Abstract
Background
Previous reviews have shown that exposure to acute prolonged sitting can have detrimental effects on several cardiovascular and cardiometabolic health markers. However, to date, there has been no synthesis of peripheral blood pressure data (including systolic blood pressure, diastolic blood pressure and mean arterial pressure), an important and translatable marker of cardiovascular health. Similarly, no previous study has consolidated the effects of sitting interruptions on peripheral blood pressure.
Objectives
We aimed to (1) assess the effect of exposure to acute prolonged sitting on peripheral blood pressure and (2) determine the efficacy of sitting interruption strategies as a means of offsetting any negative effects. Subgroup analyses by age and interruption modality were performed to explore heterogeneity.
Data Sources
Electronic databases (PubMed, Web of Science and, SPORTDiscus) were searched from inception to March 2021. Reference lists of eligible studies and relevant reviews were also screened.
Study Selection
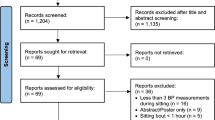
Inclusion criteria for objective (1) were: (i) peripheral blood pressure was assessed non-invasively in the upper limb pre-sitting and post-sitting; (ii) studies were either randomised controlled, randomised crossover or quasi-experimental pre-test vs post-test trials; (iii) the sitting period was ≥ 1 h; (iv) pre-sitting and post-sitting measures were performed in the same posture; and (v) participants were adults (aged ≥ 18 years), free of autonomic or neuromuscular dysfunction. Additional criteria for objective (2) were: (i) the interruption strategy was during the sitting period; (ii) there was an uninterrupted sitting control condition; and (iii) the interruption strategy must have involved participants actively moving their upper or lower limbs.
Appraisal and Synthesis Methods
In total, 9763 articles were identified, of which 33 met inclusion criteria for objective (1). Of those articles, 22 met inclusion criteria for objective (2). Weighted mean difference (WMD), 95% confidence intervals (95% CI), and standardised mean difference (SMD) were calculated for all trials using inverse variance heterogeneity meta-analysis modelling. Standardised mean difference was used to determine the magnitude of effect, where < 0.2, 0.2, 0.5 and 0.8 were defined as trivial, small, moderate and large, respectively.
Results
(1) Prolonged uninterrupted sitting resulted in trivial and small significant increases in systolic blood pressure (WMD = 3.2 mmHg, 95% CI 0.6 to 5.8, SMD = 0.14) and mean arterial pressure (WMD = 3.3 mmHg, 95% CI 2.2 to 4.4, SMD = 0.37), respectively, and a non-significant trivial increase in diastolic blood pressure. Subgroup analyses indicated that the increases in systolic blood pressure and mean arterial pressure were more pronounced in younger age groups. (2) Interrupting bouts of prolonged sitting resulted in significantly lower systolic blood pressure (WMD = − 4.4 mmHg, 95% CI − 7.4 to − 1.5, SMD = 0.26) and diastolic blood pressure (WMD = − 2.4 mmHg, 95% CI − 4.5 to − 0.3, SMD = 0.19) compared with control conditions, particularly when using aerobic interruption strategies.
Conclusions
Exposure to acute prolonged uninterrupted sitting results in significant increases in systolic blood pressure and mean arterial pressure, particularly in younger age groups. Regularly interrupting bouts of prolonged sitting, particularly with aerobic interruption strategies may reduce negative effects.

Similar content being viewed by others
References
Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary Behavior Research Network (SBRN): terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14:75.
Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388:1302–10.
Ekelund U, Brown WJ, Steene-Johannessen J, Fagerland MW, Owen N, Powell KE, et al. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2019;53:886–94.
Paterson C, Fryer S, Zieff G, Stone K, Credeur DP, Barone Gibbs B, et al. The effects of acute exposure to prolonged sitting, with and without interruption, on vascular function among adults: a meta-analysis. Sports Med. 2020;50:1929–42.
Benatti FB, Ried-Larsen M. The effects of breaking up prolonged sitting time: a review of experimental studies. Med Sci Sports Exerc. 2015;47:2053–61.
Chastin SFM, Egerton T, Leask C, Stamatakis E. Meta-analysis of the relationship between breaks in sedentary behavior and cardiometabolic health. Obesity. 2015;23:1800–10.
Saunders TJ, Atkinson HF, Burr J, MacEwen B, Skeaff CM, Peddie MC. The acute metabolic and vascular impact of interrupting prolonged sitting: a systematic review and meta-analysis. Sports Med. 2018;48:2347–66.
Loh R, Stamatakis E, Folkerts D, Allgrove JE, Moir HJ. Effects of interrupting prolonged sitting with physical activity breaks on blood glucose, insulin and triacylglycerol measures: a systematic review and meta-analysis. Sports Med. 2020;50:295–330.
Barone Gibbs B, Kowalsky RJ, Perdomo SJ, Taormina JM, Balzer JR, Jakicic JM. Effect of alternating standing and sitting on blood pressure and pulse wave velocity during a simulated workday in adults with overweight/obesity. J Hypertens. 2017;35:2411–8.
Carter SE, Draijer R, Holder SM, Brown L, Thijssen DH, Hopkins ND. Regular walking breaks prevent the decline in cerebral blood flow associated with prolonged sitting. J Appl Physiol. 2018;125:790–8.
Evans WS, Stoner L, Willey Q, Kelsch E, Credeur DP, Hanson ED. Local exercise does not prevent the aortic stiffening response to acute prolonged sitting: a randomized crossover trial. J Appl Physiol. 1985;2019(127):781–7.
Garten RS, Hogwood AC, Weggen JB, Fralin RC, LaRosa K, Lee D, et al. Aerobic training status does not attenuate prolonged sitting-induced lower limb vascular dysfunction. Appl Physiol Nutr Metab. 2019;44:425–33.
Larsen RN, Kingwell BA, Sethi P, Cerin E, Owen N, Dunstan DW. Breaking up prolonged sitting reduces resting blood pressure in overweight/obese adults. Nutr Metab Cardiovasc Dis. 2014;24:976–82.
Morishima T, Restaino RM, Walsh LK, Kanaley JA, Padilla J. Prior exercise and standing as strategies to circumvent sitting-induced leg endothelial dysfunction. Clin Sci. 2017;131:1045–53.
Morishima T, Tsuchiya Y, Ueda H, Tsuji K, Ochi E. Sitting-induced endothelial dysfunction is prevented in endurance-trained individuals. Med Sci Sports Exerc. 2020;52:1770–5.
Morishima T, Tsuchiya Y, Padilla J, Ochi E. Eight weeks of fish oil supplementation does not prevent sitting-induced leg endothelial dysfunction. Appl Physiol Nutr Metab. 2020;45:55–60.
O’Brien MW, Johns JA, Al-Hinnawi A, Kimmerly DS. Popliteal flow-mediated dilatory responses to a bout of prolonged sitting between earlier and later phases of natural menstrual and contraceptive pill cycles. J Appl Physiol. 1985;2020(129):637–45.
O’Brien MW, Johns JA, Williams TD, Kimmerly DS. Sex does not influence impairments in popliteal endothelial-dependent vasodilator or vasoconstrictor responses following prolonged sitting. J Appl Physiol. 1985;2019(127):679–87.
Vranish JR, Young BE, Kaur J, Patik JC, Padilla J, Fadel PJ. Influence of sex on microvascular and macrovascular responses to prolonged sitting. Am J Physiol Heart Circ Physiol. 2017;312:H800–5.
Champion RB, Smith LR, Smith J, Hirlav B, Maylor BD, White SL, et al. Reducing prolonged sedentary time using a treadmill desk acutely improves cardiometabolic risk markers in male and female adults. J Sports Sci. 2018;36:2484–91.
Kowalsky RJ, Jakicic JM, Hergenroeder A, Rogers RJ, Gibbs BB. Acute cardiometabolic effects of interrupting sitting with resistance exercise breaks. Appl Physiol Nutr Metab Physiol Appl Nutr Metab. 2019;44:1025–32.
Zeigler ZS, Mullane SL, Crespo NC, Buman MP, Gaesser GA. Effects of standing and light-intensity activity on ambulatory blood pressure. Med Sci Sports Exerc. 2016;48:175–81.
Clemes SA, O’connell SE, Edwardson CL. Office workers’ objectively measured sedentary behavior and physical activity during and outside working hours. J Occup Environ Med. 2014;56:298–303.
Clemes SA, Houdmont J, Munir F, Wilson K, Kerr R, Addley K. Descriptive epidemiology of domain-specific sitting in working adults: the Stormont Study. J Public Health. 2015;38:53–60.
Bauman A, Ainsworth BE, Sallis JF, Hagströmer M, Craig CL, Bull FC, et al. The descriptive epidemiology of sitting: a 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am J Prev Med. 2011;41:228–35.
Healy GN, Wijndaele K, Dunstan DW, Shaw JE, Salmon J, Zimmet PZ, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care. 2008;31:369–71.
Jans MP, Proper KI, Hildebrandt VH. Sedentary behavior in Dutch workers: differences between occupations and business sectors. Am J Prev Med. 2007;33:450–4.
Mabry R, Koohsari MJ, Bull F, Owen N. A systematic review of physical activity and sedentary behaviour research in the oil-producing countries of the Arabian Peninsula. BMC Public Health. 2016;16:1003.
Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–81.
Thorp AA, Healy GN, Winkler E, Clark BK, Gardiner PA, Owen N, et al. Prolonged sedentary time and physical activity in workplace and non-work contexts: a cross-sectional study of office, customer service and call centre employees. Int J Behav Nutr Phys Act. 2012;9:128.
Win AM, Yen LW, Tan KH, Lim RBT, Chia KS, Mueller-Riemenschneider F. Patterns of physical activity and sedentary behavior in a representative sample of a multi-ethnic South-East Asian population: a cross-sectional study. BMC Public Health. 2015;15:318.
Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20:21–35.
Safar ME. Systolic blood pressure, pulse pressure and arterial stiffness as cardiovascular risk factors. Curr Opin Nephrol Hypertens. 2001;10:257–61.
Safar ME, Nilsson PM, Blacher J, Mimran A. Pulse pressure, arterial stiffness, and end-organ damage. Curr Hypertens Rep. 2012;14:339–44.
Belz GG. Elastic properties and Windkessel function of the human aorta. Cardiovasc Drugs Ther. 1995;9:73–83.
Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75:285–92.
Mitchell GF. Effects of central arterial aging on the structure and function of the peripheral vasculature: implications for end-organ damage. J Appl Physiol. 2008;105:1652–60.
Yoon HE, Choi BS. The renin-angiotensin system and aging in the kidney. Korean J Intern Med. 2014;29:291–5.
Department of Health and Social Care. UK Chief Medical Officers’ physical activity guidelines. 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832868/uk-chief-medical-officers-physical-activity-guidelines.pdf. Accessed 2 Dec 2021.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–62.
Australian Government Department of Health. Australia’s physical activity and sedentary behaviour guidelines: tips and ideas for adults (18–64 years). Australian Government Department of Health. https://www1.health.gov.au/internet/main/publishing.nsf/Content/ti-18-64years. Accessed 31 July 2020.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Schneider CA, Rasband WS, Eliceiri KW. NIH image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9:671–5.
Hallgren KA. Computing inter-rater reliability for observational data: an overview and tutorial. Tutor Quant Methods Psychol. 2012;8:23.
Heyland DK, Novak F, Drover JW, Jain M, Su X, Suchner U. Should immunonutrition become routine in critically ill patients? A systematic review of the evidence. JAMA. 2001;286:944–53.
Heyland DK, MacDonald S, Keefe L, Drover JW. Total parenteral nutrition in the critically ill patient: a meta-analysis. JAMA. 1998;280:2013–9.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Chichester: Wiley; 2008.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria; 2020. https://www.R-project.org/. Accessed 2 Dec 2021.
Cohen J. Quantitative methods in psychology: a power primer. Psychol Bull. 1992;112:1155–9.
Doi SAR, Barendregt JJ, Khan S, Thalib L, Williams GM. Advances in the meta-analysis of heterogeneous clinical trials I: the inverse variance heterogeneity model. Contemp Clin Trials. 2015;45:130–8.
Viechtbauer W, Cheung MW-L. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1:112–25.
Furuya-Kanamori L, Barendregt JJ, Doi SA. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int J Evid Based Healthc. 2018;16:195–203.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Bhammar DM, Sawyer BJ, Tucker WJ, Gaesser GA. Breaks in sitting time: effects on continuously monitored glucose and blood pressure. Med Sci Sports Exerc. 2017;49:2119–30.
Wheeler MJ, Dunstan DW, Ellis KA, Cerin E, Phillips S, Lambert G, et al. Effect of morning exercise with or without breaks in prolonged sitting on blood pressure in older overweight/obese adults. Hypertension. 2019;73:859–67.
Climie RE, Wheeler MJ, Grace M, Lambert EA, Cohen N, Owen N, et al. Simple intermittent resistance activity mitigates the detrimental effect of prolonged unbroken sitting on arterial function in overweight and obese adults. J Appl Physiol. 2018;125:1787–94.
Dempsey PC, Sacre JW, Larsen RN, Straznicky NE, Sethi P, Cohen ND, et al. Interrupting prolonged sitting with brief bouts of light walking or simple resistance activities reduces resting blood pressure and plasma noradrenaline in type 2 diabetes. J Hypertens. 2016;34:2376–82.
Dogra S, Wolf M, Jeffrey MP, Foley RC, Logan-Sprenger H, Jones-Taggart H, et al. Disrupting prolonged sitting reduces IL-8 and lower leg swell in active young adults. BMC Sports Sci Med Rehabil. 2019;11:23.
Freire YA, de Macêdo GAD, Browne RAV, Farias-Junior LF, Bezerra ÁDL, Fayh APT, et al. Effect of breaks in prolonged sitting or low-volume high-intensity interval exercise on markers of metabolic syndrome in adults with excess body fat: a crossover trial. J Phys Act Health. 2019;16:727–35.
Headid RJ, Pekas EJ, Wooden TK, Son W-M, Layec G, Shin J, et al. Impacts of prolonged sitting with mild hypercapnia on vascular and autonomic function in healthy recreationally active adults. Am J Physiol Heart Circ Physiol. 2020;319:H468–80.
Kruse NT, Hughes WE, Benzo RM, Carr LJ, Casey DP. Workplace strategies to prevent sitting-induced endothelial dysfunction. Med Sci Sports Exerc. 2018;50:801–8.
Peddie MC, Kessell C, Bergen T, Gibbons TD, Campbell HA, Cotter JD, et al. The effects of prolonged sitting, prolonged standing, and activity breaks on vascular function, and postprandial glucose and insulin responses: a randomised crossover trial. PLoS ONE. 2021;16:e0244841.
Taylor FC, Dunstan DW, Homer AR, Dempsey PC, Kingwell BA, Climie RE, et al. Acute effects of interrupting prolonged sitting on vascular function in type 2 diabetes. Am J Physiol-Heart Circ Physiol. 2020;320:H393-403.
Wennberg P, Boraxbekk C-J, Wheeler M, Howard B, Dempsey PC, Lambert G, et al. Acute effects of breaking up prolonged sitting on fatigue and cognition: a pilot study. BMJ Open. 2016;6:e009630.
Yates T, Edwardson CL, Celis-Morales C, Biddle SJH, Bodicoat D, Davies MJ, et al. Metabolic effects of breaking prolonged sitting with standing or light walking in older South Asians and white Europeans: a randomized acute study. J Gerontol A Biol Sci Med Sci. 2020;75:139–46.
Kerr J, Crist K, Vital DG, Dillon L, Aden SA, Trivedi M, et al. Acute glucoregulatory and vascular outcomes of three strategies for interrupting prolonged sitting time in postmenopausal women: a pilot, laboratory-based, randomized, controlled, 4-condition, 4-period crossover trial. PLoS ONE. 2017;12:e0188544.
Carter SE, Gladwell VF. Effect of breaking up sedentary time with callisthenics on endothelial function. J Sports Sci. 2017;35:1508–14.
Credeur DP, Miller SM, Jones R, Stoner L, Dolbow DR, Fryer SM, et al. Impact of prolonged sitting on peripheral and central vascular health. Am J Cardiol. 2019;123:260–6.
Charlett OP, Morari V, Bailey DP. Impaired postprandial glucose and no improvement in other cardiometabolic responses or cognitive function by breaking up sitting with bodyweight resistance exercises: a randomised crossover trial. J Sports Sci. 2021;39:792–800.
Hartman YA, Tillmans LC, Benschop DL, Hermans AN, Nijssen KM, Eijsvogels TM, et al. Long-term and acute benefits of reduced sitting on vascular flow and function. Med Sci Sports Exerc. 2021;53:341–50.
Decker KP, Feliciano PG, Kimmel MT, Hogwood AC, Weggen JB, Darling AM, et al. Examining sex differences in sitting-induced microvascular dysfunction: insight from acute vitamin C supplementation. Microvasc Res. 2021;135:104147.
Ballard KD, Duguid RM, Berry CW, Dey P, Bruno RS, Ward RM, et al. Effects of prior aerobic exercise on sitting-induced vascular dysfunction in healthy men. Eur J Appl Physiol. 2017;117:2509–18.
Turner JR, Viera AJ, Shimbo D. Ambulatory blood pressure monitoring in clinical practice: a review. Am J Med. 2015;128:14–20.
Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006;354:2368–74.
Hodgkinson J, Mant J, Martin U, Guo B, Hobbs FDR, Deeks JJ, et al. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BMJ. 2011;342:d3621.
Millar-Craig M, Bishop C, Raftery EB. Circadian variation of blood pressure. Lancet. 1978;311:795–7.
Mancia G, Ferrari A, Gregorini L, Parati G, Pomidossi G, Bertinieri G, et al. Blood pressure and heart rate variabilities in normotensive and hypertensive human beings. Circ Res. 1983;53:96–104.
Smolensky MH, Hermida RC, Portaluppi F. Circadian mechanisms of 24-hour blood pressure regulation and patterning. Sleep Med Rev. 2017;33:4–16.
Kawano Y. Diurnal blood pressure variation and related behavioral factors. Hypertens Res. 2011;34:281–5.
Morishima T, Restaino RM, Walsh LK, Kanaley JA, Fadel PJ, Padilla J. Prolonged sitting-induced leg endothelial dysfunction is prevented by fidgeting. Am J Physiol Heart Circ Physiol. 2016;311:H177-182.
Shvartz E, Gaume JG, White RT, Reibold RC. Hemodynamic responses during prolonged sitting. J Appl Physiol. 1983;54:1673–80.
Restaino RM, Holwerda SW, Credeur DP, Fadel PJ, Padilla J. Impact of prolonged sitting on lower and upper limb micro-and macrovascular dilator function. Exp Physiol. 2015;100:829–38.
Stone KJ, Fryer SM, Ryan T, Stoner L. The validity and reliability of continuous-wave near-infrared spectroscopy for the assessment of leg blood volume during an orthostatic challenge. Atherosclerosis. 2016;251:234–9.
Atlas SA. The renin-angiotensin aldosterone system: pathophysiological role and pharmacologic inhibition. J Manag Care Pharm. 2007;13:9–20.
Stoner L, Stone K, Zieff G, Blackwell J, Diana J, Credeur DP, et al. Endothelium function dependence of acute changes in pulse wave velocity and flow-mediated slowing. Vasc Med. 2020;25:419–26.
Schmitt M, Avolio A, Qasem A, McEniery CM, Butlin M, Wilkinson IB, et al. Basal NO locally modulates human iliac artery function in vivo. Hypertension. 2005;46:227–31.
Laughlin MH, Davis MJ, Secher NH, van Lieshout JJ, Arce-Esquivel AA, Simmons GH, et al. Peripheral circulation. Compr Physiol. 2011;2:321–447.
London G, Marchais S, Guerin A, Pannier B. Arterial stiffness: pathophysiology and clinical impact. Clin Exp Hypertens. 2004;26:689–99.
Van de Vosse FN, Stergiopulos N. Pulse wave propagation in the arterial tree. Annu Rev Fluid Mech. 2011;43:467–99.
Stergiopulos N, Meister JJ, Westerhof N. Determinants of stroke volume and systolic and diastolic aortic pressure. Am J Physiol. 1996;270:H2050–9.
Belmin J, Lévy BI, Michel J-B. Changes in the renin-angiotensin-aldosterone axis in later life. Drugs Aging. 1994;5:391–400.
Zozaya JL, Viloria MP, Castro A. The effect of age on the renin-angiotensin-aldosterone systems and other physiological variables in normal subjects. Res Commun Chem Pathol Pharmacol. 1983;42:463–70.
Halliwill JR. Mechanisms and clinical implications of post-exercise hypotension in humans. Exerc Sport Sci Rev. 2001;29:65–70.
MacDonald JR. Potential causes, mechanisms, and implications of post exercise hypotension. J Hum Hypertens. 2002;16:225–36.
Bhammar DM, Angadi SS, Gaesser GA. Effects of fractionized and continuous exercise on 24-h ambulatory blood pressure. Med Sci Sports Exerc. 2012;44:2270–6.
Angadi SS, Weltman A, Watson-Winfield D, Weltman J, Frick K, Patrie J, et al. Effect of fractionized vs continuous, single-session exercise on blood pressure in adults. J Hum Hypertens. 2010;24:300–2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflicts of interest/competing interests
Craig Paterson, Simon Fryer, Keeron Stone, Gabriel Zieff, Louise Turner and Lee Stoner declare that they have no conflicts of interest relevant to the content of this review.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of data and material
The data analysed for this meta-analysis and the corresponding R script for analysis are available from the corresponding author on reasonable request.
Authors’ contributions
Conceptualisation: CP and LS. Literature search: CP and LS. Quality assessment: CP, KS and SF. Data extraction: CP and GZ. Data analysis: CP and LS. CP, SF and KS wrote the first draft of the manuscript. GZ, LS and LT revised the original manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
40279_2021_1614_MOESM2_ESM.pdf
Supplementary file2 Electronic Supplementary Material Appendix S2 Forest plot for meta-analysis of the effect of uninterrupted sitting on systolic blood pressure (PDF 7 kb)
40279_2021_1614_MOESM3_ESM.pdf
Supplementary file3 Electronic Supplementary Material Appendix S3 Forest plot for meta-analysis of the effect of uninterrupted sitting on diastolic blood pressure (PDF 6 kb)
40279_2021_1614_MOESM4_ESM.pdf
Supplementary file4 Electronic Supplementary Material Appendix S4 Forest plot for meta-analysis of the effect of uninterrupted sitting on mean arterial pressure (PDF 7 kb)
40279_2021_1614_MOESM5_ESM.pdf
Supplementary file5 Electronic Supplementary Material Appendix S5 Forest plot for meta-analysis of the effect of interrupted sitting on systolic blood pressure (PDF 7 kb)
40279_2021_1614_MOESM6_ESM.pdf
Supplementary file6 Electronic Supplementary Material Appendix S6 Forest plot for meta-analysis of the effect of interrupted sitting on diastolic blood pressure (PDF 7 kb)
40279_2021_1614_MOESM7_ESM.docx
Supplementary file7 Electronic Supplementary Material Appendix S7 Subgroup analysis of mean arterial pressure, systolic, and diastolic blood pressure by assessment type (DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Paterson, C., Fryer, S., Stone, K. et al. The Effects of Acute Exposure to Prolonged Sitting, with and Without Interruption, on Peripheral Blood Pressure Among Adults: A Systematic Review and Meta-Analysis. Sports Med 52, 1369–1383 (2022). https://doi.org/10.1007/s40279-021-01614-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-021-01614-7