Abstract
Background
A previous meta-analysis reported that: (i) an acute bout of prolonged uninterrupted sitting induces a significant increase in peripheral blood pressure (BP) and (ii) the increase in BP can be offset by interrupting the sitting bout with light aerobic activities such as walking. However, the temporal association between prolonged uninterrupted sitting and BP was not determined. A better understanding of temporality, for example, how long it takes BP to increase, will assist in prescribing sitting interruption strategies.
Objectives
We aimed to determine: (1) the temporal association between the duration of uninterrupted sitting and BP and (2) whether regular sitting interruptions moderate the association between uninterrupted sitting and BP.
Data Sources
Electronic databases (PubMed, Web of Science, SPORTDiscus) were searched from inception to July 2022. Reference lists of eligible studies and relevant reviews were also screened.
Study Selection
Inclusion criteria for objective (1) were: (i) participants aged ≥ 18 years; (ii) a prolonged sitting bout ≥ 1 h; and (iii) peripheral BP measurements (systolic BP, diastolic BP, and/or mean arterial pressure) at more than two timepoints during the sitting bout. Additional criteria for objective (2) were: (i) the sitting interruption strategy was implemented during the sitting bout (i.e., not prior to engaging in sitting) and (ii) the study included a control (uninterrupted sitting) condition or group.
Appraisal and Synthesis Methods
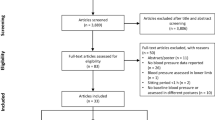
There were 1555 articles identified, of which 33 met inclusion criteria for objective (1). Of those articles, 20 met inclusion criteria for objective (2). To investigate the effect of sitting duration on the BP response, unstandardized b coefficients (mmHg/h) and 95% confidence intervals (CIs) were calculated using a three-level mixed-effect meta-regression.
Results
Increased sitting duration was positively associated with systolic BP (b = 0.42 mmHg/h, 95% CI 0.18–0.60), diastolic BP (b = 0.24 mmHg/h, 95% CI 0.06–0.42), and mean arterial pressure (b = 0.66 mmHg/h, 95% CI 0.36–0.90). In trials where sitting was interrupted, there was a significant decrease in systolic BP (b = − 0.24 mmHg/h, 95% CI − 0.42 to − 0.06) and diastolic BP (b = − 0.24 mmHg/h, 95% CI − 0.42 to − 0.12), and a non-significant change in mean arterial pressure (p = 0.69).
Conclusions
Increased uninterrupted sitting duration results in greater increases in BP; however, regularly interrupting sitting may offset negative effects.







Similar content being viewed by others
References
Tremblay MS, Aubert S, Barnes JD, et al. Sedentary behavior research network (SBRN)—terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14:1–17. https://doi.org/10.1186/s12966-017-0525-8.
Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388:1302–10. https://doi.org/10.1016/S0140-6736(16)30370-1.
Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults a systematic review and meta-analysis. Ann Intern Med. 2015;162:123–32. https://doi.org/10.7326/M14-1651.
Matthews CE, Carlson SA, Saint-Maurice PF, et al. Sedentary behavior in U.S. adults: fall 2019. Med Sci Sports Exerc. 2021;53:2512–9. https://doi.org/10.1249/MSS.0000000000002751.
Clemes SA, Houdmont J, Munir F, et al. Descriptive epidemiology of domain-specific sitting in working adults: the Stormont Study. J Public Health (Oxf). 2016;38:53–60. https://doi.org/10.1093/PUBMED/FDU114.
Clemes SA, Oêconnell SE, Edwardson CL. Office workers’ objectively measured sedentary behavior and physical activity during and outside working hours. J Occup Environ Med. 2014;56:298–303. https://doi.org/10.1097/JOM.0000000000000101.
Bauman A, Ainsworth BE, Sallis JF, et al. The descriptive epidemiology of sitting: a 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am J Prev Med. 2011;41:228–35. https://doi.org/10.1016/J.AMEPRE.2011.05.003.
Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care. 2008;31:369–71. https://doi.org/10.2337/DC07-1795.
Jans MP, Proper KI, Hildebrandt VH. Sedentary behavior in Dutch workers: differences between occupations and business sectors. Am J Prev Med. 2007;33:450–4. https://doi.org/10.1016/J.AMEPRE.2007.07.033.
Mabry R, Koohsari MJ, Bull F, et al. A systematic review of physical activity and sedentary behaviour research in the oil-producing countries of the Arabian Peninsula. BMC Public Health. 2016;16:1–22. https://doi.org/10.1186/S12889-016-3642-4.
Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–81. https://doi.org/10.1093/AJE/KWM390.
Thorp AA, Healy GN, Winkler E, et al. Prolonged sedentary time and physical activity in workplace and non-work contexts: a cross-sectional study of office, customer service and call centre employees. Int J Behav Nutr Phys Act. 2012;9:1–9. https://doi.org/10.1186/1479-5868-9-128/.
Win AM, Yen LW, Tan KH, et al. Patterns of physical activity and sedentary behavior in a representative sample of a multi-ethnic South-East Asian population: a cross-sectional study. BMC Public Health. 2015;15:1–11. https://doi.org/10.1186/S12889-015-1668-7/TABLES/2.
Paterson C, Fryer S, Stone K, et al. The effects of acute exposure to prolonged sitting, with and without interruption, on peripheral blood pressure among adults: a systematic review and meta-analysis. Sports Med. 2022;52:1369–83. https://doi.org/10.1007/S40279-021-01614-7.
Paterson C, Fryer S, Zieff G, et al. The effects of acute exposure to prolonged sitting, with and without interruption, on vascular function among adults: a meta-analysis. Sports Med. 2020;50:1929–42. https://doi.org/10.1007/S40279-020-01325-5.
Loh R, Stamatakis E, Folkerts D, et al. Effects of interrupting prolonged sitting with physical activity breaks on blood glucose, insulin and triacylglycerol measures: a systematic review and meta-analysis. Sports Med. 2020;50:295–330. https://doi.org/10.1007/S40279-019-01183-W.
Stoner L, Barone Gibbs B, Meyer ML, et al. A primer on repeated sitting exposure and the cardiovascular system: considerations for study design, analysis, interpretation, and translation. Front Cardiovasc Med. 2021;8: 716938. https://doi.org/10.3389/FCVM.2021.716938.
Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–62. https://doi.org/10.1136/BJSPORTS-2020-102955.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/BMJ.N71.
Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. Second Edition. Hoboken: Wiley-Blackwell; 2019. https://doi.org/10.1002/9781119536604.
Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9:671–5. https://doi.org/10.1038/nmeth.2089.
Perks J, Zaccardi F, Paterson C, et al. Effect of high-pain versus low-pain structured exercise on walking ability in people with intermittent claudication: meta-analysis. Br J Surg. 2022;109:686–94. https://doi.org/10.1093/bjs/znac134.
Champion RB, Smith LR, Smith J, et al. Reducing prolonged sedentary time using a treadmill desk acutely improves cardiometabolic risk markers in male and female adults. J Sports Sci. 2018;36:2484–91. https://doi.org/10.1080/02640414.2018.1464744.
Larsen RN, Kingwell BA, Sethi P, et al. Breaking up prolonged sitting reduces resting blood pressure in overweight/obese adults. Nutr Metab Cardiovasc Dis. 2014;24:976–82. https://doi.org/10.1016/j.numecd.2014.04.011.
Wheeler MJ, Dunstan DW, Ellis KA, et al. Effect of morning exercise with or without breaks in prolonged sitting on blood pressure in older overweight/obese adults: evidence for sex differences. Hypertension. 2019;73:859–67. https://doi.org/10.1161/HYPERTENSIONAHA.118.12373.
Bailey DP, Locke CD. Breaking up prolonged sitting with light-intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. J Sci Med Sport. 2015;18:294–8. https://doi.org/10.1016/J.JSAMS.2014.03.008.
Younger AM, Pettitt RW, Sexton PJ, et al. Acute moderate exercise does not attenuate cardiometabolic function associated with a bout of prolonged sitting. J Sports Sci. 2015;34:658–63. https://doi.org/10.1080/02640414.2015.1068435.
Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:I4898. https://doi.org/10.1136/BMJ.L4898.
Team RC. R: a language and environment for statistical computing. 2022. https://www.r-project.org/. Accessed 25 Aug 2023.
Viechtbauer W. Conducting meta-analyses in R with the metafor. J Stat Softw. 2010;36:1–48. https://doi.org/10.18637/JSS.V036.I03.
Harrell FE. Regression modeling strategies. New York: Springer International Publishing; 2015. https://doi.org/10.1007/978-3-319-19425-7.
Viechtbauer W, Cheung MW-L. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1:112–25. https://doi.org/10.1002/jrsm.11.
Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557. https://doi.org/10.1136/BMJ.327.7414.557.
Dobashi S, Kawaguchi S, Ando D, et al. Alternating work posture improves postprandial glucose response without reducing computer task performance in the early afternoon. Physiol Behav. 2021;237: 113431. https://doi.org/10.1016/j.physbeh.2021.113431.
Morishima T, Tsuchiya Y, Padilla J, et al. Eight weeks of fish oil supplementation does not prevent sitting-induced leg endothelial dysfunction. Appl Physiol Nutr Metab. 2020;45:55–60. https://doi.org/10.1139/apnm-2019-0138.
Morishima T, Iemitsu M, Fujie S, et al. Prior beetroot juice ingestion offsets endothelial dysfunction following prolonged sitting. J Appl Physiol. 2022;133:69–74. https://doi.org/10.1152/JAPPLPHYSIOL.00200.2022/ASSET/IMAGES/MEDIUM/JAPPL-00200-2022R01.PNG.
Dempsey PC, Sacre JW, Larsen RN, et al. Interrupting prolonged sitting with brief bouts of light walking or simple resistance activities reduces resting blood pressure and plasma noradrenaline in type 2 diabetes. J Hypertens. 2016;34:2376–82. https://doi.org/10.1097/HJH.0000000000001101.
Miyashita M, Burns SF, Stensel DJ. Accumulating short bouts of brisk walking reduces postprandial plasma triacylglycerol concentrations and resting blood pressure in healthy young men. Am J Clin Nutr. 2008;88:1225–31. https://doi.org/10.3945/AJCN.2008.26493.
Gotshall RW, Aten LA, Yumikura S. Difference in the cardiovascular response to prolonged sitting in men and women. Can J Appl Physiol. 1994;19:215–25. https://doi.org/10.1139/h94-016.
Carter SE, Gladwell VF. Effect of breaking up sedentary time with callisthenics on endothelial function. J Sports Sci. 2017;35:1508–14. https://doi.org/10.1080/02640414.2016.1223331.
Freire YA, de Araújo Dantas de Macêdo G, Browne RAV, et al. Effect of breaks in prolonged sitting or low-volume high-intensity interval exercise on markers of metabolic syndrome in adults with excess body fat: a crossover trial. J Phys Act Health. 2019;16:727–35. https://doi.org/10.1123/JPAH.2018-0492.
Barone Gibbs B, Kowalsky RJ, Perdomo SJ, et al. Effect of alternating standing and sitting on blood pressure and pulse wave velocity during a simulated workday in adults with overweight/obesity. J Hypertens. 2017;35:2411–8. https://doi.org/10.1097/HJH.0000000000001463.
Kruse NT, Hughes WE, Benzo RM, et al. Workplace strategies to prevent sitting-induced endothelial dysfunction. Med Sci Sports Exerc. 2018;50:801–8. https://doi.org/10.1249/MSS.0000000000001484.
Kowalsky RJ, Jakicic JM, Hergenroeder A, et al. Acute cardiometabolic effects of interrupting sitting with resistance exercise breaks. Appl Physiol Nutr Metab. 2019;44:1025–32. https://doi.org/10.1139/apnm-2018-0633.
Taylor FC, Dunstan DW, Homer AR, et al. Acute effects of interrupting prolonged sitting on vascular function in type 2 diabetes. Am J Physiol Heart Circ Physiol. 2021;320:H393-403. https://doi.org/10.1152/AJPHEART.00422.2020/ASSET/IMAGES/LARGE/AJ-AHRT200086F004.JPEG.
Evans WS, Stoner L, Willey Q, et al. Local exercise does not prevent the aortic stiffening response to acute prolonged sitting: a randomized crossover trial. J Appl Physiol. 2019;127:781–7. https://doi.org/10.1152/japplphysiol.00318.2019.
Lunde MSH, Hjellset VT, Høstmark AT. Slow post meal walking reduces the blood glucose response: an exploratory study in female Pakistani immigrants. J Immigr Minor Health. 2012;14:816–22. https://doi.org/10.1007/S10903-012-9574-X.
Park SY, Wooden TSK, Pekas EJ, et al. Effects of passive and active leg movements to interrupt sitting in mild hypercapnia on cardiovascular function in healthy adults. J Appl Physiol. 2022;132:874–87. https://doi.org/10.1152/japplphysiol.00799.2021.
Peddie MC, Kessell C, Bergen T, et al. The effects of prolonged sitting, prolonged standing, and activity breaks on vascular function, and postprandial glucose and insulin responses: a randomised crossover trial. PLoS ONE. 2021;16: e0244841. https://doi.org/10.1371/journal.pone.0244841.
Wennberg P, Boraxbekk CJ, Wheeler M, et al. Acute effects of breaking up prolonged sitting on fatigue and cognition: a pilot study. BMJ Open. 2016;6:1–9. https://doi.org/10.1136/bmjopen-2015-009630.
Carter SE, Draijer R, Holder SM, et al. Effect of different walking break strategies on superficial femoral artery endothelial function. Physiol Rep. 2019;7: e14190. https://doi.org/10.14814/phy2.14190.
Cho MJ, Bunsawat K, Kim HJ, et al. The acute effects of interrupting prolonged sitting with stair climbing on vascular and metabolic function after a high-fat meal. Eur J Appl Physiol. 2020;120:829–39. https://doi.org/10.1007/s00421-020-04321-9.
Ballard KD, Duguid RM, Berry CW, et al. Effects of prior aerobic exercise on sitting-induced vascular dysfunction in healthy men. Eur J Appl Physiol. 2017;117:2509–18. https://doi.org/10.1007/s00421-017-3738-2.
Headid RJ, Pekas EJ, Wooden TK, et al. Impacts of prolonged sitting with mild hypercapnia on vascular and autonomic function in healthy recreationally active adults. Am J Physiol Heart Circ Physiol. 2020;319:H468–80. https://doi.org/10.1152/AJPHEART.00354.2020.
Morishima T, Restaino RM, Walsh LK, et al. Prior exercise and standing as strategies to circumvent sitting-induced leg endothelial dysfunction. Clin Sci. 2017;131:1045–53. https://doi.org/10.1042/CS20170031.
O’Brien MW, Johns JA, Al-Hinnawi A, et al. Popliteal flow-mediated dilatory responses to an acute bout of prolonged sitting between earlier and later phases of natural menstrual and oral contraceptive pill cycles. J Appl Physiol. 2020;129:637–45. https://doi.org/10.1152/japplphysiol.00424.2020.
Vranish JR, Young BE, Kaur J, et al. Influence of sex on microvascular and macrovascular responses to prolonged sitting. Am J Physiol Heart Circ Physiol. 2017;312:H800–5. https://doi.org/10.1152/ajpheart.00823.2016.
O’Brien MW, Johns JA, Williams TD, et al. Sex does not influence impairments in popliteal endothelial-dependent vasodilator or vasoconstrictor responses following prolonged sitting. J Appl Physiol. 2019;127:679–87. https://doi.org/10.1152/japplphysiol.00887.2018.
Garten RS, Hogwood AC, Weggen JB, et al. Aerobic training status does not attenuate prolonged sitting-induced lower limb vascular dysfunction. Appl Physiol Nutr Metab. 2019;44:425–33. https://doi.org/10.1139/apnm-2018-0420.
Sugawara J, Tanabe T, Miyachi M, et al. Non-invasive assessment of cardiac output during exercise in healthy young humans: comparison between Modelflow method and Doppler echocardiography method. Acta Physiol Scand. 2003;179:361–6.
Meah VL, Backx K, Shave RE, et al. Comparison between Modelflow® and echocardiography in the determination of cardiac output during and following pregnancy at rest and during exercise. J Hum Sport Exerc. 2022;17:116–35. https://doi.org/10.14198/JHSE.2022.171.12.
Tam E, Azabji Kenfack M, Cautero M, et al. Correction of cardiac output obtained by Modelflow from finger pulse pressure profiles with a respiratory method in humans. Clin Sci. 2004;106:371–6. https://doi.org/10.1042/CS20030302.
Ahuja KD, Robertson IK, Ball MJ. Acute effects of food on postprandial blood pressure and measures of arterial stiffness in healthy humans. Am J Clin Nutr. 2009;90:298–303. https://doi.org/10.3945/ajcn.2009.27771.
Visvanathan R, Chen R, Garcia M, et al. The effects of drinks made from simple sugars on blood pressure in healthy older people. Br J Nutr. 2005;93:575–9. https://doi.org/10.1079/BJN20051401.
Morishima T, Tsuchiya Y, Ueda H, et al. Sitting-induced endothelial dysfunction is prevented in endurance-trained individuals. Med Sci Sports Exerc. 2020;52:1770–5. https://doi.org/10.1249/MSS.0000000000002302.
Horiuchi M, Stoner L. Effects of compression stockings on lower-limb venous and arterial system responses to prolonged sitting: a randomized cross-over trial. Vasc Med. 2021;26:386–93. https://doi.org/10.1177/1358863X20988899.
Credeur DP, Miller SM, Jones R, et al. Impact of prolonged sitting on peripheral and central vascular health. Am J Cardiol. 2019;123:260–6. https://doi.org/10.1016/j.amjcard.2018.10.014.
Stergiopulos N, Meister JJ, Westerhof N. Determinants of stroke volume and systolic and diastolic aortic pressure. Am J Physiol. 1996;270(6 Pt 2):H2050–9. https://doi.org/10.1152/AJPHEART.1996.270.6.H2050.
Shvartz E, Gaume JG, White RT, et al. Hemodynamic responses during prolonged sitting. J Appl Physiol. 1983;54:1673–80. https://doi.org/10.1152/JAPPL.1983.54.6.1673.
Morishima T, Restaino RM, Walsh LK, et al. Prolonged sitting-induced leg endothelial dysfunction is prevented by fidgeting. Am J Physiol Heart Circ Physiol. 2016;311:H177–82. https://doi.org/10.1152/ajpheart.00297.2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the National Heart, Lung, and Blood Institute Grants R01 HL157187 and R01 HL162805A (both to Lee Stoner).
Conflict of interest
Nathan T. Adams, Craig Paterson, Simon Higgins, Jillian Poles, and Lee Stoner have no conflicts of interest that are directly relevant to the content of this review.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The data analyzed for this meta-analysis and the corresponding R script for analysis are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
Conceptualization: NA, CP, and LS. Literature search: NA and JP. Quality assessment: NA and JP. Data extraction: NA and JP. Data analysis: NA and CP. NA and CP wrote the first draft of the manuscript. SH, JP, and LS revised the original manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Adams, N.T., Paterson, C., Poles, J. et al. The Effect of Sitting Duration on Peripheral Blood Pressure Responses to Prolonged Sitting, With and Without Interruption: A Systematic Review and Meta-Analysis. Sports Med 54, 169–183 (2024). https://doi.org/10.1007/s40279-023-01915-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-023-01915-z