Abstract
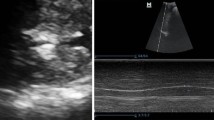
Spinal muscular atrophy with respiratory distress type 1 (SMARD1, OMIM #604,320), is a rare autosomal recessive disease resulting from degeneration of motor neurons in the anterior horns, which leads irreversible diaphragmatic palsy and progressive distal symmetrical muscular weakness. Respiratory distress is the main symptom and is severe, rapidly progressive, and frequently requiring invasive ventilation. Despite diaphragm being one of the target organ of the disease, no specific study has been done using ultrasound.We report diaphragm and lung ultrasound findings of a 13-month-old girl affected by SMARD1 (homozygosis c.1540G > A mutation in IGHMPB2 gene) with respiratory failure requiring permanent mechanical ventilation since birth and we discuss the role of diaphragmatic and lung ultrasound in this category of patients and its clinical implications.

Similar content being viewed by others
References
Saladini M, Nizzardo M, Govoni A et al (2020) Spinal muscular atrophy with respiratory distress type 1: clinical phenotypes, molecular pathogenesis and therapeutic insights. J Cell Mol Med 24(2):1169–1178
Vanoli F, Rinchetti P, Porro F, Parente V, Corti S (2015) Clinical and molecular features and therapeutic perspectives of spinal muscular atrophy with respiratory distress type 1. J Cell Mol Med 19:2058–2066
Ullmann N, D’Andrea ML, Gioachin A et al (2020) Lung ultrasound: a useful additional tool in clinician’s hands to identify pulmonary atelectasis in children with neuromuscular disease. PediatrPulmonol 55(6):1490–1494
Buonsenso D, Supino MC, Giglioni E et al (2018) Point of care diaphragm ultrasound in infants with bronchiolitis: A prospective study. PediatrPulmonol 53:778–786
Buonsenso D, Berti B, Palermo C, et al (2020) Ultrasound assessment of diaphragmatic function in type spinal muscular atrophy. PediatrPulmonol 55(7):1781-1788
Harlaar L, Ciet P, van der Ploeg AT et al (2018) Imaging of respiratory muscles in neuromuscular disease: a review. NeuromusculDisord 28:246–256
Fayssoil A, Behin A, Ogna A et al (2018) Diaphragm: pathophysiology and ultrasound imaging in neuromuscular disorders. J Neuromuscul Dis 5(1):1–10
Baldwin CE, Paratz JD, Bersten AD (2011) Diaphragm and peripheral muscle thickness on ultrasound: intra-rater reliability and variability of a methodology using non-standard recumbent positions. Respirology 16(7):1136–1143
Dubé BP, Dres M, Mayaux J, Demiri S, Similowski T, Demoule A (2017) Ultrasound evaluation of diaphragm function in mechanically ventilated patients: comparison to phrenic stimulation and prognostic implications. Thorax 72(9):811–818
Testa A, Soldati G, Giannuzzi R, Berardi S, Portale G, GentiloniSilveri N (2011) Ultrasound M-mode assessment of diaphragmatic kinetics by anterior transverse scanning in healthy subjects. Ultrasound Med Biol 37(1):44–52
Musolino AM, Tomà P, Supino MC et al (2020) Lung ultrasound features of children with complicated and non-complicated community acquired pneumonia: a prospective study. PediatrPulmonol 54:1479–1486
Tomà P (2020) Lung ultrasound in pediatric radiology - cons. PediatrRadiol 50:314–320
Buonsenso D, De Rose C, Morello R, Lazzareschi I, Valentini P (2020) Aspiration pneumonia in children with neurological disorders: a new indication for lung ultrasound? A case series. J Ultra. https://doi.org/10.1007/s40477-020-00520-4
Berce V, Tomazin M, Gorenjak M, Berce T, Lovrenčič B (2019) The usefulness of lung ultrasound for the aetiological diagnosis of community-acquired pneumonia in children. Sci Rep 9(1):17957
Joshi P, Vasishta A, Gupta M (2019) Ultrasound of the pediatric chest. Br J Radiol 92(1100):20190058
Lovrenski J (2020) Pediatric lung ultrasound - pros and potentials. PediatrRadiol 50(3):306–313
Funding
Nothing to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Nothing to declare.
Ethical statement
The study was approved by the Institutional Review Board and Ethic Committee (prot.36173/19 ID2729).
Informed consent
Written informed consent was obtained from a parent or guardian before data collection.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Berti, B., Buonsenso, D., De Rose, C. et al. Point-of-care lung and diaphragm ultrasound in a patient with spinal muscular atrophy with respiratory distress type 1. J Ultrasound 25, 395–398 (2022). https://doi.org/10.1007/s40477-021-00584-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-021-00584-w