Abstract
Purpose of review
This review establishes current evidence supporting antimicrobial stewardship programs for malignant hematology and hematopoietic stem cell transplant patients. It describes best practices and identifies opportunities for research. It examines metrics relevant to the patient population, and new approaches to the management of high-risk febrile neutropenia.
Recent findings
There is an urgent need for antimicrobial stewardship programs to optimize antimicrobial use in malignant hematology and stem cell transplant patients. Audit and feedback is effective and safe. Febrile neutropenia is a key area to optimize antimicrobial use. Shortening duration of antimicrobial therapy in fever of unknown origin appears to be feasible. Routine antimicrobial prophylaxis has been reexamined. Locally developed guideline for high-risk febrile neutropenia is a major intervention. Antifungal stewardship and rapid diagnostic technologies reduce unnecessary antifungal use. Metrics for antimicrobial stewardship programs in malignant hematology and stem cell transplant are multifaceted.
Summary
Antimicrobial stewardship in the malignant hematology and stem cell transplant population is feasible, effective, and safe. Current gaps in knowledge include the optimal duration of antimicrobial use in fever of unknown origin, and the safety of targeted therapy despite neutropenia. The ideal human resources requirement is unclear. Cost-effectiveness of antimicrobial stewardship interventions remains to be determined.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
•• Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, et al. Implementing an antibiotic stewardship program: guidelines by the infectious diseases society of america and the society for healthcare epidemiology of america. Clin Infect Dis. 2016;62(10):e51–77. https://doi.org/10.1093/cid/ciw118. Current guideline.
Center for Disease Control and Prevention. Antibiotic Prescribing and Use. National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) Division of Healthcare Quality Promotion (DHQP), Atlanta, GA, USA. 2018. https://www.cdc.gov/antibiotic-use/. Accessed 7 Jan 2019.
Accreditation Canada. Required Organizational Practices Handbook 2017. Ottawa: Accreditation Canada; 2017.
•• Baur D, Gladstone BP, Burkert F, Carrara E, Foschi F, Döbele S, et al. Effect of antibiotic stewardship on the incidence of infection and colonization with antibiotic-resistant bacteria and Clostridium difficile infection: a systematic review and meta-analysis. Lancet Infect Dis. 2017;17(9):990–1001.https://doi.org/10.1016/s1473-3099(17)30325-0. Only systemic review to highlight the scarcity of data and the potential high impact of antimicrobial stewardship in oncolgy patients.
•• Abbo LM, Ariza-Heredia EJ. Antimicrobial stewardship in immunocompromised hosts. Infect Dis Clin N Am. 2014;28(2):263–79. https://doi.org/10.1016/j.idc.2014.01.008. Comprehensive overview on the challenges in antimicrobial stewardship in immunocompromised hosts.
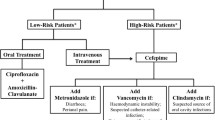
•• Averbuch D, Orasch C, Cordonnier C, Livermore DM, Mikulska M, Viscoli C, et al. European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European Conference on Infections in Leukemia. Haematologica. 2013;98(12):1826–35. An early guideline for management of high-risk febrile neutropenia that advocated for a diagnostic-driven approach with timely escalation/de-escalation strategies.
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52(4):e56–93. https://doi.org/10.1093/cid/cir073.
Donnelly JP, Blijlevens NM, van der Velden WJ. Infections in the immunocomproised host: general principles. In: Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 8th ed. Philadelphia: Elsevier Saunders; 2015. p. 3384–94e4.
•• Gyssens IC, Kern WV, Livermore DM. The role of antibiotic stewardship in limiting antibacterial resistance among hematology patients. Haematologica. 2013;98(12):1821–5. Highlights the need for antimicrobial stewardship in patients with hematological malignancies.
•• O’Neill J. Tackling drug-resistant infections globally: final report and recommendations. The reveiw on antimicrobial resistance. United Kingdom: HM Government UK 2016. Highlights the projected negative impact on mortality due to antimicrobial resistance, which is expected to surpass deaths due to cancer.
Centers for Disease Control and Prevention. US Department of Health and Human Services and the Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States 2013. 2013.http://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf. Accessed 24 July 2015.
•• Averbuch D, Tridello G, Hoek J, Mikulska M, Akan H, Yanez San Segundo L, et al. Antimicrobial resistance in Gram-negative rods causing bacteremia in hematopoietic stem cell transplant recipients: intercontinental prospective study of the infectious diseases working party of the European Bone Marrow Transplantation Group. Clin Infect Dis. 2017;65(11):1819–28.https://doi.org/10.1093/cid/cix646. Significance of antimicrobial resistnce to the stem cell transplant population.
•• Teillant A, Gandra S, Barter D, Morgan DJ, Laxminarayan R. Potential burden of antibiotic resistance on surgery and cancer chemotherapy antibiotic prophylaxis in the USA: a literature review and modeling study. Lancet Infect Dis. 2015;15(12):1429–37. https://doi.org/10.1016/s1473-3099(15)00270-4. Highlights the burden of antibiotic resistance in patients with hematological malignancies.
Baker TM, Satlin MJ. The growing threat of multidrug-resistant Gram-negative infections in patients with hematologic malignancies. Leuk Lymphoma. 2016;57(10):2245–58.https://doi.org/10.1080/10428194.2016.1193859.
•• Trecarichi EM, Pagano L, Candoni A, Pastore D, Cattaneo C, Fanci R, et al. Current epidemiology and antimicrobial resistance data for bacterial bloodstream infections in patients with hematologic malignancies: an Italian multicentre prospective survey. Clin Microbiol Infect. 2015;21(4):337–43.https://doi.org/10.1016/j.cmi.2014.11.022. Highlights the burden of antibiotic resistance in patients with hematological malignancies.
•• Satlin MJ, Walsh TJ. Multidrug-resistant Enterobacteriaceae, Pseudomonas aeruginosa, and vancomycin-resistant Enterococcus: three major threats to hematopoietic stem cell transplant recipients. Transpl Infect Dis. 2017;19(6).https://doi.org/10.1111/tid.12762. Highlights the burden of vancomycin-resistant enterococcus infections in patietns with hematological malignancies.
•• Papanicolaou GA, Ustun C, Young JH, Chen M, Kim S, Ahn KW, et al. Bloodstream infection (BSI) due to vancomycin-resistant Enterococcus (VRE) is associated with increased mortality after hematopoietic cell transplantation for acute leukemia and myelodysplastic syndrome: a multicenter, retrospective cohort study. Clin Infect Dis. 2019. https://doi.org/10.1093/cid/ciz031. Highlights the burden of vancomycin-resistant enterococcus infections in patietns with hematological malignancies.
Tsuji BT, Pogue JM, Zavascki AP, Paul M, Daikos GL, Forrest A, et al. International Consensus Guidelines for the Optimal Use of the Polymyxins. Pharmacotherapy. 2019;39(1):10–39. https://doi.org/10.1002/phar.2209.
Tamma PD, Cosgrove SE, Maragakis LL. Combination therapy for treatment of infections with gram-negative bacteria. Clin Microbiol Rev. 2012;25(3):450–70. https://doi.org/10.1128/CMR.05041-11.
Bagdasarian N, Rao K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA. 2015;313(4):398–408.https://doi.org/10.1001/jama.2014.17103.
•• Kamboj M, Son C, Cantu S, Chemaly RF, Dickman J, Dubberke E, et al. Hospital-onset Clostridium difficile infection rates in persons with cancer or hematopoietic stem cell transplant: a C3IC Network report. Infect Control Hosp Epidemiol. 2012;33(11):1162–5. https://doi.org/10.1086/668023. Highlights the burden of C. difficile infections in cancer or hematopoietic stem cell transplant patients.
•• Luo R, Greenberg A, Stone CD. Outcomes of Clostridium difficile infection in hospitalized leukemia patients: a nationwide analysis. Infect Control Hosp Epidemiol. 2015;36(7):794–801. https://doi.org/10.1017/ice.2015.54. Highlights the burden of C. difficile infections in cancer or hematopoietic stem cell transplant patients.
•• Gross AE, Johannes RS, Gupta V, Tabak YP, Srinivasan A, Bleasdale SC. The effect of a piperacillin/tazobactam shortage on antimicrobial prescribing and Clostridium difficile risk in 88 US medical centers. Clin Infect Dis. 2017;65(4):613–8. https://doi.org/10.1093/cid/cix379. Highlights the impact of antibiotic shortages on patient care.
•• Garrett K, Walker ST, Devchand M, Khumra S, Mahony AA, Trubiano JA, et al. Counting the cost of critical antibiotic shortages. J Antimicrob Chemother. 2018;74(1):273–5. https://doi.org/10.1093/jac/dky410. Highlights the impact of antibiotic shortage on patient care.
American Society of Health-Systems Pharmacists. Current Drug Shortages. American Society of Health-Systems Pharmacists. 2019. https://www.ashp.org/Drug-Shortages/Current-Shortages. Accessed 2 Feb 2019.
Theuretzbacher U, Gottwalt S, Beyer P, Butler M, Czaplewski L, Lienhardt C, et al. Analysis of the clinical antibacterial and antituberculosis pipeline. Lancet Infect Dis. 2019;19(2):e40–50. https://doi.org/10.1016/s1473-3099(18)30513-9.
•• Hakki M, Lewis JS 2nd. Ceftolozane-tazobactam therapy for multidrug-resistant Pseudomonas aeruginosa infections in patients with hematologic malignancies and hematopoietic-cell transplant recipients. Infection. 2018;46(3):431–4. https://doi.org/10.1007/s15010-018-1125-5. Highlights the risk of emerging resistance among new antibiotics.
Haidar G, Philips NJ, Shields RK, Snyder D, Cheng S, Potoski BA, et al. Ceftolozane-tazobactam for the treatment of multidrug-resistant Pseudomonas aeruginosa infections: clinical effectiveness and evolution of resistance. Clin Infect Dis. 2017;65(1):110–20. https://doi.org/10.1093/cid/cix182.
•• Elgarten CW, Arnold SD, Li Y, Huang YV, Riches ML, Gerber JS, et al. Hospital-level variability in broad-spectrum antibiotic use for children with acute leukemia undergoing hematopoietic cell transplantation. Infect Control Hosp Epidemiol. 2018;39(7):797–805. https://doi.org/10.1017/ice.2018.96. Highlights the need for resource stewardship in leukemia and hematopoietic stem cell transplant patients.
Centers for Disease Control and Prevention. US Center for Disease Control and Prevention. Get Smart for HealthCare Core Elements of Hospital Antimicrobial Stewardship Program. 2015. http://www.cdc.gov/getsmart/healthcare/implementation.html. Accessed 24 Oct 2015.
•• Monsees E, Popejoy L, Jackson MA, Lee B, Goldman J. Integrating staff nurses in antibiotic stewardship: opportunities and barriers. Am J Infect Control. 2018. https://doi.org/10.1016/j.ajic.2018.03.028. Review on the role of nurses in antimicrobial stewardship.
•• Pulcini C, Morel CM, Tacconelli E, Beovic B, de With K, Goossens H, et al. Human resources estimates and funding for antibiotic stewardship teams are urgently needed. Clin Microbiol Infect. 2017;23(11):785–7. https://doi.org/10.1016/j.cmi.2017.07.013. Summary recommendation on the human resources needs for antimicrobial stewardship programs in hospitals.
•• So M, Mamdani MM, Morris AM, Lau TTY, Broady R, Deotare U, et al. Effect of an antimicrobial stewardship programme on antimicrobial utilization and costs in patients with leukemia: a retrospective interventional controlled study. Clin Microbiol Infect. 2018;24(8):882–8. https://doi.org/10.1016/j.cmi.2017.11.009. Study demonstrating the feasibility and safety of antimicrobial stewardship in leukemia patients.
Morris AM, Stewart TE, Shandling M, McIntaggart S, Liles WC. Establishing an antimicrobial stewardship program. Healthc Q. 2010;13(2):64–70. https://doi.org/10.12927/hcq.2013.21672.
Yeo CL, Wu JE, Chung GW-T, Chan DS-G, Chen HH, Hsu LY. Antimicrobial stewardship auditing of patients reviewed by infectious diseases physicians in a tertiary university hospital. Antimicrob Resist Infect Control. 2013;2(1):29. https://doi.org/10.1186/2047-2994-2-29.
•• Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterizing and designing behaviour change interventions. Implement Sci. 2011;6:42. Comprehensive review on behavioural change interventions.
•• Lorencatto F, Charani E, Sevdalis N, Tarrant C, Davey P. Driving sustainable change in antimicrobial prescribing practice: how can social and behavioral sciences help? J Antimicrob Chemother. 2018. https://doi.org/10.1093/jac/dky222. Comprehensive review on applying behavioural change interventions in antimicrobial stewardship.
•• Avorn J. Academic detailing: “marketing” the best evidence to clinicians. JAMA. 2017;317(4):361–2. https://doi.org/10.1001/jama.2016.16036. Concise summary on the elements for academic detailing as a behavioural change intervention.
•• Ubel PA, Rosenthal MB. Beyond nudges—when improving health calls for greater assertiveness. N Engl J Med. 2019;380(4):309–11. https://doi.org/10.1056/NEJMp1806371. Summary on behavioural change interventions beyond nudging.
Yeo C-L, Chan DS-G, Earnest A, Wu T-S, Yeoh S-F, Lim R, et al. Prospective audit and feedback on antibiotic prescription in an adult hematology-oncology unit in Singapore. Eur J Clin Microbiol Infect Dis. 2012;31(4):583–90. https://doi.org/10.1007/s10096-011-1351-6.
Yeo CL, Wu JE, Chung GW-T, Chan DS-G, Fisher D, Hsu LY. Specialist trainees on rotation cannot replace dedicated consultant clinicians for antimicrobial stewardship of specialty disciplines. Antimicrob Resist Infect Control. 2012;1(1):36. https://doi.org/10.1186/2047-2994-1-36.
•• Aguilar-Guisado M, Espigado I, Martín-Peña A, Gudiol C, Royo-Cebrecos C, Falantes J, et al. Optimisation of empirical antimicrobial therapy in patients with hematological malignancies and febrile neutropenia (how long study): an open-label, randomized, controlled phase 4 trial. Lancet Haematol. 2017;4(12):e573–e83. https://doi.org/10.1016/s2352-3026(17)30211-9. A clinical trial demonstrating the feasibility in reducing exposure to antibiotics in patients with high-risk febrile neutropenia.
•• la Martire G, Robin C, Oubaya N, Lepeule R, Beckerich F, Leclerc M, et al. De-escalation and discontinuation strategies in high-risk neutropenic patients: an interrupted time series analyses of antimicrobial consumption and impact on outcome. Eur J Clin Microbiol Infect Dis. 2018;37(10):1931–40. https://doi.org/10.1007/s10096-018-3328-1. Study demonstrating the feasibility of incorporating antimicrobial stewardship in management of febrile neutropenia.
Mikulska M, Averbuch D, Tissot F, Cordonnier C, Akova M, Calandra T, et al. Fluoroquinolone prophylaxis in hematological cancer patients with neutropenia: ECIL critical appraisal of previous guidelines. J Infect. 2018;76(1):20–37. https://doi.org/10.1016/j.jinf.2017.10.009 Highlights issues of routine fluoroquinolone prophylaxis.
Mikulska M, Cordonnier C. Fluoroquinolone prophylaxis during neutropenia: what can we expect nowadays? Clin Microbiol Infect. 2018;24(7):678–9 Highlights issues of routine fluoroquinolone prophylaxis.
•• Slavin MA, Worth LJ, Seymour JF, Thursky KA. Better sepsis management rather than fluoroquinolone prophylaxis for patients with cancer-related immunosuppression. J Clin Oncol. 2019;0(0):JCO.18.01474. https://doi.org/10.1200/jco.18.01474. Highlights issues of routine fluoroquinolone prophylaxis.
Taplitz RA, Kennedy EB, Bow EJ, Crews J, Gleason C, Hawley DK, et al. Antimicrobial prophylaxis for adult patients with cancer-related immunosuppression: ASCO and IDSA clinical practice guideline update. J Clin Oncol. 2018;36(30):3043–54. https://doi.org/10.1200/jco.18.00374.
Shekelle PG. Clinical practice guidelines: what’s next? Key issues in the development of clinical practice guidelines. JAMA. 2018;320(8):757–8. https://doi.org/10.1001/jama.2018.9660 Highlights issues with international guidelines.
Heneghan C, Mahtani KR, Goldacre B, Godlee F, Macdonald H, Jarvies D. Evidence based medicine manifesto for better healthcare. BMJ. 2017;357:j2973. https://doi.org/10.1136/bmj.j2973.
Santarossa M, Aitken SL, Nagel J. Improving antimicrobial stewardship in cancer patients through implementation of clinical guidelines. Curr Treat Options Infect Dis. 2017;9(3):333–46. https://doi.org/10.1007/s40506-017-0131-y.
Canada Health Infoway. Change management toolkit: leading change in health care. 2015. https://www.infoway-inforoute.ca/en/resource-centre/toolkits/change-management. Accessed 1 Mar 2019.
Goitein L, James B. Standardized best practices and individual craft-based bedicine: a conversation about quality. JAMA Intern Med. 2016;176(6):835–8. https://doi.org/10.1001/jamainternmed.2016.1641.
•• Shenoy ES, Macy E, Rowe T, Blumenthal KG. Evaluation and management of penicillin allergy: a review. JAMA. 2019;321(2):188–99. https://doi.org/10.1001/jama.2018.19283. Comprehensive reivew on penicillin allergy.
•• Huang KG, Cluzet V, Hamilton K, Fadugba O. The impact of reported beta-lactam allergy in hospitalized patients with hematologic malignancies requiring antibiotics. Clin Infect Dis. 2018. https://doi.org/10.1093/cid/ciy037. Highights issues with self-reported beta-lactam allergy on outcome.
MacFadden DR, LaDelfa A, Leen J, Gold WL, Daneman N, Weber E, et al. Impact of reported beta-lactam allergy on inpatient outcomes: a multicenter prospective cohort study. Clin Infect Dis. 2016;63(7):904–10. https://doi.org/10.1093/cid/ciw462.
Leis JA, Palmay L, Ho G, Raybardhan S, Gill S, Kan T, et al. Point-of-care beta-lactam allergy skin testing by antimicrobial stewardship programs: a pragmatic multicenter prospective evaluation. Clin Infect Dis. 2017. https://doi.org/10.1093/cid/cix512.
Taremi M, Artau A, Foolad A, Berlin S, White C, Jiang Y, et al. Safety, efficacy, and clinical impact of penicillin skin testing in immunocompromised cancer patients. J Allergy Clin Immunol Pract. https://doi.org/10.1016/j.jaip.2019.03.025.
•• Patel R, Fang FC. Diagnostic stewardship: opportunity for a laboratory–infectious diseases partnership. Clin Infect Dis. 2018;67(5):799–801. https://doi.org/10.1093/cid/ciy077. Comprehensive review on partnership with microbiology lab in antimicrobial stewardship and infectious diseases.
Miller JM, Binnicker MJ, Campbell S, Carroll KC, Chapin KC, Gilligan PH, et al. A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2018 update by the Infectious Diseases Society of America and the American Society for Microbiologya. Clin Infect Dis. 2018:ciy381–ciy. https://doi.org/10.1093/cid/ciy381.
Patterson TF, Thompson GR, Denning DW, Fishman JA, Hadley S, Herbrecht R, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016. https://doi.org/10.1093/cid/ciw326.
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62(4):e1–50. https://doi.org/10.1093/cid/civ933.
Morrissey CO, Chen SCA, Sorrell TC, Milliken S, Bardy PG, Bradstock KF, et al. Galactomannan and PCR versus culture and histology for directing use of antifungal treatment for invasive aspergillosis in high-risk hematology patients: a randomized controlled trial. Lancet Infect Dis. 2013;13(6):519–28. https://doi.org/10.1016/s1473-3099(13)70076-8.
Aguado JM, Vazquez L, Fernandez-Ruiz M, Villaescusa T, Ruiz-Camps I, Barba P, et al. Serum galactomannan versus a combination of galactomannan and polymerase chain reaction-based Aspergillus DNA detection for early therapy of invasive aspergillosis in high-risk hematological patients: a randomized controlled trial. Clin Infect Dis. 2015;60(3):405–14. https://doi.org/10.1093/cid/ciu833.
Tissot F, Agrawal S, Pagano L, Petrikkos G, Groll AH, Skiada A, et al. ECIL-6 guidelines for the treatment of invasive candidiasis, aspergillosis and mucormycosis in leukemia and hematopoietic stem cell transplant patients. Haematologica. 2017;102(3):433–44. https://doi.org/10.3324/haematol.2016.152900.
Maertens JA, Girmenia C, Bruggemann RJ, Duarte RF, Kibbler CC, Ljungman P, et al. European guidelines for primary antifungal prophylaxis in adult hematology patients: summary of the updated recommendations from the European Conference on Infections in Leukemia. J Antimicrob Chemother. 2018. https://doi.org/10.1093/jac/dky286.
Ananda-Rajah MR, Slavin MA, Thursky KT. The case for antifungal stewardship. Curr Opin Infect Dis. 2012;25(1):107–15. https://doi.org/10.1097/QCO.0b013e32834e0680.
Valerio M, Rodriguez-Gonzalez CG, Munoz P, Caliz B, Sanjurjo M, Bouza E, et al. Evaluation of antifungal use in a tertiary care institution: antifungal stewardship urgently needed. J Antimicrob Chemother. 2014;69(7):1993–9. https://doi.org/10.1093/jac/dku053.
van de Peppel RJ, Visser LG, Dekkers OM, de Boer MGJ. The burden of Invasive Aspergillosis in patients with hematological malignancy: a meta-analysis and systematic review. J Infect. 2018;76(6):550–62. https://doi.org/10.1016/j.jinf.2018.02.012.
Mourad A, Perfect JR. Tolerability profile of the current antifungal armory. J Antimicrob Chemother. 2018;73(suppl_1):i26–32. https://doi.org/10.1093/jac/dkx446.
Benedict K, Jackson BR, Chiller T, Beer KD. Estimation of direct healthcare costs of fungal diseases in the United States. Clin Infect Dis. 2018. https://doi.org/10.1093/cid/ciy776.
Vallabhaneni S, Benedict K, Derado G, Mody RK. Trends in hospitalizations related to invasive aspergillosis and mucormycosis in the United States, 2000–2013. Open Forum Infect Dis. 2017;4(1):ofw268. https://doi.org/10.1093/ofid/ofw268.
Perlin DS, Rautemaa-Richardson R, Alastruey-Izquierdo A. The global problem of antifungal resistance: prevalence, mechanisms, and management. Lancet Infect Dis. 2017;17(12):e383–e92. https://doi.org/10.1016/s1473-3099(17)30316-x.
Lestrade PP, Bentvelsen RG, Schauwvlieghe A, Schalekamp S, van der Velden W, Kuiper EJ, et al. Voriconazole resistance and mortality in invasive aspergillosis: a multicenter retrospective cohort study. Clin Infect Dis. 2018. https://doi.org/10.1093/cid/ciy859.
Lamoth F, Lockhart SR, Berkow EL, Calandra T. Changes in the epidemiological landscape of invasive candidiasis. J Antimicrob Chemother. 2018;73(Supplement 1:i4–i13.
Micallef C, Aliyu SH, Santos R, Brown NM, Rosembert D, Enoch DA. Introduction of an antifungal stewardship programme targeting high-cost antifungals at a tertiary hospital in Cambridge, England. J Antimicrob Chemother. 2015;70(6):1908–11. https://doi.org/10.1093/jac/dkv040.
Valerio M, Munoz P, Rodriguez CG, Caliz B, Padilla B, Fernandez-Cruz A, et al. Antifungal stewardship in a tertiary-care institution: a bedside intervention. Clin Microbiol Infect. 2015;21(5):492 e1–9. https://doi.org/10.1016/j.cmi.2015.01.013.
Alfandari S, Berthon C, Coiteux V. Antifungal stewardship: implementation in a French teaching hospital. Med Mal Infect. 2014;44(4):154–8.
Valerio M, Vena A, Rodriguez-Gonzalez CG, de Vega EC, Mateos M, Sanjurjo M, et al. Repeated antifungal use audits are essential for selecting the targets for intervention in antifungal stewardship. Eur J Clin Microbiol Infect Dis. 2018;37(10):1993–2000. https://doi.org/10.1007/s10096-018-3335-2.
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813–21. https://doi.org/10.1086/588660.
Barnes R, Earnshaw S, Herbrecht R, Morrissey O, Slavin M, Bow E, et al. Economic comparison of an empirical versus diagnostic-driven strategy for treating invasive fungal disease in immunocompromised patients. Clin Ther. 2015;37(6):1317–28 e2. https://doi.org/10.1016/j.clinthera.2015.03.021.
•• Whitney L, Al-Ghusein H, Glass S, Koh M, Klammer M, Ball J, et al. Effectiveness of an antifungal stewardship programme at a London teaching hospital 2010–16. J Antimicrob Chemother. 2019;74(1):234–41. https://doi.org/10.1093/jac/dky389. Study demonstrated the safety and feasibility of antifungal stewardship interventions.
Morris AM. Antimicrobial stewardship programs: appropriate measures and metrics to study their impact. Curr Treat Options Infect Dis. 2014;6(2):101–12. https://doi.org/10.1007/s40506-014-0015-3.
•• Bienvenu AL, Argaud L, Aubrun F, Fellahi JL, Guerin C, Javouhey E, et al. A systematic review of interventions and performance measures for antifungal stewardship programmes. J Antimicrob Chemother. 2018;73(2):297–305. https://doi.org/10.1093/jac/dkx388. Evaluation on antifungal stewardship programs.
van Santen KL, Edwards JR, Webb AK, Pollack LA, O’Leary E, Neuhauser MM, et al. The standardized antimicrobial administration ratio: a new metric for measuring and comparing antibiotic use. Clin Infect Dis. 2018;67(2):179–85. https://doi.org/10.1093/cid/ciy075.
Health Quality Ontario (2013). HQO Quality Improvement Science. Ontario: Ontario Ministry of Health and Long-Term Care (MOHLTC); 2013.
•• Jones B, Vaux E, Olsson-Brown A. How to get started in quality improvement. BMJ. 2019;364:k5408. https://doi.org/10.1136/bmj.k5437. Summary on quality improvement process in the clinical setting.
National Centre for Antimicrobial Stewardship Australian Commission on Safety and Quality in Health Care. National Antimicrobial Prescribing Survey (NAPS). Australia; 2019. https://www.naps.org.au/Default.aspx. Accessed 10 Mar 2019.
James R, Upjohn L, Cotta M, Luu S, Marshall C, Buising K, et al. Measuring antimicrobial prescribing quality in Australian hospitals: development and evaluation of a national antimicrobial prescribing survey tool. J Antimicrob Chemother. 2015;70(6):1912–8. https://doi.org/10.1093/jac/dkv047.
Denny KJ, Gartside JG, Alcorn K, Cross JW, Maloney S, Keijzers G. Appropriateness of antibiotic prescribing in the Emergency Department. J Antimicrob Chemother. 2019;74(2):515–20. https://doi.org/10.1093/jac/dky447.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Antimicrobial Stewardship
Rights and permissions
About this article
Cite this article
So, M. Antimicrobial Stewardship in Patients with Hematological Malignancies: Key Considerations. Curr Treat Options Infect Dis 11, 161–176 (2019). https://doi.org/10.1007/s40506-019-00189-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40506-019-00189-2