Abstract
Introduction
With the availability of an increasing number of therapeutic options for advanced prostate cancer (APC), optimal sequencing and combination of therapies have emerged to be the areas of challenges. In the Indian context, there is a dearth of consensus recommendations to guide clinicians regarding optimal sequencing of therapy in APC management. A Delphi-based consensus regarding optimal therapy sequencing in APC management was developed by an expert panel of medical oncologists from across India.
Methods
An expert scientific committee of 11 medical oncologists and an expert panel of 53 medical oncologists from India constituted the panel for the Delphi consensus. In the first phase, a questionnaire with 41 clinical statements was developed in several critical controversial areas in APC treatment. In the second phase, 29 clinical statements were reworked and sent to eight experts to obtain their opinions on best practices. The consensus ratings were based on a 9-point Likert scale. Based on the overall response, statements with a mean score of ≥ 7 with 1 outlier were considered as “consensus.”
Results
Degarelix was the preferred androgen deprivation therapy (ADT). While ADT plus docetaxel was the preferred option for metastatic castrate-sensitive/naïve prostate cancer patients with high-volume disease, ADT with abiraterone was the preferred choice for low-volume disease. Docetaxel was the preferred first-line treatment option in men who received ADT alone in the castrate-sensitive/naïve setting. For patients progressing on or after docetaxel for metastatic castrate-resistant prostate cancer (without prior abiraterone or enzalutamide), the experts reached a consensus on the use of enzalutamide as the preferred second-line treatment option. No consensus was reached for the third-line treatment options.
Conclusion
This article is intended to serve as a guide to help clinicians discuss with their patients as part of the shared and multidisciplinary decision-making for improved APC management in India.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Although several treatment options are available for advanced prostate cancer (APC), the next challenge in the effective management of APC is determination of the best combination and sequence of available therapeutic regimens. |
No guideline (National Comprehensive Cancer Network [NCCN], American Society of Clinical Oncology [ASCO], or European Society for Medical Oncology [ESMO]) has emphasized the clear sequencing of molecules in APC management. |
In the Indian scenario, there is a lack of any consensus recommendations to guide clinicians regarding optimal sequencing of systemic therapeutic agents in APC. |
An expert panel of medical oncologists from India developed Delphi-method based consensus recommendations on optimal therapy sequencing in APC management. |
This consensus document will offer expert guidance to Indian oncologists on decision-making regarding optimum sequencing of therapy for APC in real-world clinical practice. |
Introduction
Prostate cancer is the second most common cancer among men globally and the second most common cause of cancer-related mortality [1, 2]. In India, it is the third most common cancer [3]. Notably, despite the low overall incidence of prostate cancer in India, the associated mortality is relatively high as compared to those of other countries with higher incidence rates [3]. Moreover, the incidence of new prostate cancer cases in India is estimated to increase from 34,500 in 2020 to 65,100 in 2040 [4]. These statistics are of concern, which indicates the need for early diagnosis and optimized management of the disease in the country.
Despite the 5-year survival rate of localized prostate cancer being > 99%, advanced prostate cancer (APC) is mostly incurable [2]. The categories of APC are nonmetastatic, metastatic, and castrate-resistant prostate cancer (CRPC) [5]. About 10–20% of cases of APC progress to CRPC within 5 years, among which ≥ 84% are diagnosed with metastatic CRPC (mCRPC).
Since the 1940s, androgen deprivation therapy (ADT) has served as the cornerstone of APC management. The ADT lowers circulating androgen to castration levels, thereby slowing disease progression [1, 2]. Unfortunately, castrate-sensitive prostate cancer (CSPC) develops resistance even at low testosterone levels and progresses to CRPC, whereby ADT as a single agent fails to prevent disease progression [1]. However, with an improved understanding of the in-depth mechanisms of the disease and the availability of new treatment options, there has been a paradigm shift in the management of this cancer [2].
Currently, the agents used for the management of metastatic CSPC (mCSPC) are docetaxel, abiraterone acetate, apalutamide, and enzalutamide (novel anti-androgen therapies). For CRPC patients, the current standard therapy includes ADT, chemotherapy (docetaxel as the first line and cabazitaxel as the second line), sipuleucel-T (immunotherapy), anti-androgen therapy (abiraterone acetate and enzalutamide), targeted therapy against specific mutations in DNA damage repair genes (such as rucaparib and olaparib, and poly (ADP-ribose) polymerase [PARP] inhibitors), and radiopharmaceuticals, such as radium-223, in case of bone metastases [1]. Besides these agents, other radiopharmaceuticals and immunotherapies also serve as effective therapeutic options for mCRPC treatment [6]. Previously, mCSPC was managed with ADT, mostly in combination with androgen receptor (AR) antagonists like bicalutamide and flutamide [7]. However, no benefit in overall survival (OS) could be achieved with such therapy, and CSPC inevitably progressed to CRPC [7]. Based on recent clinical data, ADT combined with upfront therapies, such as enzalutamide, apalutamide, and abiraterone acetate, has been approved by the US Food and Drug Administration (FDA) for mCSPC, in addition to CRPC [8]. Recent data suggest that the use of dual androgen suppressor, i.e., addition of apalutamide to the established therapy of abiraterone and prednisone in mCRPC patients, further improves the radiographic progression-free survival (PFS) [9].
Although immunotherapy has revolutionized the therapeutic landscape for multiple solid cancers and hematological malignancies, the scenario is not so promising for mCRPC patients. The usage of sipuleucel-T, the only FDA-approved cancer vaccine for mCRPC, is relatively limited in routine clinical practice. In this context, one of the key challenges is the identification of specific molecular or histological biomarkers for predicting response to immunotherapy in different subgroups of mCRPC patients. Nevertheless, it has been suggested that a few subsets of prostate cancer patients could benefit from immunotherapy [10]. An emerging area of interest in prostate cancer management is the interaction between cancer and the microbiome, especially regarding the impact of the microbiota on the pathogenesis of prostate cancer development, and response to therapy [11]. A detailed understanding of the specifics of altered microbiota associated with prostate cancer could be the key to the development of personalized treatment for this genitourinary malignancy [12]. Recent data suggest that prostate cancer patients with TMPRSS:ERG gene fusion (an early event in prostate cancer development) and receiving anti-androgen therapy are at a lower risk of SARS-CoV-2 infection or severity [13].
One of the challenges in CRPC management is the determination of the best combination and sequence of regimens; hence, this will likely be the next giant leap for the successful management of prostate cancer [5]. To address this issue, consensus recommendations on the sequencing of therapy are being developed in different countries, such as Canada and Europe [14, 15]. However, there are no consensus guidelines on the sequencing of therapy for APC management in India.
In this context, an attempt was made to arrive at a consensus regarding the sequencing of systemic therapies in the management of APC in India using the Delphi method. This article provides a series of stepwise recommendations based on the existing clinical evidence along with consensus statements to aid the specialists with appropriate decision-making for sequencing of therapy in the management of APC in India.
Methods
An expert scientific committee of 11 medical oncologists and an expert panel of 53 medical oncologists from India constituted the panel of experts for the Delphi consensus. The panel members were selected across the country based on their expertise in the field of APC management.
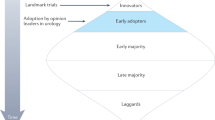
A modified Delphi method was followed for the consultation process among the 53 panel members [16]. The study methodology involved a two-step process. In the first phase, a scientific committee with 11 medical oncologists plus a coordinator identified several critical controversial areas in APC treatment and developed a questionnaire covering four topics (ADT for castrate-naïve prostate cancer, primary ADT for M1 castrate-naïve prostate cancer, secondary hormone therapy for M0 CRPC, and secondary hormone therapy for M1 CRPC) with a total of 41 clinical statements. These clinical statements were sent to 53 medical oncologists to obtain their opinions on best practices. In the second phase, 29 clinical statements that were reworked based on the response analysis of the first phase were sent to eight experts from the scientific committee to obtain their opinions on best practices (Fig. 1).
The consensus ratings were based on a 9-point Likert scale: 1 = strongly disagree; 2 = mostly disagree; 3 = disagree; 4 = slightly disagree; 5 = neutral; 6 = slightly agree; 7 = agree; 8 = mostly agree; and 9 = strongly agree. Based on the overall response, statements with a mean score of ≥ 7 with 1 outlier were considered as “consensus.” Statements with a mean score of ≥ 6.5 with ≤ 2 outliers were considered as a “near-consensus,” while statements that did not meet the above criteria for “consensus” or “near-consensus” were listed as “no consensus.”.
As this was a Delphi-based consensus document, IRB approval was not required. However, all the participants of the study were aware of the objectives of the study, and the participants were also aware that the results of the study would be published. Before the start of the consensus procedure, each participant was briefed about the nature of the activity. A consent page to participate was attached as the first page of the electronic sheet shared with all the participants. Only if the participant agreed to participate was it then possible to move forward and turn to the second page. Participants have given their independent opinion based on their previous experience. The final responses of all participants were automatically generated in the form of final percentage and graphs to ensure the protection of participants’ individual data.
Results
Androgen Deprivation Therapy
Regarding ADT for newly diagnosed castrate-sensitive/naïve prostate cancer, a near-consensus was reached by the panel of experts for both leuprolide and degarelix as the preferred choice in asymptomatic patients without any comorbidity. The experts voted for degarelix as the preferred ADT for symptomatic patients without any comorbidity (near-consensus). In the case of the presence of comorbidities, a consensus was reached for degarelix as the preferred ADT (only for cardiovascular risk factors).
Managing Disease Progression and Sequencing
Newly Diagnosed Metastatic Castrate-Naïve Prostate Cancer
No consensus was reached among the experts regarding the use of ADT alone as the preferred first-line treatment option for the majority of newly diagnosed metastatic castrate-naïve prostate cancer patients.
A consensus was reached for the use of ADT plus docetaxel as the preferred treatment option for metastatic castrate-sensitive/naïve prostate cancer patients with high-volume disease. The high-volume disease is defined as the presence of visceral disease, or ≥ 4 bone metastases, with at least one outside pelvis and vertebrae [17].
While ADT plus docetaxel is considered for patients with high-volume disease, ADT plus abiraterone is recommended even in patients with low-volume disease [17], characterized by < 3 bone lesions, spine, and lymph node. In the present study, a consensus was reached regarding the use of ADT with abiraterone as the preferred treatment option for metastatic castrate-sensitive/naïve prostate cancer patients with low-volume disease.
Castrate-Resistant Prostate Cancer
First-line Treatment in mCRPC
The experts arrived at a near-consensus recommending abiraterone as the preferred first-line treatment option for mCRPC in the majority of asymptomatic or minimally symptomatic men who received ADT alone in the castrate-sensitive/naïve setting. For symptomatic men with mCRPC, the experts arrived at a consensus on docetaxel as the preferred first-line treatment option in men who received ADT alone in the castrate-sensitive/naïve setting.
A near-consensus was achieved for abiraterone as the preferred first-line treatment option for the majority of asymptomatic or minimally symptomatic men with mCRPC and previously treated with chemotherapeutic agents like docetaxel. However, no consensus was reached on using abiraterone as the preferred first-line mCRPC treatment option in the majority of symptomatic men who did receive docetaxel in the castrate-sensitive/naïve setting.
Abiraterone was also not recommended by the experts (no consensus) for asymptomatic, minimally symptomatic, or symptomatic men who have received chemohormonal therapy and progressed within 6 months after completion of docetaxel therapy.
Second-line Treatment in mCRPC
The experts also reached a near-consensus on recommending abiraterone for men with mCRPC with the presence of baseline significant neurocognitive impairment, when all options are available.
A consensus was reached for using abiraterone in mCRPC with stable brain metastasis. However, no consensus was reached in favor of abiraterone for other medical situations, such as low cardiac ejection fraction, acute liver dysfunction, hypertension, and diabetes mellitus, requiring prescribed drug therapy.
The experts remained divided in their opinion (no consensus) on the use of enzalutamide or abiraterone as the preferred second-line mCRPC treatment option in the majority of men with asymptomatic or symptomatic mCRPC who had progressive disease after best response to first-line abiraterone or enzalutamide.
Similarly, no consensus was arrived at for the use of abiraterone or enzalutamide as the preferred second-line mCRPC treatment option in the majority of men with asymptomatic mCRPC and secondary (acquired) resistance (initial response followed by progression) after the use of first-line abiraterone or enzalutamide.
In the case of asymptomatic/minimally symptomatic men progressing on or after docetaxel for mCRPC (without prior abiraterone or enzalutamide), the experts reached a consensus on the use of enzalutamide as the preferred second-line mCRPC treatment option. No consensus was reached for the use of abiraterone in symptomatic men progressing on or after docetaxel for mCRPC (without prior abiraterone or enzalutamide).
Third-line Treatment in mCRPC
Real-world evidence suggests docetaxel as the most common third-line therapy, comprising 24% of third-line treatment options [18].
The experts remained divided in their opinion regarding the preferred third-line treatment options as follows: (a) enzalutamide or abiraterone as the preferred third-line mCRPC treatment option in the majority of men with mCRPC, progressing on or after second-line docetaxel for mCRPC and prior treatment with abiraterone or enzalutamide; (b) docetaxel rechallenge as the preferred management in mCRPC patients previously treated with docetaxel, cabazitaxel, and abiraterone/enzalutamide.
The key consensus statements are summarized in Table 1; detailed consensus results are presented in Supplementary Table 1.
Discussion
Prostate cancer management has changed in recent decades with the approval of various molecules in various stages of prostate cancer. Different classes of drugs, such as docetaxel, abiraterone, and enzalutamide, are approved in the treatment of castrate-sensitive/resistant cases, allowing oncologists to have their own preferences in management and sequencing. No guideline (National Comprehensive Cancer Network [NCCN], American Society of Clinical Oncology [ASCO], or European Society for Medical Oncology [ESMO]) has emphasized the clear sequencing of molecules in APC management. In India, there are no country-specific guidelines or recommendations for the management and sequencing of systemic therapy in the treatment of APC. Further, due to the scarcity of randomized controlled trials conducted in India and the lack of region-specific guidelines or recommendations, oncologists rely primarily on data from the Western world, which may not be replicated in Indian patients. As a result, depending on the nature of the disease, whether hormone-sensitive or hormone-resistant, high-burden or low-burden disease, or associated with comorbidities, many oncologists prefer their own choice of therapy in disease management in the treatment-naïve stage and after progression. This consensus document will offer expert guidance to oncologists on the management and sequencing of prostate cancer in real-world practice.
Androgen Deprivation Therapy
ADT for Castrate-Naïve Disease
Approximately 90% of patients with mCSPC respond to initial treatment with ADT, as the growth of prostate cancer cells is driven by high levels of androgens, and ADT lowers the production of testicular androgens. The types of ADT are luteinizing hormone-releasing hormone (LHRH) or gonadotropin-releasing hormone (GnRH) agonists that prevent luteinizing hormone secretion; LHRH antagonists that decrease luteinizing hormone secretion; and orchiectomy. The approved LHRH agonists are goserelin and leuprolide, while the only approved LHRH antagonist is degarelix [17].
Leuprolide or Degarelix or Triptorelin/Goserelin in Clinical Practice: Positioning and Patient Selection
Agonists and antagonists of GnRH serve as first-line ADT for earlier stages of prostate cancer. Because of their direct mode of action, GnRH antagonists, such as abarelix and degarelix, do not generate the initial testosterone surge, unlike GnRH agonists. Degarelix is reportedly more effective than the first-line GnRH agonist leuprolide and leads to faster castration onset, without the risk of testosterone surge or clinical flare, faster prostate-specific antigen (PSA) suppression, improved PSA PFS, and delayed castration resistance. To address the testosterone surge or clinical flare, GnRH agonists require anti-androgens, such as bicalutamide, for flare protection [19]. The key studies on first-generation ADTs are presented in Table 2 [20,21,22,23,24].
With an increased understanding of the mechanisms and adverse effects of ADT, degarelix has emerged as a newer class of ADT, which leads to a rapid and reliable decrease in serum testosterone levels. It is particularly advantageous for men with symptomatic CSPC. Although available ADT provides similar efficacy, evidence suggests that degarelix provides both cardiovascular and oncologic benefits, in contrast to GnRH agonist therapy [25]. Also, a study has reported the safety and effectiveness of leuprolide in the Asian population of prostate cancer patients, albeit in association with decreased sexual function [26].
Based on available evidence, the experts advocated the use of either leuprolide or degarelix for asymptomatic mCSPC without any comorbidity. The experts voted for only degarelix in the case of symptomatic mCSPC patients and in the presence of cardiovascular comorbidity.
Primary ADT for Metastatic (M1) Castrate-Naïve Prostate Cancer
The treatment options available for newly diagnosed metastatic castrate-naïve prostate cancer include chemohormonal therapy, AR-targeted therapy plus ADT, and ADT alone [8]. For the majority of men with mCSPC, the use of ADT alone for testosterone suppression is no longer used as the standard of care. Several upfront therapies are combined with ADT for mCSPC treatment, such as docetaxel, enzalutamide, abiraterone acetate (with corticosteroid therapy), and apalutamide [8].
Based on evidence from three clinical trials, ChemoHormonal Therapy Versus Androgen Ablation Randomized Trial for Extensive Disease in Prostate Cancer (CHAARTED), GETUG-AFU 15, and STAMPEDE arm C, ADT combined with docetaxel is considered as the standard of care for men with high-volume mCSPC [17, 27,28,29]. Further, according to the outcomes in the CHAARTED and GETUG-AFU 15 trials, no benefit was achieved with docetaxel in men with low-volume disease [17, 27, 29].
ADT Alone or with Abiraterone/Enzalutamide/Docetaxel
ADT has served as the backbone for mCSPC treatment. However, the mCSPC therapy landscape has changed significantly over the last 5 years. The addition of novel agents to ADT has resulted in improved outcomes in metastatic prostate cancer. The first randomized phase III trial, GETUG-AFU 15, assessed the use of early docetaxel in combination with ADT, as compared to ADT alone. The study showed there was no benefit in OS with early docetaxel plus ADT [29]. Since 2015, two clinical trials in mCSPC patients, CHAARTED and STAMPEDE arm C, reported improved OS with ADT plus docetaxel [17, 28, 30]. Subsequently, the LATITUDE and STAMPEDE arm G trials demonstrated that similar to docetaxel plus ADT, abiraterone plus prednisone plus ADT provides improved OS benefits, as compared to ADT alone [17, 31, 32].
Moreover, the recent findings from the phase III trials evaluating enzalutamide, ENZAMET and ARCHES, have generated further options for mCSPC treatment [2, 33, 34]. The ENZAMET trial demonstrated longer OS and PFS with enzalutamide as compared to ADT with older nonsteroidal anti-androgen agents [2, 33]. In the ARCHES trial, as compared to ADT plus placebo, ADT plus enzalutamide significantly lowered the metastatic progression of disease or death over time in men with mCSPC [34].
Considering all these reports, the experts did not favor the use of ADT alone for mCSPC. Rather, ADT plus docetaxel was recommended for mCSPC with high-volume disease, and ADT with abiraterone for mCSPC with low-volume disease. The key studies in mCSPC are presented in Table 3 [8, 29,30,31,32,33,34,35,36].
Existing Guideline Recommendations for CSPC
The recent guidelines from the NCCN recommend the use of LHRH agonist plus first-generation anti-androgen or LHRH agonist/antagonist for castrate-naïve prostate cancer. In non-metastatic CSPC (nmCSPC), ADT can be used in combination with apalutamide, enzalutamide, docetaxel, or abiraterone. The ADT options recommended for the metastatic castrate-naïve disease are LHRH agonist/antagonist ± docetaxel, LHRH agonist plus first-generation anti-androgen ± docetaxel, LHRH agonist/antagonist plus abiraterone, apalutamide, or enzalutamide [37].
According to the Advanced Prostate Cancer Consensus (APCC) recommendations, the use of ADT alone is not recommended for mCSPC patients with low-volume or high-volume disease, or without symptoms associated with the primary tumor. However, for newly diagnosed mCSPC, the use of ADT in combination with docetaxel and AR pathway inhibitor (enzalutamide, abiraterone, or apalutamide) was not recommended [15].
Secondary Hormone Therapy for CRPC
The majority of men with APC eventually stop responding to ADT, a condition designated as castrate-resistant disease or CRPC [35]. CRPC is characterized by the progression of the disease while on ADT, even with castrate levels of serum testosterone [38].
Nonmetastatic (M0) Castrate-Resistant Prostate Cancer
The stage of prostate cancer when the disease exhibits biochemical progression even after castration, but without any radiological evidence of distant metastasis, is termed nmCRPC or M0 CRPC. The independent predictive factors for risk of metastasis for these patients include baseline PSA, PSA increase rate, and PSA doubling time. The meaningful approach for the treatment of nmCRPC is to delay the incidence of metastasis and increase metastasis-free survival [39].
Abiraterone or Enzalutamide
A phase III study, Safety and Efficacy Study of Enzalutamide Versus Bicalutamide in Men with Prostate Cancer (STRIVE), compared enzalutamide with bicalutamide in nmCRPC patients (N = 139). As compared to bicalutamide, the risk of disease progression or death was significantly lower with enzalutamide in nmCRPC patients (76%; p < 0.001) [40]. Another multicenter phase III randomized trial, Safety and Efficacy Study of Enzalutamide in Patients with Nonmetastatic Castration-Resistant Prostate Cancer (PROSPER), compared enzalutamide with placebo plus ADT in 1401 nmCRPC patients. Both PSA progression time (37.2 vs. 3.9 months, respectively; p < 0.001) and median metastasis-free survival (36.6 vs. 14.7 months, respectively; p < 0.001) were significantly prolonged with enzalutamide as compared to placebo, both in combination with ADT [41]. Based on these results, enzalutamide is approved as one of the standard treatments for nmCRPC [39].
At present, there is no high-level evidence in support of the long-term benefits of abiraterone. However, since enzalutamide, with a similar mode of action, delays tumor progression in nmCSPC, theoretically, abiraterone should have a similar effect [39]. The IMpact of Abiraterone Acetate on Prostate Specific AntiGEN (IMAAGEN) study showed that in high-risk nmCSPC patients, abiraterone plus prednisone significantly reduces PSA50 (≥ 50% reduction in PSA, 86.9%; p < 0.001) [42].
Darolutamide
The AR inhibitor darolutamide is approved for the treatment of nmCRPC in combination with ADT. In the phase III ARAMIS trial, darolutamide demonstrated significantly prolonged metastasis-free survival in nmCRPC patients, as compared to placebo (40.4 vs. 18.4 months; p < 0.001) [43]. A preplanned subgroup analysis of the ARAMIS trial involving 1509 Japanese patients reported consistent efficacy benefits of darolutamide vs. placebo in nmCRPC patients, particularly in improving metastasis-free survival [44]. However, darolutamide is currently not approved in India.
Metastatic (M1) Castrate-Resistant Prostate Cancer
The US FDA approved the use of abiraterone combined with low-dose prednisone for the treatment of mCRPC in both docetaxel-naïve men and in men previously treated with docetaxel-containing chemotherapy [37]. A real-world retrospective study has reported 65% and 54% use of abiraterone/prednisone and enzalutamide for first- and second-line therapies, respectively [18]. But ADT has been associated with some adverse effects including sexual dysfunction, metabolic disturbances, cognitive defects, weight gain, and gynecomastia. While abiraterone has been associated with adverse cardiac effects, liver function test abnormalities, hypertension, and hypokalemia, enzalutamide increases the incidence of hypertension and fatigue [45,46,47]. Abiraterone might also increase the risk of hypoglycemia in prostate cancer patients with type 2 diabetes mellitus receiving concurrent glucose-lowering therapy. In contrast to chemotherapy or enzalutamide in mPC patients, abiraterone is associated with a lower likelihood of a central nervous system (CNS) event [48].
Chemotherapy or Enzalutamide/Abiraterone
Patients with metastatic lesions and with no pain or mild pain, and in good physical condition, are defined as asymptomatic or minimally symptomatic M1 CRPC [39]. In the COU-AA-302 study, 1088 asymptomatic or mildly symptomatic chemotherapy-naïve mCRPC patients were treated with abiraterone plus prednisone combination or placebo plus prednisone. The abiraterone combination improved OS as compared to the placebo group (34.7 vs. 30.3 months, respectively; p = 0.003). These findings favored the use of abiraterone in chemotherapy-naïve mCRPC patients [49]. A safety and efficacy study of oral enzalutamide in chemotherapy-naïve patients with progressive metastatic prostate cancer (PREVAIL) showed that as compared to placebo, enzalutamide significantly improved OS and radiologic PFS in chemotherapy-naïve asymptomatic or mildly symptomatic men with mCRPC, previously treated with ADT [50, 51]. In 2004, a phase III trial showed that as compared to mitoxantrone plus prednisone, docetaxel plus prednisone significantly prolonged median survival (16.5 vs. 18.9 months) and improved rates of response in terms of serum PSA level, pain, and quality of life in men with mCRPC [52]. But the study also included symptomatic patients, and adverse events were higher with docetaxel [39]. Based on these findings, docetaxel was approved for M1 CRPC patients [2]. Between chemotherapy and enzalutamide/abiraterone, the experts were in favor of abiraterone for asymptomatic or minimally symptomatic mCRPC previously treated with ADT in a CSPC setting and preferred docetaxel in symptomatic mCRPC patients previously treated with ADT alone.
For mCRPC patients, who progress after first-line chemotherapy, novel endocrine therapy should be given priority. Although cabazitaxel chemotherapy can be used for patients who respond poorly to docetaxel, the level of toxicity is significant, which might outweigh its clinical benefits [39]. The COU-AA-301 trial on mCRPC with poor response to docetaxel showed that as compared to placebo, abiraterone plus prednisone combination significantly prolonged OS (11.2 vs. 15.8 months; p < 0.001), median PSA progression (6.6 vs. 8.5 months), and radiological time to progression (3.6 vs. 5.6 months). Moreover, the proportion of patients with PSA50 was higher for the abiraterone group than for the placebo group (5.5% vs. 29%) [39, 53].
A study evaluating the efficacy and safety of the investigational drug MDV3100 (AFFIRM) evaluated the effects of enzalutamide in mCRPC patients who progressed after chemotherapy (including docetaxel). As compared to placebo plus ADT, enzalutamide plus ADT prolonged OS (13.6 vs. 18.4 months). The proportion of patients with PSA50, radiological PFS, and radiological remission rates was also in favor of enzalutamide [39, 54]. The phase III TROPIC trial demonstrated better median OS (15.1 months vs. 12.7 months; p < 0.001) with cabazitaxel as compared to mitoxantrone in combination with prednisone among mCRPC patients who progressed despite docetaxel treatment [2, 55].
With this background, the experts were of a favorable opinion regarding the use of abiraterone in asymptomatic or minimally symptomatic mCRPC patients who progressed despite docetaxel, but not for symptomatic patients.
There is limited evidence on the choice of therapy after failure of chemohormonal (chemotherapy plus abiraterone or enzalutamide) therapy in mCRPC patients. A retrospective study evaluated the efficacy of enzalutamide as the third-line therapy in mCRPC patients after docetaxel and abiraterone. Enzalutamide showed modest activity as a third-line agent. Moreover, response to earlier abiraterone therapy was not predictive of response to subsequent enzalutamide therapy [56]. The CARD trial compared the effects of cabazitaxel or an alternative androgen axis inhibitor (AAI) (abiraterone, or enzalutamide) in mCRPC patients previously treated with docetaxel and AAI but having disease progression within 12 months of the AAI treatment. As compared to alternative AAI, cabazitaxel showed superior OS (11 vs. 13.6 months; p = 0.008), median radiological PFS (3.7 vs. 8 months; p < 0.001), and median PFS (2.7 vs. 4.4 months; p < 0.001) [2, 57]. Thus, due to a lack of supportive evidence, the experts did not arrive at any consensus regarding the most preferred treatment option for mCRPC patients after the failure of chemohormonal therapy.
Existing Guideline Recommendations for CRPC
For nmCRPC, the NCCN guidelines recommend the use of ADT in combination with apalutamide, enzalutamide, or other secondary hormone therapy. Use of abiraterone, or enzalutamide, or docetaxel is recommended as first-line treatment in mCRPC. Docetaxel is the preferred second-line treatment for mCRPC patients treated with first-line abiraterone/enzalutamide, while abiraterone/enzalutamide is the preferred second-line therapy for patients treated with docetaxel in the first line. For subsequent treatment, docetaxel, or enzalutamide, or abiraterone should be preferred [37].
According to the recommendations from the APCC, in nmCRPC patients, the use of apalutamide or enzalutamide should be preferred in addition to ADT. The use of glucocorticoid regimen (prednisone/prednisolone) was recommended in mCRPC while initiating treatment with abiraterone [15].
Sequencing of Therapy in APC
Evidence of Sequencing in Literature
Since at present several treatment options are available for mCRPC, optimal sequencing and combination of these therapeutics have posed a serious challenge. Further, the trials that led to their approval for mCRPC treatment evaluated these drugs as monotherapies, and there is a lack of direct comparator trials [58]. Several retrospective studies have been performed on the sequencing of therapy in CRPC patients (Table 4) [59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74]. A study reported moderate activity of enzalutamide in patients who received abiraterone for ≥ 24 weeks before progression. Cross-resistance between abiraterone and enzalutamide was observed in the majority of patients [75]. The PLATO trial demonstrated that the reverse sequence, i.e., using abiraterone following PSA rise with enzalutamide treatment, was not indicated in mCRPC patients, and the combination was associated with frequent hypertension and increased liver enzymes [76]. A phase II cross-over trial evaluated the optimal sequencing of abiraterone plus prednisone and enzalutamide in mCRPC. The findings of the study suggested that sequencing abiraterone first followed by enzalutamide provides better clinical benefit than vice versa [77]. The optimal sequence of treatment for mCRPC is currently unknown. Ideally, sequencing decisions should be based on several factors, such as the extent and progression of the disease, previous treatments, comorbidities, and patient preferences [38].
Sequencing of Agents Drawn from the Consensus
Based on the available literature, clinical evidence, and consensus statements, the experts arrived at a general algorithm for the sequencing of therapy in APC (Fig. 2).
With the approval of immunotherapy and PARP inhibitor drugs, the usage of these therapies will increase in the treatment of prostate cancer, especially in the early stages of the disease. This will gradually limit the use of chemotherapy in prostate cancer treatment. A few years ago, chemotherapeutic agents such as cabazitaxel and docetaxel were the only drugs approved for the treatment of CRPC. However, abiraterone and enzalutamide are the preferred options now, along with the recent addition of apalutamide to the treatment landscape. Furthermore, with the availability of drugs with lower CNS toxicity/adverse events, such as darolutamide, in the near future, it can be expected that such therapies will be adopted widely for prostate cancer management.
Limitations
The authors acknowledge a few limitations of this consensus article. Since this consensus is region-specific, its applicability outside of India will be limited. Although the molecules and their positioning as discussed in the consensus have been developed by a highly specialized, multidisciplinary panel, it is at risk of becoming outdated over time as further evidence emerges and as more molecules are added to the CRPC landscape. Therefore, continuous attempts should be made to update the consensus on a timely basis. Another limitation is that the urologists and radiation oncologists were under-represented on the consensus panel. Despite these limitations, we believe that the consensus recommendations developed by the expert forum address several important gaps in the management of APC and will be useful for oncologists in India.
Conclusions
With the advancements in the mechanistic understanding of the disease, the treatment paradigm for APC is likely to undergo further modifications, with multiple new therapeutic options being added. In this scenario, with further advancement of the disease, the choice of optimal therapeutic agents, their sequencing, and the combination becomes a serious challenge for the clinicians. The development of consolidated, evidence-based consensus recommendations to guide clinicians of India regarding sequencing of therapy in APC management is the need of the hour. To the best of our knowledge, this is the first evidence-based consensus document from India to guide the clinicians of the country for appropriate selection, sequencing, and combination of therapies for implementing optimum personalized APC management.
References
Powers E, Karachaliou GS, Kao C, Harrison MR, Hoimes CJ, George DJ, et al. Novel therapies are changing treatment paradigms in metastatic prostate cancer. J Hematol Oncol. 2020;13(1):144.
Swami U, McFarland TR, Nussenzveig R, Agarwal N. Advanced prostate cancer: treatment advances and future directions. Trends Cancer. 2020;6(8):702–15.
Murthy V, Mallick I, Arunsingh M, Gupta P. Prostate radiotherapy in India: evolution, practice and challenges in the 21st century. Clin Oncol (R Coll Radiol). 2019;31(8):492–501.
GlOBOCAN 2020. India. Available at: https://gco.iarc.fr/tomorrow/en/dataviz/isotype?cancers=27&single_unit=5000&populations=356&group_populations=1&multiple_populations=1. Accessed on 15 Feb 2021.
Crawford ED, Petrylak D, Sartor O. Navigating the evolving therapeutic landscape in advanced prostate cancer. Urol Oncol. 2017;35:S1–13.
He L, Fang H, Chen C, Wu Y, Wang Y, Ge H, et al. Metastatic castration-resistant prostate cancer: academic insights and perspectives through bibliometric analysis. Medicine. 2020;99:e19760.
Laccetti AL, Morris MJ, Kantoff PW. A clinical evaluation of enzalutamide in metastatic castration-sensitive prostate cancer: guiding principles for treatment selection and perspectives on research. Onco Targets Ther. 2020;3:13247–63.
Schulte B, Morgans AK, Shore ND, Pezaro C. Sorting through the maze of treatment options for metastatic castration-sensitive prostate cancer. Am Soc Clin Oncol Educ Book. 2020;40:1–10.
Saad F, Efstathiou E, Attard G, Flaig TW, Franke F, Goodman OB Jr, et al. Apalutamide plus abiraterone acetate and prednisone versus placebo plus abiraterone and prednisone in metastatic, castration-resistant prostate cancer (ACIS): a randomised, placebo-controlled, double-blind, multinational, phase 3 study. Lancet Oncol. 2021;22(11):1541–59.
Rizzo A, Mollica V, Cimadamore A, Santoni M, Scarpelli M, Giunchi F, et al. Is there a role for immunotherapy in prostate cancer? Cells. 2020;9(9):2051.
Rizzo A, Santoni M, Mollica V, Fiorentino M, Brandi G, Massari F. Microbiota and prostate cancer. Semin Cancer Biol. 2021. https://doi.org/10.1016/j.semcancer.2021.09.007.
Sha S, Ni L, Stefil M, Dixon M, Mouraviev V. The human gastrointestinal microbiota and prostate cancer development and treatment. Investig Clin Urol. 2020;61(Suppl 1):S43–50.
Mollica V, Rizzo A, Massari F. The pivotal role of TMPRSS2 in coronavirus disease 2019 and prostate cancer. Future Oncol. 2020;16(27):2029–33.
Saad F, Canil C, Finelli A, Hotte SJ, Malone S, Shayegan B, et al. Controversial issues in the management of patients with advanced prostate cancer: results from a Canadian consensus forum. Can Urol Assoc J. 2020;14(4):E137–49.
Gillessen S, Attard G, Beer TM, Beltran H, Bjartell A, Bossi A, et al. Management of patients with advanced prostate cancer: report of the advanced prostate cancer consensus conference 2019. Eur Urol. 2020;77:508–47.
Rosenfeld RM, Nnacheta LC, Corrigan MD. Clinical consensus statement development manual. Otolaryngol Head Neck Surg. 2015;153(2S):S1–14.
Hahn AW, Higano CS, Taplin M, Ryan CJ, Agarwal N. Metastatic castration-sensitive prostate cancer: optimizing patient selection and treatment. Am Soc Clin Oncol Educ Book. 2018;23(38):363–71.
George DJ, Sartor O, Miller K, Saad F, Tombal B, Kalinovsky J, et al. Treatment patterns and outcomes in patients with metastatic castration-resistant prostate cancer in a real-world clinical practice setting in the United States. Clin Genitourin Cancer. 2020;18(4):284–94.
Poppel HV, Klotz L. Gonadotropin-releasing hormone: an update review of the antagonists versus agonists. Int J Urol. 2012;19(7):594–601.
Mason M, Richaud P, Bosnyak Z, Malmberg A, Neijber A. Degarelix versus goserelin plus bicalutamide in the short-term relief of lower urinary tract symptoms in prostate cancer patients: results of a pooled analysis. Low Urin Tract Symp. 2017;9(2):82–8.
Iversen P, Damber J, Malmberg A, Persson BE, Klotz L. Degarelix monotherapy compared with luteinizing hormone-releasing hormone (LHRH) agonists plus anti-androgen flare protection in advanced prostate cancer: an analysis of two randomized controlled trials. Ther Adv Urol. 2016;8(20):75–82.
Hosseini SA, Rajabi F, Akbari Sari A, Ayati M, Heidari S, Ghamary F. Degarelix for the treatment of advanced prostate cancer compared with GnRh-Agonists: a systematic review and meta-analysis. Med J Islam Repub Iran. 2016;9(30):317.
Bahl A, Challapalli A, Masson S, Hilman S, Hurley K, Persad R. A randomized controlled trial to determine the effect of triptorelin on reduction of prostate volume preradiotherapy compared with standard therapy(goserelin). J Clin Oncol. 2016;34(2):30.
Higano CS, Crawford ED, Shore ND. Risk of cardiovascular events with degarelix versus leuprolide after biochemical relapse of prostate cancer: exploratory analysis of a randomized controlled trial. J Clin Oncol. 2015;33(7):151.
Clinton TN, Woldu SL, Raj GV. Degarelix versus luteinizing hormone-releasing hormone agonists for the treatment of prostate cancer. Expert Opin Pharmacother. 2017;18(8):825–32.
Lee S, Lee H, Kim SW, Lee ES, Hong SJ, Kim CS, et al. Is high-dose leuprorelin acetate effective and safe in Asian men with prostate cancer? An open-label, non-comparative, multi-center clinical trial. Yonsei Med J. 2014;55(2):310–5.
Kyriakopoulos CE, Chen Y, Carducci MA, Liu G, Jarrad DF, Hahn NM, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer: long-term survival analysis of the randomized phase 3 E3805 CHAARTED Trial. J Clin Oncol. 2018;36(11):1080–7.
James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR, et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387(10024):1163–77.
Gravis G, Fizazi K, Joly F, Oudard S, Priou F, Esterni B, et al. Androgen-deprivation therapy alone or with docetaxel in non-castrate metastatic prostate cancer (GETUG-AFU 15): a randomized, open-label, phase 3 trial. Lancet Oncol. 2013;14(2):149–58.
Sweeney CJ, Chen Y, Carducci M, Liu G, Jarrad DF, Eisenberger M, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med. 2015;373(8):737–46.
Fizazi K, Tran N, Fein N, Matsubara N, Rodriguez-Antolin A, Alekseev BY, et al. Abiraterone plus prednisone in metastatic, castration-sensitive prostate cancer. N Engl J Med. 2017;377(4):352–460.
James ND, de Bono JS, Gannon M, Clarke N. Abiraterone for prostate cancer not previously treated with hormone therapy. N Engl J Med. 2017;2017(3774):338–51.
Davis ID, Martin AJ, Stockler MR, Begbie S, Chi KN, Chowdhury S, et al. Enzalutamide with standard first-line therapy in metastatic prostate cancer. N Engl J Med. 2019;381(2):121–31.
Armstrong AJ, Szmulewitz RZ, Petrylak DP, Holzbeierlein J, Villers A, Azad A, et al. ARCHES: a randomized, phase 3 study of androgen deprivation therapy eith enzalutamide or placebo in men with metastatic hormone-Sensitive prostate cancer. J Clin Oncol. 2019;37(32):2974–86.
Fizazi K, Tran N, Fein L, Matsubara N, Rodriguez- Antolin A, Alekseev BY, et al. Abiraterone acetate plus prednisone in patients with newly diagnosed high-risk metastatic castration-sensitive prostate cancer (LATITUDE): final overall survival analysis of a randomised, double-blind, phase 3 trial. Lancet Oncol. 2019;20:686–700.
Clarke NW, Ali A, Ingleby FC, Hoyle A, Amos CL, Attard G, et al. Addition of docetaxel to hormonal therapy in low- and high-burden metastatic hormone sensitive prostate cancer: long-term survival results from the STAMPEDE trial. Ann Oncol. 2019;30:1992–2003.
National Comprehensive Cancer Network (NCCN) Guidelines, prostate cancer, 2020. Available at: https://www.nccn.org/professionals/physician_gls/default.aspx#site. Accessed on 15 Feb 2021.
Parker C, Castro E, Fizazi K, Heidenreich A, Ost P, Procopio G, et al. Prostate cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31(9):1119–34.
Zhu Y, Ye D. Chinese expert consensus on the diagnosis and treatment of castration-resistant prostate cancer (2019 update). Cancer Manag Res. 2020;12(2):127–40.
Penson DF, Armstrong AJ, Concepcion R, Agarwal N, Olsson C, Dunshee LK, et al. Enzalutamide versus bicalutamide in castration-resistant prostate cancer: The STRIVE trial. J Clin Oncol. 2016;34(18):2098–106.
Hussain M, Fizazi K, Saad F, Rathenborg P, Shore N, Ferreira U, et al. Enzalutamide in Men with nonmetastatic, castrotion-resistant prostate cancer. N Engl J Med. 2018;378(26):2465–74.
Ryan CJ, Crrawford ED, Shore ND, Underwood W 3rd, Taplin M, Londhe A, et al. The IMAAGEN study: effect of abiraterone acetate and prednsone on prostate specific antigen and radiographic disease progression in patients with nonmetastatic castration resistant prostate cancer. J Urol. 2018;200(2):344–52.
Fizazi K, Shore N, Tammela TL, Ulys A, Vjaters E, Polyakov S, et al. Darolutamide in nonmetastatic, castration-resistant prostate cancer. N Engl J Med. 2019;380(13):1235–46.
Uemura H, Matsushima H, Kobayashi K, Mizusawa H, Nishimatsu H, Fizazi K, et al. Efficacy and safety of darolutamide in Japanese patients with nonmetastatic castration-resistant prostate cancer: a sub-group analysis of the phase III ARAMIS trial. Int J Clin Oncol. 2021;26:578.
Sountoulides P, Rountos T. Adverse effects of androgen deprivation therapy for prostate cancer: prevention and management. ISRN Urol. 2013;2013:240108.
Zhu J, Liao R, Su C, Liang D, Wu J, Qiu K, et al. Toxicity profile characteristics of novel androgen-deprivation therapy agents in patients with prostate cancer: a meta-analysis. Expert Rev Anticancer Ther. 2018;18(2):193–8.
Ferriero M, Mastroianni R, De Nunzio C, Cindolo L, Calabro F, Tema G, et al. Managing lines of therapy in castration-resistant prostate cancer: real-life snapshot from a multicenter cohort. World J Urol. 2020;38(7):1757–64.
Pilon D, Behl AS, Ellis LA, Robitaille M, Lefebvre P, Dawson N. Assessment of real-world central nervous system events in patients with advanced prostate cancer using abiraterone acetate, bicalcutamide, enzalutamide, or chemotherapy. Am Health Drug Benefits. 2017;10(3):143–53.
Charles RJ, Smith MR, Fizazi K. Abiraterone acetate plus prednisone versus placebo plu prednisone in chemotherapy-naïve men with metastatic castration-resistant prostate cancer (COU-AA-302): final overall survival analysis of a randomized, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2015;2:152–60.
Beer TM, Armstrong AJ, Rathkopf DE. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371(5):424–33.
Beer TM, Armstrong AJ, Rathkopf D, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in men with chemotherapy- naïve metastatic castration-resistant prostate cancer: Extended analysis of the phase 3 PREVAIL study. Eur Urol. 2017;17(2):151–4.
Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351(15):1502–12.
Sternberg CN, Castellano D, Daugaard G, Geczi L, Hotte SJ, Mainwaring PN, et al. Abiraterone acetate for patients with metastatic castration-resistant prostate cancer progressing after chemotherapy: final analysis of a multientre, open-label, early-access protocol trial. Lancet Oncol. 2014;15(11):1263–8.
Scher HI, Fizazi K, Saad F, Taplin M, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367(13):1187–97.
de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels J, Kocak I, et al. Prednsione plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomized open-label trial. Lancet. 2010;376:1147–56.
Davies RS, Smith C, Lester JF. Third-line enzalutamide following docetaxel and abiraterone in metastatic castrate-resistant prostate cancer. Anticancer Res. 2016;36(4):1799–803.
de Wit R, de Bono J, Sternberg CN, Fizazi K, Tombal B, Wulfing C, et al. Cabazitaxel versus abiraterone or enzalutamide in metastatic prostate cancer. N Engl J Med. 2019;381(26):2506–18.
Shore ND, Drake CG, Lin DW, Ryan CJ, Stratton KL, Dunshee C, et al. Optimizing the management of castration-resistant prostate cancer patients: a practical guide for clinicians. Prostate. 2020;80(14):1159–76.
Lorente D, Mateo J, Perez-Lopez R, de Bono JS, Attard G. Sequencing of agents in castration-resistant prostate cancer. Lancet Oncol. 2015;16(6):e279–92.
Mezynski J, Pezaro C, Bianchini D, Zivi A, Sandhu S, Thompson E, et al. Antitumour activity of docetaxel following treatment with the CYP17A1 inhibitor abiraterone: clinical evidence for cross-resistance. Ann Oncol. 2012;23(11):2943–7.
Schweizer MT, Zhou XC, Wang H, Bassi S, Carducci MA, Eisenberger MA, et al. The influence of prior abiraterone treatment on the clinical activity of docetaxel in men with metastatic castration-resistant prostate cancer. Eur Urol. 2014;66(4):646–52.
Aggarwal R, Harris A, Formaker C, Small EJ, Molina A, Griffin TW, et al. Response to subsequent docetaxel in a patient cohort with metastatic castration-resistant prostate cancer after abiraterone acetate treatment. Clin Genitourin Cancer. 2014;12(5):e167–72.
Azad AA, Leibowitz-Amit R, Eigl BJ, Lester R, Wells JC, Murray RN, et al. A retrospective, Canadian multi-center study examining the impact of prior response to abiraterone acetate on efficacy of docetaxel in metastatic castration-resistant prostate cancer. Prostate. 2014;74(15):1544–50.
Loriot Y, Bianchini D, Ileana E, Sandhu S, Patrikidou A, Pezaro C, et al. Antitumour activity of abiraterone acetate against metastatic castration-resistant prostate cancer progressing after docetaxel and enzalutamide (MDV3100). Ann Oncol. 2013;24(7):1807–12.
Noonan KL, North S, Bitting RL, Armstrong AJ, Ellard SL, Chi KN. Clinical activity of abiraterone acetate in patients with metastatic castration-resistant prostate cancer progressing after enzalutamide. Ann Oncol. 2013;24(7):1802–7.
Schrader AJ, Boegemann M, Ohlmann CH, Schnoeller TJ, Krabbe LM, Hajili T, et al. Enzalutamide in castration-resistant prostate cancer patients progressing after docetaxel and abirateron. Eur Urol. 2014;65(1):30–6.
Bianchini D, Lorente D, Rodriguez-Vida A, Omlin A, Pezaro C, Ferraldeschi R, et al. Antitumour activity of enzalutamide (MDV3100) in patients with metastatic castration-resistant prostate cancer (CRPC) pre-treated with docetaxel and abiraterone. Eur J Cancer. 2014;50(1):78–84.
Thomsen FB, Røder MA, Rathenborg P, Brsso K, Borre M, Iversen P. Enzalutamide treatment in patients with metastatic castration-resistant prostate cancer progressing after chemotherapy and abiraterone acetate. Scand J Urol. 2014;48(3):268–75.
Badrising S, van der Noort V, van Oort IM, van den Berg HP, Los M, Hamberg P, et al. Clinical activity and tolerability of enzalutamide (MDV3100) in patients with metastatic, castration-resistant prostate cancer who progress after docetaxel and abiraterone treatment. Cancer. 2014;120(7):968–75.
Azad AA, Eigl BJ, Murray RN, Kollmannsberger C, Chi KN. Efficacy of enzalutamide following abiraterone acetate in chemotherapy-naive metastatic castration-resistant prostate cancer patients. Eur Urol. 2015;67(1):23–9.
Pezaro CJ, Omlin AG, Altavilla A, Lorente D, Ferraldeschi R, Bianchini D, et al. Activity of cabazitaxel in castration-resistant prostate cancer progressing after docetaxel and next-generation endocrine agents. Eur Urol. 2014;66(3):459–65.
Sella A, Sella T, Peer A, Berger R, Frank SJ, Gez E, et al. Activity of cabazitaxel after docetaxel and abiraterone acetate therapy in patients with castration-resistant prostate cancer. Clin Genitourin Cancer. 2014;12(6):428–32.
Wissing MD, Coenen JL, van den Berg P, Westgeest HM, van den Eertwegh AJM, van Oort IM, et al. CAST: A retrospective analysis of cabazitaxel and abiraterone acetate sequential treatment in patients with metastatic castrate-resistant prostate cancer previously treated with docetaxel. Int J Cancer. 2015;136(6):E760–72.
Al Nakouzi N, Le Moulec S, Albigès L, Wang C, Beuzeboc P, Gross- Goupil M, et al. Cabazitaxel remains active in patients progressing after docetaxel followed by novel androgen receptor pathway targeted therapies. Eur Urol. 2015;68(2):228–35.
de Bono JS, Chowdhury S, Feyerabend S, Elliott T, Grande E, Melhem-Bertrandt A, et al. Antitumour activity and safety of enzalutamide in patients with metastatic castration-resistant prostate cancer previously treated with Abiraterone acetate plus prednisone for ≥ 24 week in Europe. Eur Urol. 2018;74(1):37–45.
Attard G, Borre M, Gurney H, Loriot Y, Andresen-Daniil C, Kalleda R, et al. Abiraterone alone or in combination with enzalutamide in metastatic castration-resistant prostate cancer with rising prostate-specific antigen during enzalutamide treatment. J Clin Oncol. 2018;36(25):2639–46.
Khalaf D, Annala M, Taavitsainen S, Finh DL, Oja C, Vergidis J, et al. Optimal sequencing of enzalutamide and abiraterone acetate plus prednisone in metastatic castration-resistant prostate cancer: a multicenter, randomized, open-label, phase 2, crossover trial. Lancet Oncol. 2019;20(12):1730–9.
Acknowledgements
Funding
No funding or sponsorship was received for this study. The Rapid Service Fee was funded by Glenmark Pharmaceuticals Limited.
Editorial Assistance
We would like to thank BioQuest solutions for providing editorial assistance. Funded by Glenmark Pharmaceuticals Limited.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors have contributed equally towards the conception, design, drafting, review and approval of manuscript.
Disclosures
Sagar Bhagat, Saiprasad Patil and Hanmant Barkate are employees of Glenmark Pharmaceuticals Ltd. who contributed toward literature search and manuscript writing. The design or procedure of the consensus and the content of the paper are in no way influenced by the grant provider. Chirag Desai, Ashok K Vaid, Ghanashyam Biswas, Sandeep Batra, Palanki S Dattatreya, Prabrajya Narayan Mohapatra, Deepak Dabkara, and Adwaita Gore all have nothing to disclose.
Compliance with Ethics Guidelines
As this was a Delphi-based consensus document, IRB approval was not required. However, all the participants of the study were aware of the objectives of the study and the participants were also aware that the results of the study would be published. Before the start of the consensus procedure, each participant was briefed about the nature of the activity. Consent page to participate was attached as the first page of the electronic sheet shared with all the participants. Only if the participant agreed to participate, then was it possible to move forward and turn to the second page. Participants have given their independent opinion based on their previous experience. The final responses of all participants were auto generated in the form of final percentage and graphs to ensure the protection of participants’ individual data.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Desai, C., Vaid, A.K., Biswas, G. et al. Sequencing of Systemic Therapies in the Management of Advanced Prostate Cancer in India: a Delphi-Based Consensus. Oncol Ther 10, 143–165 (2022). https://doi.org/10.1007/s40487-021-00181-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40487-021-00181-1