Abstract
Background
The aim of this meta-analysis was to compare single-photon emission computed tomography (SPECT/CT) and planar lymphoscintigraphy (PL) in patients with primary breast cancer, undergoing lymphoscintigraphy at initial staging. Specifically, we assessed the detection rate (DR) for sentinel lymph node (SLN), the absolute number of detected SLNs by each technique, and the proportion of patients with additional SLNs detected by one technique compared to the other one. Finally, we aimed to evaluate the impact of SPECT/CT on the surgical approach.
Methods
Original articles, providing a head-to-head comparison between SPECT/CT and PL, including patients with primary breast cancer at first presentation, were searched in PubMed/MEDLINE and Scopus databases through March 31st, 2022. The DR of the imaging techniques was calculated on a per-patient analysis; studies were pooled on their odds ratios (ORs) with a random-effects model to assess the presence of a significant difference between the DRs of SPECT/CT and PL. The number of additional SLNs, calculated as relative risk (RR), and the pooled proportion of patients with additional SLNs using one imaging technique rather than the other one were investigated. The pooled ratio of surgical procedures (SLN harvesting) influenced by the use of SPECT/CT, according to the surgeons, was calculated.
Results
Sixteen studies with 2693 patients were eligible for the calculation of the DR of SPECT/CT and PL. The DR was 92.11% [95% confidence interval (95% CI) 89.32–94.50%] for SPECT/CT, and 85.12% (95% CI 80.58–89.15%) for PL, with an OR of 1.96 (95% CI 1.51–2.55) in favor of SPECT/CT. There was a relative risk of detection of larger number of SLNs (RR: 1.22, 95% CI 1.14–1.32; 12 studies; 979 patients) for SPECT/CT (n = 3983) compared to PL (n = 3321) and a significant proportion of patients with additional SLNs detected by SPECT/CT, which were missed by PL (18.88%, 95% CI: 11.72%-27.27%; 13 studies). Four articles, with a total number of 1427 patients, revealed that 23.98% of the surgical procedures benefited from the use of SPECT/CT.
Conclusions
This meta-analysis favors SPECT/CT over PL for the identification of SLN in patients with primary breast cancer at staging due to higher DR, more SLNs depicted, and a significant proportion of subjects with additional detected SLNs by SPECT/CT compared to PL. Furthermore, SPECT/CT positively influences the surgical procedure. However, PL remains a satisfactory imaging option for imaging departments not equipped with SPECT/CT due to its good patient-based DR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rationale for identifying the sentinel lymph node (SLN), namely the lymph node directly draining the primary tumor, relies on the low likelihood of the presence of cancer cells in the subsequent lymph nodes in the case of a non-metastatic SLN [1]. SLN biopsy (SLNB) is indicated as the gold standard technique for the axillary staging of patients with breast cancer and no clinical evidence of metastatic nodes [2,3,4]. SLNB does not increase the risk of axillary recurrence in patients with breast cancer and reduces the risk of lymphedema compared to complete lymph node dissection (CLND) [5, 6].
SLNB reflects the status of the axillary cavity in over 97% of patients with breast cancer [7]. Radionuclide localization of SLN using 99mTc-labeled colloids in patients with breast cancer is a well-established procedure [8]. Nowadays, planar lymphoscintigraphy (PL) is currently a routine, simple and reliable procedure, performed in most nuclear medicine departments, for the identification of SLN and lymphatic disorders [9, 10]. The inclusion of nuclear medicine procedures for the detection of SLN in the diagnostic workup reduces the false-negative rate of SLNB in patients with breast cancer evaluated at first presentation [11]. Over the last decades, the use of single-photon emission computed tomography/computed tomography (SPECT/CT) has gained wider diffusion in nuclear medicine departments. Indeed, the use of hybrid scanners, providing complementary scintigraphic and morphological data, enables nuclear medicine physicians to offer more accurate information regarding the SLN (e.g. location, number, and surrounding anatomical structures) to the surgeons compared to PL, according to the results of a previous meta-analysis by our group involving patients with melanoma [12].
Whereas an overall superior SLN detection rate (DR) has been reported for SPECT/CT compared to PL in patients with cervical cancer [13] and melanoma [14], such evidence has not been systematically collected for patients with breast cancer.
The aim of this meta-analysis was to perform a head-to-head comparison of the DR of PL and SPECT/CT in patients with breast cancer. Furthermore, as secondary aims, we assessed whether there is a significant difference in the number of detected SLNs, and a significant proportion of patients with additional detected SLNs based on SPECT/CT rather than PL findings or vice versa. Finally, we assessed the ratio of surgical procedures (SLN harvestings) for which SPECT/CT proved a beneficial impact, according to the surgical team.
Materials and methods
The meta-analysis was conducted following the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [15]. Before starting the literature search, a protocol was developed to define the research question, search methods, inclusion criteria, quality assessment, data extraction, and statistical analysis. The protocol was registered in the International Prospective Register of Systematic Reviews, Prospero, (www.crd.york.ac.uk/prospero/;protocol CRD42022307723).
Literature search and inclusion criteria
PubMed/MEDLINE and Scopus databases were interrogated independently by two researchers to retrieve prospective or retrospective single or multicenter studies, carrying out PL and SPECT/CT with 99mTc-labeled colloids in patients with primary breast cancer at initial diagnosis before the surgical staging of the axilla.
For our primary outcome (comparison of DRs), we selected articles reporting both the DR of PL and SPECT/CT for SLN (at least 1 lymph node per patient). For our secondary outcomes, we selected articles reporting information on (1) the number of SLNs detected by SPECT/CT and PL, (2) the number of patients with additional SLNs detected by SPECT/CT and/or PL, (3) the ratio of surgical SLN harvestings influenced by SPECT/CT.
The search string was designed to capture the concepts of breast cancer, SLN, SPECT/CT, and PL within the title and article abstracts; for PubMed, the search string was Breast AND (“Sentinel Lymph Node”[Mesh] OR sentinel) AND (“Single Photon Emission Computed Tomography Computed Tomography”[Mesh] OR SPECT). For Scopus, the search string was Breast AND (“Sentinel Lymph Node” OR sentinel) AND (“Single Photon Emission Computed Tomography Computed Tomography” OR SPECT).
No date limit or language restriction was applied. The literature search was updated until March 31st, 2022. All identified references were exported to a reference management software (Endnote v. X7.5, Clarivate Analytics).
Study selection
Two investigators independently screened the titles and abstracts of the records retrieved by the search strings. Only original articles were selected. For each outcome of the present meta-analysis, articles from the same author with the risk of patients’ overlap were also excluded, selecting only the study with the largest number of patients. Duplicates were identified in Endnote and deleted.
After excluding duplicates and non-original articles, the full text of the remaining articles was retrieved to verify the inclusion criteria for this meta-analysis: (1) a study cohort or a subset of a minimum of 10 patients with breast cancer at initial staging undergoing both SPECT/CT and PL in the same day for the identification of the SLN before surgery; (2) injection of 99mTc-nanocolloids; (3) no evidence of other malignancies.
Articles in languages other than English had been planned for translation into English by native speakers before performing the meta-analysis. The references of the retrieved articles were also screened for eventually retrieving additional studies.
Data extraction
Data of all included studies in the meta-analysis were independently extracted by two researchers and any disagreement was resolved in a consensus meeting. Bibliographical and technical data extracted from the articles included: authors, publication year, country, journal, number of patients, sex, and age (mean and range).
For each article, the following data were also retrieved for statistical analysis: the absolute number of patients with at least 1 SLN depicted by SPECT/CT and/or PL, the total number of SLNs detected by SPECT/CT and/or PL, the number of patients with additional SLNs detected by SPECT/CT or PL, the number of patients evaluated for the assessment of the impact of SPECT and PL on the surgical procedure and the number of procedure influenced by the nuclear medicine examination according to the surgeons.
Methodological quality assessment
The methodological quality of the studies was assessed by two investigators using version 2 of the “Quality Assessment of Diagnostic Accuracy Studies” tool (QUADAS-2) [16], which comprises four domains: patient selection, index test, reference standard, flow and timing. The concerns about the risk of bias or applicability were described as low, high, or unclear.
Statistical analysis
Statistical analysis was carried out using MedCalc Statistical Software version 19.1.3 (MedCalc Software, Ostend, Belgium; https://www.medcalc.org; 2020). Publication bias was assessed by visual inspection of funnel plots. The I2 statistic was used to measure the degree of inconsistency across the studies, with I2 values of 25%, 50%, and 75% representing thresholds for low, moderate, and high heterogeneity. Interpretation of heterogeneity was carried out at a significance level of p = 0.05. A random-effects model was used for statistical pooling.
DR was defined based on the detection of at least one SLN in a single patient. Overall pooled DRs were calculated for SPECT/CT and PL on a per-patient-based analysis and presented using forest plots. To assess any statistically significant difference between the two pooled DRs of SPECT/CT and PL, studies were pooled on their odds ratios (ORs) with an inverse variance-weighted random effects model. Pooled data were presented with 95% confidence interval values (95% CI). A statistical difference of pooled DR among SPECT/CT and PL was present if there was no overlap among the 95% CI values.
The number of SLNs detected by SPECT/CT and PL were compared by pooling the ORs with an inverse variance-weighted random effects model. If the value 1 was not within the 95% CI, then the pooled OR is statistically significant at the 5% level (p < 0.05).
The weighted proportion of patients with additional SLNs detected by each technique compared to the other one, and the impact of SPECT/CT on surgery were pooled across the studies and presented in the form of pooled percentages on a per-patient analysis.
Results
Literature search and eligibility assessment
The comprehensive computer literature search from PubMed/MEDLINE and Scopus databases revealed 362 articles (Fig. 1). One-hundred thirty items were duplicates and excluded leading to 232 articles. After excluding non-original articles (n = 110), further 102 abstracts were excluded because they were not in the field of interest of the meta-analysis. The full text of the remaining 20 studies was searched; for two studies, the full text was not available despite contacting the corresponding authors. The characteristics of the retrieved 18 studies [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34] are presented in Table 1, whereas methodological information concerning the acquisition of PL and SPECT/CT in the studies is summarized in Table 2.
The risk of bias for the studies included in the meta-analysis was scored low using the QUADAS-2. No publication bias was detected (Fig. 2).
Sixteen studies, with a total number of 2693 patients, were available for the calculation of the pooled DR of SPECT/CT and PL.
Twelve studies were eligible for the comparison of absolute number of SLNs detected by the two techniques.
Thirteen studies were eligible for calculation of proportion of patients with additional SLNs in one of the two techniques.
Four studies (1427 patients) were eligible for the assessment of the average percentage of patients for whom surgical management was influence by one of the two techniques.
Detection rate of SPECT/CT and PL
In a per-patient analysis, the pooled DR for SLN of SPECT/CT was 92.11% [95% confidence interval (95% CI) 89.32–94.50%], whereas the DR for SLN of PL was 85.12% (95% CI 80.58–89.15%) (Figs. 3 and 4, respectively).
The DR rate of SPECT/CT for SLN ranged from 77.78% to 100% across the studies. The DR rate of PL for SLN ranged from 59.70 to 100%. A marked statistical heterogeneity was found for SPECT/CT (I2 = 78.26%) and PL (I2 = 86.76%). A significant difference between the DRs was found with a pooled OR of 1.96 (95% CI 1.51–2.55) in favor of SPECT/CT (I2 = 33.66%).
Comparison of the number of SLNs detected by SPECT/CT and PL
SPECT/CT depicted a higher number (3978 vs. 3321) of SLNs compared to PL in 979 patients, with a statistically significant OR of 1.22 (95% CI 1.14–1.32). No study reported a larger number of SLNs depicted by PL compared to SPECT/CT.
Proportion of patients with additional SLNs detected by SPECT/CT or PL
Taking into account a total sample size of 2485 patients, the pooled proportion of patients in whom SPECT/CT depicted additional SLNs compared to PL was 18.88% (95% CI 11.72–27.27%).
The proportion of patients with additional SLNs detected by PL but missed by SPECT/CT was not significant (0.82%).
Impact on surgery of SPECT/CT
The pooled percentage of cases influenced by the use of SPECT/CT according to surgeons (4 studies enrolling 1427 patients) was 23.98% (95% CI 11.34–39.53%), whereas the corresponding proportion of case influenced by PL was 1.5% (95% CI 0.29–3.90%).
Discussion
Radioisotope imaging has a lower false-negative rate than blue dye and there is no significant difference between indocyanine green (ICG) and radioisotope imaging for the SLN detection, according to a recent meta-analysis (a total of 30 studies, including 4,216 SLN procedures), which, nevertheless, did not analyze the impact of SPECT/CT in the detection performance [35].
In this meta-analysis, we focused on articles comparing SPECT/CT and PL in the same patients at initial staging rather including also studies with parallel data collection of SPECT/CT and PL, in keeping with our previous experience [14]. The reason of our choice is that head-to-head comparison provides a more accurate estimate of the outcome measures compared to matched-pair comparison [36]. We limited our analysis to patients at staging, because in case of breast cancer recurrence and previous axillary lymph node dissection (ALND), the repeat sentinel node biopsy has a significantly lower rate of harvesting and a much more aberrant lymphatic [37].
Very high rates of successful SLN detection in patients with breast cancer have been reported with either PL or SPECT/CT [24]. Nevertheless, the use of SPECT/CT has been encouraged by several authors due to substantial advantages over PL, including higher DR, better spatial resolution, more precise anatomical localization of the SLN [38] and efficient attenuation correction through the exploiting the CT data [13, 39, 40]. Conversely, the use of SPECT/CT increases the acquisition time and the radiation dose compared to PL, potentially reducing the patient workflow and bringing additional costs [41].
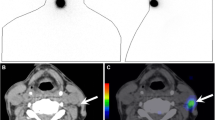
Our meta-analysis documented a superior DR for SPECT/CT compared to PL and a larger number of SLNs detected by SPECT/CT compared to PL. Higher DR and a larger number of SLNs identified by SPECT/CT in comparison with PL may also determine a meaningful impact on surgical decision-making. Nevertheless, the preoperative use of SPECT/CT for the identification of SLNs is not important only for the additional number of SLNs but also for the capability of providing anatomical information [42]. Indeed, SPECT/CT may also localize unspecific hot spots that could be mistaken as additional SLNs using PL only [43], for example in case of cutaneous contamination, skin fold, propagation from the injection site or leakage from the wire tract [27]. We found a 23.98% of change in surgical approaches in patients with breast cancer. A more precise localization of SLNs may lead to a more precise surgical procedure (due to a change in the location, size and accuracy of the incision), facilitating the surgical planning, reducing the morbidity, the duration of surgical operations and costs [44].
From our analysis, it can be observed that heterogeneity indexes are high either for SPECT/CT (I2 = 78.26%) or PL (I2 = 86.76%), which is in contrast with our previous results in melanoma patients [14], which suggested higher repeatability for SPECT compared PL, as highlighted by the lower heterogeneity index (I2) obtained for SPECT/CT (I2 = 62.45% vs. 78.96%).
van der Ploeg and coworkers suggested three main indications to perform SPECT/CT: (1) inconclusive PL due to unusual lymphatic drainage pattern, (2) difficulty in the interpretation of a lymphatic pattern, and (3) nonvisualization of SLN at PL [45], accounting approximately for a third of patients with breast cancer according to their experience [33]. Also, the recent systematic review of Ge et al., suggest to add SPECT/CT to the diagnostic work-up of patients with breast cancer recurrence when PL fails to detect the SLN, since SPECT/CT may increase the chance of detecting the lymph node also outside the axilla [37].
Certain patient characteristics may also lead to add SPEC/CT to the radioisotope mapping. Increased body mass index (BMI) is a major risk factor for the development of severe lymphedema after ALND [46] and, along with breast size, is also an important factor affecting negatively lymphoscintigraphic and intraoperative SLNs detection [47, 48]. On the other hand, Lerman et al. demonstrated the superior performance of SPECT/CT in identifying SLNs in overweight and obese breast cancer patients, even in case of intraoperative blue dye technique failure, suggesting the indication to routinely perform SPECT/CT in case of high BMIs [27].
The 2013 joint EANM and SNMMI guidelines do not indicate SPECT or SPECT/CT as mandatory, but as optional or alternate imaging, suggesting its use in the case of nonvisualization of SLN on PL, obese patients, and SLNs outside the axilla. Otherwise, the execution of SPECT/CT may be justified by the difficulty in the interpretation of PL due to unexpected or unusual lymphatic patterns (e.g. multiple sites of drainage or the appearance of the intramammary lymph node chain, SLN in the contralateral axilla, previous breast surgery, the presence of a SLN near the injection area, or suspicion of contamination) [49]. Conversely, the Chinese Society of Breast Surgery in 2021 attributed a level B (weak) strength of recommendation to lymphoscintigraphy as a mapping method of the SLN, not even mentioning SPECT/CT [50].
The current use of PL as the elective method for radioisotope mapping of the SLN relies on its high detection rate [41]. There are still few data to demonstrate that the addition of SPECT/CT improves staging, since only a few studies reported the histologic data of the SLNs depicted by SPECT/CT but missed by PL [33]. Additionally, there are still no sufficient data to confirm that a higher number of SLN identified by SPECT/CT and removed result in an improvement of control disease. Nevertheless, SPECT/CT is strongly recommended for selected indications, especially when PL fails to detect the SLN, in case of abnormal lymphatic drainage pattern, and for overweight patients.
Some limitations may affect our meta-analysis. The selected studies provided markedly variable sample sizes. Another source of bias may derive from the high heterogeneity of the DR across the studies. Further sources of bias may arise from some differences across the studies including the number of radiotracer injections, and methodology of PL and SPECT/CT execution. As suggestions for further studies, cost-effectiveness analyses should evaluate whether the use of preoperative SPECT/CT compared with PL for SNL detection in breast cancer is associated not only with higher detection of metastatic involvement but also with a significant cost reduction.
Conclusions
The present meta-analysis favors the use of SPECT/CT with 99mTc-labeled colloids over PL in patients with breast cancer for the identification of SLN due to its superior DR. Further advantages of SPECT/CT over PL are an overall larger number of depicted SLNs, a significant proportion of patients with additional SLNs detected by SPECT/CT but missed by PL, and an impact on surgical strategy on a significant percentage of patients. Nonetheless, in institutions where SPECT/CT is not available, PL remains a good option due to its good DR for the SLN on a patient-based analysis.
References
Moncayo VM, Aarsvold JN, Alazraki NP (2015) Lymphoscintigraphy and sentinel nodes. J Nucl Med 56:901–907. https://doi.org/10.2967/jnumed.114.141432
Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Costantino JP, Ashikaga T, Weaver DL, Mamounas EP, Jalovec LM, Frazier TG, Noyes RD, Robidoux A, Scarth HM, Wolmark N (2010) Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol 11:927–933. https://doi.org/10.1016/s1470-2045(10)70207-2
Mansel RE, Fallowfield L, Kissin M, Goyal A, Newcombe RG, Dixon JM, Yiangou C, Horgan K, Bundred N, Monypenny I, England D, Sibbering M, Abdullah TI, Barr L, Chetty U, Sinnett DH, Fleissig A, Clarke D, Ell PJ (2006) Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC Trial. J Natl Cancer Inst 98:599–609. https://doi.org/10.1093/jnci/djj158
Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, Intra M, Veronesi P, Robertson C, Maisonneuve P, Renne G, De Cicco C, De Lucia F, Gennari R (2003) A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med 349:546–553. https://doi.org/10.1056/NEJMoa012782
Langer I, Guller U, Berclaz G, Koechli OR, Schaer G, Fehr MK, Hess T, Oertli D, Bronz L, Schnarwyler B, Wight E, Uehlinger U, Infanger E, Burger D, Zuber M (2007) Morbidity of sentinel lymph node biopsy (SLN) alone versus SLN and completion axillary lymph node dissection after breast cancer surgery: a prospective Swiss multicenter study on 659 patients. Ann Surg 245:452–461. https://doi.org/10.1097/01.sla.0000245472.47748.ec
Canavese G, Bruzzi P, Catturich A, Tomei D, Carli F, Garrone E, Spinaci S, Lacopo F, Tinterri C, Dozin B (2016) Sentinel lymph node biopsy versus axillary dissection in node-negative early-stage breast cancer: 15-year follow-up update of a randomized clinical trial. Ann Surg Oncol 23:2494–2500. https://doi.org/10.1245/s10434-016-5177-4
Miltenburg DM, Miller C, Karamlou TB, Brunicardi FC (1999) Meta-analysis of sentinel lymph node biopsy in breast cancer. J Surg Res 84:138–142. https://doi.org/10.1006/jsre.1999.5629
Paganelli G (1998) Sentinel node biopsy: role of nuclear medicine in conservative surgery of breast cancer. Eur J Nucl Med 25:99–100. https://doi.org/10.1007/s002590050199
Pappalardo M, Cheng MH (2020) Lymphoscintigraphy for the diagnosis of extremity lymphedema: current controversies regarding protocol, interpretation, and clinical application. J Surg Oncol 121:37–47. https://doi.org/10.1002/jso.25526
Pappalardo M, Lin C, Ho OA, Kuo CF, Lin CY, Cheng MH (2019) Staging and clinical correlations of lymphoscintigraphy for unilateral gynecological cancer-related lymphedema. J Surg Oncol. https://doi.org/10.1002/jso.25817
Pesek S, Ashikaga T, Krag LE, Krag D (2012) The false-negative rate of sentinel node biopsy in patients with breast cancer: a meta-analysis. World J Surg 36:2239–2251. https://doi.org/10.1007/s00268-012-1623-z
Quartuccio N, Siracusa M, Pappalardo M, Arnone A, Arnone G (2020) Sentinel node identification in melanoma: current clinical impact, new emerging SPECT radiotracers and technological advancements. an update of the last decade. Curr Radiopharm 13:32–41. https://doi.org/10.2174/1874471012666191015100837
Hoogendam JP, Veldhuis WB, Hobbelink MG, Verheijen RH, van den Bosch MA, Zweemer RP (2015) 99mTc SPECT/CT versus planar lymphoscintigraphy for preoperative sentinel lymph node detection in cervical cancer: a systematic review and metaanalysis. J Nucl Med 56:675–680. https://doi.org/10.2967/jnumed.114.152439
Quartuccio N, Garau LM, Arnone A, Pappalardo M, Rubello D, Arnone G, Manca G (2020) Comparison of (99m)Tc-labeled colloid SPECT/CT and planar lymphoscintigraphy in sentinel lymph node detection in patients with melanoma: a meta-analysis. J Clin Med. https://doi.org/10.3390/jcm9061680
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Rev Esp Cardiol (English Ed) 74:790–799. https://doi.org/10.1016/j.rec.2021.07.010
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Arican P (2012) Planar lymphoscintigraphy and SPECT/CT in detection of sentinel lymph node in breast cancer. Turk J Surg 28:201–206. https://doi.org/10.5152/UCD.2012.20
Bennie G, Vorster M, Buscombe J, Sathekge M (2015) The added value of a single-photon emission computed tomography-computed tomography in sentinel lymph node mapping in patients with breast cancer and malignant melanoma. World J Nucl Med 14:41–46. https://doi.org/10.4103/1450-1147.150543
Brouwer OR, Vermeeren L, van der Ploeg IM, Valdés Olmos RA, Loo CE, Pereira-Bouda LM, Smit F, Neijenhuis P, Vrouenraets BC, Sivro-Prndelj F, Jap-a-Joe SM, Borgstein PJ, Rutgers EJ, Oldenburg HS (2012) Lymphoscintigraphy and SPECT/CT in multicentric and multifocal breast cancer: does each tumour have a separate drainage pattern? Results of a Dutch multicentre study (MULTISENT). Eur J Nucl Med Mol Imaging 39:1137–1143. https://doi.org/10.1007/s00259-012-2131-y
Frusciante V, Asabella AN, Castriotta G, Guerra M, Murgo R, Ciuffreda L, Lavelli V, Ferrari C, Rubini G (2016) Added value of SPECT/CT over planar imaging in improving sentinel node detection in breast cancer patients. Recenti Prog Med 107:444–449. https://doi.org/10.1701/2332.25072
Gizewska A, Witkowska-Patena E, Osiecki S, Mazurek A, Stembrowicz-Nowakowska Z, Dziuk M (2017) Utility of single-photon emission tomography/computed tomography for sentinel lymph node localization in breast cancer patients. Nucl Med Commun 38:493–499. https://doi.org/10.1097/MNM.0000000000000676
Husarik DB, Steinert HC (2007) Single-photon emission computed tomography/computed tomography for sentinel node mapping in breast cancer. Semin Nucl Med 37:29–33. https://doi.org/10.1053/j.semnuclmed.2006.08.001
Jankowska S (2016) Comparison of planar and SPECT/CT imaging in the detection of sentinel lymph nodes in breast cancer. Pomeranian J Life Sci 62:16–20
Jimenez-Heffernan A, Ellmann A, Sado H, Huic D, Bal C, Parameswaran R, Giammarile F, Pruzzo R, Kostadinova I, Vorster M, Almeida P, Santiago J, Gambhir S, Sergieva S, Calderon A, Young GO, Valdes-Olmos R, Zaknun J, Magboo VP, Pascual TN (2015) Results of a prospective multicenter international atomic energy agency sentinel node trial on the value of SPECT/CT over planar imaging in various malignancies. J Nucl Med 56:1338–1344. https://doi.org/10.2967/jnumed.114.153643
Kraft O, Havel M (2013) Sentinel lymph nodes and planar scintigraphy and SPECT/CT in various types of tumours. Estimation of some factors influencing detection success. Nucl Med Rev 16:17–25. https://doi.org/10.5603/NMR.2013.0004
Lecoanet A, Perdrisot R (2010) Interest of hybrid SPECT-CT imaging for sentinel node detection in breast cancer. Medecine Nucleaire 34:325–334. https://doi.org/10.1016/j.mednuc.2010.03.004
Lerman H, Lievshitz G, Zak O, Metser U, Schneebaum S, Even-Sapir E (2007) Improved sentinel node identification by SPECT/CT in overweight patients with breast cancer. J Nucl Med 48:201–206
Manca G, Garau LM, Mazzarri S, Mazzuca L, Muccioli S, Ghilli M, Naccarato G, Colletti PM, Rubello D, Roncella M, Volterrani D, Desideri I (2021) Novel experience in hybrid tracers: clinical evaluation of feasibility and efficacy in using ICG-99mTc nanotop for sentinel node procedure in breast cancer patients. Clin Nucl Med 46:e181–e187. https://doi.org/10.1097/RLU.0000000000003478
Mucientes Rasilla J, Farge Balbín L, Cardona Arboniés J, Moreno Elola-Olaso A, Delgado-Bolton R, Izarduy Pereyra L, Rodríguez Rey C, Lapeña Gutiérrez L, González Maté A, Román Santamaría JM, Carreras Delgado JL (2008) SPECT-CT: a new tool for localisation of sentinel lymph nodes in breast cancer patients. Rev Esp Med Nucl 27:183–190. https://doi.org/10.1157/13121028
Pecking AP, Wartski M, Cluzan RV, Bellet D, Albérini JL (2007) SPECT-CT fusion imaging radionuclide lymphoscintigraphy: potential for limb lymphedema assessment and sentinel node detection in breast cancer. Cancer Treat Res 135:79–84. https://doi.org/10.1007/978-0-387-69219-7_6
Siddique M, Nawaz MK, Bashir H (2018) The usefulness of SPECT/CT in sentinel node mapping of early stage breast cancer patients showing negative or equivocal findings on planar scintigraphy. Asia Ocean J Nucl Med Biol 6:80–89. https://doi.org/10.22038/aojnmb.2018.10720
Stanzel S, Pernthaler B, Schwarz T, Bjelic-Radisic V, Kerschbaumer S, Aigner RM (2018) Diagnostic and prognostic value of additional SPECT/CT in sentinel lymph node mapping in breast cancer patients. Nuklearmedizin Nucl Med 57:92–99. https://doi.org/10.3413/Nukmed-0929-17-09
van der Ploeg IM, Nieweg OE, Kroon BB, Rutgers EJ, Baas-Vrancken Peeters MJ, Vogel WV, Hoefnagel CA, Olmos RA (2009) The yield of SPECT/CT for anatomical lymphatic mapping in patients with breast cancer. Eur J Nucl Med Mol Imaging 36:903–909. https://doi.org/10.1007/s00259-008-1050-4
Yoneyama H, Tsushima H, Onoguchi M, Konishi T, Nakajima K, Matsuo S, Kayano D, Wakabayashi H, Inaki A, Kinuya S (2015) Optimization of attenuation and scatter corrections in sentinel lymph node scintigraphy using SPECT/CT systems. Ann Nucl Med 29:248–255. https://doi.org/10.1007/s12149-014-0939-1
Thongvitokomarn S, Polchai N (2020) Indocyanine green fluorescence versus blue dye or radioisotope regarding detection rate of sentinel lymph node biopsy and nodes removed in breast cancer: a systematic review and meta-analysis. Asian Pac J Cancer Prev 21:1187–1195. https://doi.org/10.31557/apjcp.2020.21.5.1187
Sadeghi R, Treglia G (2017) Systematic reviews and meta-analyses of diagnostic studies: a practical guideline. Clin Transl Imaging 5:83–87. https://doi.org/10.1007/s40336-016-0219-2
Ge I, Erbes T, Juhasz-Böss I (2022) Prognostic value and management of regional lymph nodes in locoregional breast cancer recurrence: a systematic review of the literature. Arch Gynecol Obstet. https://doi.org/10.1007/s00404-021-06352-9
Manca G, Mazzarri S, Rubello D, Tardelli E, Delgado-Bolton RC, Giammarile F, Roncella M, Volterrani D, Colletti PM (2017) Radioguided occult lesion localization: technical procedures and clinical applications. Clin Nucl Med 42:e498–e503. https://doi.org/10.1097/rlu.0000000000001858
Hasegawa BH, Wong KH, Iwata K, Barber WC, Hwang AB, Sakdinawat AE, Ramaswamy M, Price DC, Hawkins RA (2002) Dual-modality imaging of cancer with SPECT/CT. Technol Cancer Res Treat 1:449–458. https://doi.org/10.1177/153303460200100605
Bluemel C, Herrmann K, Giammarile F, Nieweg OE, Dubreuil J, Testori A, Audisio RA, Zoras O, Lassmann M, Chakera AH, Uren R, Chondrogiannis S, Colletti PM, Rubello D (2015) EANM practice guidelines for lymphoscintigraphy and sentinel lymph node biopsy in melanoma. Eur J Nucl Med Mol Imaging 42:1750–1766. https://doi.org/10.1007/s00259-015-3135-1
Vercellino L, Ohnona J, Groheux D, Slama A, Colletti PM, Chondrogiannis S, Merlet P, Toubert ME, Rubello D (2014) Role of SPECT/CT in sentinel lymph node detection in patients with breast cancer. Clin Nucl Med 39:431–436. https://doi.org/10.1097/RLU.0b013e31829af8c0
Tardelli E, Mazzarri S, Rubello D, Gennaro M, Fantechi L, Duce V, Romanini A, Chondrogiannis S, Volterrani D, Colletti PM, Manca G (2016) Sentinel lymph node biopsy in cutaneous melanoma: standard and new technical procedures and clinical advances. A systematic review of the literature. Clin Nucl Med 41:e498–e507. https://doi.org/10.1097/rlu.0000000000001370
Duce V, Manca G, Mazzarri S, Lorenzetti F, Colletti PM, Rubello D, Volterrani D (2016) Sentinel node mapping in melanoma of the back: SPECT/CT helps discriminate “true” and “false” in-transit lymph nodes. Clin Nucl Med 41:e66-67. https://doi.org/10.1097/rlu.0000000000000838
Stoffels I, Muller M, Geisel MH, Leyh J, Poppel T, Schadendorf D, Klode J (2014) Cost-effectiveness of preoperative SPECT/CT combined with lymphoscintigraphy vs. lymphoscintigraphy for sentinel lymph node excision in patients with cutaneous malignant melanoma. Eur J Nucl Med Mol Imaging 41:1723–1731. https://doi.org/10.1007/s00259-014-2771-1
van der Ploeg IM, Valdés Olmos RA, Nieweg OE, Rutgers EJ, Kroon BB, Hoefnagel CA (2007) The additional value of SPECT/CT in lymphatic mapping in breast cancer and melanoma. J Nucl Med 48:1756–1760. https://doi.org/10.2967/jnumed.107.043372
Petrek JA, Senie RT, Peters M, Rosen PP (2001) Lymphedema in a cohort of breast carcinoma survivors 20 years after diagnosis. Cancer 92:1368–1377. https://doi.org/10.1002/1097-0142(20010915)92:6%3c1368::aid-cncr1459%3e3.0.co;2-9
Nos C, Fréneaux P, Guilbert S, Falcou MC, Salmon RJ, Clough KB (2001) Sentinel lymph node detection for breast cancer: which patients are best suited for the patent blue dye only method of identification? Ann Surg Oncol 8:438–443. https://doi.org/10.1007/s10434-001-0438-1
Derossis AM, Fey JV, Cody HS 3rd, Borgen PI (2003) Obesity influences outcome of sentinel lymph node biopsy in early-stage breast cancer. J Am Coll Surg 197:896–901. https://doi.org/10.1016/j.jamcollsurg.2003.08.005
Giammarile F, Alazraki N, Aarsvold JN, Audisio RA, Glass E, Grant SF, Kunikowska J, Leidenius M, Moncayo VM, Uren RF, Oyen WJ, Valdés Olmos RA, Vidal Sicart S (2013) The EANM and SNMMI practice guideline for lymphoscintigraphy and sentinel node localization in breast cancer. Eur J Nucl Med Mol Imaging 40:1932–1947. https://doi.org/10.1007/s00259-013-2544-2
Ye JM, Guo BL, Liu Q, Ma F, Liu HJ, Wu Q, Xin L, Cheng YJ, Zhang H, Zhang S, Duan XN, Zhang JG, Liu YH (2021) Clinical practice guidelines for sentinel lymph node biopsy in patients with early-stage breast cancer: Chinese Society of Breast Surgery (CSBrS) practice guidelines 2021. Chin Med J (Engl) 134:886–894. https://doi.org/10.1097/cm9.0000000000001410
Funding
Open access funding provided by Università della Svizzera italiana.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors (Natale Quartuccio, Pierpaolo Alongi, Priscilla Guglielmo, Rosaria Ricapito, Gaspare Arnone, and Giorgio Treglia) declare that have nothing to disclose and did not receive any funding.
Human and animal rights
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Quartuccio, N., Alongi, P., Guglielmo, P. et al. 99mTc-labeled colloid SPECT/CT versus planar lymphoscintigraphy for sentinel lymph node detection in patients with breast cancer: a meta-analysis. Clin Transl Imaging 11, 587–597 (2023). https://doi.org/10.1007/s40336-022-00524-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-022-00524-6