Abstract
Background
Lateral ankle sprains are the most common ankle injuries in sports and have the highest recurrence rates. Almost half of the patients experiencing lateral ankle sprains develop chronic ankle instability. Patients with chronic ankle instability experience persistent ankle dysfunctions and detrimental long-term sequelae. Changes at the brain level are put forward to explain these undesirable consequences and high recurrence rates partially. However, an overview of possible brain adaptations related to lateral ankle sprains and chronic ankle instability is currently lacking.
Objective
The primary purpose of this systematic review is to provide a comprehensive overview of the literature on structural and functional brain adaptations related to lateral ankle sprains and in patients with chronic ankle instability.
Methods
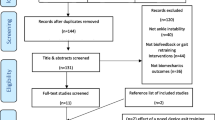
PubMed, Web of Science, Scopus, Embase, EBSCO—SPORTDiscus and Cochrane Central Register of Controlled Trials were systematically searched until 14 December, 2022. Meta-analyses, systematic reviews and narrative reviews were excluded. Included studies investigated functional or structural brain adaptations in patients who experienced a lateral ankle sprain or with chronic ankle instability and who were at least 18 years of age. Lateral ankle sprains and chronic ankle instability were defined following the recommendation of the International Ankle Consortium. Three authors independently extracted the data. They extracted the authors’ name, publication year, study design, inclusion criteria, participant characteristics, the sample size of the intervention and control groups, methods of neuroplasticity testing, as well as all means and standard deviations of primary and secondary neuroplasticity outcomes from each study. Data reported on copers were considered as part of the control group. The quality assessment tool for observational and cross-sectional studies was used for the risk of bias assessment. This study is registered on PROSPERO, number CRD42021281956.
Results
Twenty articles were included, of which only one investigated individuals who experienced a lateral ankle sprain. In all studies combined, 356 patients with chronic ankle instability, 10 who experienced a lateral ankle sprain and 46 copers were included. White matter microstructure changes in the cerebellum have been related to lateral ankle sprains. Fifteen studies reported functional brain adaptations in patients with chronic ankle instability, and five articles found structural brain outcomes. Alterations in the sensorimotor network (precentral gyrus and supplementary motor area, postcentral gyrus and middle frontal gyrus) and dorsal anterior cingulate cortex were mainly found in patients with chronic ankle instability.
Discussion
The included studies demonstrated structural and functional brain adaptations related to lateral ankle sprains and chronic ankle instability compared to healthy individuals or copers. These adaptations correlate with clinical outcomes (e.g. patients’ self-reported function and different clinical assessments) and might contribute to the persisting dysfunctions, increased re-injury risk and long-term sequelae seen in these patients. Thus, rehabilitation programmes should integrate sensorimotor and motor control strategies to cope with neuroplasticity related to ligamentous ankle injuries.


Similar content being viewed by others
References
Fong DT-PF, Hong Y, Chan L-K, Yung PS-H, Chan K-M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94.
Herzog MM, Kerr ZY, Marshall SW, Wikstrom EA. Epidemiology of ankle sprains and chronic ankle instability. J Athl Train. 2019;54(6):603–10.
Kemler E, van de Port I, Valkenberg H, Hoes AW, Backx FJ. Ankle injuries in the Netherlands: trends over 10–25 years. Scand J Med Sci Sports. 2015;25(3):331–7.
Hertel J. Functional instability following LAS. Sports Med. 2000;37(1):61–7.
Delahunt E, Bleakley CM, Bossard DS, Caulfield BM, Docherty CL, Doherty C, et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br J Sports Med. 2018;52(20):1304–10.
Dejong AF, Koldenhoven RM, Hertel J. Proximal adaptations in chronic ankle instability: systematic review and meta-analysis. Med Sci Sports Exerc. 2020;52(7):1563–75.
Thompson C, Schabrun S, Romero R, Bialocerkowski A, van Dieen J, Marshall P. Factors contributing to chronic ankle instability: a systematic review and meta-analysis of systematic reviews. Sports Med. 2018;48(1):189–205.
McKay CD, Goldie PA, Payne WR, Oakes BW. Ankle Injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103–8.
Van Dijk CN, Vuurberg G. There is no such thing as a simple ankle sprain: clinical commentary on the 2016 International Ankle Consortium position statement. Br J Sports Med. 2017;51(6):485–6.
Kaminski TW, Hertel J, Amendola N, Docherty CL, Dolan MG, Hopkins JT, et al. National Athletic Trainers’ Association position statement: conservative management and prevention of ankle sprains in athletes. J Athl Train. 2013;48(4):528–45.
Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT, et al. 2016 consensus statement of the International Ankle Consortium: prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50(24):1493–510.
Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: a prospective cohort analysis. Am J Sports Med. 2016;44(4):995–1003.
Terada M, Kosik KB, McCann RS, Gribble PA. Diaphragm contractility in individuals with chronic ankle instability. Med Sci Sports Exerc. 2016;48(10):2040–5.
Suttmiller AMB, McCann RS. Neural excitability of lower extremity musculature in individuals with and without chronic ankle instability: a systematic review and meta-analysis. J Electromyogr Kinesiol. 2020;53: 102436.
Miklovic TM, Donovan L, Protzuk OA, Kang MS, Feger MA. Acute lateral ankle sprain to chronic ankle instability: a pathway of dysfunction. Phys Sportsmed. 2018;46(1):116–22.
Khalaj N, Vicenzino B, Heales LJ, Smith MD. Is chronic ankle instability associated with impaired muscle strength? Ankle, knee and hip muscle strength in individuals with chronic ankle instability: a systematic review with meta-analysis. Br J Sports Med. 2020;54(14):839–471.
Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–75.
Xue X, Ma T, Li Q, Song Y, Hua Y. Chronic ankle instability is associated with proprioception deficits: a systematic review and meta-analysis. J Sport Health Sci. 2021;10(2):182–91.
Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34(4):612–20.
Hirose K, Murakami G, Minowa T, Kura H, Yamashita T. Lateral ligament injury of the ankle and associated articular cartilage degeneration in the talocrural joint: anatomic study using elderly cadavers. J Orthop Sci. 2004;9(1):37–43.
Golditz T, Steib S, Pfeifer K, Uder M, Gelse K, Janka R, et al. Functional ankle instability as a risk factor for osteoarthritis: using T2-mapping to analyze early cartilage degeneration in the ankle joint of young athletes. Osteoarthr Cartil. 2014;22(10):1377–85.
Hupperets MD, Verhagen EA, Heymans MW, Bosmans JE, van Tulder MW, van Mechelen W. Potential savings of a program to prevent ankle sprain recurrence: economic evaluation of a randomized controlled trial. Am J Sports Med. 2010;38(11):2194–200.
Tassignon B, Verschueren J, Delahunt E, Smith M, Vicenzino B, Verhagen E, et al. Criteria-based return to sport decision-making following lateral ankle sprain injury: a systematic review and narrative synthesis. Sports Med. 2019;49(4):601–19.
Smith MD, Vicenzino B, Bahr R, Bandholm T, Cooke R, Mendonca LM, et al. Return to sport decisions after an acute lateral ankle sprain injury: introducing the PAASS framework-an international multidisciplinary consensus. Br J Sports Med. 2021;55(22):1270–610.
Needle AR, Lepley AS, Grooms DR. Central nervous system adaptation after ligamentous injury: a summary of theories, evidence, and clinical interpretation. Sports Med. 2017;47(7):1271–88.
Ward S, Pearce AJ, Pietrosimone B, Bennell K, Clark R, Bryant AL. Neuromuscular deficits after peripheral joint injury: a neurophysiological hypothesis. Muscle Nerve. 2015;51(3):327–32.
Pietrosimone BG, McLeod MM, Lepley AS. A theoretical framework for understanding neuromuscular response to lower extremity joint injury. Sports Health. 2012;4(1):31–51.
Kim KM, Kim JS, Cruz-Díaz D, Ryu S, Kang M, Taube W. Changes in spinal and corticospinal excitability in patients with chronic ankle instability: a systematic review with meta-analysis. J Clin Med. 2019;8(7):1037.
Sharma N, Classen J, Cohen LG. Neural plasticity and its contribution to functional recovery. Handb Clin Neurol. 2013;110:3–12. https://doi.org/10.1016/B978-0-444-52901-5.00001-0.
Shitara H, Ichinose T, Shimoyama D, Sasaki T, Hamano N, Kamiyama M, et al. Neuroplasticity caused by peripheral proprioceptive deficits. Med Sci Sports Exerc. 2022;54(1):28–37.
Neto T, Sayer T, Theisen D, Mierau A. Functional brain plasticity associated with ACL injury: a scoping review of current evidence. Neural Plast. 2019;2019:3480512.
Kakavas G, Malliaropoulos N, Pruna R, Traster D, Bikos G, Maffulli N. Neuroplasticity and anterior cruciate ligament injury. Indian J Orthop. 2020;54(3):275–80.
Baumeister J, Reinecke K, Weiss M. Changed cortical activity after anterior cruciate ligament reconstruction in a joint position paradigm: an EEG study. Scand J Med Sci Sports. 2008;18(4):473–84.
Baumeister J, Reinecke K, Schubert M, Weiss M. Altered electrocortical brain activity after ACL reconstruction during force control. J Orthop Res. 2011;29(9):1383–910.
Kapreli E, Athanasopoulos S, Gliatis J, Papathanasiou M, Peeters R, Strimpakos N, et al. Anterior cruciate ligament deficiency causes brain plasticity: a functional MRI study. Am J Sports Med. 2009;37(12):2419–26.
Lepley AS, Ly MT, Grooms DR, Kinsella-Shaw JM, Lepley LK. Corticospinal tract structure and excitability in patients with anterior cruciate ligament reconstruction: a DTI and TMS study. Neuroimage Clin. 2020;25: 102157.
Diekfuss JA, Grooms DR, Yuan W, Dudley J, Barber Foss KD, Thomas S, et al. Does brain functional connectivity contribute to musculoskeletal injury? A preliminary prospective analysis of a neural biomarker of ACL injury risk. J Sci Med Sport. 2019;22(2):169–74.
Gokeler A, Neuhaus D, Benjaminse A, Grooms DR, Baumeister J. Principles of motor learning to support neuroplasticity after ACL injury: implications for optimizing performance and reducing risk of second ACL injury. Sports Med. 2019;49(6):853–65.
Rio E, Kidgell D, Moseley GL, Gaida J, Docking S, Purdam C, et al. Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. Br J Sports Med. 2016;50(4):209–15.
Grooms D, Appelbaum G, Onate J. Neuroplasticity following anterior cruciate ligament injury: a framework for visual-motor training approaches in rehabilitation. J Orthop Sports Phys Ther. 2015;45(5):381–93.
Grooms DR, Kiefer AW, Riley MA, Ellis JD, Thomas S, Kitchen K, et al. Brain-behavior mechanisms for the transfer of neuromuscular training adaptions to simulated sport: initial findings from the Train the Brain Project. J Sport Rehabil. 2018;27(5):1–5.
Ardern CL, Buttner F, Andrade R, Weir A, Ashe MC, Holden S, et al. Implementing the 27 PRISMA 2020 Statement items for systematic reviews in the sport and exercise medicine, musculoskeletal rehabilitation and sports science fields: the PERSiST (implementing Prisma in Exercise, Rehabilitation, Sport medicine and SporTs science) guidance. Br J Sports Med. 2022;56(4):175–95.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–6.
Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, et al. PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst Rev. 2021;10(1):39.
Gribble PA, Delahunt E, Bleakley CM, Caulfield B, Docherty CL, Fong DT, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. J Athl Train. 2014;49(1):121–7.
NIH. Study quality assessment tools; 2013. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed 30 Mar 2023.
McLeod MM, Gribble PA, Pietrosimone BG. Chronic ankle instability and neural excitability of the lower extremity. J Athl Train. 2015;50(8):847–53.
Harkey M, McLeod MM, Terada M, Gribble PA, Pietrosimone BG. Quadratic association between corticomotor and spinal-reflexive excitability and self-reported disability in participants with chronic ankle instability. J Sport Rehabil. 2016;25(2):137–45.
Terada M, Bowker S, Thomas AC, Pietrosimone B, Hiller CE, Gribble PA. Corticospinal excitability and inhibition of the soleus in individuals with chronic ankle instability. PM R. 2016;8(11):1090–6.
Kosik KB, Terada M, McCann RS, Drinkard CP, Gribble PA. Association between corticospinal inhibition and active dorsiflexion range of motion in patients with chronic ankle instability. Transl Sports Med. 2021;4(3):395–400.
Terada M, Kosik KB, McCann RS, Drinkard C, Gribble PA. Corticospinal activity during a single-leg stance in people with chronic ankle instability. J Sport Health Sci. 2022;11(1):58–66.
Pietrosimone BG, Gribble PA. Chronic ankle instability and corticomotor excitability of the fibularis longus muscle. J Athl Train. 2012;47(6):621–6.
Kosik KB, Terada M, Drinkard CP, McCann RS, Gribble PA. Potential corticomotor plasticity in those with and without chronic ankle instability. Med Sci Sports Exerc. 2017;49(1):141–9.
Nanbancha A, Tretriluxana J, Limroongreungrat W, Sinsurin K. Decreased supraspinal control and neuromuscular function controlling the ankle joint in athletes with chronic ankle instability. Eur J Appl Physiol. 2019;119(9):2041–52.
Needle AR. Brain regulation of muscle tone and laxity differs in functionally unstable ankles. J Sport Rehabil. 2013;22:202–11.
Thompson T, Suttmiller AMB, Ringle B, McCann RS. Corticomotor excitability of the gluteus maximus in individuals with chronic ankle instability: a pilot study. Transl Sports Med. 2020;4(1):65–71.
Needle AR, Swanik CB, Schubert M, Reinecke K, Farquhar WB, Higginson JS, et al. Decoupling of laxity and cortical activation in functionally unstable ankles during joint loading. Eur J Appl Physiol. 2014;114(10):2129–38.
Zhang X, Su W, Ruan B, Zang Y. Alterations in cortical activation among soccer athletes with chronic ankle instability during drop-jump landing: a preliminary study. Brain Sci. 2022;12(5):664.
Rosen AB, Yentes JM, McGrath ML, Maerlender AC, Myers SA, Mukherjee M. Alterations in cortical activation among individuals with chronic ankle instability during single-limb postural control. J Athl Train. 2019;54(6):718–26.
Terada M, Johnson N, Kosik K, Gribble P. Quantifying brain white matter microstructure of people with lateral ankle sprain. Med Sci Sports Exerc. 2019;51(4):640–61.
Xue X, Zhang Y, Li S, Xu H, Chen S, Hua Y. Lateral ankle instability-induced neuroplasticity in brain grey matter: a voxel-based morphometry MRI study. J Sci Med Sport. 2021. https://doi.org/10.1016/j.jsams.2021.06.013.
Xue X, Li Q, Wang Y, Lu R, Han J, Zhang H, et al. Impaired corticospinal tract in chronic ankle instability: a diffusion tensor imaging (DTI) and neurite orientation dispersion and density imaging (NODDI) study at 7.0 Tesla. J Sci Med Sport. 2022;25(8):649–54.
Xue X, Li S, Li H, Li Q, Hua Y. Deactivation of the dorsal anterior cingulate cortex indicated low postoperative sports levels in presurgical patients with chronic ankle instability. BMC Sports Sci Med Rehabil. 2021;13(1):121.
Xie HM, Xing ZT, Chen ZY, Zhang XT, Qiu XJ, Jia ZS, et al. Regional brain atrophy in patients with chronic ankle instability: a voxel-based morphometry study. Front Neurosci. 2022;16: 984841.
Xue X, Lu R, Zang DI, Li H, Zhang H, Xu H, et al. Low regional homogeneity of intrinsic cerebellar activity in ankle instability: an externally validated rs-fMRI study. Med Sci Sports Exerc. 2022;54(12):2037–44.
Shen Y, Wang W, Wang Y, Yang L, Yuan C, Yang Y, et al. Not only in sensorimotor network: local and distant cerebral inherent activity of chronic ankle instability: a resting-state fMRI study. Front Neurosci. 2022;16: 835538.
Needle AR, Palmer JA, Kesar TM, Binder-Macleod SA, Swanik CB. Brain regulation of muscle tone in healthy and functionally unstable ankles. J Sport Rehabil. 2013;22(3):202–11.
Zhang L, Zhao M, Fu W, Gao X, Shen J, Zhang Z, et al. Epidemiological analysis of trauma patients following the Lushan earthquake. PLoS One. 2014;9(5): e97416.
Hampson M, Peterson BS, Skudlarski P, Gatenby JC, Gore JC. Detection of functional connectivity using temporal correlations in MR images. Hum Brain Mapp. 2002;15(4):247–62.
Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage. 2002;15(1):273–89.
van Hedel HJ, Murer C, Dietz V, Curt A. The amplitude of lower leg motor evoked potentials is a reliable measure when controlled for torque and motor task. J Neurol. 2007;254(8):1089–98.
Luc BA, Lepley AS, Tevald MA, Gribble PA, White DB, Pietrosimone BG. Reliability of corticomotor excitability in leg and thigh musculature at 14 and 28 days. J Sport Rehabil. 2014;23(4):330–8.
Triggs WJ, Cros D, Macdonell RA, Chiappa KH, Fang J, Day BJ. Cortical and spinal motor excitability during the transcranial magnetic stimulation silent period in humans. Brain Res. 1993;628:39–48.
Fuhr P, Agostino R, Hallet M. Spinal motor neuron excitability during the silent period after cortical stimulation. Electroencephalogr Clin Neurophysiol. 1991;81(4):257–62.
Urbach D, Nebelung W, Weiler HT, Awiszus F. Bilateral deficit of voluntary quadriceps muscle activation after unilateral ACL tear. Med Sci Sports Exerc. 1999;31(12):1691.
Houston MN, Hoch JM, Hoch MC. College athletes with ankle sprain history exhibit greater fear-avoidance beliefs. J Sport Rehabil. 2018;27(5):419–23.
Houston MN, Van Lunen BL, Hoch MC. Health-related quality of life in individuals with chronic ankle instability. J Athl Train. 2014;49(6):758–63.
Song SK, Sun SW, Ramsbottom MJ, Chang C, Russell J, Cross AH. Dysmyelination revealed through MRI as increased radial (but unchanged axial) diffusion of water. Neuroimage. 2002;17(3):1429–36.
Nair G, Tanahashi Y, Low HP, Billings-Gagliardi S, Schwartz WJ, Duong TQ. Myelination and long diffusion times alter diffusion-tensor-imaging contrast in myelin-deficient shiverer mice. Neuroimage. 2005;28(1):165–74.
Kumar R, Macey PM, Woo MA, Alger JR, Harper RM. Diffusion tensor imaging demonstrates brainstem and cerebellar abnormalities in congenital central hypoventilation syndrome. Pediatr Res. 2008;64(3):275–80.
Ciccarelli O, Behrens TE, Altmann DR, Orrell RW, Howard RS, Johansen-Berg H, et al. Probabilistic diffusion tractography: a potential tool to assess the rate of disease progression in amyotrophic lateral sclerosis. Brain. 2006;129(Pt 7):1859–71.
Sun SW, Liang HF, Trinkaus K, Cross AH, Armstrong RC, Song SK. Noninvasive detection of cuprizone induced axonal damage and demyelination in the mouse corpus callosum. Magn Reson Med. 2006;55(2):302–10.
Hanaie R, Mohri I, Kagitani-Shimono K, Tachibana M, Azuma J, Matsuzaki J, et al. Altered microstructural connectivity of the superior cerebellar peduncle is related to motor dysfunction in children with autistic spectrum disorders. Cerebellum. 2013;12(5):645–56.
Song S-K, Sun S-W, Ju W-K, Lin S-J, Cross AH, Neufeld AH. Diffusion tensor imaging detects and differentiates axon and myelin degeneration in mouse optic nerve after retinal ischemia. Neuroimage. 2003;20(3):1714–22.
Budde MD, Kim JH, Liang HF, Schmidt RE, Russell JH, Cross AH, et al. Toward accurate diagnosis of white matter pathology using diffusion tensor imaging. Magn Reson Med. 2007;57(4):688–95.
Zhang H, Schneider T, Wheeler-Kingshott CA, Alexander DC. NODDI: practical in vivo neurite orientation dispersion and density imaging of the human brain. Neuroimage. 2012;61(4):1000–16.
Therrien AS, Bastian AJ. The cerebellum as a movement sensor. Neurosci Lett. 2019;1(688):37–40.
Weiller MJC. A review of differences between basal ganglia and cerebellar control of movements as revealed by functional imaging studies. Brain. 1998;121:1437–49.
Hertel J, Corbett RO. An updated model of chronic ankle instability. J Athl Train. 2019;54(6):572–88.
Delahunt E, Monaghan K, Caulfield B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. Am J Sports Med. 2006;34(12):1970–6.
Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Sweeney K, et al. Lower limb interjoint postural coordination one year after first-time lateral ankle sprain. Med Sci Sports Exerc. 2015;47(11):2398–405.
Terada M, Ball LM, Pietrosimone BG, Gribble PA. Altered visual focus on sensorimotor control in people with chronic ankle instability. J Sports Sci. 2016;34(2):171–80.
Terada M, Bowker S, Thomas AC, Pietrosimone B, Hiller CE, Rice MS, et al. Alterations in stride-to-stride variability during walking in individuals with chronic ankle instability. Hum Mov Sci. 2015;40:154–62.
Terada M, Pietrosimone BG, Gribble PA. Alterations in neuromuscular control at the knee in individuals with chronic ankle instability. J Athl Train. 2014;49(5):599–607.
Van Deun S, Staes FF, Stappaerts KH, Janssens L, Levin O, Peers KK. Relationship of chronic ankle instability to muscle activation patterns during the transition from double-leg to single-leg stance. Am J Sports Med. 2007;35(2):274–81.
Theisen A, Day J. Chronic ankle instability leads to lower extremity kinematic changes during landing tasks: a systematic review. Int J Exerc Sci. 2019;12(1):24–33.
Wikstrom EA, Bishop MD, Inamdar AD, Hass CJ. Gait termination control strategies are altered in chronic ankle instability subjects. Med Sci Sports Exerc. 2010;42(1):197–205.
Wikstrom EA, Brown CN. Minimum reporting standards for copers in chronic ankle instability research. Sports Med. 2014;44(2):251–68.
Draganova R, Konietschke F, Steiner KM, Elangovan N, Gumus M, Goricke SM, et al. Motor training-related brain reorganization in patients with cerebellar degeneration. Hum Brain Mapp. 2022;43(5):1611–29.
Machan T, Krupps K. The neuroplastic adaptation trident model: a suggested novel framework for ACL rehabilitation. Int J Sports Phys Ther. 2021;16(3):896–991.
Johnson BP, Cohen LG. Reward and plasticity: implications for neurorehabilitation. Handb Clin Neurol. 2022;184:331–40.
Czyz SH, Marusiak J, Klobusiakova P, Sajdlova Z, Rektorova I. Neuroplasticity in motor learning under variable and constant practice conditions: protocol of randomized controlled trial. Front Hum Neurosci. 2022;16: 773730.
Dordevic M, Taubert M, Muller P, Riemer M, Kaufmann J, Hokelmann A, et al. Which effects on neuroanatomy and path-integration survive? Results of a randomized controlled study on intensive balance training. Brain Sci. 2020;10(4):210. https://doi.org/10.3390/brainsci10040210.
Ardern CL, Osterberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48(22):1613–91.
Christino MA, Fantry AJ, Vopat BG. Psychological aspects of recovery following anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2015;23(8):501–9.
Bauer M, Feeley BT, Wawrzyniak JR, Pinkowsky G, Gallo RA. Factors affecting return to play after anterior cruciate ligament reconstruction: a review of the current literature. Phys Sportsmed. 2014;42(4):71–91.
Hsu CJ, Meierbachtol A, George SZ, Chmielewski TL. Fear of reinjury in athletes. Sports Health. 2017;9(2):162–7.
Picot B, Hardy A, Terrier R, Tassignon B, Lopes R, Fourchet F. Which functional tests and self-reported questionnaires can help clinicians make valid return to sport decisions in patients with chronic ankle instability? A narrative review and expert opinion. Front Sports Active Living. 2022;4: 902886.
Picot B, Remy-Neris O, Forestier N. Proprioceptive postural control strategies differ among non-injured athletes. Neurosci Lett. 2022;19:769. https://doi.org/10.1016/j.neulet.2021.136366.
Acknowledgements
We thank our colleagues from the Luxembourg Institute of Research in Orthopedics, Sports Medicine and Science (LIROMS) and the Strategic Research Program Exercise and the Brain in Health & Disease: The Added Value of Human-Centered Robotics (SRP17) who provided insight and expertise that assisted the research. Bart Roelands is a Collen-Francqui research professor.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of Interest
Alexandre Maricot, Emilie Dick, Annemiek Walravens, Bert Pluym, Elke Lathouwers, Kevin De Pauw, Jo Verschueren, Bart Roelands, Romain Meeusen and Bruno Tassignon have no conflicts of interest that are directly relevant to the content of this review.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Code Availability
Not applicable.
Author Contributions
AM substantially contributed to the conception and design of the work, as well as to the acquisition, analysis and interpretation of data for the work. BT, RM, JV, BR, KDP and EL substantially contributed to the conception and design of the work and the interpretation of data for the work. AW, ED and BP substantially contributed to the acquisition and analysis of data for the work. All authors revised the work critically for important intellectual content and gave final approval of the final version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maricot, A., Dick, E., Walravens, A. et al. Brain Neuroplasticity Related to Lateral Ankle Ligamentous Injuries: A Systematic Review. Sports Med 53, 1423–1443 (2023). https://doi.org/10.1007/s40279-023-01834-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-023-01834-z