Abstract
Padel is a racket sport, combining high-frequency and low-intensity athletic gestures, that has been gaining growing scientific interest in recent years. Musculoskeletal injuries are very common among padel players with an incidence rate of 3 per 1000 h of training and 8 per 1000 matches. To the best of our knowledge, a comprehensive collection describing the most common sonographic findings in padel players with musculoskeletal injuries is lacking in the pertinent literature. In this sense, starting from the biomechanical features of padel-specific gestures we have reported the ultrasonographic patterns of most frequent injuries involving the upper limb, the trunk, and the lower limb. Indeed, comprehensive knowledge of the biomechanical and clinical features of musculoskeletal injuries in padel is paramount to accurately perform a detailed ultrasound examination of the affected anatomical site. So, the present investigation aims to provide a practical guide, simple and ready-to-use in daily practice, to optimize the sonographic assessment of padel players by combining it with the clinical findings and the biomechanical features of athletic gestures.
Similar content being viewed by others
Introduction
Padel is a racket sport following rules and a scoring system similar to tennis. Enclosed synthetic glass and metal court with a size of 20 m × 10 m, allowing the ball to rebound off the lateral and back walls can be considered the main difference with the tennis. This peculiar court with perimetral walls results in specific gestures such as fast-paced lateral movements, quick changes in direction, a high number of overhead shots, and explosive movements toward the net [1].
Musculoskeletal injuries are very common among padel players with an incidence rate of 3 per 1000 h of training and 8 per 1000 matches [2]. A systematic review published by Dahmen et al. in 2023 involving 8 studies with 2022 participants defined an overall prevalence range of injuries in padel of 40%-90%, with the elbow identified as the most frequent anatomical site [2]. In the same year, Tagliafico et al., confirmed the lateral elbow tendinopathy as the most frequent pathological condition affecting the upper limb in padel players through a survey involving 800 subjects [3]. Interestingly, the same authors reported the majority of musculoskeletal injuries were located on the lower limb (N = 49/85), most of which affected the knee joint (N = 16/49) [3].
Priego Quesada et al., in 2018 recruited 80 non-professional padel players and using a self-administered questionnaire described ankle sprain as the most common musculoskeletal injury; and, subacromial-subdeltoid bursitis and lateral epicondylitis as the most frequent pathologies affecting the upper limb [4].
Pérez et al., in 2023 published a retrospective cross-sectional study involving 44 musculoskeletal injuries of 36 players who participated in the World Padel Tour 2021 reporting the muscle injuries of the lower leg as the most common (28.13%) [5]. The same research group also described a higher prevalence of muscle injuries in top-ranked padel players and, tendon injuries in low-ranked players [5].
Based on the aforementioned epidemiological data described above, the present investigation aims to accurately describe common sonographic findings characterizing the musculoskeletal injuries in padel players, starting by the biomechanical features of their specific gestures. Indeed, a comprehensive knowledge of padel-specific movements can be considered paramount in order to perform a detailed sonographic assessment of the affected anatomical site. The upper limb, trunk, and lower limb have been identified as the three main sections of the manuscript. For each of them, biomechanical features of specific gestures and movements have been described and matched with sonographic findings that commonly characterize the corresponding musculoskeletal injuries.
We strongly believe the present research can be considered a useful and practical guide to accurately perform the ultrasound (US) examination in padel players in daily practice.
Upper limb
Shoulder
Biomechanics
The biomechanical function of the subacromial-subdeltoid (SASD) bursa is to protect the underlying tendon tissue from wear by dissipating friction in the anatomical space between the rotator cuff and the overlying coracoacromial arch. The latter can be considered a fat-filled anatomical interface in which the synovial layers of the SASD bursa glide over each other [6].
Anterosuperior impingement syndrome is a common cause of SASD bursitis in racquet sports. Indeed, overhead activities with repetitive movements of abduction and elevation of the humerus over 90 degrees reduce the acromion-humeral space with potential impingement of the rotator cuff and synovial bursa (Table 1) [7]. As previously mentioned, padel is played on a smaller court than tennis, leading to an increase in the frequency of overhead shots taken and the number of combined movements of abduction-external rotation of the shoulder to perform them (Fig. 1) [4]. Among many types of overhead strokes, smash (classic, par 3, and par 4), rulo or roll, vibora, bandeja, cuchilla, gancho and chancletazo are the most frequent. The latter, also known as “a hit with a big flip-flop”, is an aggressive, flat, finishing shot from a player very close to the net when they receive an easy ball to their forehand side. Moreover, the frequent bounces on the perimetral walls cause the ball to rise upwards, away from the ground, several times during a single match favoring the execution of multiple overhead shots. Muñoz et al., in 2022 identified the shoulder as the second most common anatomical site of injury of the upper body, after the elbow, in a cohort of 950 amateur padel players using a specific questionnaire [8].
Combined movements of abduction (over 90 degrees) and external rotation (red dotted circle) of the shoulder (A, B), and elevations (white dotted circle) of the upper limb overhead (C), are very frequently performed during a padel match considering the court’s size and, the upward trajectory of the ball due to the multiple bounces on the perimetral walls
Usually, de-coaptation exercises (e.g., Codman’s pendulum) and strengthening for the humeral head depressor muscles are performed during athletic training by professional padel players to rebalance the force vectors involved in the vertical shoulder movements [9].
Clinical findings
The clinical scenario of SASD bursitis often presents with anterolateral pain of the shoulder exacerbating over 90 degrees of abduction. Padel players with chronic nodular bursitis may also complain of a feeling of painful clicking during the elevation of the upper limb due to the snap of thickened synovial walls of the SASD bursa under the coracoacromial arch [6]. Of note, the snap usually occurs in the intermediate degrees of the shoulder range of motion. On physical examination, the patient commonly presents multiple points of tenderness over the anterior and lateral surface of the deltoid region and a positive painful arch test during active abduction of the shoulder [9].
Sonographic findings
Anechoic effusion inside the lumen of the SASD bursa is the most common sonographic finding in cases of acute and sub-acute exudative bursitis (Fig. 2). Depending on the position of the patient during the US examination, the effusion may distribute mainly in the lateral portion of the bursa (tear sign) or in its medial portion at the level of the coracoid space mimicking an articular effusion involving the subscapular recess of the glenohumeral joint [10]. In the chronic phase of anterolateral shoulder impingement, a hypoechoic proliferation of the synovial layers can be observed floating within the effusion – i.e., hypertrophic bursitis [9]. Accurately setting the color/power Doppler by adjusting the size/position of the box and the pulse repetition frequency, hypervascularization can be sometimes depicted within the hypertrophic synovial tissue of the bursa (Fig. 2) [11].
In the acute phase, the effusion (yellow asterisks) is the most common sonographic finding defining exudative bursitis (A). Progressively, synovial hypertrophy (B) with hypervascularization (white arrowhead) and fibrotic septae (yellow arrowhead) can develop within the bursal cavity (C). Adhesive bursopathy (D) shows a well-defined, hypoechoic, nodular thickening (green arrowhead) of the synovial tissue (white asterisk) close to the overlying hyperechoic coracoacromial ligament (L). HH humeral head, RC rotator cuff, PD power Doppler
A third sonographic pattern of SASD bursitis is known as adhesive bursopathy, referring to a thickening of the bursal walls greater than 3 mm with or without nodular formations (Fig. 2) [6]. In the authors’ experience, this type of SASD bursitis is the most challenging to diagnose especially for beginners considering the absence of effusion that acts as a natural contrast agent to easily visualize the bursal walls. Unlike the hypertrophic type, adhesive bursopathy usually does not show hyperemia at color/power Doppler.
Lastly, a dynamic ultrasound assessment can be performed to promptly visualize the eventual snapping or pinching of the SASD bursa under the coracoacromial arch [12].
Elbow
Lateral elbow tendinopathy
Biomechanics
Lateral elbow tendinopathy, also known as lateral epicondylitis or tennis elbow, typically involves the extensor carpi radialis brevis (ECRB) tendon due to microtrauma from repetitive backhand strokes, particularly with the one-handed technique [2]. Of note, expert and novice players use different techniques to perform backhand strokes. Expert players hit the ball with a hyperextended wrist and keep the wrist extended throughout impact (Fig. 3); instead, novice players strike the ball with a flexed wrist and, move the wrist into further flexion throughout impact leading the common extensor tendon (CET) of the elbow to progressive eccentric stress [13]. For this reason, novice players are more prone to lateral elbow tendinopathy if compared to expert players.
The repeated contraction of the forearm extensor muscles and the corresponding mechanical overload of the proximal origin of the ECRB tendon over the lateral epicondyle (LE) results in micro-tearing of the tendon tissue with subsequent failure of the healing process and angiofibroblastic degeneration (i.e., tendinosis) [14].
Other biomechanical aspects representing potential risk factors of lateral tendinopathy in padel players are the repetitive varus stresses of the elbow; and, the continuous rubbing of the ECRB tendon against the lateral edge of the capitellum, coupled with its compression between the extensor carpi radialis longus muscle and the underlying bone, during the extension phase of the elbow or to perform specific gestures and strokes such as the backhand or the backhand volley (Table 1) [15].
Lastly, the high number of vibrations, originating from the padel racket at the ball contact due to hard materials, seems to be proximally transmitted to the CET increasing the risk of tendinopathy. In this sense, a soft racket core and anti-vibration systems should be considered to optimize its technical features. Indeed, the density of core materials (rubber core, foam core, hybrid core, etc.) highly influences the control and power of the racket [16].
Clinical findings
Pain or burning around the LE, often radiating along the dorsal surface forearm, are the most common symptoms complained by the athlete. Both are usually triggered or exacerbated by active contraction of the common extensor mass of the forearm which puts tension on the corresponding tendon at the elbow. Weakness in gripping may also be referred by the patient. Severe tenderness by palpating the origin of the ECRB tendon can be considered the most common clinical finding during physical examination. Cozen’s test, Maudsley’s test, and forearm supination with the elbow in the extended position are clinical tests aiming to reproduce lateral elbow pain [17].
Direct compression of the posterolateral surface of the radial head, coupled with passive pronation/supination of the forearm, can be performed to test the eventual presence of radiohumeral synovitis and/or radial head chondropathy mimicking the lateral elbow tendinopathy [18].
Sonographic findings
Ultrasound assessment of the lateral elbow compartment is usually performed with the elbow flexed to 90 degrees and the forearm pronated. Angiofibroblastic hyperplasia, also known as tendinosis, is the most common sonographic finding in padel players with lateral elbow pain. Hypoechoic thickening of the CET and disappearance of the normal fibrillar pattern in the longitudinal view is its typical appearance (Fig. 4) [14]. Combining the transverse plane with the longitudinal one the exact portion of the common tendinous mass affected by the degenerative changes can be accurately identified to plan a tailored rehabilitation approach [19]. Using color/power Doppler the vascular pattern of degenerated tendon tissue due to the local proliferation of neovessels can be assessed by accurately setting the size of the Doppler box, the gain, and the pulse repetition frequency [11]. Hypervascularization of the CET usually presents larger and horizontally oriented vessels (feeding vessels) running in the subcutaneous tissue and, smaller vertically oriented vessels (penetrating vessels) that creep into the tendon tissue [14].
Hypoechoic thickening (white asterisk) of the CET in B-Mode (A) and neo-vessels (yellow arrowheads) in color/power Doppler (B) are the most common sonographic findings in padel players with lateral elbow tendinopathy. Focal injury (white arrows) of the CET (C) and calcific depositions (white arrowheads) can also be identified especially in players with recalcitrant lateral elbow pain (D). LE lateral epicondyle, RH radial head, PD power Doppler
Focal tendinosis of the CET can be coupled with partial injury of the tendon tissue, calcific deposits (Fig. 4), bony spur of the lateral epicondyle, and irregularities of the tendon-bone interface in padel players with lateral elbow pain [20,21,22]. The latter is also defined as mechanical enthesopathy and usually presents irregularities of the cortical bone of the lateral epicondyle, lamellar calcifications of the tendon collagen fibers, and hypervascularization of the hypoechoic cartilaginous plate of the tendon-bone interface [14, 23].
Medial elbow tendinopathy
Biomechanics
Medial elbow tendinopathy is commonly known as golfer’s elbow. Degenerative changes of the common flexor-pronator tendon (CFPT) are usually related to the overload of the pronator teres and flexor carpi radialis muscles [24]. Considering the small size of the padel court, the number of shots from the halfway point of the court and at the net is much higher compared to other sports racquet as tennis (Table 1) [25]. These shots are often performed with an explosive combination of wrist flexion and forearm pronation to smash the ball to the ground with maximal power – the “whipping” effect such as in the smash, especially the par 3 smash (Fig. 5). Moreover, the global torsional movement of the upper limb resulting from the simultaneous wrist flexion and forearm pronation allows the athlete to optimize the trajectory of the ball targeting a specific segment of the opposite half of the court. In this sense, unlike lateral elbow tendinopathy, medial tendinopathy is more common in professional padel players rather than in novice players due to the aforementioned specific gestures frequently and massively involving the flexor and pronator muscles of the forearm.
By rapidly activating the pronator teres and flexor carpi radialis muscles, a sudden flexion of the wrist (yellow arrow) coupled with complete pronation of the forearm (white curved arrow) can be performed by elite padel players—the “whipping” effect (A, B). The aforementioned gestures result in a global torsional movement of the upper limb pivotal to increase the power/velocity of the ball and control its trajectory (C)
Moreover, rapid pronation of the forearm during the forehand stroke is performed by the padel player, by rolling the racket face over the ball via the area of contact, to generate a topspin effect on the ball. Likewise, by pronating the wrist on the backhand the slice spin effect is generated. In this sense, repetitive and explosive contractions of the pronator teres muscle are pivotal to performing shots that put the opponent in difficulty. Lastly, some padel-specific shots such as the vibora and the bandeja – as well as the forehand and forehand volley—may lead to excessive mechanical stresses of the CFPT of the elbow.
Clinical findings
Medial elbow tendinopathy is characterized by pain of insidious onset, which is worsened by resisted forearm pronation and wrist flexion. Tenderness to palpation usually occurs over the medial epicondyle and, distally along the muscular belly of pronator teres and the flexor carpi radialis [26]. The authors strongly suggest also performing a 30-degree valgus stress test of the elbow to assess the ulnar collateral ligament that in pathological conditions can be considered the “big mime” of medial tendinopathy [26].
Sonographic findings
The most common sonographic pattern in padel players with medial elbow pain is characterized by hypoechoic thickening of the CFPT with loss of fibrillar pattern (i.e., tendinosis) with or without intra-tendinous and peri-tendinous hypervascularization (Fig. 6). As previously mentioned for the CET, also the tendinosis of CFPT can be coupled with partial injury, calcific deposits, bony spur of the medial epicondyle, and enthesopathy of the tendon-bone junction [26, 27].
Hypoechoic thickening (white arrowhead) of the conjoint tendon (CT) in B-Mode (A) with neo-vessels (yellow arrowheads) penetrating the degenerated tendon tissue in power Doppler (PD) (B) are common sonographic findings in padel players with medial elbow pain. More rarely, a small bony fragment (yellow arrow) embedded in the ulnar collateral ligament (ucl) and surrounded by an intense hypervascularization (C) can be observed close to the painful medial epicondyle (ME). Of note, a small ossicle (white arrow) within the collagen fibers of the ulnar collateral ligament (ucl), commonly rounded in shape and not encircled by neo-vessels, can be identified also in asymptomatic volunteers (D). U ulna, CD color Doppler
In padel players with recalcitrant medial elbow pain and poor response to conservative treatments focused on the tendon compartment, eventual sonographic abnormalities of the ulnar collateral ligament should be scrutinized. A small bony fragment linear-in-shape with hypervascularization of the surrounding soft tissues is a quite frequent pathological finding exactly located in the most painful site complained by the patient (Fig. 6). Of note, a dome-shaped ossicle can be normally identified within the ulnar collateral ligament of the elbow also in asymptomatic athletes (Fig. 6) and should not be misinterpreted as the pathological and painful bony fragment previously mentioned. In this sense, the different shape of the hyperechoic formation (linear vs. dome-shaped), and the abundant vascular signals surrounding the painful bony fragment but not the physiological ossicle can be considered a pivotal sonographic signs for the differential diagnosis.
Wrist
Biomechanics
Repetitive ulnar and radial deviations of the wrist during the padel match to orientate the racquet and hit the ball may overload the wrist extensor tendons, especially the first and sixth compartments largely involved in these movements (Fig. 7). Likewise, rapid and repeated torsional movements of the wrist (“screwing” effect) to optimize the trajectory of the ball, produce topspin and slice spin effects, and force the stroke require violent contractions of the forearm muscles tensioning the corresponding tendons (Table 1).
Four are the traditional single-handed grip positions of the racket in padel: the continental, Eastern, semi-Western, and Western grips. Each hand grip position of the racket offers unique advantages and disadvantages, influencing the load to the wrist during gameplay. Interestingly, the Eastern grip, often preferred by expert padel players to increase the power of both forehand and backhand strokes and impart top-spin effects to the ball, particularly overloads the first extensor tendon compartment of the wrist – i.e., the abductor pollicis longus and extensor pollicis brevis [28]. Anatomically, the wrist extensor compartments are stabilized by an inverted U-shape fibrous retinaculum and, present a tenosynovial sheath surrounding the tendons to promote their smooth gliding. In this sense, tenosynovitis, tendinosis, and focal injury are the most common pathological changes involving the aforementioned tendons in padel players [29].
Lastly, repetitive flexion and extension of the wrist may also lead to extra frictions between the first and second (extensor carpi radialis brevis and extensor carpi radialis longus) compartment 4 cm proximally to the radiocarpal joint – i.e., the proximal intersection syndrome.
Clinical findings
Pain, focal swelling, and snapping are the most common clinical findings on the radial or ulnar side of the wrist related to the first and sixth tendon compartments respectively. Clinical tests by passively moving the wrist in a radial or ulnar direction (e.g., Finkelstein's maneuver) may provoke and/or exacerbate the aforementioned symptoms confirming the diagnosis. In chronic cases, synovial adhesions and retinacular hypertrophy can markedly impair the tendon gliding with a reduced active and passive wrist range of motion in different spatial planes.
Sonographic findings
Tendon sheath effusion, tenosynovial hypertrophy, retinacular thickening, tendinosis, and partial injury of tendon tissue are the most common sonographic findings in wrist extensor tendons compartments of padel players (Fig. 8) [30, 31]. The presence of a vertical fibrous septum within the first compartment is often related to a “selective” synovitis involving the sheath of extensor pollicis brevis tendon and not the abductor pollicis longus tendon [32]. The color/power Doppler, especially in the acute phase, shows hypervascularization mainly involving the synovial tissue of the tendon sheath and, more rarely the tendon tissue itself.
Thickening of the fibrous retinaculum (yellow arrowhead), sheath effusion (white asterisks), tenosynovial hypertrophy (white arrowhead) with hypervascularization of the first extensor compartment is visualized in a padel player with radial wrist pain (A, B). Likewise, tenosynovitis of the extensor carpi ulnaris tendon with multiple vascular signals within the hypertrophic synovial sheath (white arrowhead) can be observed on the ulnar side (C, D). Rad radius, A artery, V vein, PD power doppler, Ul ulna, Tri triquetrum, L lunate, 5M fifth metacarpal bone
Dynamic ultrasound assessment can be performed on padel players with feelings of painful clicks at the wrist. The most common sonographic findings are the instability of extensor carpi ulnaris tendon at the ulnar bony groove and, the snapping of the first extensor tendons compartment due to the entrapment within the thickened osteofibrous tunnel [33].
Aberrant vascular signals in the anatomical interface between the first and second extensor compartment, peri tendinous anechoic edema, and a painful sono-palpation of the intersectional area are the typical sonographic signs in athletes with proximal intersection syndrome of the wrist [34, 35]. Sometimes, local effusion can be confined inside a proper synovial neo-bursa located in between the tendons [36].
Trunk
Biomechanics
Overhead strokes in padel require a great power of core muscles. Most of the overhead shots previously described are characterized by an early phase necessary to store the energy in the abdominal muscles; and, a late phase with rapid and violent release of the elastic energy to hit the ball as hard as possible (Fig. 9) [37]. The loading phase is characterized by hyperextension of the spine—with progressive elongation of the rectus abdominis muscles (eccentric contraction)—coupled with a twist of the trunk. In this way, elastic energy is stored in the trunk’s walls like a “spring mechanism”. Instead, during the impact phase, the abdominal muscles contract forcefully generating an abrupt flexion and rotation of the trunk to force the ball to the opposite side of the court with the maximal energy and velocity (Table 1). Indeed, the trunk acts as a functional bridge transmitting the forces from the lower limbs to the upper limbs. Especially in the acceleration phase of the trunk, the rectus and oblique abdominal muscles contralateral to the service side are exposed to a high risk of traumatic injury due to an explosive concentric contraction [37, 38].
The transition from the loading to impact phase of overhead strokes during a Padel match requires a very rapid and explosive change of the shape of the core (red dotted lines). Indeed, an eccentric contraction of abdominal muscles to control the hyperextension of the spine (A) is immediately followed by powerful concentric contractions to flex and rotate the trunk (B) transmitting the forces from the lower to upper limbs
Clinical findings
Pain, local ecchymosis, and loss of function/strength are the most common findings in patients with abdominal wall muscle injuries during the physical examination [38, 39]. For the rectus abdominis muscle, active contractions by flexing the thoracolumbar spine and/or its elongation during the spinal hyperextension can be considered additional clinical maneuvers to trigger local pain along the anterior surface of the abdominal wall. Likewise, active twisting of the trunk combined with lateral bending of the spine can be performed to test the oblique abdominal muscles [40]. The Valsalva maneuver can be used to increase the intra-abdominal pressure tensioning the corresponding abdominal wall muscles. In the authors’ experience, especially in low-energy trauma and small-size myofascial injuries, the clinical tests are not accurate enough to evoke pain and accurately localize the anatomical site of injury.
Sonographic findings
The most common US findings are myofascial injuries due to indirect trauma (Fig. 10) [38]. A sonographic classification commonly used in clinical practice defines three main grades of severity for myofascial injuries after indirect trauma [41]: Grade 1: US examination may be either negative or exhibit focal/diffuse areas of increased echogenicity of the muscle tissue. The latter are related to the local edema and/or a micro-bleeding infiltrating the muscle tissue. Grade 2: US imaging shows areas of muscle fiber disruption with blood collections. Of note, in grade 2 the injury does not involve the entire cross-sectional area of the target muscle but only a part of it (partial tear). Grade 3: complete discontinuity or disruption of the target muscle with retraction of the corresponding muscle fibers (full-thickness tear).
Combining transverse (A, B) and longitudinal (C) scans, a focal injury (white arrowhead) involving the superficial fibers of rectus abdominis muscle (RA)—with a mild peri-lesional hypervascularization (B) in power Doppler (PD)—can be observed in a professional padel player due to a powerful overhead stroke with massive contraction of the core muscles. Instead, a full-thickness tear (yellow arrowheads) of the rectus abdominis (RA) with blood collections (white asterisks) within the muscle belly can be visualized in transverse sonograms of an amatorial padel player (D, E). Of note, the longitudinal scan (F) confirms the anatomical integrity of the deep lamina of its fascial sheath (blue arrowhead). sc subcutaneous tissue
In some athletes, and especially in the early phases after the trauma, the hyperechogenicity due to the acute bleeding can make the diagnosis of muscle injury quite challenging. In this sense, dynamic ultrasound examination with passive elongation and/or active contraction of the target muscle can be considered a powerful diagnostic tool to “open the gap” and promptly confirm the disruption of muscle tissue [42].
During the sonographic assessment of the rectus abdominis muscle, the structural integrity of its connective (hyperechoic) sheath should be accurately checked. Indeed, especially the deep lamina of the muscular sheath is widely crossed by perforating branches of the epigastric vessels, and; after a sport-related trauma, a rectus sheath hematoma should be considered among the potential complications [39].
Shifting the probe laterally to the rectus abdominis muscle the external oblique, internal oblique, and transverse abdominis muscles can be visualized. The internal oblique muscle can be injured during an extreme and unbalanced eccentric contraction to twist the trunk—the so-called “side strain syndrome” (Fig. 11) [43].
Comparative ultrasound scanning, in a transverse plane, of the normal (A, B) and painful (C) side of the anterolateral abdominal wall clearly shows a massive thickening and hyperechogenicity of the left internal oblique muscle (IO) due to severe intramuscular edema with a loss of the normal echotexture. Shifting the probe distally (D), disruption of its muscle fibers with a large intramuscular hematoma (yellow asterisk) has been identified confirming the post-traumatic myofascial injury with a sparing of the overlying external oblique muscle (EO). TA transversus abdominis muscle, RA rectus abdominis muscle
Lower limb
Knee
Biomechanics
Considering the small size of the court and the presence of perimeter walls involving vertical bounces, the trajectories of the ball during a padel match lead the athlete to perform extremely rapid changes of direction and abrupt braking to reach it [1]. So, the knee extensor mechanism mainly composed of the quadriceps muscle and tendon, the patella, and the patellar tendon (PT) is pivotal to dynamically stabilizing the knee during the multiple valgus/rotatory stresses (Table 1). Moreover, the landing phase of jumps involves an eccentric load on the PT on the knee and the Achilles tendon at the ankle to accurately control the braking of the lower limb on the ground (Fig. 12).
Rapid combined knee flexion-rotation movements (white dotted circle) are often necessary to correctly orientate the trunk and hit the ball at the optimal height (A). The patellar tendon (yellow arrow) and Achilles tendon (green arrow) function as shock absorber cords during the landing phase of the jump (black dotted arrow) modulating the velocity of braking and reducing the risk of knee/ankle sprain (B)
Clinical findings
Anterior knee pain, mainly localized at the inferior pole of the patella, is the main clinical finding complained by the padel player with patellar tendinopathy. In the early phase, the pain is triggered by intense workouts or specific sports gestures; but, progressively if not properly managed, it can present also at rest or during common movements such as rising from a chair or climbing the stairs [44]. The most painful site on palpation during physical examination is the inferior edge of the patella where the proximal segment of PT is inserted. The maximal flexion can evoke anterior knee pain putting in tension the PT and mechanically stressing its enthesis to the inferior pole of the patella. Lastly, the athlete may be asked to perform a functional test as the squat – at different degrees of knee flexion—which can evoke pain in both the eccentric and concentric phases of the exercise.
Sonographic findings
The most common sonographic finding in padel players with patellar tendinopathy is the hypoechoic thickening of the inferior and proximal fibers of PT with loss of the fibrillar pattern. Intratendinous calcific deposits and abnormalities of the tendon-bone interface are commonly associated with the aforementioned sonographic signs of tendinosis (Fig. 13). The latter sonographic sign, clinically known as mechanical enthesopathy, is usually characterized by the pitting of the cortical bone of the inferior pole of the patella and thin linear in shape enthesophytes [45]. In doubtful cases, dynamic sonographic assessment with active extension of the knee can be performed to optimize the differential diagnosis between the focal tendinosis and the partial tear of the deep fibers of PT [46].
Normally (A), the patellar tendon presents a fibrillar echotexture in the longitudinal scan; instead, a hypoechoic thickening of the deep and proximal fibers (white asterisk), lamellar calcifications (yellow arrowhead), and cortical irregularities (white arrowhead) of the inferior pole of the patella (Pat) can be commonly observed in padel players with patellar tendinopathy (B). The color Doppler (CD) depicts neo-vessels (C) originating from the Hoffa fat pad (FP) and infiltrating the hypoechoic degenerated tendon tissue (white asterisk). More rarely, an isolated longitudinal tear of the PT (green arrowhead) can be identified with a regular enthesis (orange arrowhead) (D)
Using the color/power Doppler hypervascularization can be observed with neo-vessels usually originating from the underlying Hoffa fat pad and invading the degenerated tendon tissue. Indeed, in the pertinent literature, the US-guided disruption of the neo-vessels/neo-nerves crossing the tendon-fat pad interface has been proposed as an interventional technique to manage chronic recalcitrant patellar tendinopathy (i.e., the US-guided scraping of PT) [47].
Posterior leg
Biomechanics
Ankle plantarflexion coupled with a simultaneous and abrupt extension of the knee implies an active contraction and passive stretching of the gastrocnemius muscle. The aforementioned mix of elongation and contraction is a well-known biomechanical risk factor for myofascial/myotendinous injury of the medial gastrocnemius muscle (MGM) [48, 49]. The aforementioned biomechanical mechanism is very common during a padel match to rapidly change direction and to rise from the ground performing the so-called jump shots (Table 1). Specifically, during the take-off phase of a jump, an explosive contraction of the triceps surae is coupled with the knee extension to increase as much as possible the distance from the ground. Likewise, during the landing phase, the triceps surae contracts during passive dorsiflexion of the ankle and with the knee slightly flexed to optimize the braking and modulate the impact of the lower limb to the ground (Fig. 14). In this sense, in both the aforementioned phases the MGM actively contracts during its passive elongation – i.e., eccentric loads. Tagliafico et al., have reported 85 cases of MGM injuries in a cohort of 800 padel players [3]. The authors defined injury of the MGM as the second most common musculoskeletal disorder in this specific population after lateral elbow tendinopathy. Also known as tennis leg, this musculoskeletal injury can show an extremely variable histological/anatomical damage involving the muscle tissue of the medial gastrocnemius, its anterior aponeurosis, its free aponeurosis, and the posterior aponeurosis of the soleus muscle – i.e., the myo-aponeurotic complex of the triceps surae [48].
Powerful contraction of the triceps surae and extension of the knee (yellow arrow) are key biomechanical factors during the take-off phase of the jump (black dotted arrow) to reach the ball (A). Likewise, during the landing phase of the jump (white dotted arrow), contraction of the gastrocnemius muscle with the knee slightly flexed (yellow arrow) allows soft braking protecting the ankle from an excessive mechanical overload (B)
Clinical findings
Sudden pain in the calf and eventual feeling of “pop” are the most common symptoms complained by the player in the acute phase. Active/passive elongation of the gastrocnemius muscle elicits pain in the posterior compartment of the leg; and, the patient is usually unable to perform the single-leg heel raise test [50]. In the sub-acute phase, the calf tightens up and sometimes a local hematoma can be observed along the posteromedial surface of the leg extending to the medial compartment of the ankle. Interestingly, especially in patients with small-size injuries of the MGM or in cases of deeply located blood effusion; no superficial hematoma can be visually identified during the physical examination.
Sonographic findings
As previously mentioned, sonographic signs of MGM injuries in padel players can be highly variable, involving the muscle tissue proper and/or its external connective scaffold. Post-traumatic discontinuity of its anterior aponeurosis implies a spilling of the hematoma within the intermuscular septum progressively dilatating the inter aponeurotic space between the MGM and the soleus muscle (Fig. 15) [48]. In padel players with a moderate to severe inter aponeurotic hematoma, the authors strongly suggest ultrasound-guided drainage coupled with rehabilitation treatments to avoid a progressive organization of the blood effusion with the development of (soft) granulation tissue [51]. Moreover, in patients with inter aponeurotic hematoma, and aponeurotic disruption involving more than 50% of the cross-sectional area of the muscle measured in a transverse plan; asynchronous movements between the MGM and soleus have been demonstrated during dynamic scanning—with plantarflexion and dorsiflexion of the ankle—with a longer return to play [51]. Lastly, disruption of its free aponeurosis can be histologically considered a tendinous injury with a worse prognosis and longer rehabilitation management for the return to play (Fig. 15) [48].
A small injury of the anterior aponeurosis (white arrowhead) of the medial gastrocnemius (MG) is enough to allow the blood to spill within the inter aponeurotic space (green arrowhead) of the triceps surae muscle (A). Instead, post-traumatic disruption of deep fibers of its free aponeurosis (white asterisk), with sparing of superficial fibers (yellow arrowhead), should be considered such as a tendon injury (B) with a worse functional prognosis compared to the previous myoaponeurotic lesion. In padel athletes with a large hematoma (yellow asterisks) in the inter aponeurotic space of the triceps surae muscle (C) ultrasound-guided drainage is paramount to avoid progression toward an irregular mass of granulation tissue (white dotted line) that “blocks” a correct healing process (D). Sol soleus muscle
Foot
Biomechanics
As previously mentioned for the PT and MGM, repetitive concentric and eccentric loads during the take-off and landing phases of the jump shots can be considered repetitive mechanical stresses on the Achilles tendon (AT) during a padel match (Fig. 14) [52]. The take-off phase requires a powerful plantar forefoot thrust with the knee extended to increase the distance from the ground as much as possible optimizing the so-called elevation performance. Likewise, during the landing phase, the AT acts as an elastic spring curbing the ankle dorsiflexion approaching the ground (Fig. 14). The latter biomechanical mechanism is paramount to avoid ankle sprains with violent dorsiflexion and loss of balance landing phase from the jump.
Moreover, the multiple rapid directional changes due to the irregular ball bouncing off the perimetral walls of the playing field may lead to extra friction between the AT and the surrounding elastic sleeve (paratenon) with a higher risk of peri tendinitis compared to tennis. Indeed, overuse syndromes of the gastrocnemius muscle lead to a repetitive overstretch of the crural fascia with thickening/inflammation of the underlying paratenon [53].
Clinical findings
Non-insertional Achilles tendinopathy
The most common clinical finding by inspecting the AT is the presence of a fusiform thickening usually located from 2 to 6 cm proximally to its calcaneal insertion. The squeeze test by pinching the tendon thickening with two fingers of the hand often reproduces the pain. Stiffness of the gastrocnemius-soleus complex during passive stretching is another frequent complaint by the athlete especially in chronic cases. Sometimes, by placing the hand over the AT and asking the patient for active movements of the ankle, a grinding sensation can be felt called crepitus [54]. The latter clinical sign may be related to the presence of local adhesions in the AT-paratenon gliding interface.
Insertional Achilles tendinopathy
The pain is mainly located at the attachment site of AT over the posterior aspect of the calcaneus. Active/passive elongation of the tendon can be used as a clinical test to increase the mechanical stress to the enthesis and reproduce the painful feeling. The presence of tenderness over the medial and lateral aspect of the insertional segment of AT may be related to the presence of deep retrocalcaneal bursitis [55]. Likewise, a painful pinching of the skin covering the distal portion of AT may be related to superficial retrocalcaneal bursitis. In some padel athletes, a bump can be identified at this level related to the presence of intra-tendinous calcification and/or bony spur of the calcaneus.
Achilles tendon rupture
The acute rupture of the AT usually onsets with severe pain and the inability to fully load the affected lower limb or walk on tiptoe [56]. The player presents impairment in walking losing the normal phases of rolling the foot on the ground. Physical examination may reveal a weakness in plantar flexion of the ankle, a positive Thompson’s test, and in some patients a soft spot along the course of the AT. Epidemiologically, the Achilles tendon rupture presents a bimodal distribution with a first peak commonly occurring in patients aged 25–40 years and a second peak in those older than 60 years [57]. Interestingly, in the first group of patients, the tendon rupture is often secondary to high-energy sport-relates trauma; instead, in the second group, low-energy trauma can be sufficient to trigger a tendon injury considering the pre-existing chronic Achilles tendinosis.
Sonographic findings
Achilles tendinopathy can be considered a generic medical definition that encompasses an extremely variable cluster of histological changes. Among many, midportion tendinosis, peri tendinitis, partial tear, enthesopathy, and superficial/deep retrocalcaneal bursitis are the most common. In padel players, very often several sono-histological changes coexist making the Achilles tendinopathy a real challenge for the clinician/surgeon.
Non-insertional Achilles tendinopathy
Hypoechoic thickening of the tendon is the most common sonographic finding in padel players with non-insertional Achilles tendinopathy (Fig. 16). Loss of the fibrillar pattern in the longitudinal plane, and a rounded shape in the transverse plane, are typical signs of focal tendinosis at this level. Color/power Doppler often shows neo-vessels originating from the underlying Kager fat pad and invading the degenerated segment of the AT (Fig. 16). Of note, neo-nerves are coupled with neo-vessels and seem to play a pivotal role in the genesis of tendon pain through a neurogenic inflammation mechanism [58]. Another common sonographic finding is the hypoechoic thickening of the paratenon, coupled with the midportion Achilles tendinosis or (more rarely) as a unique sonographic sign. Longitudinally the peri tendinitis simply appears as a hypoechoic band in between the subcutaneous tissue and the dorsal surface of the AT; instead, in a transverse plane it presents an inverted U-shape surrounding the dorsal, medial, and lateral aspects of the tendon [59]. Using high-sensitive color/power Doppler and accurately setting the pulse repetition frequency, hypervascularization surrounding the AT can be observed especially in players with acute peri tendinitis (Fig. 16).
Fusiform hypoechoic thickening (white arrowheads) of the midportion of AT and its hypervascularization with neo-vessels (yellow arrowheads) originating from the underlying Kager fat pad (FP) can be considered the most common sonographic signs of non-insertional pathology (A–C). More rarely, isolated peri tendinitis may be identified with vascular signals (blue arrowheads) confined inside the thickened paratenon and a normal thickness/echotexture of the underlying AT (D). In players with suspected partial injury of the AT, ankle dorsiflexion may be performed to dynamically and selectively glide the disrupted tendon fibers (white asterisks) confirming the diagnosis (E). CD color doppler, PD power doppler
Lastly, midportion Achilles tendinosis if not accurately managed may progress to mechanical disruption of tendon fibers – i.e., partial or complete tear. Proximal/distal stump usually presents a glove finger shape and, dynamic scanning can be promptly performed to “open the gap” optimizing its visibility [60]. Sometimes a linear hyperechoic fibrillar structure may be observed crossing the space in between the stumps of AT which represents the plantaris tendon [61].
Insertional Achilles tendinopathy
Posterosuperior calcaneal bony spur is a very frequent sonographic finding in both symptomatic and asymptomatic padel players; instead, hypoechoic thickening of the insertional segment of AT, with coarse pattern and loss of fibrillar texture, seems to be a more specific sign of painful insertional tendinopathy (Fig. 17) [62]. Unlike the aforementioned midportion tendinopathy, color/power Doppler often reveals penetrating neo-vessels originating from the subcutaneous fat tissue rather than to the Kager fat pad in the insertional tendinopathy. Partial tendon injury, intra-tendinous calcifications, and enthesophyte of the tendon-bone interface may also be observed [63].
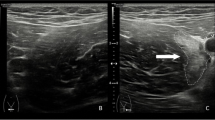
Comparative scanning (A, B) shows bilaterally the posterosuperior bony spur (bS) of calcaneus but, the hypoechoic thickening of the insertional portion of AT (yellow arrowhead) only on the painful side. The color/power Doppler (CD) confirms the presence of neo-vessels (white arrowhead) originating from the subcutaneous fat and penetrating the tendon tissue selectively on the painful heel (C). In another padel player with heel pain, the B-mode scan (D) showed effusion in the deep retrocalcaneal bursa (b), and color Doppler (CD) confirmed its hypervascularization (yellow arrow) (E). Interestingly, hyperemia also involves the superficial retrocalcaneal bursa (white arrow) and the underlying tendon tissue (E). Cal calcaneus
Effusion of the deep retrocalcaneal bursa is another common sonographic finding in padel players (Fig. 17) but, as the calcaneal spur, may be observed also in asymptomatic players. In this sense, the authors strongly suggest to perform always a comparative scanning of this anatomical region to better match to each other the clinical and ultrasonographic signs. Moreover, rather than the bursal effusion in M-mode, hyperemia of the synovial bursal walls in color/power Doppler seems to be a more specific sonographic sign of painful retrocalcaneal bursitis.
The superficial retrocalcaneal bursa is squeezed between the AT and superficial soft tissues so very rarely can be observed distended due to effusion. Usually, bursitis at this level shows hypoechoic thickening of the synovial lining with hypervascularization on color/power Doppler (Fig. 17) [64]. This anatomical structure, often overlooked, presents the highest density of nociceptors in patients with insertional Achilles tendinopathy compared to the tendon itself, the bone of calcaneus, and the deep retrocalcaneal bursa [65] In this sense, considering its pivotal role as a pain generator, some authors have also proposed the ultrasound-guided injection or debridement of the superficial bursal tissue [62].
Conclusion
Musculoskeletal injuries are very common among padel players and a detailed knowledge of biomechanical features of padel-specific gestures is pivotal to performing a detailed sonographic assessment of the affected anatomical site. To the best of our knowledge, a head-to-head comparison between sport-specific movements and the corresponding sonographic findings is lacking in the pertinent literature, also considering the growth and diffusion recent of this sport. In this sense, the present research is intended as a ready-to-use guide to accurately perform the US examination in Padel players in daily practice.
Abbreviations
- US:
-
Ultrasound
- SASD:
-
Subacromial-subdeltoid
- ECRB:
-
Extensor carpi radialis brevis
- CET:
-
Common extensor tendon
- LE:
-
Lateral epicondyle
- CFPT:
-
Common flexor-pronator tendon
- PT:
-
Patellar tendon
- MGM:
-
Medial gastrocnemius muscle
- AT:
-
Achilles tendon
References
García-Giménez A, de la Fuente FP, Otín CC, Páez LC (2022) Performance outcome measures in padel: a scoping Review. Int J Environ Res Public Health 19:4395
Dahmen J, Emanuel KS, Fontanellas-Fes A, Verhagen E, Kerkhoffs GMMJ, Pluim BM (2023) Incidence, prevalence and nature of injuries in padel: a systematic review. BMJ Open Sport Exerc Med 9(2):e001607. https://doi.org/10.1136/bmjsem-2023-001607
Tagliafico AS, Torri L, Righetto R (2023) Injuries in non-professional padel tennis players. Results of a survey of the Italian Federation of Tennis in Liguria, Italy. J Sports Med Phys Fitn 63(4):566–569. https://doi.org/10.23736/S0022-4707.22.14280-5
Priego Quesada JI, Sanchís Almenara M, Kerr ZY, Alcantara E (2018) Examination of the risk factors associated with injured recreational padel players in Spain. J Sports Med Phys Fitn 58(1–2):98–105. https://doi.org/10.23736/S0022-4707.16.06729-3
Pérez F, Rubia A, Cañadas E, Lorenzo-Calvo J, Marquina M, García-Sánchez C (2023) Musculoskeletal injury prevalence in professional padel players. A retrospective study of the 2021 season. Phys Ther Sport 63:9–16. https://doi.org/10.1016/j.ptsp.2023.06.003
Ricci V, Galletti S, Chang KV, Özçakar L (2020) Ultrasound imaging and guidance in the management of adhesive bursopathy of the shoulder: a video demonstration. J Ultrasound Med 39(3):633–635. https://doi.org/10.1002/jum.15117
Allen H, Chan BY, Davis KW, Blankenbaker DG (2019) Overuse injuries of the shoulder. Radiol Clin North Am 57(5):897–909. https://doi.org/10.1016/j.rcl.2019.03.003
Muñoz D, Coronado M, Robles-Gil MC, Martín M, Escudero-Tena A (2022) Incidence of upper body injuries in amateur padel players. Int J Environ Res Public Health 19(24):16858. https://doi.org/10.3390/ijerph192416858
Ricci V, Mezian K, Chang KV, Özçakar L (2022) Clinical/sonographic assessment and management of calcific tendinopathy of the shoulder: a narrative review. Diagnostics (Basel) 12(12):3097. https://doi.org/10.3390/diagnostics12123097
Ricci V, Mezian K, Naňka O, Özçakar L (2022) Assessing/imaging the subcoracoid space: from anatomy to dynamic sonography. J Ultrasound Med 41(9):2149–2155. https://doi.org/10.1002/jum.15898. (PMID: 34845753)
Ricci V, Ricci C, Tamborrini G, Chang KV, Mezian K, Zunica F, Naňka O, Kara M, Özçakar L (2023) From histology to sonography in synovitis: EURO-MUSCULUS/USPRM approach. Pathol Res Pract 241:154273. https://doi.org/10.1016/j.prp.2022.154273
Ricci V, Chang KV, Güvener O, Mezian K, Kara M, Leblebicioğlu G, Stecco C, Pirri C, Ata AM, Dughbaj M, Jain NB, Özçakar L (2022) EURO-MUSCULUS/USPRM dynamic ultrasound protocols for shoulder. Am J Phys Med Rehabil 101(3):e29–e36. https://doi.org/10.1097/PHM.0000000000001833
Blackwell JR, Cole KJ (1994) Wrist kinematics differ in expert and novice tennis players performing the backhand stroke: implications for tennis elbow. J Biomech 27(5):509–516. https://doi.org/10.1016/0021-9290(94)90062-0
Ricci V, Cocco G, Mezian K, Chang KV, Naňka O, Tamborrini G, Kara M, Özçakar L (2023) Anatomy and sonographic examination for lateral epicondylitis: EURO-MUSCULUS/USPRM approach. Am J Phys Med Rehabil 102(4):300–307. https://doi.org/10.1097/PHM.0000000000002090
Bunata RE, Brown DS, Capelo R (2007) Anatomic factors related to the cause of tennis elbow. J Bone Jt Surg Am 89(9):1955–1963. https://doi.org/10.2106/JBJS.F.00727
Blanes C, Correcher A, Beltrán P, Mellado M (2022) Identifying the inertial properties of a padel racket: an experimental maneuverability proposal. Sensors (Basel) 22(23):9266. https://doi.org/10.3390/s22239266
Ahmad Z, Siddiqui N, Malik SS, Abdus-Samee M, Tytherleigh-Strong G, Rushton N (2013) Lateral epicondylitis: a review of pathology and management. Bone Jt J 95-B(9):1158–1164. https://doi.org/10.1302/0301-620X.95B9.29285
Arrigoni P, Cucchi D, Menon A, Randelli P (2017) It’s time to change perspective! New diagnostic tools for lateral elbow pain. Musculoskelet Surg 101(Suppl 2):175–179. https://doi.org/10.1007/s12306-017-0486-8
Ricci V, Schroeder A, Özçakar L (2020) Ultrasound imaging for lateral elbow pain: pinpointing the epicondylosis. Am J Phys Med Rehabil 99(6):560–561. https://doi.org/10.1097/PHM.0000000000001253
Kotnis NA, Chiavaras MM, Harish S (2012) Lateral epicondylitis and beyond: imaging of lateral elbow pain with clinical-radiologic correlation. Skeletal Radiol 41(4):369–386. https://doi.org/10.1007/s00256-011-1343-8
Walz DM, Newman JS, Konin GP, Ross G (2010) Epicondylitis: pathogenesis, imaging, and treatment. Radiographics 30(1):167–184. https://doi.org/10.1148/rg.301095078
Levin D, Nazarian LN, Miller TT, O’Kane PL, Feld RI, Parker L, McShane JM (2005) Lateral epicondylitis of the elbow: US findings. Radiology 237(1):230–234. https://doi.org/10.1148/radiol.2371040784
Ricci V, Mezian K, Cocco G, Tamborrini G, Fari G, Zunica F, Chang KV, Kara M, Özçakar L (2023) Ultrasonography for injecting (Around) the lateral epicondyle: EURO-MUSCULUS/USPRM perspective. Diagnostics (Basel) 13(4):717. https://doi.org/10.3390/diagnostics13040717
Ricci V, Güvener O, Chang KV, Wu WT, Mezian K, Kara M, Leblebicioğlu G, Pirri C, Ata AM, Dughbaj M, Jain NB, Stecco C, Özçakar L (2022) EURO-MUSCULUS/USPRM dynamic ultrasound protocols for elbow. Am J Phys Med Rehabil 101(6):e83–e92. https://doi.org/10.1097/PHM.0000000000001915
Demeco A, de Sire A, Marotta N, Spanò R, Lippi L, Palumbo A, Iona T, Gramigna V, Palermi S, Leigheb M, Invernizzi M, Ammendolia A (2022) Match analysis, physical training, risk of injury and rehabilitation in padel: overview of the literature. Int J Environ Res Public Health 19(7):4153. https://doi.org/10.3390/ijerph19074153
Ciccotti MC, Schwartz MA, Ciccotti MG (2004) Diagnosis and treatment of medial epicondylitis of the elbow. Clin Sports Med 23(4):693–705. https://doi.org/10.1016/j.csm.2004.04.011
Konarski W, Poboży T, Poboży K, Domańska J, Konarska K (2023) Current concepts of natural course and in management of medial epicondylitis: a clinical overview. Orthop Rev (Pavia) 9(15):84275. https://doi.org/10.52965/001c.84275
García-Fernández P, Guodemar-Pérez J, Ruiz-López M et al (2019) Epidemiology of injuries in professional and amateur Spanish paddle players. Rev Int Med Cienc Act Fís Deport 19:641–654
Castillo-Lozano R, Casuso-Holgado MJ (2017) Incidence of musculoskeletal sport injuries in a sample of male and female recreational paddle-tennis players. J Sports Med Phys Fitn 57(6):816–821. https://doi.org/10.23736/S0022-4707.16.06240-X
Mezian K, Ricci V, Jačisko J, Sobotová K, Angerová Y, Naňka O, Özçakar L (2021) Ultrasound imaging and guidance in common wrist/hand pathologies. Am J Phys Med Rehabil 100(6):599–609. https://doi.org/10.1097/PHM.0000000000001683
Sole JS, Wisniewski SJ, Newcomer KL, Maida E, Smith J (2015) Sonographic evaluation of the extensor carpi ulnaris in asymptomatic tennis players. PM R 7(3):255–263. https://doi.org/10.1016/j.pmrj.2014.08.951
Corvino A, Lonardo V, Corvino F, Tafuri D, Pizzi AD, Cocco G (2023) “Daddy wrist”: a high-resolution ultrasound diagnosis of de Quervain tenosynovitis. J Clin Ultrasound 51(5):845–847. https://doi.org/10.1002/jcu.23440
Mezian K, Ricci V, Güvener O, Jačisko J, Novotny T, Kara M, Ata AM, Wu WT, Chang KV, Stecco C, Pirri C, Leblebicioğlu G, Özçakar L (2022) EURO-MUSCULUS/USPRM dynamic ultrasound protocols for wrist and hand. Am J Phys Med Rehabil 101(9):e132–e138. https://doi.org/10.1097/PHM.0000000000002005
Montechiarello S, Miozzi F, D’Ambrosio I, Giovagnorio F (2010) The intersection syndrome: ultrasound findings and their diagnostic value. J Ultrasound 13(2):70–73. https://doi.org/10.1016/j.jus.2010.07.009
Ricci V, Özçakar L (2019) Life after ultrasound: are we speaking the same (or a new) language in physical and rehabilitation medicine? J Rehabil Med 51(3):234–235. https://doi.org/10.2340/16501977-2527
Draghi F, Bortolotto C (2014) Intersection syndrome: ultrasound imaging. Skeletal Radiol 43(3):283–287. https://doi.org/10.1007/s00256-013-1786-1
Maquirriain J, Ghisi JP, Kokalj AM (2007) Rectus abdominis muscle strains in tennis players. Br J Sports Med 41(11):842–848. https://doi.org/10.1136/bjsm.2007.036129
Draghi F, Cocco G, Richelmi FM, Schiavone C (2020) Abdominal wall sonography: a pictorial review. J Ultrasound 23(3):265–278. https://doi.org/10.1007/s40477-020-00435-0
Cocco G, Ricci V, Boccatonda A, Stellin L, De Filippis G, Soresi M, Schiavone C (2021) Sonographic demonstration of a spontaneous rectus sheath hematoma following a sneeze: a case report and review of the literature. J Ultrasound 24(2):125–130. https://doi.org/10.1007/s40477-020-00493-4
Grevious MA, Cohen M, Shah SR, Rodriguez P (2006) Structural and functional anatomy of the abdominal wall. Clin Plast Surg 33(2):169–179. https://doi.org/10.1016/j.cps.2005.12.005
Peetrons P (2002) Ultrasound of muscles. Eur Radiol 12(1):35–43. https://doi.org/10.1007/s00330-001-1164-6
Mezian K, Ricci V, Güvener O, Jačisko J, Novotný T, Kara M, Chang KV, Naňka O, Pirri C, Stecco C, Dughbaj M, Jain NB, Özçakar L (2022) EURO-MUSCULUS/USPRM dynamic ultrasound protocols for (Adult) hip. Am J Phys Med Rehabil 101(11):e162–e168. https://doi.org/10.1097/PHM.0000000000002061
Maquirriain J, Ghisi JP (2006) Uncommon abdominal muscle injury in a tennis player: internal oblique strain. Br J Sports Med 40(5):462–463. https://doi.org/10.1136/bjsm.2005.023457
Warden SJ, Brukner P (2003) Patellar tendinopathy. Clin Sports Med 22(4):743–759. https://doi.org/10.1016/s0278-5919(03)00068-1
Cocco G, Ricci V, Villani M, Delli Pizzi A, Izzi J, Mastandrea M, Boccatonda A, Naňka O, Corvino A, Caulo M, Vecchiet J (2022) Ultrasound imaging of bone fractures. Insights Imaging 13(1):189. https://doi.org/10.1186/s13244-022-01335-z
Pirri C, Stecco C, Güvener O, Mezian K, Ricci V, Jačisko J, Novotný T, Kara M, Chang KV, Dughbaj M, Jain NB, Özçakar L (2023) EURO-MUSCULUS/USPRM dynamic ultrasound protocols for knee. Am J Phys Med Rehabil 102(5):e67–e72. https://doi.org/10.1097/PHM.0000000000002173. (PMID: 36729007)
Hall MM, Rajasekaran S (2016) Ultrasound-guided scraping for chronic patellar tendinopathy: a case presentation. PM R 8(6):593–596. https://doi.org/10.1016/j.pmrj.2015.10.013
Pedret C, Balius R, Blasi M, Dávila F, Aramendi JF, Masci L, de la Fuente J (2020) Ultrasound classification of medial gastrocnemious injuries. Scand J Med Sci Sports 30(12):2456–2465. https://doi.org/10.1111/sms.13812
Flecca D, Tomei A, Ravazzolo N, Martinelli M, Giovagnorio F (2007) US evaluation and diagnosis of rupture of the medial head of the gastrocnemius (tennis leg). J Ultrasound 10(4):194–198. https://doi.org/10.1016/j.jus.2007.09.007
Garrick JG, Couzens GS (1992) Tennis leg. Phys Sportsmed 20(5):203–207. https://doi.org/10.1080/00913847.1992.11947439
Yoon ES, Lin B, Miller TT (2021) Ultrasound of musculoskeletal hematomas: relationship of sonographic appearance to age and ease of aspiration. AJR Am J Roentgenol 216(1):125–130. https://doi.org/10.2214/AJR.19.22752
Gheidi N, Kernozek TW (2019) The effects of both jump/land phases and direction on Achilles tendon loading. J Sports Med Phys Fitness 59(10):1684–1690. https://doi.org/10.23736/S0022-4707.19.09428-3
Stecco C, Cappellari A, Macchi V, Porzionato A, Morra A, Berizzi A, De Caro R (2014) The paratendineous tissues: an anatomical study of their role in the pathogenesis of tendinopathy. Surg Radiol Anat 36(6):561–572. https://doi.org/10.1007/s00276-013-1244-8
Paavola M, Järvinen TA (2005) Paratendinopathy. Foot Ankle Clin 10(2):279–292. https://doi.org/10.1016/j.fcl.2005.01.008
Weinfeld SB (2014) Achilles tendon disorders. Med Clin North Am 98(2):331–338. https://doi.org/10.1016/j.mcna.2013.11.005
Park SH, Lee HS, Young KW, Seo SG (2020) Treatment of acute Achilles tendon rupture. Clin Orthop Surg 12(1):1–8. https://doi.org/10.4055/cios.2020.12.1.1
Nillius SA, Nilsson BE, Westlin NE (1976) The incidence of Achilles tendon rupture. Acta Orthop Scand 47(1):118–121. https://doi.org/10.3109/17453677608998983
Wasker SVZ, Challoumas D, Weng W, Murrell GAC, Millar NL (2023) Is neurogenic inflammation involved in tendinopathy? A systematic review. BMJ Open Sport Exerc Med 9(1):e001494. https://doi.org/10.1136/bmjsem-2022-001494
Stecco A, Busoni F, Stecco C, Mattioli-Belmonte M, Soldani P, Condino S, Ermolao A, Zaccaria M, Gesi M (2015) Comparative ultrasonographic evaluation of the Achilles paratenon in symptomatic and asymptomatic subjects: an imaging study. Surg Radiol Anat 37(3):281–285. https://doi.org/10.1007/s00276-014-1338-y
Özçakar L, Ricci V, Mezian K, Pirri C (2022) A New and dedicated video gallery: EURO-MUSCULUS/USPRM protocols for dynamic ultrasound examination of the joints. Am J Phys Med Rehabil 101(3):201–202. https://doi.org/10.1097/PHM.0000000000001956
Smith J, Alfredson H, Masci L, Sellon JL, Woods CD (2017) Differential plantaris-Achilles tendon motion: a sonographic and cadaveric investigation. PM R 9(7):691–698. https://doi.org/10.1016/j.pmrj.2016.10.013. (PMID: 27789336)
Chimenti RL, Stover DW, Fick BS, Hall MM (2019) Percutaneous ultrasonic tenotomy reduces insertional Achilles tendinopathy pain with high patient satisfaction and a low complication rate. J Ultrasound Med 38(6):1629–1635. https://doi.org/10.1002/jum.14835
Chimenti RL, Chimenti PC, Buckley MR, Houck JR, Flemister AS (2016) Utility of ultrasound for imaging osteophytes in patients with insertional Achilles tendinopathy. Arch Phys Med Rehabil 97(7):1206–1209. https://doi.org/10.1016/j.apmr.2015.12.009
Alfredson H, Spang C (2020) Surgical treatment of insertional Achilles tendinopathy: results after removal of the subcutaneous bursa alone-a case series. BMJ Open Sport Exerc Med 6(1):e000769. https://doi.org/10.1136/bmjsem-2020-000769
Andersson G, Backman LJ, Christensen J, Alfredson H (2017) Nerve distributions in insertional Achilles tendinopathy - a comparison of bone, bursae and tendon. Histol Histopathol 32(3):263–270. https://doi.org/10.14670/HH-11-790
Acknowledgements
We thank the professional padel player Lorenzo Di Giovanni for the photos used in this manuscript representing the sport-specific gestures of the padel. His contribution was also paramount in the detailed description of the biomechanical features of athletic movements provided in the present manuscript.
Funding
Open access funding provided by Università Parthenope di Napoli within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Informed consent
Written permission was obtained from the patients.
Consent for publication
The work described has not been published previously, it is not under consideration for publication elsewhere, its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out, and, if accepted, it will not be published elsewhere in the same form, in English or in any other languages, including electronically without the written consent of the copyright- holder.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cocco, G., Ricci, V., Corvino, A. et al. Musculoskeletal disorders in padel: from biomechanics to sonography. J Ultrasound (2024). https://doi.org/10.1007/s40477-023-00869-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40477-023-00869-2