Abstract
Purpose
To examine implications of the COVID-19 pandemic on eating disorder (ED) features and psychopathology in female adolescents with anorexia nervosa (AN).
Method
In total 79 females with first-onset AN (aged 12–22 years) were included and were followed up across a period of 1 year. We assessed AN participants recruited pre-pandemic (n = 49) to those recruited peri-pandemic (n = 30). Pre- (n = 37) and peri-pandemic (n = 38) age-, and education-matched typically developing (TD) girls (n = 75) were used as a reference cohort. ED features and psychopathology were assessed at baseline. After 1 year of follow-up the association between pandemic timing and clinical course was assessed. Analyses of covariance were used to examine differences in ED features and psychopathology.
Results
Peri-pandemic AN participants experienced less ED symptoms at baseline compared to pre-pandemic AN participants. In particular, they were less dissatisfied with their body shape, and experienced less interpersonal insecurity. In addition, the peri-pandemic AN group met fewer DSM-IV criteria for comorbid disorders, especially anxiety disorders. In contrast, peri-pandemic AN participants had a smaller BMI increase over time. In TD girls, there were no differences at baseline in ED features and psychopathology between the pre- and peri-pandemic group.
Conclusion
Overall, peri-pandemic AN participants were less severely ill, compared to pre-pandemic AN participants, which may be explained by less social pressure and peer contact, and a more protective parenting style during the pandemic. Conversely, peri-pandemic AN participants had a less favorable clinical course, which may be explained by reduced access to health care facilities during the pandemic.
Level of evidence
Level III: Evidence obtained from well-designed cohort or case–control analytic studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anorexia nervosa (AN) is a life-threatening mental disorder characterized by an extremely low body weight, a distorted body image and an intense fear to gain weight [1]. The onset of AN is often during adolescence and its lifetime prevalence is around 1–4% in women and 0.2–0.3% in men [2, 3]. AN is challenging to treat and the often long road to recovery focuses on weight restoration and psychotherapy [4]. Several risk factors have been identified, including psychosocial factors such as stressful life events which not only influence the susceptibility to develop an eating disorder (ED), but also have implications for the course of the disease, i.e., severity and duration [5]. A recent example of a traumatic stressor is the COVID-19 pandemic, which had a major impact on the mental health of the global community [6, 7]. To limit the transmission of the virus, governments implemented extensive measures, including social distancing, closure of non-essential services, and limitations in social interactions [8]. The mental health of adolescents was a main concern during the pandemic [9, 10], since adolescence is a formative period for socio-emotional, cognitive and coping skills development [11]. Therefore, adolescents with AN especially may have been extra vulnerable and susceptible to the harmful effects of the pandemic [12].
Since the onset of the COVID-19 pandemic, an increase of 15% in ED presentations [13], 83% in pediatric ED hospital admissions and 16% in adult admissions [14] has been reported. Despite the relatively larger increase in pediatric admissions, previous studies have mainly focused on adults who had been diagnosed with AN prior to the pandemic. Overall, these studies showed mixed results [12, 14, 15]. Some studies found a worsening of ED symptoms [16,17,18,19], and increased levels of depression- and anxiety symptoms [17, 20, 21], while others showed an improvement in ED symptoms, more social support, and more time for self-reflection in the pandemic period compared to pre-pandemic [22,23,24,25,26]. Springall et al. [27] conducted in adolescents, a large retrospective chart review from 2017 to 2020 of all individuals with AN presenting to a children’s hospital, with respect to hospitalization outcomes, body mass index (BMI), and comorbid psychopathology. Despite the increase in ED presentations peri-pandemic, they found no year-over-year differences in disorder severity. Other studies comparing pre-pandemic and peri-pandemic adolescent AN cohorts have shown conflicting results. One cross-sectional prospective study found no differences in ED symptomatology, but did find lower BMI and more compensatory over-exercising in the peri-pandemic group [28]. Another retrospective chart-review study, found no differences in BMI, but found greater medical instability and higher hospitalization rates in the peri-pandemic AN cohort compared to the pre-pandemic AN cohort [29]. Meneguzzo et al. [30] discovered that the peri-pandemic AN cohort had an increase in binge eating episodes, more difficulties with interoceptive awareness, and fewer obsessive–compulsive disorder (OCD) symptoms compared to the pre-pandemic AN cohort.
Our study addresses several knowledge gaps that may help to improve our understanding of the impact of the COVID-19 pandemic on illness severity and disease course among adolescents with first-onset clinical AN. First, previous work of Springall [27], Spettigue [29], and Meneguzzo [30] was based on a retrospective chart review in which data were not systematically collected, whereas our study extensively assessed AN participants at two timepoints (at baseline and after 1 year of follow-up) in multiple domains during face-to-face appointments using structured interviews. Second, we are the first study to examine the one-year clinical course of adolescent AN during the pandemic. Finally, we used an age-, gender- and education-matched typically developing (TD) group as a reference cohort. Our findings may be helpful in the clinical management of adolescents with AN during stressful situations such as the COVID-19 pandemic.
In this context, we aim to investigate the implications of the COVID-19 pandemic in adolescents with AN. The current study is embedded in the BRAVE study; the BRAVE study is a first-onset AN prospective longitudinal cohort study focusing on the following four research areas: (1) behavior, (2) neurobiology, (3) cognitive functions, and (4) physical health. As the onset of the COVID-19 pandemic occurred in the middle of data collection, our study provided a natural experiment in which we could examine the impact of the COVID-19 pandemic on ED features and comorbid psychopathology in a large group of adolescent females with first-onset AN.
We hypothesized that AN participants enrolled peri-pandemic would have more severe ED, i.e., a lower BMI and more ED symptoms, and experience more psychopathology compared to AN participants enrolled pre-pandemic. We expected that TD girls enrolled peri-pandemic would experience more ED symptoms and psychopathology, albeit at a subclinical level, compared to TD girls enrolled pre-pandemic. Second, to examine the effect of the COVID-19 pandemic on the one-year disease course, we examined the longitudinal association between ED features and the timing of the pandemic during the one-year follow-up period, i.e., both the pre-pandemic and peri-pandemic time-periods.
Materials and methods
Participants
The sample consisted of a total of 154 female adolescents: 79 participants with first-onset AN and 75 TD girls. AN inclusion criteria included: female gender, aged 12–22 years, diagnosed with first-onset AN or atypical AN according to DSM-5 criteria. The onset of the DSM-5 diagnosis of AN should be within 12 months of the date of inclusion. AN participants were recruited from 16 mental health institutions and hospitals in the Netherlands via the providers. In addition, they were recruited via advertisements on social media and through patient organizations.
An age-, gender-, and education-matched TD group was also included. To be included, TD girls were required to have a healthy body weight, defined as a body mass index—standard deviation score (BMI-SDS) between − 1.3 and + 1.3. TD girls were recruited via advertisements on social media, sport clubs or via AN participants (e.g., classmates, friends). Exclusion criteria for both the AN and TD group were presence of a psychotic-, neurologic-, or a substance abuse disorder, severe motor and sensory disturbances, IQ < 70 measured by an intelligence test, and insufficient Dutch language skills.
Study design
The study was conducted between May 2017 and January 2023. The study had a longitudinal design with identical measurements performed at baseline (T1) and after 1 year of follow-up (T2). As previous studies have shown that the COVID-19 restrictions in particular have had a major impact on people’s lives [31,32,33], the cut-off point (pre- versus peri-pandemic) in this study was set at the 15th of March, 2020, the date on which the Dutch government announced the first major restrictions.
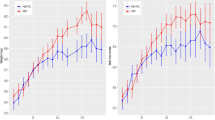
ED features and psychopathology at T1 were compared between separate groups: a pre-pandemic cohort (assessed between 3/5/2017 and 15/3/2020) and a peri-pandemic cohort (assessed between 16/3/2020 and 14/10/2021). The AN group consisted of 49 participants enrolled pre-pandemically and 30 participants enrolled peri-pandemically. The TD group consisted of, respectively, 38 participants enrolled pre- and 37 enrolled peri-pandemically. T2 data were available for 72% (n = 57) of AN participants and 88% (n = 66) of TD girls. To explore the longitudinal association between timing of the pandemic and ED features, we compared three groups: (1) Pre-pandemic cohort (AN, n = 19; TD, n = 12), in which all data were collected pre-pandemically; (2) pre/peri-pandemic cohort (AN, n = 21, TD, n = 22), in which inclusion was pre-pandemic and 1-year follow-up occurred peri-pandemically; (3) peri-pandemic cohort (AN, n = 17; TD, n = 32), in which all data were collected peri-pandemically (Fig. 1a and b).
a Overview of pre-pandemic, pre/peri-pandemic, and peri-pandemic AN participants. AN: anorexia nervosa. Each line represents the trajectory of each individual AN participant in the BRAVE study. b Overview of pre-pandemic, pre/peri-pandemic, and peri-pandemic TD girls. TD: typically developing. Each line represents the trajectory of each individual TD participant in the BRAVE study
Procedure
The eligibility of adolescents who were interested in participating in our study was assessed by screening inclusion and exclusion criteria by telephone. After the screening, potential participants were provided information about the study and were contacted again 2 weeks later to answer any remaining questions. If the adolescent wished to participate, a consent meeting was scheduled to obtain informed consent and verify eligibility. For both the TD and AN groups, we assessed inclusion and exclusion criteria by using the Mini International Neuropsychiatric Interview (MINI)-KID/PLUS to check for psychotic disorders and substance-related disorders. For the AN participants, DSM-5 criteria for AN were evaluated, and interviews/questionnaires were administered focusing on the following research domains: (1) behavior, (2) neurobiology, (3) cognitive functions, and (4) physical health. Two visits at the Erasmus MC-Sophia Children’s Hospital were planned in random order. During one visit neuropsychological assessments, including intelligence tests and cognitive tasks, were administered. During the second visit, mental health measures were obtained. Participants also completed online questionnaires that included ED-related questionnaires, sociodemographic information, and psychopathology related questionnaires. Between T1 and T2 AN participants received treatment as usual. To determine eligibility for TD girls, we assessed their height and body weight to ensure they met the criteria for a healthy weight. Additionally, we screened them for the presence of eating disorders. Our aim was to include a control group that accurately represents the general population in terms of the prevalence of psychopathology. TD girls underwent the same procedure as AN participants.
Materials
Primary outcomes
BMI-SDS. BMI was corrected for age and gender to obtain an adjusted BMI (BMI-SDS), using a growth calculator tool (https://groeiweb.pgdata.nl/calculator.asp).
ED symptomatology. The Eating Disorder Examination version 12.0 (EDE) is considered the gold standard for assessing ED psychopathology [34], consisting of four subscales (rated on a 7-point Likert scale): dietary concerns, food concerns, body weight concerns and body shape concerns. The internal consistency of the global score was high (α = 0.92) [35].
In addition, ED symptoms were assessed using the Eating Disorder Inventory, version 3 (EDI-3) [36], a self-report questionnaire consisting of 91 items, each rated on a 4-point Likert scale spanning 12 subscales. Higher scores indicate an increased risk of having or developing an ED. The EDI questionnaire demonstrates high internal consistency, with a range above α = 0.80 [37].
Body shape concerns. The Body Shape Questionnaire (BSQ) is a self-report questionnaire that was used to assess body shape concerns typical for ED symptoms in the prior 4 weeks [38]. The BSQ consists of 34 items scored on a 6-point Likert scale. Higher scores indicate greater perceived body shape dissatisfaction. The internal consistency among adolescents is high (α = 0.97) [39].
Physical exercise. Time spent on physical exercise during a typical week was recorded, divided into high and low intensity. High-intensity physical exercise was defined as vigorous activity (e.g., running, swimming). Low-intensity physical exercise was low impact (e.g., walking, yoga).
Hand grip strength. Muscle strength was measured using a hand grip instrument (JAMAR®-plus + Digital Hand Dynamometer) set to kg; averaged over three trials.
Arm circumference, averaged over both upper arms.
Secondary outcomes
General psychopathology. The Mini International Neuropsychiatric Interview (MINI-KID (< 17 years) /MINI-PLUS (> 18 years) is a structured interview used to assess general psychopathology based on DSM-IV criteria. The MINI-KID/MINI-PLUS based on DSM-5 criteria was not available at the start of our study. Test–retest kappa (k = 0.76–0.93) and the specificity for all diagnoses (range 0.72–0.92) is moderate–high [40].
Depression. The Beck Depression Inventory-Second Edition (BDI-II) was used to measure severity of depressive symptoms using statements reflecting mood symptoms within the past week [41], consisting of 21 items, rated on a 4-point Likert scale. A score of 0–20 points indicates ‘no or minimal depression’, a score of 21–30 ‘moderate depression’, a score of 31–40 ‘severe depression’ and a score of 41–63 ‘very severe depression’. The internal consistency is high (α = 0.9) and the test–retest reliability is moderate–high (range 0.73–0.96) [42].
Anxiety. The Screening for Child Anxiety Related Emotional Disorders (SCARED) assessed anxiety symptoms using DSM-IV-TR criteria [43]. The SCARED consists of 69 items scored on a 3-point Likert scale. Scores above 25 were considered indicative of an anxiety disorder [44]. Internal consistency is moderate–high (α = 0.74–0.93) [45].
Obsessive–compulsive disorder (OCD). The (Children’s Yale-Brown Obsessive–Compulsive Scales ((C)Y-BOCS) questionnaire assesses obsessive–compulsive thoughts and behaviors [46]. The CY-BOCS was administered to ages 12–17 year olds and the Y-BOCS to 18–22 year olds. This questionnaire consists of 10 items, scored on a 5-point Likert scale. The Y-BOCS has a high internal consistency (α = 0.87) [47].
Autism. The Social Responsiveness Scale (SRS) assesses autistic traits [48]. The SRS-2 was completed by parents in participants aged 12–17 years; the SRS-A was used in participants aged 18–22 years. The internal consistency of the SRS-2 is high (α = 0.91) and the interrater reliability ranging between α = 0.76 and α = 0.95 [48]. The internal consistency of the SRS-A is also high (α = 0.89) in adults with autism spectrum disorder (ASD) and moderate (α = 0.71) in TD adults [49].
Intelligence. Intelligence was assessed using the Wechsler Abbreviated Scale of Intelligence-Second Edition (WASI-II) [50]. The resulting Full Scale Intelligence Quotient (FSIQ) provides a reliable estimate of cognitive functioning [51]. The internal consistency is high (α = 0.87–0.91) [50].
Covariates
Age and socioeconomic status (SES) were considered as covariates. The SES was based on the education of the mother. Maternal education was divided into: low (primary education and lower general secondary education), middle (higher general secondary education), and high (higher vocational secondary education or University degree).
Statistical analyses
Data analyses were performed using SPSS Statistics (version 28.0, IBM Corporation, Armonk, NY, USA). Effect sizes were reported as partial eta squared (η2p), with 0.01 indicating a small effect size, 0.06 a medium effect size and 0.14 a large effect size [52].
Cross-sectional analyses
Sociodemographic variables were analyzed using a 2-sided independent Student’s t-test or a Mann–Whitney U test for non-parametric data. Separate analyses were performed for the AN and TD groups. A Kruskal–Wallis one-way ANOVA was used to compare group differences in ethnicity, SES and recruitment method.
For comparisons between AN participants, pre-pandemic and peri-pandemic measures of emotional dysregulation (EDI subscale) and physical exercise were log-transformed to approximate a normal distribution. For the analyses within the TD group, measures of ED symptomatology (EDE and EDI scores), body shape satisfaction (BSQ), obsessive–compulsive symptoms (Y-BOCS), and physical exercise were log-transformed to approximate a normal distribution. Comparisons between ED features and psychopathology symptoms were made using one-way analyses of covariance (ANCOVA), corrected for age and SES. The independent variable was group (pre- vs. peri-pandemic) and the dependent variables were ED features and comorbid psychiatric symptoms. Comparisons between number of DSM-IV diagnoses were analyzed using Pearson Chi-square tests.
In addition, we performed a double subtraction analysis in order to perform a case–control comparison of pre- versus peri-pandemic. For both pre- and peri-pandemic analyses measures of ED—(EDE), OCD—(Y-BOCS), ASD symptoms (SRS-2/SRS-A), and physical exercise were log-transformed in order to approximate a normal distribution. We performed multiple ANCOVAs to test for differences between ED features and comorbid psychopathology between AN and TD participants both pre- and peri-pandemic. Group differences in the number of DSM-IV diagnoses were carried out using Pearson Chi-squared tests. Correction for multiple testing was performed by controlling for false discovery rate (FDR) at a q-value of 0.05.
Longitudinal analyses
To examine the longitudinal association between ED features and pandemic timing (pre-pandemic vs. peri-pandemic), we calculated a mean difference score between T1 and T2 for the pre-pandemic, pre/peri-pandemic and peri-pandemic cohorts. Longitudinal comparisons for the main clinical outcomes (BMI-SDS and ED symptomatology), were performed using ANCOVAs adjusted for age, SES, follow-up time, and baseline BMI-SDS and EDE scores, respectively. Post hoc analyses were performed to assess differences in the course of ED features between the pre-pandemic, pre/peri-pandemic, and peri-pandemic subgroups.
Non-response analyses
AN and TD participants with missing data at follow-up were compared with participants with available follow-up data on age, SES, ED symptoms and BMI-SDS.
Results
Sample characteristics
Sociodemographic characteristics are shown in Table 1. The SES of peri-pandemic AN participants was higher compared to pre-pandemic AN participants (p < 0.05). There were no differences in age, ethnicity, IQ, and duration of illness between pre- and peri-pandemic AN participants. All pre-pandemic AN participants (100%) were recruited via health care providers, whereas 60% of the peri-pandemic AN participants were recruited through their health care providers (n = 18). The remainder were recruited via social media 33.3% (n = 10) or via flyers and other means 2.7% (n = 2). Of note, ED features and comorbid psychopathology did not differ between peri-pandemic recruitment methods (Supplemental Table 1). There were no differences in age, ethnicity, SES, and IQ between TD girls enrolled pre- and peri-pandemic. In the non-response analyses, AN participants with missing follow-up data (n = 22) were compared with AN participants with available follow-up data (n = 57). AN participants with missing data at follow-up had less severe ED symptoms at baseline compared to AN participants for whom data were available (p = 0.04). Pre- and peri-pandemic AN participants did not differ in age and SES. TD participants with missing data at follow-up (n = 8) were compared with TD participants for whom follow-up data were available (n = 67). There was no selective drop-out based on age, SES, ED symptoms and BMI-SDS.
Cross-sectional baseline comparisons of ED features and comorbid psychopathology pre-pandemic and peri-pandemic
Case–case comparisons
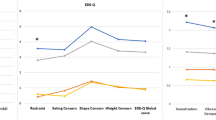
AN participants recruited peri-pandemic reported fewer ED symptoms at enrollment, as assessed by the EDE compared to AN participants recruited pre-pandemic (p = < 0.001). Further EDE analyses revealed that peri-pandemic AN participants experienced fewer dietary concerns (p = 0.007), food concerns (p = 0.005), body weight concerns (p = 0.009), and body shape concerns (p = < 0.001) compared to pre-pandemic AN participants (Tables 2 and 3, Fig. 2). The effect sizes of these findings were moderate to large (η2p 0.10–0.17). Peri-pandemic AN participants experienced less interpersonal insecurity (EDI-3 subscale Interpersonal insecurity: p = 0.001), and reported being less dissatisfied with their body shape (EDI-3 subscale Body dissatisfaction: p = 0.007) in comparison with pre-pandemic AN participants. The effect sizes were moderate to large (η2p 0.11–0.15). AN participants included peri-pandemic had less hand grip strength (p = 0.034) and a lower arm circumference (p = 0.032) than AN participants included pre-pandemic, although this finding was no longer significant after multiple-testing correction. There was no difference in BMI-SDS between AN participants included pre- and peri-pandemic. AN participants recruited peri-pandemic fulfilled less DSM-IV classifications compared to AN participants recruited pre-pandemic ((X2) = 13.29, df = 5, p < 0.021) (Supplemental Fig. 1), primarily driven by less classifications for anxiety disorders ((X2) = 21.72, df = 1, p < 0.001; Supplemental Table 3). There were no differences in depression-, anxiety-, OCD- and ASD symptoms between AN participants included pre- and peri-pandemic.
Control–control comparisons
Peri-pandemic TD girls perceived less maturity fears (EDI-3 scale Maturity fears: p = 0.004) than pre-pandemic TD girls, although no longer significant after multiple-testing correction. There were no other differences in ED features and in depression-, anxiety-, OCD- and ASD symptoms between TD girls included pre- and peri-pandemic (Table 4).
Case–control comparisons
AN participants had a lower BMI-SDS, arm-circumference, EDE-, EDI-, and BSQ-score compared to TD girls, both pre- and peri-pandemic (p < 0.05, Supplemental Table S).
Pre- and peri-pandemic, AN participants had higher depression-, anxiety-, and ASD symptoms compared to TD girls (p < 0.05). Pre-pandemic, AN participants displayed significantly more OCD symptoms than TD girls, similar to peri-pandemic although this difference was no longer significant due to a slight increase in OCD symptoms in TD girls peri-pandemic.
Longitudinal association between ED features and timing of the pandemic during the one-year follow-up period
Case–case comparisons
Within the AN group, the peri-pandemic group had a lower BMI-SDS increase between baseline and follow-up compared to the pre-pandemic AN group and the pre/peri-pandemic AN group (p = 0.028) (Fig. 3, Table 5). There were no significant between-group differences in ED symptoms over time.
Control–control comparisons
Within the TD group there were no significant between-group differences in ED features over time.
Discussion
We examined cross-sectional differences in ED features and comorbid psychopathology among adolescents with AN enrolled in our BRAVE study before and during the pandemic. In addition, we assessed the association between pandemic timing and 1-year clinical outcome. Peri-pandemic AN participants had fewer ED symptoms, were less dissatisfied with their body shape, and perceived less interpersonal insecurity compared to pre-pandemic AN participants. In addition, peri-pandemic AN participants fulfilled less DSM-IV criteria for comorbid disorders, in particular less anxiety disorders compared to pre-pandemic AN participants. Conversely, longitudinal analyses showed that the AN peri-pandemic group had a lower increase in BMI after 1-year follow-up compared to the AN pre-pandemic group. Among the reference group, TD girls, there were no significant differences in ED features and psychopathology between pre- and peri-pandemic TD girls.
ED features
Interestingly, peri-pandemic AN participants reported less severe general ED symptomatology, perceived less concerns about diet, body weight and body shape compared to pre-pandemic AN participants. This appears to be in contrast with previous literature with a comparable case–case study design which showed either an increase in binge eating episodes [30] a trend towards more food restraint [29], or no significant differences in ED symptoms [28] among adolescents with an ED peri-pandemic versus pre-pandemic. The observed discrepancy could be explained by differences between the respective populations, e.g., age, severity of illness, duration of illness, specific time period during the pandemic, or differences in COVID-19 regulations imposed by different governments in response to the pandemic. The retrospective chart review by Spettigue et al. [29] studied a population with different types of EDs at high risk of medical complications, whereas we studied prospectively a patient group at different stages of illness. In addition, the current study collected data during a more extensive period during the pandemic (March 2020–October 2021), while previous studies [28, 29] collected data during a relatively short period during the pandemic (6–9 months). The study by Meneguzzo [30] conducted a study on a patient population that was relatively comparable to ours. However, their patient population had a slightly longer disease duration and their study was conducted in another country with different COVID-19-related restrictions at that specific time point. It is hypothesized that the interaction between imposed restrictions, coping strategies, and the presence of risk factors (i.e., fear of contagion, feeling of increased isolation) and resilience factors (more family cohesion, less social pressure) [53] contributed significantly to the symptom presentation of AN and may explain the differential findings. Two other studies conducted in both adolescent and adult inpatients with an ED [54, 55] using a similar case–case design also demonstrated higher levels of ED symptoms and psychopathology in the peri-pandemic ED cohort compared to the pre-pandemic ED cohort. As these studies did not differentiate between adolescents and adults, and were conducted in inpatients with different types of ED, they were not directly comparable to our study.
Another finding is that peri-pandemic AN participants were less insecure during social interactions compared to pre-pandemic AN participants. Possibly, reduced social interactions with peers might have a positive impact on social insecurity among adolescents with AN, since peer relationships could contribute to the disorder’s persistence [56]. Moreover, virtual social interactions, in which one sees only someone's face instead of their whole body, were predominant during the COVID-19 pandemic. This may be less confronting for participants with AN and potentially beneficial for their ED symptoms [56]. Additionally, during the COVID-19 pandemic AN participants were more in their home environment because of school closure and had more interactions with their parents, which has the potential to create a more protective environment and facilitate earlier detection of an ED [57, 58]. Strong parent–child relationships are linked to social competence [59], and the quality of friendships [60], potentially leading to a decrease in interpersonal insecurity.
BMI-SDS and physical exercise did not differ between the pre- and peri-pandemic AN group, which contradicts the findings of Datta et al. [28] where peri-pandemic AN participants had a lower BMI and increased over-exercising. Interestingly, our study reveals that peri-pandemic AN participants had less hand grip strength and a lower arm circumference compared to pre-pandemic AN participants. Although these findings lost significance after multiple-testing correction. In addition to BMI-SDS, arm circumference and hand grip strength are considered as markers of nutritional status [61,62,63,64]. It is speculated that arm circumference and hand grip strength may be more effective than BMI-SDS in detecting subtle differences, suggesting that peri-pandemic AN participants experienced poorer nutritional status compared to those included pre-pandemic. Furthermore, peri-pandemic AN participants had less weight gain after 1 year of follow-up compared to pre-pandemic AN participants. It is possible that decreased accessibility of health care facilities peri-pandemic [24] or the slightly higher body weight of the peri-pandemic group at baseline resulted in less catch-up in weight.
Peri-pandemic TD girls had lower perceptions of fear towards maturity compared to pre-pandemic TD girls. However, this effect ceased to be significant after multiple-testing correction. No other cross-sectional differences in ED symptoms were observed between the pre- and peri-pandemic TD groups. This finding is not in line with the increased prevalence of EDs within the general population during the pandemic [65, 66]. Our findings suggest that TD girls experienced less social pressure [67], and increased family cohesion during the peri-pandemic period, potentially protecting against the emergence of psychopathology [68].
Comorbid psychopathology
Peri-pandemic AN participants fulfilled fewer DSM-IV classifications compared to pre-pandemic AN participants, primarily due to fewer anxiety disorder classifications. Remarkably, psychopathology symptoms did not significantly differ between pre- and peri-pandemic AN participants, consistent with Springall et al. findings [27]. One potential explanation for the divergence in psychopathology classifications and symptoms is that peri-pandemic AN participants may have experienced fewer anxiety-inducing situations, such as reduced physical gatherings, and less crowding in public. As a result, their daily lives may have been less impacted by anxious feelings, resulting in fewer DSM-IV anxiety disorder classifications.
Strengths and limits
The study's strengths involve the application of objective measures alongside self-report data, as well as the use of a longitudinal design and a matched reference group in terms of age, gender, and education. Additionally, the emergence of the COVID-19 pandemic amidst our data collection allowed for analysis of the pandemic’s impact on illness severity upon presentation and disease progression in adolescent AN.
There may be limitations due to our extensive test battery, which could result in a possible absence of severe AN cases, as participants must be psychically and mentally capable of taking part in our study The number of measures and statistical analyses performed increased the probability of Type I errors, therefore a correction for multiple testing (i.e., Benjamini–Hochberg adjustment) was applied to reduce the risk of false-positive results. Another limitation of this study is the relatively high drop-out rate during follow-up in the AN group compared to the TD group. Although this drop-out rate is consistent with those reported in other longitudinal studies on AN [69], it may have influenced the results. It is unclear whether the patients who dropped out had a more favorable or more severe disease course compared to those with available follow-up data. We anticipate that this effect will be insignificant since we found no differences in sociodemographic and clinical variables between AN participants with and without follow-up data at the time of inclusion. Additionally, since our study only consisted of participants with AN, we cannot draw conclusions for other EDs. Lastly, there were slight differences in recruitment methods for AN participants between pre- and peri-pandemic periods, with fewer recruited through their healthcare providers during the latter. This could be attributed to the shift from in-person appointments to teleconsultations, and longer waiting lists of specialized services for eating disorders. The pandemic has resulted in greater reliance on social media advertising for recruitment. It is noteworthy that most participants recruited via social media received care through mental health institutions within our collaborative network. Furthermore, there were no significant differences in ED features, psychopathology, and duration of illness among participants enrolled through their healthcare provider and those recruited through social media during the peri-pandemic period, indicating minimal selection bias.
Conclusion
In conclusion, this study shows that adolescents with AN enrolled peri-pandemic had fewer ED symptoms, were less dissatisfied with their body shape, perceived less interpersonal insecurity, and fulfilled fewer DSM-IV criteria for comorbid psychiatric disorders, compared to AN participants enrolled pre-pandemic. At the same time, there were no cross-sectional differences in ED features and psychopathology between pre-pandemic and peri-pandemic TD girls. The exploratory analyses showed that the peri-pandemic AN group gained less weight over time, compared to the pre-pandemic AN group, which was possibly due to less access to mental health services in the peri-pandemic period. Mental health services should be aware of a less favorable clinical course under stressful conditions such as the COVID-19 pandemic. Our findings are important for the clinical management of AN patients, by increasing awareness of the effects of the pandemic on ED features, psychopathology, and the course of the disease. Future studies are needed not only to replicate our findings, but also to investigate the mechanisms by which the COVID-19 pandemic affected the physical and mental health of adolescents with peri-pandemic diagnosed AN. Furthermore, our study indicates the need for careful interpretation of scientific results based on peri-pandemic conditions, as we have shown that pre- and peri-pandemic enrolled AN groups are not directly comparable. Therefore, we recommend studies that enrolled participants both during the pandemic and before or after the pandemic take into account the timing of the pandemic.
What is already known on this subject?
There has been a rapid increase in ED presentations since the onset of the COVID-19 pandemic. Studies focusing on the impact of the COVID-19 pandemic on the behavior and mental health of individuals with AN have shown mixed results. While some studies found a worsening of ED symptoms and increased levels of psychopathology, others showed an improvement in ED symptoms possibly due to less peer pressure and more time for self-reflection during the pandemic period compared to before the pandemic. To date, there has been a great deal of heterogeneity in the methodological approaches used in previous studies, which makes comparability between studies difficult. In particular, age and disease stage may influence the severity of ED symptoms, comorbid psychopathology, and the way in which individuals perceive the pandemic [70]. To date, most studies have focused on adults with long-standing ED, while few studies have focused on young people with a short-lived illness. In the BRAVE study, we assessed a subset of people with first-onset AN at different stages of the disease who were physically and mentally able to participate in the study. Therefore, our findings cannot be extrapolated to all people with ED.
What this study adds?
This study shows that adolescents with first-onset AN recruited during the COVID-19 pandemic had less severe ED symptoms and comorbidity at baseline than those recruited before the pandemic. However, AN participants recruited during the pandemic had less weight gain at 1-year follow-up. While most studies have not systematically collected data, our study comprehensively assessed AN participants in multiple domains during face-to-face appointments at two timepoints, allowing us to assess the clinical course over one year. Furthermore, we used an age-, gender-, and education-matched control group as a reference. Our results underline the importance of addressing the impact that the COVID-19 pandemic has had on AN patients, as well as improving patient management by highlighting the differences in clinical features between pre- and peri-pandemic first-onset AN patients. Moreover, our study contributes to the careful interpretation of research carried out in this area during the COVID-19 pandemic.
Data availability
Data access and requests for collaboration are welcome, and will be conducted in accordance with the European Union's General Data Protection Regulation (GDPR).
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders. Arlington, American Psychiatric Association
Galmiche M et al (2019) Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am J Clin Nutr 109(5):1402–1413
Bulik CM et al (2006) Prevalence, heritability, and prospective risk factors for anorexia nervosa. Arch Gen Psychiatry 63(3):305–312
Bulik CM (2014) The challenges of treating anorexia nervosa. Lancet 383(9912):105–106
Brewerton TD (2007) Eating disorders, trauma, and comorbidity: focus on PTSD. Eat Disord 15(4):285–304
Cui J et al (2022) COVID-19 impact on mental health. BMC Med Res Methodol 22(1):15
Gloster AT et al (2020) Impact of COVID-19 pandemic on mental health: an international study. PLoS ONE 15(12):e0244809
Nicola M et al (2020) The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg 78:185–193
Katzman DK (2021) The COVID-19 pandemic and eating disorders: a wake-up call for the future of eating disorders among adolescents and young adults. J Adolesc Health 69(4):535–537
Solmi F, Downs JL, Nicholls DE (2021) COVID-19 and eating disorders in young people. Lancet Child Adolesc Health 5(5):316–318
Tetzner J, Becker M, Maaz K (2017) Development in multiple areas of life in adolescence: interrelations between academic achievement, perceived peer acceptance, and self-esteem. Int J Behav Dev 41(6):704–713
McLean CP, Utpala R, Sharp G (2022) The impacts of COVID-19 on eating disorders and disordered eating: a mixed studies systematic review and implications. Front Psychol 13:926709
Taquet M et al (2021) Incidence and outcomes of eating disorders during the COVID-19 pandemic. Br J Psychiatry 220(5):1–3
Devoe JD et al (2022) The impact of the COVID-19 pandemic on eating disorders: a systematic review. Int J Eat Disord 56(1):5–25
Meier K, van Hoeken D, Hoek HW (2022) Review of the unprecedented impact of the COVID-19 pandemic on the occurrence of eating disorders. Curr Opin Psychiatry 35(6):353–361
Brown S et al (2021) A qualitative exploration of the impact of COVID-19 on individuals with eating disorders in the UK. Appetite 156:104977
Monteleone AM et al (2021) The impact of COVID-19 lockdown and of the following “re-opening” period on specific and general psychopathology in people with Eating Disorders: the emergent role of internalizing symptoms. J Affect Disord 285:77–83
McCombie C et al (2020) “Now It’s Just Old Habits and Misery”-understanding the impact of the Covid-19 pandemic on people with current or life-time eating disorders: a qualitative study. Front Psychiatry 11:589225
Nistico V et al (2021) The psychological impact of COVID-19-related lockdown measures among a sample of Italian patients with eating disorders: a preliminary longitudinal study. Eat Weight Disord 26(8):2771–2777
Birgegard A et al (2021) Longitudinal experiences and impact of the COVID-19 pandemic among people with past or current eating disorders in Sweden. Eat Disord 30:1–16
Favreau M et al (2021) Psychological consequences and differential impact of the COVID-19 pandemic in patients with mental disorders. Psychiatry Res 302:114045
Branley-Bell D, Talbot CV (2020) Exploring the impact of the COVID-19 pandemic and UK lockdown on individuals with experience of eating disorders. J Eat Disord 8:44
Frayn M, Fojtu C, Juarascio A (2021) COVID-19 and binge eating: patient perceptions of eating disorder symptoms, tele-therapy, and treatment implications. Curr Psychol 40(12):6249–6258
Termorshuizen JD et al (2020) Early impact of COVID-19 on individuals with self-reported eating disorders: a survey of ~1,000 individuals in the United States and the Netherlands. Int J Eat Disord 53(11):1780–1790
Castellini G et al (2020) The impact of COVID-19 epidemic on eating disorders: a longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. Int J Eat Disord 53(11):1855–1862
Giel KE et al (2021) Eating behaviour and symptom trajectories in patients with a history of binge eating disorder during COVID-19 pandemic. Eur Eat Disord Rev 29(4):657–662
Springall G et al (2022) Impact of the coronavirus pandemic on anorexia nervosa and atypical anorexia nervosa presentations to an Australian tertiary paediatric hospital. J Paediatr Child Health 58(3):491–496
Datta N et al (2022) The COVID-19 pandemic and youth with anorexia nervosa: a retrospective comparative cohort design. Int J Eat Disord 56:263–268
Spettigue W et al (2021) The impact of COVID-19 on adolescents with eating disorders: a cohort study. J Eat Disord 9(1):65
Meneguzzo P et al (2023) The psychological and medical landscape of anorexia nervosa over a decade: a retrospective study of possible physical and psychological shifts. J Clin Med 12(23):7294
Muth L et al (2022) Effects of the COVID-19 restrictions on eating behaviour and eating disorder symptomology in female adolescents. Int J Environ Res Public Health 19(14):8480
Gao YQ, Bagheri N, Furuya-Kanamori L (2022) Has the COVID-19 pandemic lockdown worsened eating disorders symptoms among patients with eating disorders? A systematic review. J Public Health-Heidelberg 30(11):2743–2752
Monthuy-Blanc J, Corno G, Abou Chabake S (2023) Exploring the impact of the COVID-19 pandemic on perceptual disturbances and dysfunctional eating attitudes and behaviors: a review of the literature. Front Psychol 14:1139261
Guest T (2000) Using the eating disorder examination in the assessment of bulimia and anorexia: issues of reliability and validity. Soc Work Health Care 31(4):71–83
de Vos JA et al (2018) Having an eating disorder and still being able to flourish? Examination of pathological symptoms and well-being as two continua of mental health in a clinical sample. Front Psychol 9:2145
Clausen L et al (2011) Validating the eating disorder inventory-3 (EDI-3): a comparison between 561 female eating disorders patients and 878 females from the general population. J Psychopathol Behav Assess 33(1):101–110
Cumella E (2006) Review of the eating disorder inventory–3. J Pers Assess 87:116–117
Cooper PJ et al (1987) The development and validation of the body shape questionnaire. Int J Eat Disord 6(4):485–494
Di Pietro M, Silveira DX (2009) Internal validity, dimensionality and performance of the Body Shape Questionnaire in a group of Brazilian college students. Braz J Psychiatry 31(1):21–24
Lecrubier Y et al (1997) The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry 12(5):224–231
Beck A, Steer RA, Brown GK. Beck Depression Inventory Manual 1996, The Psychological Corporation San Antonio, TX.
Wang YP, Gorenstein C (2013) Psychometric properties of the Beck Depression Inventory-II: a comprehensive review. Braz J Psychiatry 35(4):416–431
Muris P et al (1998) The Screen for Child Anxiety Related Emotional Disorders (SCARED) and traditional childhood anxiety measures. J Behav Ther Exp Psychiatry 29(4):327–339
Caporino NE et al (2017) Establishing clinical cutoffs for response and remission on the screen for child anxiety related emotional disorders (SCARED). J Am Acad Child Adolesc Psychiatry 56(8):696–702
Birmaher B et al (1997) The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry 36(4):545–553
Goodman WK et al (1989) The Yale-brown Obsessive Compulsive Scale. 1. Development, use, and reliability. Arch General Psychiatry 46(11):1006–1011
Scahill L et al (1997) Children’s Yale-Brown Obsessive Compulsive Scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 36(6):844–852
Bolte S, Poustka F, Constantino JN (2008) Assessing autistic traits: cross-cultural validation of the social responsiveness scale (SRS). Autism Res 1(6):354–363
Bölte S (2012) Brief report: the social responsiveness scale for adults (SRS-A): initial results in a German cohort. J Autism Dev Disord 42(9):1998–1999
McCrimmon AW, Smith AD (2013) Wechsler abbreviated scale of intelligence, 2nd edition (WASI-II). J Psychoeduc Assess 31(3):337–341
Irby SM, Floyd RG (2013) Wechsler abbreviated scale of intelligence, second edition. Can J School Psychol 28(3):295–299
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. L. Erlbaum Associates, Mahwah
Monteleone AM et al (2021) Risk and resilience factors for specific and general psychopathology worsening in people with eating disorders during COVID-19 pandemic: a retrospective Italian multicentre study. Eat Weight Disord 26(8):2443–2452
Martini M et al (2023) Increased general, eating, and body-related psychopathology in inpatients in a specialized eating disorders unit after the beginning of the COVID-19 pandemic: a retrospective comparison with the pre-pandemic period. J Clin Med 12(2):573
Todisco P et al (2023) Preparing for the next pandemic by understanding the impact of COVID-19 mitigation measures on patients with eating disorders: observations from an inpatient setting. Int J Psychiatry Clin Pract 27(4):323–329
Lieberman M et al (2001) Interpersonal influence and disordered eating behaviors in adolescent girls: the role of peer modeling, social reinforcement, and body-related teasing. Eat Behav 2(3):215–236
Holtom-Viesel A, Allan S (2014) A systematic review of the literature on family functioning across all eating disorder diagnoses in comparison to control families. Clin Psychol Rev 34(1):29–43
Wertheim EH et al (1997) Why do adolescent girls watch their weight? An interview study examining sociocultural pressures to be thin. J Psychosom Res 42(4):345–355
McDowell DJ, Parke RD (2009) Parental correlates of children’s peer relations: an empirical test of a tripartite model. Dev Psychol 45(1):224–235
Shomaker LB, Furman W (2009) Parent-adolescent relationship qualities, internal working models, and attachment styles as predictors of adolescents’ interactions with friends. J Soc Pers Relat 26(5):579–603
Norman K et al (2011) Hand grip strength: outcome predictor and marker of nutritional status. Clin Nutr 30(2):135–142
Mitchell IM et al (1995) Nutritional status of children with congenital heart disease. Br Heart J 73(3):277–283
Smith DE, Stevens MCG, Booth IW (1991) Malnutrition at diagnosis of malignancy in childhood - common but mostly missed. Eur J Pediatr 150(5):318–322
Ansorge MS, Hen R, Gingrich JA (2007) Neurodevelopmental origins of depressive disorders. Curr Opin Pharmacol 7(1):8–17
Agostino H et al (2021) Trends in the incidence of new-onset anorexia nervosa and atypical anorexia nervosa among youth during the COVID-19 pandemic in Canada. JAMA Netw Open 4(12):e2137395
Reed J, Ort K (2022) The rise of eating disorders during COVID-19 and the impact on treatment. J Am Acad Child Adolesc Psychiatry 61(3):349–350
Dejonckheere E, Bastian B (2021) Perceiving social pressure not to feel negative is linked to a more negative self-concept. J Happiness Stud 22(2):667–679
Mendez JHM, Sanchez JPE, Becerra MIG (2020) Role of parenting styles in internalizing, externalizing, and adjustment problems in children. Salud Mental 43(2):73–84
Steinhausen HC (2002) The outcome of anorexia nervosa in the 20th century. Am J Psychiatry 159(8):1284–1293
Linardon J et al (2022) A systematic scoping review of research on COVID-19 impacts on eating disorders: a critical appraisal of the evidence and recommendations for the field. Int J Eat Disord 55(1):3–38
Acknowledgements
The authors would like to thank all the participants and their parents. The BRAVE study was conducted within the Erasmus MC-Sophia in close collaboration with Altrecht-Rintveld, Bravis Hospital, Curium-LUMC, Elisabeth-TweeSteden hospital, Emergis, Emergis-Ithaka, GGNet-Amarum, GGZ Delfland, GGZ-Rivierduinen, GGZ-WNB, Franciscus Gasthuis and Vlietland hospital, Reinier de Graaf Gasthuis, Stichting Human Concern and the Van Weel Bethesda hospital. We would like to thank all our collaboration partners for introducing the BRAVE study to the AN participants.
Funding
This study was granted by the Sophia Foundation for Scientific Research (SSWO) (Grant Numbers: S15-13, S22-65) and through financial support of an internal Erasmus MV grant of the department of Radiology and Nuclear Medicine of the Erasmus University Medical Center. The work of TW was supported in part by the Intramural Research Program from the National Institutes of Mental Health.
Author information
Authors and Affiliations
Contributions
KB and CS: conceptualization; data curation; formal analysis; methodology; visualization; writing—original draft; writing—review and editing. TvdH, RP, MBvB, AvE, MH, JH, HdJZ, LKA, FLvdS, JL, FS, CS, LvW, CW: data curation; writing—review and editing. JL, BD, PdN: conceptualization; data curation; methodology; writing—review and editing. MV and MH: conceptualization, funding acquisition, writing—review and editing. TW and GD: conceptualization, data curation, formal analysis, funding acquisition, methodology, project administration, supervision, writing—original draft, writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
None declared.
Consent to participate
Informed consent/assent was obtained from all participants and in cases where the participant was younger than 16 years, informed consent of both parents was obtained.
Ethics approval
The BRAVE study was approved by the Medical Ethical Committee of the Erasmus Medical Centre – Sophia Children’s hospital (Erasmus MC-Sophia) (MEC 2016–194/NL55175.078.16) and the study was conducted in agreement with the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bracké, K., Steegers, C., van der Harst, T. et al. The implications of the COVID-19 pandemic on eating disorder features and comorbid psychopathology among adolescents with anorexia nervosa and matched controls: a comparative cohort design study. Eat Weight Disord 29, 13 (2024). https://doi.org/10.1007/s40519-024-01640-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40519-024-01640-0