Abstract
Background & aim
More elderly patients are diagnosed with kidney tumors where partial nephrectomy is technically possible. We investigated whether patients ≥ 75 years old had an increased risk of complications following robot-assisted partial nephrectomy (RAPN) compared to younger patients.
Methods
Retrospective, consecutive study including patients who underwent RAPN between May 2016 – April 2023. Preoperative data, operative data and complications within 90 days were recorded by patient record review. Complications were classified according to Clavien-Dindo (CD).
Results
451 patients underwent RAPN and a postoperative complication was recorded in 131 (29%) patients of which 28 (6%) were CD ≥ III. Any postoperative complication was recorded in 24/113 patients (21%) < 55 years, 40/127 patients (31%) 55–64 years, 45/151 patients (42%) 65–74 years, and 22/60 patients (37%) ≥ 75 years. Comparable numbers for a CD ≥ III postoperative complication were 2/113 (2%) < 55 years, 6/127 (7%) 55–64 years, 12/151 (8%) 65–74 years, and 5/60 (8%) ≥ 75 years. In multivariate logistic regression analysis, patients ≥ 75 years had a non-significant increased risk of complications when controlling for preoperative variables (OR 1.82 [95% CI 0.80–4.13]) or perioperative variables (OR 1.98 [95% CI 0.86–4.58]) compared to patients < 55 years. Two patients died postoperatively. Both were ≥ 75 years (2/60, 3%).
Discussion and conclusions
Selected patients ≥ 75 years can undergo RAPN without a significantly increased risk of postoperative complications. However, a mortality rate of 3% in this age group indicates that these patients are frail when postoperative complications occur.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) represents approximately 3% of all cancers [1]. In the European Union alone, 100 000 patients are diagnosed with RCC each year. The risk of RCC increases with age [2], and the incidence has been increasing over the last 20 years and is projected to continue to increase in the future [3]. Most of this increase is caused by incidental findings of small renal masses [4,5,6,7]. Moreover, people worldwide are living longer, and the proportion of older persons in the population is increasing [8]. Taken together more elderly patients will be diagnosed with localized RCC.
The preferred curative treatment modality for localized RCC is partial nephrectomy, when technically feasible, since it better preserves renal function compared to radical nephrectomy while still providing excellent oncological outcome [3, 9, 10]. However, there are caveats, as surgical treatment is not without risk, and many patients are diagnosed with small tumors that will pose little threat for many years [11, 12].
Previous studies have shown that frail patients are at an increased risk of postoperative complications after surgery [13]. Treatment selection for elderly patients is influenced by clinician bias, patient preferences and limited data on surgery within this age group [14, 15]. This highlights the need for knowledge about the effects of robot-assisted partial nephrectomy (RAPN) in this patient group to aid treatment selection. The purpose of this study was to investigate if patients aged 75 years or older are at an increased risk of suffering postoperative complications after RAPN compared to younger patients.
Material & methods
Retrospective, consecutive study including patients who underwent RAPN for nonmetastatic, localized renal tumors between May 2016 – April 2023 at the Department of Urology, Copenhagen University Hospital, Herlev and Gentofte Hospital, Herlev, Denmark. The following data were recorded by electronic patient record review: preoperative data (age, gender, Charlson Comorbidity Index [CCI] [16], American Society of Anesthesiologists classification [ASA] [17], body mass index [BMI], smoking status, kidney function, tumor size), operative data (duration of the procedure, warm ischemia time, blood loss), and complications within 90 days. In order to minimize bias, data retrieval and analysis was not performed by the primary operating surgeons (data retrieval and analysis was performed by R.D.P and F.F.T). Postoperative complications were classified according to the Clavien-Dindo classification (CD) [18]. The study received ethical and legal approval from the regional center for register research of the Capital Region of Denmark according to Danish law (journal number: R-23018007).
Descriptive statistics were used, and the chi-square test was used to test differences in baseline characteristics between age groups. We stratified in age groups (< 55 years, 55–64 years, 65–74 years and ≥ 75 years) in order to compare the risk of complications in different age categories. Odds ratios (OR) with 95% confidence intervals (CI) for postoperative complications were assessed with uni- and multivariate logistic regression analyses controlling for pre- and perioperative variables. The variables controlled for were, preoperative: gender (female, male), CCI (0, 1, ≥ 2), ASA (1,2, ≥ 3), BMI (< 25,25–29, ≥ 30), smoking status (never, current, former), tumor size (quartiles), and perioperative: duration of the procedure (quartiles), warm ischemia time (quartiles), and blood loss (quartiles). All tests were two-sided, and the significance level was set to p < 0.05. Statistical analysis was performed with R version 4.0.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
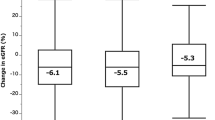
A total of 451 patients underwent RAPN, and no patients were lost to follow-up. Baseline characteristics are presented in Table 1.
152 (34%) patients were female and 299 (66%) were male. A total of 60 (13%) patients were aged ≥ 75 years (range 75–87 years), 151 (33%) were 74 − 65 years, 127 (28%) were 55–64 years and 113 (25%) were < 55 years. The median operation time was 173 (IQR 145–204) min, the median warm ischemia time was 15 (IQR 12–19) min, and the median perioperative blood loss was 100 (IQR 50–200) ml. Intraoperatively were 7 (1.5%) procedures converted to radical nephrectomy and 3 (1%) procedures were converted to open surgery, none of the cases were overlapping. There were 8 (2%) intraoperative complications: 4 spleen lesions, 2 diaphragm perforations, 1 kidney vein injury and 1 small bowel perforation. All were managed with either sutures and/or synthetic haemostatic patch. The median length of stay at the hospital was 3 (2–4 IQR) days.
Postoperative complications were recorded in 131 (29%) patients (Table 2).
Complications stratified according to CD grade: 24 (5%) patients had a CD I, 79 (18%) patients had a CD II, and 28 (6%) patients had a CD ≥ III. The most common complication was postoperative infection, which was recorded in 61 (13%) patients; out of these 42/61 (69%) patients commenced antibiotics solely because of postoperative fever, and their subsequent blood and urine cultures were negative, however they were still registered as complications in the analyses. The most frequent major complication (CD ≥ III) was postoperative bleeding, where 13 (3%) patients required intervention with either surgery or embolization.
Two (0.4%) patients died within 90 days of the procedure. Both patients were aged 75 years or older (2/60, 3%), had a CCI of 1, an ASA of 2–3 and were smokers or former smokers. The operative time and perioperative blood loss were in the upper quartile. Both had a prolonged postoperative stay with renal failure (between 13 and 16 days). One died of cardiac arrest while receiving dialysis. The other went into delirium, which could not be reversed.
Complications stratified by age group are presented in Table 3.
In univariate logistic regression analysis, patients ≥ 75 years had a higher risk of a postoperative complication (OR 2.15 [95% CI 1.07–4.31]), including CD ≥ III (OR 5.05 [95% CI 1.05-36]) compared to patients aged < 55 years (Table 3). When controlling for preoperative variables, patients ≥ 75 years had a non-significantly increased risk of any complication (OR 1.82 [95% CI 0.80–4.13]) or CD ≥ III (OR 3.21 [95% CI 0.57-25]) compared to patients < 55 years. Comparable numbers when patients aged ≥ 75 years were compared directly to (1) patients aged 55–64 years: OR 1.48 (95% CI 0.66–3.32) and 1.93 (95% CI 0.43–8.33), and (2) patients aged 65–74 years: OR 1.22 (95% CI 0.59–2.49) and 1.01 (0.26–3.55).
The same was found when controlling for perioperative variables, where patients ≥ 75 years had a non-significantly increased risk of any complication OR 1.98 (95% CI 0.86–4.58) or CD ≥ III OR 2.48 (95% CI 0.43-19) compared to patients < 55 years. Comparable numbers when patients aged ≥ 75 years were compared directly to (1) patients aged 55–64 years: OR 1.45 (95% CI 0.64–3.26) and 0.78 (95% CI 0.18–3.02), and (2) patients aged 65–74 years: OR 1.59 (95% CI 0.72–3.53) and 1.21 (0.28–4.76). A post hoc power calculation showed that the study has a power of 0.78 to show a difference in the risk of any complication between patients aged < 55 years and patients aged ≥ 75 years, with a type I error of 5%.
Large perioperative bleeding (Q4 vs. Q1 OR 2.16 [95% CI 1.11–4.21]) and long warm ischemia time (Q4 vs. Q1 OR 2.28 [95% CI 1.09–4.87]) were the only variables that were significantly associated with an increased risk of any postoperative complications in multivariate analyses. In addition, long operative time (Q4 vs. Q1 OR 4.33 [95% CI 1.02-30]) and large perioperative bleeding (Q4 vs. Q1 OR 3.96 [95% CI 1.06-19]) were the only variables that were significantly associated with an increased risk of CD ≥ III postoperative complications. Full logistic regression models are available in Supplemental Tables 1–2.
Discussion
In this retrospective consecutive study of 451 patients who underwent RAPN, we found that patients ≥ 75 years had an increased risk of postoperative complications compared to patients < 55 years, but when we controlled for pre- and perioperative variables, older age was no longer significantly associated with an increased risk of complications. Additionally, patients ≥ 75 years had a similar risk of suffering postoperative complications when compared to patients aged 55–64 and 65–74 years. This indicates that age in itself may not be a risk factor for postoperative complications following RAPN. However, with two postoperative deaths in patients ≥ 75 years, it is possible that older patients are frailer when suffering a postsurgical complication.
The main limitation of the study is its retrospective design, which could introduce biases that we were unable to control for as well as underreporting of postoperative complications. Moreover, these data were not suited to identify which patients aged ≥ 75 years were at increased risk of a major complication. The strengths of the study were the complete follow-up and that the data retrieval and analyses were not performed by the primary operating surgeons. Furthermore, postoperative care was similar for the entire cohort, as all patients were treated at the same center.
Our results are in line with those of previous publications [19,20,21,22,23,24,25]. In a recent registry study, the risk of a postoperative CD ≥III complication following 1 056 “minimal invasive” partial nephrectomies was 6.2%, and age was not found to be an independent risk factor for a postoperative complication [22]. Sandberg et al. reported comparable complication rates following RAPN in patients aged < 70 years (n = 268) vs. ≥70 years (n = 71), with 5.6% CD ≥III complications in the elderly cohort [19]. Thomas et al. found that patients aged ≥ 80 years (n = 41) did not have an increased risk of postoperative complications following laparoscopic partial nephrectomy compared to patients younger than 80 years (n = 791) [23].
The increase in the detection of small renal masses [4, 5] remains a clinical dilemma for physicians and their patients, especially in elderly patients with long expected survival. Some of these masses are benign, which could lead to overtreatment if surgical excision was performed in all these cases [26,27,28,29]. Adding a preoperative biopsy to the work-up of small renal masses could improve the diagnostics of benign tumors and thus spare some patients from undergoing unnecessary surgery [30,31,32,33]. Additionally, Lane et al. found no difference in RCC-specific or overall survival between patients aged ≥ 75 years diagnosed with cT1 kidney tumors and managed with curative intent (surgery or ablation) vs. observation [34]. On the other hand, older patients are less likely to receive surgical treatment for cancer compared to their younger counterparts, even when adjusting for comorbidity and performance status, and it has been theorized that this could contribute to poorer overall survival [14, 15]. The life expectancy of the average 75-year-old in Denmark is over 10-years. Thus, elderly patients should not be excluded as candidates for curative treatment based solely on their age [35]. This highlights the complexity of treating elderly patients with potential curable RCC and the need for further data to aid decision-making.
Studies on preoperative information which can identify patients at increased risk of postoperative complications are warranted. Also, improving preoperative optimization and postoperative rehabilitation could possibly further increase the benefits of surgery [36]. Finally, there is little information available on patient-related outcomes, such as patient choice and quality of life after cancer treatment, in elderly patients [14].
Conclusion
Selected patients aged 75 years or older can undergo RAPN without a significantly increased risk of suffering postoperative complications. However, a mortality rate of 3% in this age group indicates that these patients are frail when suffering postoperative complications. Future studies should focus on the optimal selection of surgical candidates as well as improving preoperative optimization and postoperative rehabilitation.
Data availability
No datasets were generated or analysed during the current study.
References
Ferlay J, Colombet M, Soerjomataram I, Dyba T, Randi G, Bettio M, Gavin A, Visser O, Bray F (2018) Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer. https://doi.org/10.1016/j.ejca.2018.07.005
Capitanio U, Bensalah K, Bex A, Boorjian SA, Bray F, Coleman J, Gore JL, Sun M, Wood C, Russo P (2019) Epidemiology of renal cell carcinoma [Figure presented]. https://doi.org/10.1016/j.eururo.2018.08.036. Eur Urol
Ljungberg B, Albiges L, Abu-Ghanem Y et al (2022) European Association of Urology Guidelines on Renal Cell Carcinoma: the 2022 Update. Eur Urol. https://doi.org/10.1016/j.eururo.2022.03.006
Nguyen MM, Gill IS, Ellison LM (2006) The evolving presentation of Renal Carcinoma in the United States: Trends from the Surveillance, Epidemiology, and end results program. J Urol. https://doi.org/10.1016/j.juro.2006.07.144
Hollingsworth JM, Miller DC, Daignault S, Hollenbeck BK (2006) Rising incidence of small renal masses: a need to reassess treatment effect. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djj362
Leone AR, Diorio GJ, Spiess PE, Gilbert SM (2016) Contemporary issues surrounding small renal masses: evaluation, Diagnostic Biopsy, Nephron Sparing, and Novel Treatment modalities. Oncol (Williston Park) 30
Patel HD, Gupta M, Joice GA, Srivastava A, Alam R, Allaf ME, Pierorazio PM (2019) Clinical Stage Migration and Survival for Renal Cell Carcinoma in the United States. https://doi.org/10.1016/j.euo.2018.08.023. Eur Urol Oncol
Gerland P, Hertog S, Wheldon M et al (2022) World Population Prospects 2022: Summary of results
Kim SP, Campbell SC, Gill I, Lane BR, Van Poppel H, Smaldone MC, Volpe A, Kutikov A (2017) Collaborative review of Risk Benefit Trade-offs between partial and radical nephrectomy in the management of Anatomically Complex Renal masses. Eur Urol. https://doi.org/10.1016/j.eururo.2016.11.038
Scosyrev E, Messing EM, Sylvester R, Campbell S, Van Poppel H (2014) Renal function after nephron-sparing surgery versus radical nephrectomy: results from EORTC randomized trial 30904. Eur Urol. https://doi.org/10.1016/j.eururo.2013.06.044
Alam R, Patel HD, Riffon MF, Trock BJ, Uzosike A, Chang P, Wagner AJ, McKiernan JM, Allaf M, Pierorazio PM (2017) Intermediate-term outcomes from the DISSRM registry: a prospective analysis of active surveillance in patients with small renal masses. J Clin Oncol. https://doi.org/10.1200/jco.2017.35.6_suppl.430
Gupta M, Alam R, Patel HD et al (2019) Use of delayed intervention for small renal masses initially managed with active surveillance. Urologic Oncology: Seminars Original Investigations. https://doi.org/10.1016/j.urolonc.2018.10.001
Partridge JSL, Harari D, Dhesi JK (2012) Frailty in the older surgical patient: a review. Age Ageing. https://doi.org/10.1093/ageing/afr182
Akinoso-Imran AQ, O’Rorke M, Kee F, Jordao H, Walls G, Bannon FJ (2022) Surgical under-treatment of older adult patients with cancer: a systematic review and meta-analysis. J Geriatr Oncol. https://doi.org/10.1016/j.jgo.2021.11.004
Dale DC (2003) Poor prognosis in elderly patients with cancer: the role of bias and undertreatment. J Support Oncol 1
Charlson ME, Carrozzino D, Guidi J, Patierno C (2022) Charlson Comorbidity Index: a critical review of Clinimetric Properties. Psychother Psychosom. https://doi.org/10.1159/000521288
Mayhew D, Mendonca V, Murthy BVS (2019) A review of ASA physical status – historical perspectives and modern developments. https://doi.org/10.1111/anae.14569. Anaesthesia
Mitropoulos D, Artibani W, Graefen M, Remzi M, Rouprêt M, Truss M (2012) Reporting and grading of complications after urologic surgical procedures: an ad hoc EAU guidelines panel assessment and recommendations. Eur Urol. https://doi.org/10.1016/j.eururo.2011.10.033
Sandberg JM, Krane LS, Hemal AK (2014) A nonrandomized prospective comparison of robotic-assisted partial nephrectomy in the elderly to a younger cohort: an analysis of 339 patients with intermediate-term follow-up. Urology. https://doi.org/10.1016/j.urology.2014.07.004
Ishiyama Y, Kondo T, Yoshida K, Iizuka J, Tanabe K, Takagi T (2022) Efficacy and feasibility of robot-assisted partial nephrectomy for octogenarians: comparison with younger counterparts. J Robot Surg. https://doi.org/10.1007/s11701-021-01350-0
Jivanji D, Shpeen B, Kaplan-Marans E, Neckonoff E, Silver M, Schulman A (2023) Assessing the safety of minimally invasive partial nephrectomy in octogenarians. J Robot Surg. https://doi.org/10.1007/s11701-023-01600-3
Åkerlund J, Sundqvist P, Ljungberg B, Lundstam S, Peeker R, Månsson M, Grenabo Bergdahl A (2023) Predictors for complication in renal cancer surgery: a national register study. Scand J Urol. https://doi.org/10.2340/sju.v58.12356
Thomas AA, Aron M, Hernandez AV, Lane BR, Gill IS Laparoscopic Partial Nephrectomy in Octogenarians., Urology (2009) https://doi.org/10.1016/j.urology.2009.04.099
Vartolomei MD, Matei DV, Renne G et al (2019) Long-term oncologic and functional outcomes after robot-assisted partial nephrectomy in elderly patients. Minerva Urol Nefrol. https://doi.org/10.23736/S0393-2249.18.03006-0
Antonelli A, Veccia A, Pavan N et al (2019) Outcomes of partial and radical nephrectomy in octogenarians – a Multicenter International Study (resurge). https://doi.org/10.1016/j.urology.2019.03.009. Urology
Ball MW, Bezerra SM, Gorin MA, Cowan M, Pavlovich CP, Pierorazio PM, Netto GJ, Allaf ME (2015) Grade Heterogeneity in Small Renal masses: potential implications for renal Mass Biopsy. J Urol. https://doi.org/10.1016/j.juro.2014.06.067
Tomaszewski JJ, Uzzo RG, Smaldone MC (2014) Heterogeneity and renal mass biopsy: a review of its role and reliability. Cancer Biol Med. https://doi.org/10.7497/j.issn.2095-3941.2014.03.002
Dash A, Sweet RM (2022) Evaluation and management of localized renal tumors. In: Partin Alan W. MDP, Kavoussi Louis R. MDMBA, Peters Craig A. MD, Dmochowski Roger R. MDMF (eds) Campbell Walsh Wein Handbook of Urology. pp 709–747
Johnson DC, Vukina J, Smith AB et al (2015) Preoperatively Misclassified, surgically removed Benign Renal masses: a systematic review of Surgical Series and United States Population Level Burden Estimate. J Urol. https://doi.org/10.1016/j.juro.2014.07.102
Kim JH, Li S, Khandwala Y, Chung KJ, Park HK, Chung BI (2019) Association of Prevalence of Benign Pathologic Findings after partial nephrectomy with Preoperative Imaging Patterns in the United States from 2007 to 2014. JAMA Surg. https://doi.org/10.1001/jamasurg.2018.4602
Marcelin C, Ambrosetti D, Bernhard JC, Roy C, Grenier N, Cornelis FH (2017) Percutaneous image-guided biopsies of small renal tumors: current practice and perspectives. https://doi.org/10.1016/j.diii.2017.07.008. Diagn Interv Imaging
Sinks A, Miller C, Holck H, Zeng L, Gaston K, Riggs S, Matulay J, Clark PE, Roy O (2023) Renal Mass Biopsy Mandate is Associated with Change in Treatment decisions. J Urol. https://doi.org/10.1097/JU.0000000000003429
Patel HD, Nichols PE, Su ZT, Gupta M, Cheaib JG, Allaf ME, Pierorazio PM (2020) Renal Mass Biopsy is Associated with reduction in surgery for early-stage kidney Cancer. https://doi.org/10.1016/j.urology.2019.08.043. Urology
Lane BR, Abouassaly R, Gao T, Weight CJ, Hernandez AV, Larson BT, Kaouk JH, Gill IS, Campbell SC (2010) Active treatment of localized renal tumors may not impact overall survival in patients aged 75 years or older. Cancer. https://doi.org/10.1002/cncr.25184
Statistics Denmark (2024) HISB8: Life Table (2 years tables) by sex, age and life table. www.statbank.dk/HISB8. Accessed 19 Mar 2024
Wangjian W, Tianyi L, Xiaoqian M, Di Z, Chuan Z, Chao W, Zijian D, Tongtong J, Fenghai Z (2023) Application of enhanced recovery after surgery in partial nephrectomy for renal tumors: a systematic review and meta-analysis. Front Oncol. https://doi.org/10.3389/fonc.2023.1049294
Funding
Open access funding provided by Copenhagen University
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by F.F.T. and R.D.P. R.D.P. drafted the manuscript and all authors contributed to the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Petersson, R.D., Fode, M., Niebuhr, M.H. et al. Robot-assisted partial nephrectomy in patients aged 75 years or older – comparing the risk of complications with their younger counterparts. Aging Clin Exp Res 36, 107 (2024). https://doi.org/10.1007/s40520-024-02751-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40520-024-02751-5