Abstract
Background
Frailty, a condition characterized by a reduced physiological reserve and resilience, is highly prevalent among older adults.
Aims
This study examined differences in physical activity (PA) level, sedentary behavior (SB) time, and cognitive performance in older adults living in a senior housing facility (SHF) as a function of frailty status.
Methods
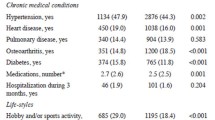
This study assessed 100 older adults from a SHF in the Midwest area of the United States. Participants were categorized as frail or non-frail according to scores observed in the short physical performance battery (SPPB), using the cutoff of nine previously stated in the literature. PA level and SB time were self-reportedly assessed using the physical activity scale for the elderly (PASE) and SB using a specific questionnaire developed for the older adult population. Cognitive performance was assessed using a collection of tests measuring cognitive processing speed, verbal learning, visuospatial memory, and verbal fluency.
Results
Frail and non-frail older adults reported similar PA level and SB time (P > .05). Frail older adults performed significantly (P < .05) worse than their counterparts, non-frail in all measures of cognitive function. However, after controlling the analysis for age, only processing speed (SDMT scores) remained statistically different (P < .05) between groups.
Discussion/conclusion
Older adults living in a SHF with different frailty status (i.e., frail vs. non-frail) report similar levels of PA level and SB time; but our findings suggest that non-frail older adults appear to have better cognitive function in terms of processing speed compared to the frail group.
Similar content being viewed by others
References
Colby SL, Ortman JM (2015) Projections of the size and composition of the US population: 2014 to 2060, Current Population Reports, P25-1143, U.S. Census Bureau, Washington, DC, 2014
Ward BW, Schiller JS, Goodman RA (2014) Multiple chronic conditions among US adults: a 2012 update. Prev Chronic Dis 11:130389. https://doi.org/10.5888/pcd11.130389
Sebastião E, Galvez PAE, Nakamura PM et al (2017) Activity behavior, nutritional status and perceived health in older Brazilian adults: does the number of chronic diseases matter? Geriatr Gerontol Int 17:2376–2382. https://doi.org/10.1111/ggi.13078
Lee SJ, Go AS, Lindquist K et al (2008) Chronic conditions and mortality among the oldest old. Am J Public Health. https://doi.org/10.2105/AJPH.2007.130955
Centers for Disease Control and Prevention (2013) The State of aging and health in America 2013. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services
Kanwar A, Singh M, Lennon R et al (2013) Frailty and health-related quality of life among residents of long-term care facilities. J Aging Health. https://doi.org/10.1177/0898264313493003
Sternberg SA, Schwartz AW, Karunananthan S et al (2011) The identification of frailty: a systematic literature review. J Am Geriatr Soc 59:2129–2138. https://doi.org/10.1111/j.1532-5415.2011.03597.x
Ahmed N, Mandel R, Fain MJ (2007) Frailty: an emerging geriatric syndrome. Am J Med 120:748–753
Clegg A, Young J, Iliffe S et al (2013) Frailty in elderly people. Lancet 381:752–762
McIsaac DI, Moloo H, Bryson GL et al (2017) The association of frailty with outcomes and resource use after emergency general surgery: a population-based cohort study. Anesth Analg 124:1653–1661. https://doi.org/10.1213/ANE.0000000000001960
Ter Chao C, Wang J, Chien KL et al (2018) Both pre-frailty and frailty increase healthcare utilization and adverse health outcomes in patients with type 2 diabetes mellitus 11 medical and health sciences 1103 clinical sciences. Cardiovasc Diabetol. https://doi.org/10.1186/s12933-018-0772-2
Saum KU, Schöttker B, Meid AD et al (2017) Is polypharmacy associated with frailty in older people? Results from the ESTHER cohort study. J Am Geriatr Soc 65:e27–e32. https://doi.org/10.1111/jgs.14718
Sánchez-Jurado PM, Salvador T, Ariza G et al (2017) Frailty, polypharmacy, and health outcomes in older adults: the frailty and dependence in Albacete study. J Am Med Dir Assoc 19:46–52. https://doi.org/10.1016/j.jamda.2017.07.008
dos Tavares DM, Faria PM, Pegorari MS et al (2018) Frailty syndrome in association with depressive symptoms and functional disability among hospitalized elderly. Issues Ment Health Nurs 39:433–438. https://doi.org/10.1080/01612840.2018.1429035
Brañas F, Jiménez Z, Sánchez-Conde M et al (2017) Frailty and physical function in older HIV-infected adults. Age Ageing 46:522–526. https://doi.org/10.1093/ageing/afx013
Wei K, Nyunt M-S-Z, Gao Q et al (2018) Association of frailty and malnutrition with long-term functional and mortality outcomes among community-dwelling older adults. JAMA Netw Open 1:e180650. https://doi.org/10.1001/jamanetworkopen.2018.0650
Huisingh-Scheetz M, Wroblewski K, Kocherginsky M et al (2018) The relationship between physical activity and frailty among U.S. older adults based on hourly accelerometry data. J Gerontol A Biol Sci Med Sci 73:622–629. https://doi.org/10.1093/gerona/glx208
Jansen FM, Prins RG, Etman A et al (2015) Physical activity in non-frail and frail older adults. PLoS One. https://doi.org/10.1371/journal.pone.0123168
Brigola AG, Rossetti ES, Rodrigues B et al (2015) Relationship between cognition and frailty in elderly: a systematic review. Dement Neuropsychol 9:107–116
Guralnik JM, Simonsick EM, Ferrucci L et al (1994) A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. https://doi.org/10.1093/geronj/49.2.M85
Verghese J, Xue X (2010) Identifying frailty in high functioning older adults with normal mobility. Age Ageing 39:382–385. https://doi.org/10.1093/ageing/afp226
da Câmara SMA, Alvarado BE, Guralnik JM et al (2013) Using the short physical performance battery to screen for frailty in young-old adults with distinct socioeconomic conditions. Geriatr Gerontol Int 13:421–428. https://doi.org/10.1111/j.1447-0594.2012.00920.x
Tieland M, Brouwer-Brolsma EM, Nienaber-Rousseau C et al (2013) Low vitamin D status is associated with reduced muscle mass and impaired physical performance in frail elderly people. Eur J Clin Nutr. https://doi.org/10.1038/ejcn.2013.144
Morley JE, Malmstrom TK, Miller DK (2012) A simple frailty questionnaire (frail) predicts outcomes in middle aged african americans. J Nutr Health Aging 16(7):601–608. https://doi.org/10.1007/s12603-012-0084-2
Washburn R, Smith K, Jette A et al (1993) The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol 46:153–162. https://doi.org/10.1016/0895-4356(93)90053-4
Martin KA, Rejeski WJ, Miller ME et al (1999) Validation of the PASE in older adults with knee pain and physical disability. Med Sci Sports Exerc 31:627–633. https://doi.org/10.1097/00005768-199905000-00001
Washburn RA, McAuley E, Katula J et al (1999) The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol 52:643–651. https://doi.org/10.1016/S0895-4356(99)00049-9
Visser M, Koster A (2013) Development of a questionnaire to assess sedentary time in older persons—A comparative study using accelerometry. BMC Geriatr. https://doi.org/10.1186/1471-2318-13-80
Smith A (1982) Symbol digit modalities test (SDMT). Manual (revised). West Psychological Services, Los Angeles. https://doi.org/10.1111/cen.13307
Sheridan LK, Fitzgerald HE, Adams KM et al (2006) Normative symbol digit modalities test performance in a community-based sample. Arch Clin Neuropsychol 21:23–28. https://doi.org/10.1016/j.acn.2005.07.003
Paolo AM, Tröster AI, Ryan JJ (1997) California verbal learning test: normative data for the elderly. J Clin Exp Neuropsychol 19:220–234. https://doi.org/10.1080/01688639708403853
Paolo AM, Tröster AI, Ryan JJ (1997) Test–retest stability of the California verbal learning test in older persons. Neuropsychology 11:613–616. https://doi.org/10.1037/0894-4105.11.4.613
Kane KD, Yochim BP (2014) Construct validity and extended normative data for older adults for the brief visuospatial memory test, revised. Am J Alzheimers Dis Other Dement 29:601–606. https://doi.org/10.1177/1533317514524812
Rosen WG (1980) Verbal fluency in aging and dementia. J Clin Neuropsychol 2:135–146. https://doi.org/10.1080/01688638008403788
Cohen J (1988) Statistical power analysis for the behavioral sciences (2ª ed.). New York: Lawrence Erlbaum Pub
Prins RG, Pierik F, Etman A et al (2014) How many walking and cycling trips made by elderly are beyond commonly used buffer sizes: results from a GPS study. Heal Place 27:127–133. https://doi.org/10.1016/j.healthplace.2014.01.012
da Silva VD, Tribess S, Meneguci J et al (2018) Time spent in sedentary behaviour as discriminant criterion for frailty in older adults. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph15071336
Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA et al (2009) American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc 41:1510–1530. https://doi.org/10.1249/MSS.0b013e3181a0c95c
Physical Activity Guidelines Advisory Committee (2018) Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S. Department of Health and Human Services
Ball K, Edwards JD, Ross LA (2007) The impact of speed of processing training on cognitive and everyday functions. J Gerontol B Psychol Sci Soc Sci 62:19–31. https://doi.org/10.1093/geronb/62.special_issue_1.19
Fried LP, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M157. https://doi.org/10.1093/gerona/56.3.M146
Acknowledgements
The author would like to thank Luis Hernandez for proof reading the final version of the manuscript, Joshua Pak for helping with data collection, and David Benner Jr. for assisting with the logistics in the senior housing facility. All three are from the Department of Kinesiology and Physical Education at Northern Illinois University.
Funding
This work was supported by the Dean’s Office, College of Education, Northern Illinois University (Dean’s Research Grant CoE-NIU 2017–2018).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that there is no conflict of interest.
Statement of human and animal rights
All procedures performed in this cross-sectional study involving human participants were in accordance with the ethical standards of the Northern Illinois University Institutional Review Board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from alll participants included in the study prior data collection.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sebastião, E. Activity behavior and cognitive performance in older adults living in a senior housing facility: the impact of frailty status. Aging Clin Exp Res 32, 703–709 (2020). https://doi.org/10.1007/s40520-019-01254-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01254-y