, Luís R. Engineering patient-specific bioprinted constructs for treatment of degenerated intervertebral disc. Mater Today Commun. 2018:1–7. https://doi.org/10.1016/j.mtcomm.2018.01.011.
Khandaker M, Riahanizad S. Evaluation of electrospun nanofiber-anchored silicone for the degenerative intervertebral disc. J Healthc Eng. 2017;2017:1–8. https://doi.org/10.1155/2017/5283846.
Sato M, et al. Tissue engineering of the intervertebral disc with cultured annulus fibrosus cells using atelocollagen honeycomb-shaped scaffold with a membrane seal (ACHMS scaffold). Med Biol Eng Comput. 2003;41:365–71.
Isa ILM, et al. Hyaluronic acid based hydrogels attenuate inflammatory receptors and neurotrophins in interleukin-1β induced inflammation model of nucleus pulposus cells. Biomacromolecules. 2015;16(6):1714–25.
Mohd Isa IL, et al. Implantation of hyaluronic acid hydrogel prevents the pain phenotype in a rat model of intervertebral disc injury. Sci Adv. 2018;4(eaaq0597):1–19.
Pluijm SMF, et al. Collagen type I a1 Sp1 polymorphism, osteoporosis, and intervertebral disc degeneration in older men and women. Ann Rheum Dis. 2004;63:71–7.
Mio F, et al. A functional polymorphism in COL11A1, which encodes the α1 chain of type XI collagen, is associated with susceptibility to lumbar disc herniation. Am J Hum Genet. 2007;81(6):1271–7.
Solovieva S, et al. Intervertebral disc degeneration in relation to the COL9A3 and the IL-1β gene polymorphisms. Eur Spine J. 2006;15:613–9.
Solovieva S, et al. Interleukin 1 polymorphisms and intervertebral disc degeneration. Epidemiology. 2004;15(5):626–33.
Sarath Babu N, Krishnan S, Brahmendra Swamy CV, Venkata Subbaiah GP, Gurava Reddy AV, Idris MM. Quantitative proteomic analysis of normal and degenerated human intervertebral disc. Spine J. 2016;16(8):989–1000.
Collin EC, et al. Unique glycosignature for intervertebral disc and articular cartilage cells and tissues in immaturity and maturity. Sci Rep. 2016;6(23062):1–12.
Acknowledgements
Authors would like to acknowledge Science Foundation Ireland (SFI); the European Regional Development Fund (Grant Number 13/RC/2073); and CMNHS Scholarship, National University Ireland, Galway.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Isma Liza Mohd Isa, Büşra Günay, Kieran Joyce and Abhay Pandit each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Intervertebral Disk Degeneration and Regeneration
Rights and permissions
About this article
Cite this article
Isa, I.L.M., Günay, B., Joyce, K. et al. Tissue Engineering: Biomaterials for Disc Repair. Curr Mol Bio Rep 4, 161–172 (2018). https://doi.org/10.1007/s40610-018-0106-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40610-018-0106-x