Abstract
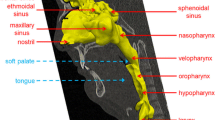
Human pleural cavity pressure rises substantially because of Valsalva maneuver during sneezing. However, the deformations in the upper airway respiratory system significantly increase due to flow rate growth in sneezing, and laryngeal fracture can be mentioned as one of the symptoms of this severe deformation during the Valsalva maneuver. Therefore, the accurate study of the distribution of pressure and velocity, in this case, is very important. In the present study, using a real human upper airway model, the pressure and velocity of the air flow, generated in the tract during the sneezing, have been investigated. Moreover, using a spirometer device, the outlet flow rate from the mouth during the sneezing was obtained. The simulation results indicated that the inlet pressure to the tract, existing in the bronchus region, reached a maximum of 14 kPa. By having such pressure input, the highest deformation, created in the upper airway, was calculated using the fluid–structure interaction method and it has been confirmed that the majority of the deformation happened in the maxillary sinus as well as the thyroid cartilage.













Similar content being viewed by others
References
Zhang Z, Lessmann R (1996) Computer simulation of the flow field and particle deposition by diffusion in a 3-D human airway bifurcation. Aerosol Sci Technol 25:338–352
Cebral JR, Summers RM (2004) Tracheal and central bronchial aerodynamics using virtual bronchoscopy and computational fluid dynamics. IEEE Trans Med Imaging 23(8):1021–1033
Wen J, Inthavong K, Tu J, Wang S (2008) Numerical simulations for detailed airflow dynamics in a human nasal cavity. Respir Physiol Neurobiol 161(2):125–135
Grgic B, Martin A, Finlay W (2006) The effect of unsteady flow rate increase on in vitro mouth–throat deposition of inhaled boluses. J Aerosol Sci 37(10):1222–1233
Liu Y, So RMC, Zhang CH (2002) Modeling the bifurcation flow in a human lung airway. J Biomech 35:465–473
Moghadas H, Abouali O, Faramarzi A, Ahmadi G (2011) Numerical investigation of nasal septal deviation effect on micro/nano-particles deposition in a human realistic geometry. Respir Physiol Neurobiol 177:9–18
Nithiarasu P, Hassan O, Morgan K, Weatherill NP, Fielder C, Whittet H, Ebden P, Lewis KR (2008) Steady flow through a realistic human upper airway geometry. Int J Numer Methods Fluids 57:631–651
Tavakoli B, Abouali O, Bagheri MH, Yazdi M, Ahmadi G (2012) Micro particles transport and deposition in realistic geometry of human upper airways. Int J Eng Trans A (Basics) 25(4):315–322
Malve M, Perezdel Palomar A, Lopez-Villalobos JL, Ginel A, Doblare M (2010) FSI analysis of the coughing mechanism in a human trachea. Ann Biomed Eng 38:1556–1565
Chen C, Lin CH, Jiang Z, Chen Q (2014) Simplified models for exhaled airflow from a cough with the mouth covered. Indoor Air J 24(6):580–591
Zhu S, Kato S, Yang JH (2006) Study on transport characteristics of saliva droplets produced by coughing in a calm indoor environment. Build Environ 41:1691–1702
Tang JW, Settles GS (2008) Images in clinical medicine, coughing and aerosols. New Engl J Med 15:359
Gupta J, Lin CH, Chen Q (2009) Flow dynamics and characterization of a cough. Indoor Air J 19:517–525
Wells WF (1955) Airborne contagion and air hygiene: an ecological study of droplet infection. Harvard University Press, Cambridge, pp 1–19
Xie X, Li Y, Chwang AT, Ho PL, Seto WH (2007) How far droplets can move in indoor environments–revisiting the Wells evaporation-falling curve. Indoor Air J 17:211–225
Jennison MW, Edgerton HE (1940) Droplet infection of air; high-speed photography of droplet production by sneezing. Proc Soc Exp Biol Med 43:455–458
Tang JW, Nicolle AD, Klettner CA, Pantelic J, Wang L, Suhaimi AB, Tan AYL, Ong GWX, Su R, Sekhar C, Cheong DDW, Tham KW (2013) Airflow dynamics of human jets: sneezing and breathing—potential sources of infectious aerosols. Plos ONE J 8(4):e59970. https://doi.org/10.1371/journal.pone.0059970
Nishimura H, Sakata S, Kaga A (2013) A new methodology for studying dynamics of aerosol particles in sneeze and cough using a digital high-vision, high-speed video system and vector analyses. Plos ONE J 8(11):e80244. https://doi.org/10.1371/journal.pone.0080244
Bourouiba L, Dehandschoewercker E, Bush JWM (2014) Violent expiratory events: on coughing and sneezing. J Fluid Mech 745:537–563
Gwaltney JM, Hendley JO, Phillips CD, Bass CR, Mygind N, Winther B (2000) Nose blowing propels nasal fluid into the paranasal sinuses. Clin Infect Dis 30(2):387–391
Rahiminejad M, Haghighi A, Dastan A, Abouali O, Farid M, Ahmadi G (2016) Computer simulations of pressure and velocity fields in ahuman upper airway during sneezing. Comput Biol Med 71:115–127
Faden DL, Elackatuu A, Platt M (2011) The closed-airway sneeze: an unusual cause of laryngeal fracture. J Otolaryngol Head Neck Surg 145(3):515–516
Martinez BA, Juara AM, Moya LJJ (2007) Fracture of thyroid cartilage after a sneezing episode. Acta Otorrinolaringol Esp 58(2):73–74
Mylavarapu G, Murugappan S, Mihaescu M, Kalra M, Khosla S, Gutmark E (2009) Validation of computational fluid dynamics methodology used for human upper airway flow simulations. J Biomech 42:1553–1559
Zubair M, Abdullah MZ, Ismail R, Shuaib IL, Hamid SA, Ahmad KA (2012) Review: a critical overview of limitations of CFD modeling in nasal airflow. J Med Biol Eng 32(2):77–84
MIR MiniSpir™. Simplified operation guide
Zhao M, Barber T, Cistulli PT, Sutherland K, Rosengarten G (2013) Simulation of upper airway occlusion without and with mandibular advancement in obstructive sleep apnea using fluid-structure interaction. J Biomech 46:2586–2592
Birch MJ, Srodon PD (2009) Biomechanical properties of the human soft palate. Cleft Palate Craniofac J 46(3):268–274
Patankar S (1980) Numerical heat transfer and fluid flow. Series on computational methods in mechanics and thermal science hemisphere publishing corporation, 1st edn. CRC Press, Boca Raton. https://doi.org/10.1201/9781482234213
Leong SC, Chen XB, Lee HP (2010) A review of the implications of computational fluid dynamic studies on nasal airflow and physiology. Rhinology 48:139–145
Sommer F, Scheithauer M, Kröger R, Rettinger G, Lindemann J (2014) Sneezing as a mechanical defence—a numerical simulation and analysis of the nasal flow. Laryngo- Rhino- Otologie 93(11):746–750
Nunn AJ, Gregg I (1989) New regression equations for predicting peak expiratory flow in adults. BMJ 298:1068–1070
Matrka L, Li M (2018) Laryngeal fracture following violent sneeze: management and biomechanical analysis. Am Acad Otolaryngol Head Neck Surg 2:24
Acknowledgements
We thank Taba-Parto Shiraz radiology center for assistance with 3D CT scan, and Shamsizadeh clinic that provided the spirometer device that greatly improved the manuscript.
Funding
The research was not funded by any organization or university.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors of this paper declare that they consider no conflict of interest.
Human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Technical Editor: Estevam Barbosa Las Casas, Ph. D.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mortazavy Beni, H., Hassani, K. & Khorramymehr, S. Study of the sneezing effects on the real human upper airway using fluid–structure interaction method. J Braz. Soc. Mech. Sci. Eng. 41, 181 (2019). https://doi.org/10.1007/s40430-019-1677-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40430-019-1677-z