Abstract
Background
Darolutamide, an oral androgen receptor inhibitor, has been approved for treating nonmetastatic castration-resistant prostate cancer (nmCRPC), based on significant improvements in metastasis-free survival (MFS) in the ARAMIS clinical trial. Efficacy and safety of darolutamide in Japanese patients are reported here.
Methods
In this randomized, double-blind, placebo-controlled phase III trial, 1509 patients with nmCRPC and prostate-specific antigen (PSA) doubling time ≤ 10 months were randomized 2:1 to darolutamide 600 mg twice daily or matched placebo while continuing androgen deprivation therapy. The primary endpoint was MFS.
Results
In Japan, 95 patients were enrolled and randomized to darolutamide (n = 62) or placebo (n = 33). At the primary analysis (cut-off date: September 3, 2018), after 20 primary end-point events had occurred, median MFS was not reached with darolutamide vs. 18.2 months with placebo (HR 0.28, 95% CI 0.11–0.70). Median OS was not reached due to limited numbers of events in both groups but favored darolutamide in the Japanese subgroup. Time to pain progression, time to PSA progression, and PSA response also favored darolutamide. Among Japanese patients randomized to darolutamide vs. placebo, incidences of treatment-emergent adverse events (TEAEs) were 85.5 vs. 63.6%, and incidences of treatment discontinuation due to TEAEs were 8.1 vs. 6.1%.
Conclusions
Efficacy outcomes favored darolutamide in Japanese patients with nmCRPC, supporting the clinical benefit of darolutamide in this patient population. Darolutamide was well tolerated; however, due to the small sample size, it is impossible to conclude with certainty whether differences in the safety profile exist between Japanese and overall ARAMIS populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, prostate cancer poses a major health issue among men. In 2018, there were an estimated 1,276,106 new diagnoses of, and 358,989 new deaths from, prostate cancer worldwide [1]. In Japan, prostate cancer ranked as the fourth most common cancer in men in 2014 [2]. In 2018, there were an estimated 70,654 new cases of prostate cancer and 12,424 deaths from prostate cancer [3].
Prostate cancer progression is mediated by the androgen receptor signaling pathway [4], and androgen deprivation therapy (ADT) is considered the standard of care for many patients with recurrent disease [5]. Most patients eventually develop resistance to ADT and progress to castration-resistant prostate cancer (CRPC) [6], which is characterized by rising levels of prostate-specific antigen (PSA) despite castrate levels of testosterone [7]. CRPC in the absence of detectable metastases with conventional imaging is classified as nonmetastatic CRPC (nmCRPC) [7]. Of 249,053 Japanese patients with prostate cancer included in the large-scale, Medical Data Vision health claims database, 1236 cases were identified as nmCRPC between 2003 and 2018, although limitations of claims databases may underestimate this proportion (0.50%) [8]. An earlier analysis of population cancer registries from 28 countries reported the 5-year prevalence of nmCRPC in Asia (including Japan, China, India, Russia, and Turkey) as 3% in 2013 [9].
Patients with nmCRPC are at substantial risk of progressing to metastatic CRPC (mCRPC) [5]. In a 2005 study by Smith et al., 33% of patients with nmCRPC developed bone metastases within 2 years of follow-up [10]. Metastatic disease carries a poor prognosis, with shorter overall survival (OS) compared to patients without metastases [11]. Given that the nmCRPC population is largely asymptomatic [12], delaying the development of metastasis and hence maintaining the quality of life in these patients is a key therapeutic goal, especially when treatment beyond ADT may be required.
Apalutamide and enzalutamide are androgen receptor inhibitors approved for the treatment of nmCRPC in combination with ADT [13,14,15,16,17,18]. There were specific treatment-related adverse effects more frequently reported with these agents than with placebo, including fatigue, cognitive impairment, seizures, falls, and fractures. In addition, rash and hypothyroidism were observed with apalutamide, while hypertension and major adverse cardiovascular events were observed with enzalutamide [19, 20].
Darolutamide is a structurally distinct androgen receptor inhibitor [21] approved in combination with ADT for treating men with nmCRPC [22,23,24,25], after demonstrating significantly prolonged metastasis-free survival (MFS) in the primary analysis of the phase III ARAMIS trial (median 40.4 months vs. 18.4 months; hazard ratio (HR) 0.41, 95% confidence interval (CI) 0.34–0.50, P < 0.001; data cut-off September 3, 2018) [26]. Darolutamide also significantly improved OS (HR 0.69, 95% CI 0.53–0.88, P = 0.003) at the final analysis (data cut-off November 15, 2019) [27]. Darolutamide exhibits a favorable safety profile: at the primary analysis, incidences of treatment-emergent adverse events (TEAEs) ≥ 5% were generally similar between darolutamide and placebo groups [26]. Furthermore, the incidence of key adverse events (AEs) known to be associated with second-generation androgen receptor inhibitors, including falls, hypertension, and central nervous system (CNS)-related effects, was similar between treatment groups at the primary and final analyses [26]. The low blood–brain barrier penetration of darolutamide, as observed in rodent models and supported by a neuroimaging study in humans [28, 29], may be associated with a low risk of CNS adverse effects. In addition, patient quality of life was maintained with darolutamide treatment [26, 30], and the risk of clinically relevant drug–drug interactions between darolutamide and comedications used in men with nmCRPC was low [31]. Phase I/II studies of mCRPC also support the tolerability of darolutamide and its low risk of TEAEs [32,33,34] and no differences were observed in safety and pharmacokinetics in Japanese patients relative to Western patients in a small cohort (n = 9) [35].
Here, we evaluated the efficacy and safety of darolutamide in Japanese patients with nmCRPC from pre-planned subgroup analyses of the primary data from the ARAMIS trial (data cut-off September 3, 2018).
Patients and methods
Study design and patients
The design and patient eligibility of this randomized, double-blind, placebo-controlled, phase III trial (NCT02200614) have been reported previously [26]. Briefly, patients aged ≥ 18 years had histologically or cytologically confirmed adenocarcinoma of the prostate, CRPC, a baseline PSA level of ≥ 2 ng/mL, a PSA doubling time (PSADT) of ≤ 10 months, and an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1. Patients were excluded if they had a history of metastatic disease or distant metastases detected by whole body radionuclide bone scan and computed tomography (CT), or magnetic resonance imaging (MRI) of the pelvis, abdomen and chest; presence of pelvic lymph nodes < 2 cm in the short axis below the aortic bifurcation was allowed. Patients with prior seizures or conditions predisposing to seizure were permitted to enter this trial.
The review board at each participating institution approved the trial, which was conducted in compliance with the principles of the Declaration of Helsinki and in accordance with the International Conference on Harmonisation Guidelines for Good Clinical Practice. An independent Data and Safety Monitoring Board reviewed unblinded safety data throughout the trial. All patients provided written informed consent.
Randomization and treatment
Patients were randomized 2:1 to receive darolutamide 600 mg (two tablets of 300 mg) twice daily with food or matched placebo in a double-blind manner. Randomization was stratified by PSADT (≤ 6 vs. > 6 months) and the use of osteoclast-targeted therapy at randomization (yes vs. no). Patients continued treatment until protocol-defined progression, intolerable AEs, or withdrawal of consent. Patients continued receiving ADT (luteinizing hormone-releasing hormone agonist or antagonist) throughout the trial. Patients who initiated a prohibited therapy before confirmation of metastasis were required to discontinue study treatment, and thereafter, were followed for survival status [26].
Assessments
Patient demographics, relevant medical history, and other pertinent clinical conditions were recorded at screening. Vital signs and blood samples for laboratory safety assessments were obtained at the study research center at screening and every scheduled visit (Day 1, Day 15, Day 29, at 16 weeks, and at 16-week intervals thereafter). Serum PSA concentrations and pain [evaluated with the Brief Pain Inventory Short Form (BPI-SF) questionnaire] were assessed at screening, Day 1, Week 16, and at every subsequent visit until the end of study or death. Disease assessments, including evaluation of ECOG performance status, chest, abdomen, and pelvic CT/MRI, and 99mTc bone scintigraphy were performed at screening, Week 16, and at every subsequent 16-week visit. All imaging was evaluated both locally and by blinded independent central review.
Data on TEAEs, including type, severity (according to the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.03), seriousness, and whether they were related to the study treatment according to investigator assessment, were recorded at each visit.
Endpoints
The primary endpoint was MFS, defined as the time from randomization to confirmed evidence of distant metastasis on imaging or death from any cause, whichever occurred first. Secondary endpoints comprised OS, time to pain progression (defined as an increase of ≥ 2 points from baseline as assessed using the BPI-SF questionnaire or start of opioid treatment for cancer pain, whichever occurred first), time to first cytotoxic chemotherapy, and time to first symptomatic skeletal event (SSE; defined as external beam radiation therapy to relieve skeletal symptoms, new symptomatic pathologic bone fracture, the occurrence of spinal cord compression, or tumor-related orthopedic surgical intervention). Exploratory endpoints included time to PSA progression [defined according to Prostate Cancer Working Group 2 (PCWG2) criteria [36]] and PSA response [defined as the percentage of patients who experienced a decline from baseline in the PSA level of ≥ 50% (according to PCWG2 criteria [36]) or ≥ 90%].
Statistical analysis
Statistical analysis of efficacy and safety endpoints in the Japanese patient population was conducted as previously described for the global population [26]. Briefly, MFS, all secondary endpoints, and time to PSA progression were analyzed using a stratified log-rank test. Kaplan–Meier curves, including median survival times and their 95% CI were calculated; the HR was calculated with a Cox proportional-hazards model. The percent of patients with a PSA response was analyzed using the Cochran–Mantel–Haenszel test.
Statistical analysis and subject data listings were performed with SAS® for UNIX (SAS Institute Inc., Cary, NC, USA). Incomplete event occurrence dates were imputed as the earliest possible date.
Efficacy was evaluated in the intention-to-treat population, which comprised all randomized patients. Safety was evaluated in the safety population, which comprised all randomized patients who received at least one dose of any study drug.
Results
Patients
In total, 95 Japanese patients from the ARAMIS overall population (N = 1509) were randomized to darolutamide (n = 62) or placebo (n = 33). The clinical cut-off date for the primary analysis was September 3, 2018. In this subset of Japanese patients, baseline demographics and clinical characteristics were well balanced between treatment groups except for age, primary tumor classification, and use of osteoclast-targeted therapy. More patients were aged ≥ 85 years (19.4 vs. 6.1%) or had T3a disease (40.3 vs. 18.2%), fewer patients used osteoclast-targeted therapy (8.1 vs. 15.2%), and the median time from first prior ADT was longer (64.8 vs. 53.6 months) in the darolutamide group than in the placebo group (Table 1).
The Japanese patient population showed some variation in baseline disease characteristics from the overall global ARAMIS population. Japanese patients tended to be older and had a lower median baseline PSA than the overall ARAMIS population. Compared to the overall ARAMIS population, more Japanese patients had a PSADT ≤ 6 months, ECOG performance status 0, T3a disease, Gleason score ≥ 7, and had received ≥ 2 prior hormonal therapies (Table 1).
The median duration of treatment was 14.8 months (range 0.4–26.1 months) with darolutamide and 10.9 months (range 2.1–18.6 months) with placebo in the Japanese subgroup (Supplementary Table 1). In this study, 93.5% of patients with darolutamide and 93.9% of patients with placebo received ≥ 90% of the planned dose (Supplementary Table 2). Treatment duration and dosage administered were comparable between Japanese and overall ARAMIS populations.
Efficacy
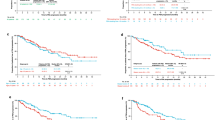
At the time of the primary analysis, 20 MFS events (9 in the darolutamide group, 11 in the placebo group) had been observed. MFS favored darolutamide (HR 0.28; 95% CI 0.11–0.70) in the Japanese subgroup. The median MFS was not reached with darolutamide vs. 18.2 months with placebo (Fig. 1).
At the cut-off date for the primary analysis, median OS was not reached due to the limited number of events in both groups but favored darolutamide in the Japanese subgroup patient population. After 23 pain progression events (13 in the darolutamide group, 10 in the placebo group) occurred, the median time to pain progression was not reached with darolutamide vs. 19.1 months with placebo. Median times to first cytotoxic chemotherapy and the first symptomatic skeletal event also were not reached in either treatment group (Table 2).
Analysis of time to PSA progression was performed after 25 PSA progression events (8 in the darolutamide group, 17 in the placebo group) occurred. The median time to PSA progression was not reached with darolutamide vs. 7.4 months with placebo (Table 2). A clear PSA response at 16 weeks was observed in Japanese patients (Fig. 2); 77.4% of patients with darolutamide vs. 12.1% of patients with placebo achieved a decrease in PSA level from baseline of ≥ 50%, while 43.5% of patients with darolutamide vs. zero patients with placebo attained a ≥ 90% decrease (Table 2).
Waterfall plot of the percentage change in PSA from baseline at Week 16 in Japanese patients treated with darolutamide (a) and placebo (b). PSA prostate serum antigen. Nine patients in the darolutamide group and two patients in the placebo group had missing percentages. For patients who discontinued study treatment prior to Week 16, their PSA results prior to Week 16 were included and summarized
Safety
Overall, AEs were reported by 85.5 and 63.6% of patients receiving at least one dose of darolutamide and placebo, respectively, in the Japanese subgroup (Table 3). Most AEs were Grade 1–2 in severity (56.5% with darolutamide vs. 51.5% with placebo). In Japanese patients, any Grade 3 AE occurred in 25.8% of patients randomized to darolutamide and in 12.1% of those randomized to placebo; all events occurred in only one or two patients each and were not related to any particular organ system (Supplementary Table 3). The incidence of Grade 4 or 5 AEs was comparable between the two arms [two patients with darolutamide (3.2%; one Grade 4 hepatic function abnormality and one Grade 5 influenza) vs. one patient with placebo (3.0%; Grade 4 renal failure)]. Few Grade 3–5 AEs were considered by investigators to be drug-related [one Grade 3 neutropenia, one Grade 3 decreased neutrophil count, and one Grade 4 hepatic function abnormality with darolutamide (4.8%) vs. zero with placebo]. The incidence of serious AEs was higher in patients randomized to darolutamide than those assigned placebo (32.3 vs. 9.1%). TEAEs leading to permanent discontinuation of study drug occurred in 8.1% of patients with darolutamide and in 6.1% of patients with placebo in the Japanese subgroup (Table 3).
In the overall ARAMIS population, among the AEs that occurred in ≥ 5% of patients in either treatment group, constipation, reported as Grade 1–2 severity in all patients, was the only event reported in > 10% of darolutamide-treated patients in the Japanese subgroup (Table 3). With respect to the AEs of interest, bone fracture [seven patients with darolutamide (11.3%) vs. one patient with placebo (3.0%)] and fall [eight patients with darolutamide (12.9%) vs. one patient with placebo 3.0%)] demonstrated the most noticeable difference in incidence rates between darolutamide and placebo in Japanese patients (Table 4). Most fractures and falls were Grade 1 or 2, with only one Grade 3 fall (1.6%) and one Grade 3 fracture (1.6%); none led to dose modification or discontinuation and none were considered to be treatment related. Incidences of other AEs associated with androgen receptor inhibitors were generally comparable between darolutamide and placebo groups, accounting for variability due to small sample size. Seizures, mental impairment disorders, depressed mood disorders, and breast disorders/gynecomastia were not reported with darolutamide or placebo in Japanese patients.
Discussion
In this pre-specified analysis of Japanese patients with nmCRPC in the phase III ARAMIS study, efficacy and safety of darolutamide were generally consistent with the overall ARAMIS population. Differences were noted in baseline and clinical characteristics between the overall ARAMIS population and the small number of patients in the Japanese subgroup, some of which may be related to differences in clinical practice. In contrast to Western clinical practice guidelines, treatment algorithms in Japan include ADT for localized prostate cancer in patients for whom prostatectomy or radiation is not indicated [37, 38]. This may explain the greater number of prior hormonal therapies received by the Japanese subgroup of ARAMIS compared with the overall study population. The Japanese subgroup also included greater proportions of older patients and patients with a higher Gleason score (≥ 7) and/or more advanced primary tumor classification (T3a), in line with other studies of Japanese or Asian patients with nmCRPC [39, 40].
Efficacy outcomes of darolutamide across the small number of patients enrolled and survival events that occurred in the Japanese subgroup were generally comparable with those of the overall ARAMIS population. Darolutamide prolonged MFS in the Japanese subgroup, with a HR of 0.28 (95% CI 0.11–0.70). Although median OS was not reached in the Japanese subgroup, it trended toward favoring darolutamide, with a HR of 0.72 (95% CI 0.12–4.31). Other secondary and exploratory endpoints, including the time to pain progression, time to PSA progression, and PSA response, also favored darolutamide, providing further evidence to support its clinical benefit in Japanese men with nmCRPC.
Darolutamide was well tolerated, with ≥ 93% of patients receiving ≥ 90% of the planned dose in both the Japanese subgroup and the overall ARAMIS population. Safety outcomes of darolutamide in the Japanese population were generally consistent with those of the overall ARAMIS population; similar incidences of any grade AE, Grade 1–2, and Grade 3–4 events, and TEAEs leading to permanent discontinuation of study drug were reported among darolutamide-treated patients. While reports of Grade 5 AEs were approximately 59% lower in the Japanese subgroup compared with those in the overall ARAMIS population, serious AEs occurred more frequently in darolutamide-treated patients in the Japanese subgroup (32.3%) than in the overall ARAMIS population (24.8%). However, the correlation with active study drug was low in the majority of these cases.
Certain differences were noted between Japanese and overall ARAMIS populations with respect to the AEs most frequently reported with darolutamide. Fatigue, which occurred more commonly with darolutamide than placebo in the overall ARAMIS population [26], was similar between treatment arms in the Japanese subgroup. Also, incidences of constipation, falls, and fractures tended to be higher with darolutamide than placebo in the Japanese subgroup but showed no difference between treatment groups in the overall ARAMIS population at primary analysis.
As no remarkable differences in darolutamide pharmacokinetic parameters exist between Japanese and Western patients [35], this is unlikely to account for any potential differences in the safety profile of darolutamide observed in the Japanese and overall ARAMIS populations. The higher incidence of fractures associated with darolutamide in the Japanese subgroup may be related to more elderly patients (aged ≥ 85 years) in the darolutamide group as compared with the placebo group (19.4 vs. 6.1%), since advanced age is a significant risk factor for fracture in men with prostate cancer [41, 42]. In addition, the longer duration of prior ADT in the darolutamide group may have contributed to the higher incidence of fractures, consistent with previous studies demonstrating an association between duration of ADT and fracture risk in both Western and Japanese [41, 43,44,45,46]. As ADT-related fracture risk also may increase with advancing age [47], an additive effect may have been induced by the higher proportion of patients aged ≥ 85 years combined with greater exposure to ADT in the darolutamide group. The difference in age distribution between the treatment arms in the Japanese subgroup also may have contributed to the higher incidence of constipation with darolutamide vs. placebo [48,49,50]. Considered together, the small sample size, small number of AEs observed overall, and differences in duration of exposure to study treatment (14.8 months with darolutamide vs. 10.9 months with placebo), these potential confounding variables suggest that differences in safety between darolutamide and placebo in the Japanese subgroup should be interpreted with caution and further investigations should be considered.
The safety observations described herein may be best understood in the context of tumor extension, age, and chronic comorbidities in the Japanese subgroup. The darolutamide group enrolled more elderly patients and patients with locally advanced cancer compared with the placebo group. The overall median age of the Japanese subgroup was higher than that of the global population, and similarly to the global population, almost all patients had at least one comorbidity. In line with our findings, subgroup analyses of efficacy in Japanese or Asian patients with nmCRPC treated with apalutamide in the phase III SPARTAN trial found the delay in the development of metastases to be consistent with the overall ARAMIS population. In general, safety profiles also aligned with those of the overall trial populations, with few differences such as increased incidence of rash [39], possibly related to ethnicity. Data from Asian patients with nmCRPC in PROSPER have not been published to date. In subgroup analyses of Asian patients with mCRPC treated with enzalutamide in the phase III PREVAIL trial, AEs commonly reported by patients treated with enzalutamide were generally similar to those reported in the overall study population [51, 52] Although a small number of AEs including falls occurred more frequently in the subgroup, the authors highlight that any differences should be interpreted with caution due to the small patient numbers.
In conclusion, improvements in MFS and other efficacy endpoints observed with darolutamide in the Japanese subgroup are generally consistent with the overall ARAMIS population, supporting the clinical benefit of darolutamide in Japanese patients with nmCRPC. Darolutamide was well tolerated in Japanese patients. Given the small number of patients in the Japanese subgroup, it is impossible to conclude with certainty whether differences in the safety profile exist between Japanese and overall ARAMIS populations.
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
National Cancer Center (2019) Latest cancer statistics. https://ganjoho.jp/reg_stat/statistics/stat/summary.html. Accessed 10 Sept 2019
International Agency for Research on Cancer (2018) Japan fact sheet. https://gco.iarc.fr/today/home. Accessed 05 Nov 2020
Montgomery RB, Mostaghel EA, Vessella R et al (2008) Maintenance of intratumoral androgens in metastatic prostate cancer: a mechanism for castration-resistant tumor growth. Cancer Res 68(11):4447–4454. https://doi.org/10.1158/0008-5472.Can-08-0249
Anantharaman A, Small EJ (2017) Tackling non-metastatic castration-resistant prostate cancer: special considerations in treatment. Expert Rev Anticancer Ther 17(7):625–633. https://doi.org/10.1080/14737140.2017.1333903
Luo J, Beer TM, Graff JN (2016) Treatment of nonmetastatic castration-resistant prostate cancer. Oncology 30(4):336–344
Gillessen S, Attard G, Beer TM et al (2020) Management of patients with advanced prostate cancer: report of the advanced prostate cancer consensus conference 2019. Eur Urol 77(4):508–547. https://doi.org/10.1016/j.eururo.2020.01.012
Mori A, Hashimoto K, Koroki Y, Wu DB, Masumori N (2019) The correlation between metastasis-free survival and overall survival in non-metastatic castration resistant prostate cancer patients from the Medical Data Vision claims database in Japan. Curr Med Res Opin 35(10):1745–1750. https://doi.org/10.1080/03007995.2019.1619543
Liede A, Arellano J, Hechmati G, Bennett B, Wong S (2013) International prevalence of nonmetastatic (M0) castration-resistant prostate cancer (CRPC). J Clin Oncol 31(15_suppl):e16052–e16052. https://doi.org/10.1200/jco.2013.31.15_suppl.e16052
Smith MR, Kabbinavar F, Saad F et al (2005) Natural history of rising serum prostate-specific antigen in men with castrate nonmetastatic prostate cancer. J Clin Oncol 23(13):2918–2925. https://doi.org/10.1200/jco.2005.01.529
Norgaard M, Jensen AO, Jacobsen JB et al (2010) Skeletal related events, bone metastasis and survival of prostate cancer: a population based cohort study in Denmark (1999 to 2007). J Urol 184(1):162–167. https://doi.org/10.1016/j.juro.2010.03.034
Mateo J, Fizazi K, Gillessen S et al (2019) Managing nonmetastatic castration-resistant prostate cancer. Eur Urol 75(2):285–293. https://doi.org/10.1016/j.eururo.2018.07.035
European Medicines Agency (2019) Summary of product characteristics: ERLEADA. https://www.ema.europa.eu/en/documents/product-information/erleada-epar-product-information_en.pdf. Accessed 05 Nov 2020
Janssen Ortho LLC (2018) Erleada (apalutamide) US prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/210951s000lbl.pdf. Accessed 05 Nov 2020
Astellas Pharma US Inc (2018) Xtandi (enzalutamide) US prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/203415s014lbl.pdf. Accessed 05 Nov 2020
European Medicines Agency (2019) Summary of product characteristics: XTANDI. https://www.ema.europa.eu/en/documents/product-information/xtandi-epar-product-information_en.pdf. Accessed 05 Nov 2020
Pharmaceuticals and Medical Devices Agency Japan (2013) New drugs approved in financial year 2013. https://www.pmda.go.jp/files/000232771.pdf. Accessed 05 Nov 2020
Pharmaceuticals and Medical Devices Agency Japan (2018) New drugs approved in financial year 2018. https://www.pmda.go.jp/files/000235288.pdf. Accessed 05 Nov 2020
Smith MR, Saad F, Chowdhury S et al (2018) Apalutamide treatment and metastasis-free survival in prostate cancer. N Engl J Med 378(15):1408–1418. https://doi.org/10.1056/NEJMoa1715546
Hussain M, Fizazi K, Saad F et al (2018) Enzalutamide in men with nonmetastatic, castration-resistant prostate cancer. N Engl J Med 378(26):2465–2474. https://doi.org/10.1056/NEJMoa1800536
Moilanen AM, Riikonen R, Oksala R et al (2015) Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies. Sci Rep 5:12007. https://doi.org/10.1038/srep12007
Bayer HealthCare Pharmaceuticals Inc (2019) Nubeqa (darolutamide) US prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/212099Orig1s000lbl.pdf. Accessed 05 Nov 2020
Bayer HealthCare Pharmaceuticals Inc (2020) Nubeqa (darolutamide) Summary of product characteristics. https://www.ema.europa.eu/documents/product-information/nubeqa-epar-product-information_en.pdf. Accessed 05 Nov 2020
Guia da Farmácia (2019) ANVISA aprova novo tratamento para on câncer de próstata. https://guiadafarmacia.com.br/anvisa-aprova-novo-tratamento-para-o-cancer-de-prostata/. Accessed 05 Nov 2020
Bayer Global Investor News (2020) Bayer receives approval for darolutamide in Japan. https://www.investor.bayer.de/en/nc/news/investor-news/investor-news/bayer-receives-approval-for-darolutamide-in-japan/. Accessed 05 Nov 2020
Fizazi K, Shore N, Tammela TL et al (2019a) Darolutamide in nonmetastatic, castration-resistant prostate cancer. N Engl J Med 380(13):1235–1246. https://doi.org/10.1056/NEJMoa1815671
Fizazi K, Shore N, Tammela TL et al (2020) Nonmetastatic, castration-resistant prostate cancer and survival with darolutamide. N Engl J Med 383(11):1040–1049. https://doi.org/10.1056/NEJMoa2001342
Williams S, Mazibuko N, O’Daly O et al (2020) Significant localized reduction in cerebral blood flow (CBF) in regions relevant to cognitive function with enzalutamide (ENZA) compared to darolutamide (DARO) and placebo (PBO) in healthy volunteers. J Clin Oncol 38:abstr 326. https://doi.org/10.1200/JCO.2020.38.6_suppl.326
Zurth C, Sandman S, Trummel D et al (2019) Higher blood–brain barrier penetration of [14C]apalutamide and [14C]enzalutamide compared to [14C]darolutamide in rats using whole-body autoradiography. J Clin Oncol 37(7_suppl):156. https://doi.org/10.1200/JCO.2019.37.7_suppl.156
Fizazi K, Shore ND, Tammela T et al (2019b) Impact of darolutamide (DARO) on pain and quality of life (QoL) in patients (Pts) with nonmetastatic castrate-resistant prostate cancer (nmCRPC). J Clin Oncol 37(15_suppl):5000. https://doi.org/10.1200/JCO.2019.37.15_suppl.5000
Shore N, Zurth C, Fricke R et al (2019) Evaluation of clinically relevant drug–drug interactions with darolutamide in the phase 3 ARAMIS trial for patients with nonmetastatic castration-resistant prostate cancer. Targ Oncol 14(5):527–539. https://doi.org/10.1007/s11523-019-00674-0
Fizazi K, Massard C, Bono P et al (2014) Activity and safety of ODM-201 in patients with progressive metastatic castration-resistant prostate cancer (ARADES): an open-label phase 1 dose-escalation and randomised phase 2 dose expansion trial. Lancet Oncol 15(9):975–985. https://doi.org/10.1016/s1470-2045(14)70240-2
Fizazi K, Massard C, Bono P et al (2017) Safety and antitumour activity of ODM-201 (BAY-1841788) in castration-resistant, CYP17 inhibitor-naive prostate cancer: results from extended follow-up of the ARADES trial. Eur Urol Focus 3(6):606–614. https://doi.org/10.1016/j.euf.2017.01.010
Shore ND, Tammela TL, Massard C et al (2018) Safety and antitumour activity of ODM-201 (BAY-1841788) in chemotherapy-naive and CYP17 inhibitor-naive patients: follow-up from the ARADES and ARAFOR trials. Eur Urol Focus 4(4):547–553. https://doi.org/10.1016/j.euf.2017.01.015
Matsubara N, Mukai H, Hosono A et al (2017) Phase 1 study of darolutamide (ODM-201): a new-generation androgen receptor antagonist, in Japanese patients with metastatic castration-resistant prostate cancer. Cancer Chemother Pharmacol 80(6):1063–1072. https://doi.org/10.1007/s00280-017-3417-3
Scher HI, Halabi S, Tannock I et al (2008) Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol 26(7):1148–1159. https://doi.org/10.1200/JCO.2007.12.4487
Kakehi Y, Sugimoto M, Taoka R, Committee for Establishment of the Evidenced-Based Cinical Practice Guideline for Prostate Cancer of the Japanese Urological Association (2017) Evidenced-based clinical practice guideline for prostate cancer (summary: Japanese Urological Association, 2016 edition). Int J Urol 24(9):648–666. https://doi.org/10.1111/iju.13380
Akaza H, Hinotsu S, Usami M et al (2013) Evaluation of primary androgen deprivation therapy in prostate cancer patients using the J-CAPRA risk score. Prostate Int 1(2):81–88. https://doi.org/10.12954/PI.12016
Mainwaring P, Small E, Uemura H et al (2018) Efficacy and safety of apalutamide (APA) in patients (pts) with nonmetastatic castration-resistant prostate cancer (nmCRPC) from SPARTAN: Asian subpopulation. Ann Oncol. https://doi.org/10.1093/annonc/mdy434.001
Shah R, Botteman M, Waldeck R (2019) Treatment characteristics for nonmetastatic castration-resistant prostate cancer in the United States Europe and Japan. Future Oncol 15(35):4069–4081. https://doi.org/10.2217/fon-2019-0563
Sharma A, Sinha RJ, Singh V et al (2019) Implications of the Fracture Risk Assessment Algorithm for the assessment and improvement of bone health in patients with prostate cancer: a comprehensive review. Turk J Urol 45(4):245–253. https://doi.org/10.5152/tud.2019.11736
Wallander M, Axelsson KF, Lundh D, Lorentzon M (2019) Patients with prostate cancer and androgen deprivation therapy have increased risk of fractures-a study from the fractures and fall injuries in the elderly cohort (FRAILCO). Osteoporos Int 30(1):115–125. https://doi.org/10.1007/s00198-018-4722-3
Beebe-Dimmer JL, Cetin K, Shahinian V et al (2012) Timing of androgen deprivation therapy use and fracture risk among elderly men with prostate cancer in the United States. Pharmacoepidemiol Drug Saf 21(1):70–78. https://doi.org/10.1002/pds.2258
Graham-Steed TR, Soulos PR, Dearing N et al (2014) Development and validation of a prognostic index for fracture risk in older men undergoing prostate cancer treatment. J Geriatr Oncol 5(4):343–351. https://doi.org/10.1016/j.jgo.2014.08.004
Kawahara T, Fusayasu S, Izumi K et al (2016) Bone management in Japanese patients with prostate cancer: hormonal therapy leads to an increase in the FRAX score. BMC Urol 16(1):32. https://doi.org/10.1186/s12894-016-0151-9
Nguyen C, Lairson DR, Swartz MD, Du XL (2018) Risks of major long-term side effects associated with androgen-deprivation therapy in men with prostate cancer. Pharmacotherapy 38(10):999–1009. https://doi.org/10.1002/phar.2168
Thorstenson A, Bratt O, Akre O et al (2012) Incidence of fractures causing hospitalisation in prostate cancer patients: results from the population-based PCBaSe Sweden. Eur J Cancer 48(11):1672–1681. https://doi.org/10.1016/j.ejca.2012.01.035
Gallegos-Orozco JF, Foxx-Orenstein AE, Sterler SM, Stoa JM (2012) Chronic constipation in the elderly. Am J Gastroenterol 107(1):18–25. https://doi.org/10.1038/ajg.2011.349 (quiz 26)
Kubota Y, Iso H, Tamakoshi A (2016) Bowel movement frequency, laxative use, and mortality from coronary heart disease and stroke among Japanese men and women: the Japan Collaborative Cohort (JACC) Study. J Epidemiol 26(5):242–248. https://doi.org/10.2188/jea.JE20150123
Miwa H (2008) Prevalence of irritable bowel syndrome in Japan: Internet survey using Rome III criteria. Patient Prefer Adherence 2:143–147
Kim CS, Theeuwes A, Kwon DD et al (2016) The PREVAIL trial of enzalutamide in men with chemotherapy-naive, metastatic castration-resistant prostate cancer: post hoc analysis of Korean patients. Investig Clin Urol 57(3):174–183. https://doi.org/10.4111/icu.2016.57.3.174
Kim CS, Choi YD, Lee SE et al (2017) Post hoc analyses of East Asian patients from the randomized placebo-controlled PREVAIL trial of enzalutamide in patients with chemotherapy-naive, metastatic castration-resistant prostate cancer. Medicine 96(27):e7223. https://doi.org/10.1097/MD.0000000000007223
Acknowledgements
This study was funded by Bayer AG and Orion Pharma. The authors would like to thank the patients, their families, and all investigators involved in this study. Medical writing support, including assisting authors with the development of the outline and initial draft and incorporation of comments was provided by Charlotte Simpson, PhD, and editorial support, including fact checking, referencing, figure preparation, formatting, proofreading, and submission was provided by Annabel Ola, MSc, both of Scion, London, UK, supported by Bayer AG according to Good Publication Practice guidelines (Link). The Sponsor was involved in the study design, collection, analysis, and interpretation of data, as well as data checking of information provided in the manuscript. However, the ultimate responsibility for opinions, conclusions, and data interpretation lies with the authors.
Author information
Authors and Affiliations
Contributions
KF and MS were involved in the design of the study. Orion and Bayer employees were involved in the design of the study, analysis and interpretation of the data, and also participated in the conduct of the study. All authors contributed to writing and reviewing the report, and collectively made decisions regarding content. All authors had full access to all study data and had final responsibility for the decision to submit the manuscript for publication.
Corresponding author
Ethics declarations
Conflict of interest
Hiroji Uemura has received honoraria from Bayer, Janssen, Astellas, Takeda, and AstraZeneca, and research funding from Astellas and Takeda. Hisashi Matsushima, Kazuki Kobayashi, Hiroya Mizusawa, Hiroaki Nishimatsu, Masahiro Iinuma, Tetsuo Momma, Satoshi Fukasawa, and Tadahiro Kobayashi report no conflicts of interest. Karim Fizazi has received honoraria from, and acted as a consultant for Janssen, Bayer, Astellas, Sanofi, Orion, Curvec, AstraZeneca, Essa, Amgen, and Roche, and has received accommodation or travel expenses from Amgen and Janssen. Matthew Smith has received honoraria from and acted as a consultant for, Amgen, Astellas, Bayer, Clovis, Gilead, Janssen, Eli Lilly, Novartis, and Pfizer. Neal Shore has acted as a consultant for Bayer, Janssen, Tolmar, Ferring, Medivation, Amgen, Pfizer, AstraZeneca, Genentech/Roche, Myovant Sciences, Astellas Pharma, Merck, and Dendreon, and has received honoraria from Bayer, Janssen, Tolmar, Ferring, Medivation, Amgen, Pfizer, AstraZeneca, Genentech/Roche, Myovant Sciences, Astellas Pharma, Merck. Teuvo Tammela has received honoraria from Janssen, and research funding from Bayer, Lidds AB, and Astellas Pharma. Ken-ichi Tabata has received honoraria from Janssen. Nobuaki Matsubara has received honoraria from Chugai Pharmaceutical, MSD, Bayer, Sanofi, and Janssen, and research funding from Chugai Pharmaceutical, MSD, Bayer, Janssen, Astellas, AstraZeneca, Taiho Pharmaceutical, and Pfizer. Hirotsugu Uemura has acted as an advisor for Bayer, Janssen, and Sanofi; has received honoraria from Astellas, AstraZeneca, Bayer, Janssen, MSD, Sanofi, and Takeda; and has received research funding from Astellas, AstraZeneca, Janssen, Ono, Sanofi, Taiho, and Takeda. Mototsugu Oya has received honoraria from Astellas, Sanofi, Janssen, AstraZeneca, and Takeda, and research funding from Astellas. Mutsushi Kawakita has acted as an advisor for Medicaroid Corporation. Iris Kuss is an employee of and holds stocks in Bayer AG. Marie-Aude Le Berre is an employee of Bayer HealthCare. Amir Snapir was an employee of Orion Pharma and is currently an employee of PCI Biotech. Toni Sarapohja is an employee of Orion Pharma. Kazuhiro Suzuki has received honoraria from Bayer, Takeda, Astellas, Daiichi-Sankyo, AstraZeneca, Janssen, and Sanofi, and has received research funding from Takeda, Astellas, Daiichi-Sankyo.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Uemura, H., Matsushima, H., Kobayashi, K. et al. Efficacy and safety of darolutamide in Japanese patients with nonmetastatic castration-resistant prostate cancer: a sub-group analysis of the phase III ARAMIS trial. Int J Clin Oncol 26, 578–590 (2021). https://doi.org/10.1007/s10147-020-01824-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-020-01824-5