Abstract
Background
Pharmaceuticals are usually granted a marketing authorisation on the basis of randomised controlled trials (RCTs). Occasionally the efficacy of a treatment is assessed without a randomised comparator group (either active or placebo).
Objective
To identify and develop a taxonomic account of economic modelling approaches for pharmaceuticals licensed without RCT data.
Methods
We searched PubMed, the websites of UK health technology assessment bodies and the International Society for Pharmacoeconomics and Outcomes Research Scientific Presentations Database for assessments of treatments granted a marketing authorisation by the US Food and Drug Administration or European Medicines Agency from January 1999 to May 2014 without RCT data (74 indications). The outcome of interest was the approach to modelling efficacy data.
Results
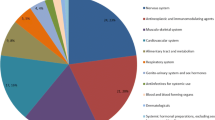
Fifty-one unique models were identified in 29 peer-reviewed articles, 30 health technology appraisals, and 15 International Society for Pharmacoeconomics and Outcomes Research abstracts concerning 30 indications (44 indications had not been modelled). We noted the high rate of non-submission to health technology assessment agencies (28/98). The majority of models (43/51) were based on ‘historical controls’—comparisons to previous meta-analysis or pooling of trials (5), individual trials (16), registries/case series (15), or expert opinion (7). Other approaches used the patient as their own control, performed threshold analysis, assumed time on treatment was added to overall survival, or performed cost-minimisation analysis.
Conclusions
There is considerable variation in the quality and approach of models constructed for drugs granted a marketing authorisation without a RCT. The most common approach is of a naive comparison to historical data (using other trials/registry data as a control group), which has considerable scope for bias.



Similar content being viewed by others
References
Hill SR, Mitchell AS, Henry DA. Problems with the interpretation of pharmacoeconomic analyses: a review of submissions to the Australian Pharmaceutical Benefits Scheme. JAMA. 2000;283:2116–21.
ICH Expert Working Group. ICH Harmonised Tripartite guideline E 10: choice of control group and related issues in clinical trials. In: International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use choice. 2000.
Buxton MJ, Drummond MF, Van Hout BA, et al. Modelling in economic evaluation: an unavoidable fact of life. Health Econ. 1997;6:217–27.
Sutton A, Ades AE, Cooper N, Abrams K. Use of indirect and mixed treatment comparisons for technology assessment. PharmacoEconomics. 2008;26:753–67.
Glasziou P, Chalmers I, Rawlins M, McCulloch P. When are randomised trials unnecessary? Picking signal from noise. BMJ. 2007;334:349–51.
Hatswell A, Baio G, Irs A, et al. The regulatory approval of pharmaceuticals without a randomised controlled study: analysis of EMA and FDA approvals 1999–2014. BMJ Open. Accepted for publication.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Pocock SJ. The combination of randomized and historical controls in clinical trials. J Chronic Dis. 1976;29:175–88.
Freemantle N, Marston L, Walters K, et al. Making inferences on treatment effects from real world data: propensity scores, confounding by indication, and other perils for the unwary in observational research. BMJ. 2013;347:f6409.
Signorovitch JE, Sikirica V, Erder MH, et al. Matching-adjusted indirect comparisons: a new tool for timely comparative effectiveness research. Value Health. 2012;15:940–7.
Annemans L, Van Cutsem E, Humblet Y, et al. Cost-effectiveness of cetuximab in combination with irinotecan compared with current care in metastatic colorectal cancer after failure on irinotecan: a Belgian analysis. Acta Clin Belg. 2007;62:419–25.
Sacks H, Chalmers TC, Smith H Jr. Randomized versus historical controls for clinical trials. Am J Med. 1982;72:233–40.
Diehl LF, Perry DJ. A comparison of randomized concurrent control groups with matched historical control groups: are historical controls valid? J Clin Oncol. 1986;4:1114–20.
MacLehose RR, Reeves BC, Harvey IM, et al. A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies. Health Technol Assess Winch Engl. 2000;4:1–154.
Moroz V, Wilson JS, Kearns P, Wheatley K. Comparison of anticipated and actual control group outcomes in randomised trials in paediatric oncology provides evidence that historically controlled studies are biased in favour of the novel treatment. Trials. 2014;15:481.
Ioannidis JP, Haidich AB, Pappa M, et al. Comparison of evidence of treatment effects in randomized and nonrandomized studies. JAMA. 2001;286:821–30.
Briggs AH, O’Brien BJ. The death of cost-minimization analysis? Health Econ. 2001;10:179–84.
Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408–12.
Hoyle M, Crathorne L, Garside R, Hyde C. Ofatumumab for the treatment of chronic lymphocytic leukaemia in patients who are refractory to fludarabine and alemtuzumab: a critique of the submission from GSK. Health Technol Assess Winch Engl. 2011;15(Suppl 1):61–7.
Tappenden P, Jones R, Paisley S, Carroll C. Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer. Health Technol Assess. 2007;11(12):1–128, iii–iv.
Wagstaff A, Culyer AJ. Four decades of health economics through a bibliometric lens. J Health Econ. 2012;31:406–39.
Woods B, Thompson J, Barcena L, et al. PSY5: comparing brentuximab vedotin overall survival data to standard of care in patients with relapsed/refractory Hodgkin lymphoma post-autologus stem cell transplant. Dublin: ISPOR Europe; 2013.
Faria R, Alava MH, Manca A, Wailoo AJ. NICE DSU technical support document 17: the use of observational data to inform estimates of treatment effectiveness in technology appraisal: methods for comparative individual patient data. 2015. http://www.nicedsu.org.uk/TSD17%20-%20DSU%20Observational%20data%20FINAL.pdf. Accessed 28 Jan 2016.
Weinstein MC, Siegel JE, Gold MR, et al. Recommendations of the panel on cost-effectiveness in health and medicine. J Am Med Assoc. 1996;276:1253–8.
Caro JJ, Briggs AH, Siebert U, Kuntz KM. Modeling good research practices: overview. A report of the ISPOR-SMDM Modeling Good Research Practices Task Force-1. Med Decis Making. 2012;32:667–77.
NICE. Guide to the methods of technology appraisal 2013. NICE; 2013. https://www.nice.org.uk/process/pmg9/resources/guide-to-the-methods-of-technologyappraisal-2013-pdf-2007975843781.
Scottish Medicines Consortium. Guidance to manufacturers for completion of New Product Assessment Form (NPAF). NHS Scotland; 2014. https://www.scottishmedicines.org.uk/files/submissionprocess/Guidance_on_NPAF_Final_October_2014.doc. Accessed 17 Oct 2016.
All Wales Medicines Strategy Group. Form B guidance notes. All Wales Medicines Strategy Group; 2013. http://www.awmsg.org/docs/awmsg/appraisaldocs/inforandforms/Form%20B%20guidance%20notes.pdf. Accessed 17 Oct 2016.
Australian Government Department of Health. Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee Version 4.4. Australian Government Department of Health; 2013. http://www.pbac.pbs.gov.au/content/information/printable-files/pbacg-book.pdf. Accessed 5 March 2015.
Pharmaceutical Management Agency. Prescription for pharmacoeconomic analysis: methods for cost-utility analysis version 2.1. New Zealand Government; 2012. https://www.pharmac.health.nz/assets/pfpa-final.pdf. Accessed 17 Oct 2016.
New Zealand Government. Guidelines for funding applications to PHARMAC. New Zealand Government; 2015. http://www.pharmac.govt.nz/2010/02/11/Guidelines%20for%20Suppliers%20Submissions.pdf. Accessed 17 Oct 2016.
Canadian Agency for Drugs and Technologies in Health. Guidelines for the economic evaluation of health technologies: Canada, 3rd edn. Canadian Agency for Drugs and Technologies in Health; 2006. http://www.cadth.ca/media/pdf/186_EconomicGuidelines_e.pdf. Accessed 17 Oct 2016.
Canadian Agency for Drugs and Technologies in Health. Addendum to CADTH’s guidelines for the economic evaluation of health technologies: specific guidance for oncology products. Canadian Agency for Drugs and Technologies in Health; 2009. http://www.cadth.ca/media/pdf/H0405_Guidance_for_Oncology_Prodcuts_gr_e.pdf. http://www.cadth.ca/media/pdf/186_EconomicGuidelines_e.pdf. Accessed 17 Oct 2016.
Scott WG, Scott HM. Economic evaluation of third-line treatment with alemtuzumab for chronic lymphocytic leukaemia. Clin Drug Investig. 2007;27:755–64.
Castro-Jaramillo HE. The cost-effectiveness of enzyme replacement therapy (ERT) for the infantile form of Pompe disease: comparing a high-income country’s approach (England) to that of a middle-income one (Colombia). Rev Salud Pública. 2012;14:143–55.
Scottish Medicines Consortium. Alglucosidase alfa 50mg powder for concentrate for solution for infusion (Myozyme) No. (352/07). Scottish Medicines Consortium; 2007. https://www.scottishmedicines.org.uk/files/alglucosidase_alfa_50mg_powder_Myozyme__352-07_.pdf. Accessed 17 Oct 2016.
Kanters TA, Hoogenboom-Plug I, Rutten-Van Mölken MP, et al. Cost-effectiveness of enzyme replacement therapy with alglucosidase alfa in classic-infantile patients with Pompe disease. Orphanet J Rare Dis. 2014;9:75.
Bennett CL, Weinberg PO, Golub RM. Cost-effectiveness model of a phase II clinical trial of a new pharmaceutical for essential thrombocythemia: is it helpful to policy makers? Semin Hematol. 1999;36:26–9.
Golub R, Adams J, Dave S, Bennett CL. Cost-effectiveness consideration in the treatment of essential thrombocytopenia. Semin Oncol. 2002;29:28–32.
Scottish Medicines Consortium. Re-submission: anagrelide 0.5 mg capsule (Xagrid). Scottish Medicines Consortium; 2005.
Goldberg Arnold R, Kim R, Tang B. The cost-effectiveness of argatroban treatment in heparin-induced thrombocytopenia: the effect of early versus delayed treatment. Cardiol Rev. 2006;14:7–13.
Patrick AR, Winkelmayer WC, Avorn J, Fischer MA. Strategies for the management of suspected heparin-induced thrombocytopenia: a cost-effectiveness analysis. PharmacoEconomics. 2007;25:949–61.
AWMSG. AWMSG Secretariat Assessment Report: Advice No. 4312 Argatroban (Exembol®). All Wales Medicines Strategy Group; 2012. http://www.awmsg.org/awmsgonline/grabber;jsessionid=1f631736a0503b59c6ed8236c4b8?resId=308. Accessed 17 Oct 2016.
Scottish Medicines Consortium. Argatroban, 100 mg/ml, concentrate for solution for infusion (Exembol) SMC No. (812/12). Scottish Medicines Consortium; 2012. https://www.scottishmedicines.org.uk/files/advice/argatroban_Exembol_FINAL_October_2012_for_website.pdf. Accessed 17 Oct 2016.
Peters B, Goeckner B, Ponzillo J, et al. Pegaspargase versus asparaginase in adult ALL: a pharmacoeconomic assessment. Formulary. 1995;30:388–93.
Scottish Medicines Consortium. Resubmission: betaine anhydrous oral powder (Cystadane) No. (407/07). Scottish Medicines Consortium; 2010. https://www.scottishmedicines.org.uk/files/betaine_anhydrous_Cystadane_2nd_RESUBMISSION_FINAL_July_2010.pdf. Accessed 17 Oct 2016.
Yoong K, Attard C, Sehn L. Cost-effectiveness analysis of bortezomib in relapsed mantle cell lymphoma patients in Canada. Paris: ISPOR Europe; 2009.
Mehta J, Duff SB, Gupta S. Cost effectiveness of bortezomib in the treatment of advanced multiple myeloma. Manag Care Interface. 2004;17:52–61.
Pennington B, Hatswell A, Clifton-Brown E. CL1: a comparison of methodologies for estimating survival in patients treated with second-generation tyrosine-kinase inhibitors for chronic myeloid leukaemia. Dublin: 2013.
Scottish Medicines Consortium. Bosutinib 100 mg, 500 mg film-coated tablets (Bosulif®) SMC No. (910/13). Scottish Medicines Consortium; 2013. https://www.scottishmedicines.org.uk/files/advice/bosutinib_Bosulif_FINAL_October_2013_for_website_Amended_31.03.14.pdf. Accessed 17 Oct 2016.
NICE. NICE technology appraisal guidance 299: bosutinib for previously treated chronic myeloid leukaemia. NICE; 2013. http://www.nice.org.uk/nicemedia/live/14310/65847/65847.pdf. Accessed 17 Oct 2016.
Hoyle M, Snowsill T, Haasova M, et al. Bosutinib for previously treated chronic myeloid laukaemia: a single technology appraisal. Exeter: University of Exeter Medical School; 2013.
Telléz Girón G, Salgado J, Soto H. PCN71: cost effectiveness analysis of busulfan + cyclophosphomide (BUCY2) as conditioning regimen before allogeneic human steam cell transplantation (HSCT): comparison of oral versus IV busulfan. Washington, DC: ISPOR International; 2012.
Scottish Medicines Consortium. Carglumic acid 200 mg dispersible tablets (Carbaglu®) SMC No. (899/13). Scottish Medicines Consortium; 2013. https://www.scottishmedicines.org.uk/files/advice/carglumic_acid_Carbaglu_FINAL_September_2013_website.pdf. Accessed 17 Oct 2016.
Starling N, Tilden D, White J, Cunningham D. Cost-effectiveness analysis of cetuximab/irinotecan vs active/best supportive care for the treatment of metastatic colorectal cancer patients who have failed previous chemotherapy treatment. Br J Cancer. 2007;96:206–12.
Merck Pharmaceuticals. Cetuximab (Erbitux) 100 mg solution for infusion (2 mg/mL): submission to the National Institute for Health and Clinical Excellence. National Institute for Health and Clinical Excellence; 2005. https://www.nice.org.uk/guidance/TA118/documents/merck2. Accessed 17 Oct 2016.
Tappenden P, Jones R, Paisley S, Carroll C. The use of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer. School of Health and Related Research (ScHARR), The University of Sheffield; 2006. https://www.nice.org.uk/guidance/TA118/documents/colorectal-cancer-metastatic-bevacizumab-cetuximab-assessment-report2. Accessed 17 Oct 2016.
Guest JF, Smith H, Sladkevicius E, Jackson G. Cost-effectiveness of pentostatin compared with cladribine in the management of hairy cell leukemia in the United Kingdom. Clin Ther. 2009;31:2398–415.
AWMSG. Final appraisal report: clofarabine (Evoltra®). All Wales Medicines Strategy Group; 2007. http://www.awmsg.org/awmsgonline/grabber?resId=520. Accessed 17 Oct 2016.
Scottish Medicines Consortium. Clofarabine, 1mg/ml concentrate for solution for infusion (Evoltra®) (No. 327/06). Scottish Medicines Consortium; 2006. https://www.scottishmedicines.org.uk/files/clofarabine_1mgml_concentrate_solution_infusion_Evoltra.pdf. Accessed 17 Oct 2016.
AWMSG. Final appraisal report: dasatinib (Sprycel®) for chronic, accelerated or blast phase CML. All Wales Medicines Strategy Group; 2007. http://www.awmsg.org/awmsgonline/grabber?resId=251. Accessed 17 Oct 2016.
Thompson Coon J, Hoyle M, Pitt M, et al. Dasatinib and nilotinib for imatinib-resistant or -intolerant chronic myeloid leukaemia: a systematic review and economic evaluation. Peninsula Technology Assessment Group (PenTAG), Peninsula Medical School, Peninsula College of Medicine and Dentistry; 2009. http://www.nice.org.uk/guidance/ta241/documents/assessment-report2. Accessed 17 Oct 2016.
Scottish Medicines Consortium. Dasatinib, 20 mg, 50 mg, 70 mg tablets (Sprycel) No. (370/07). Scottish Medicines Consortium; 2007. https://www.scottishmedicines.org.uk/files/dasatanib__Sprycel__CML_FINAL_April_2007__amended_010507__for_website.pdf. Accessed 17 Oct 2016.
AWMSG. Final appraisal report: dasatinib (Sprycel®) for lymphoid blast CML and PH + ALL. All Wales Medicines Strategy Group; 2007. http://www.awmsg.org/awmsgonline/grabber?resId=250. Accessed 17 Oct 2016.
Scottish Medicines Consortium. Defibrotide, 80 mg/mL, concentrate for solution for infusion (Defitelio®) SMC No. (967/14). Scottish Medicines Consortium; 2014. https://www.scottishmedicines.org.uk/files/advice/M__Scottish_Medicine_Consortium_Web_Data_Audit_advice_Advice_by_Year_2014_No.6_-_June_2014_defibrotide__Defitelio__FINAL_May_2014_for_website.pdf. Accessed 17 Oct 2016.
Ratcliffe A, Beard S, Wolowacz S. A pharmacoeconomic model of the cost-effectiveness of gefitinib (‘Iressa’) compared with best supportive care (BSC) in third-line treatment of patients with refractory advanced non-small-cell lung cancer (NSCLC) in the UK. Hamburg: ISPOR Europe; 2004.
Lang K, Menzin J, Earle CC, Mallick R. Outcomes in patients treated with gemtuzumab ozogamicin for relapsed acute myelogenous leukemia. Am J Health Syst Pharm. 2002;59:941–8.
Garside R, Round A, Dalziel K, et al. The effectiveness and cost-effectiveness of imatinib (STI 571) in chronic myeloid leukaemia. Exeter: University of Exeter; 2002.
Warren E, Ward S, Gordois A, Scuffham P. Cost-utility analysis of imatinib mesylate for the treatment of chronic myelogenous leukemia in the chronic phase. Clin Ther. 2004;26:1924–33.
NICE. Guidance on the use of imatinib for chronic myeloid leukemia. London: National Institute for Clinical Excellence; 2003. http://www.nice.org.uk/nicemedia/live/11516/32754/32754.pdf. Accessed 13 Feb 2014.
Gordois A, Scuffham P, Warren E, Ward S. Cost-utility analysis of imatinib mesilate for the treatment of advanced stage chronic myeloid leukaemia. Br J Cancer. 2003;89:634–40.
Wilson J, Connock M, Song F, et al. Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation. Health Technol Assess. 2005;9(25):1–142.
Huse DM, von Mehren M, Lenhart G, et al. Cost effectiveness of imatinib mesylate in the treatment of advanced gastrointestinal stromal tumours. Clin Drug Investig. 2007;27:85–93.
Wilson J, Connock M, Song F, et al. Imatinib for the treatment of patients with unresectable and/or metastatic gastro-intestinal stromal tumours: a systematic review and economic evaluation. National Institute for Clinical Excellence; 2003. https://www.nice.org.uk/guidance/TA86/documents/gastrointestinal-stromal-tumours-imatinib-assessment-report-2. Accessed 17 Oct 2016.
De Abreu Lourenco R, Wonder M. The cost-effectiveness of imatinib for the treatment of patients with gastroinstestinal stromal tumours. Kobe: ISPOR Asia; 2003.
AWMSG. Final appraisal report: nelarabine for the treatment of T-cell acute lymphoblastic leukaemia and T-cell lymphoblastic lymphoma. All Wales Medicines Strategy Group; 2009. http://www.awmsg.org/awmsgonline/grabber?resId=365. Accessed 17 Oct 2016.
Scottish Medicines Consortium. Nelarabine, 5 mg/ml solution for infusion (Atriance) No. (454/08). Scottish Medicines Consortium; 2008. https://www.scottishmedicines.org.uk/files/nelarabine__Atriance__FINAL_March_2008.doc_for_website.pdf. Accessed 17 Oct 2016.
Scottish Medicines Consortium. Nilotinib, 200 mg capsules (Tasigna) (440/08). Scottish Medicines Consortium; 2008. https://www.scottishmedicines.org.uk/files/nilotinib_200mg_capsules_Tasigna_FINAL_Feb_2008_amended_May_2008_for_Website.pdf. Accessed 17 Oct 2016.
Taylor M, Lewis L, Lebmeier M, Wang Q. An economic evaluation of dasatinib for the treatment of imatinib-resistant patients with chronic-phase chronic myelogenous leukaemia. Baltimore: ISPOR International; 2011.
Loveman E, Cooper K, Bryant J, et al. Dasatinib, high-dose imatinib and nilotinib for the treatment of imatinib-resistant chronic myeloid leukaemia: a systematic review and economic evaluation. Health Technol Assess. 2011;16(23):iii–xiii, 1–137.
Scottish Medicines Consortium. Ofatumumab, 100 mg concentrate for solution for infusion (Arzerra) No. (626/10). Scottish Medicines Consortium; 2010. https://www.scottishmedicines.org.uk/files/ofatumumab_Arzerra_FINAL_July_2010.pdf. Accessed 17 Oct 2016.
Almond C, Stevens J, Ren K, Batty A. The estimated survival of patient with double refractory chronic lymphocytic leukaemia: a reanalysis of NICE TA202 using Bayesian methodology to model observed data. Dublin: ISPOR Europe; 2013.
Batty A, Thompson G, Maroudas P, Delea T. Estimating cost-effectiveness based on the results of uncontrolled clinical trials: ofatumumab for the treatment of fludarabine- and alemtuzumab-refractory chronic lymphocytic leukaemia. Prague: ISPOR Europe; 2010.
Hoyle M, Crathorne L, Moxham T, et al. Ofatumumab (Arzerra®) for the treatment of chronic lymphocytic leukaemia in patients who are refractory to fludarabine and alemtuzumab: a critique of the submission from GSK. Exeter: University of Exeter; 2010.
Van Nooten F, Dewilde S, Van Belle S, Marbaix S. Cost-effectiveness of sunitinib as second line treatment in patients with metastatic renal cancer in belgium. Dublin: ISPOR Europe; 2007.
Aiello EC, Muszbek N, Richardet E, et al. Cost-effectiveness of new targeted therapy sunitinib malate as second line treatment in metastatic renal cell carcinoma in Argentina. Arlington: ISPOR International; 2007.
Paz-Ares L, del Muro JG, Grande E, Díaz S. A cost-effectiveness analysis of sunitinib in patients with metastatic renal cell carcinoma intolerant to or experiencing disease progression on immunotherapy: perspective of the Spanish National Health System. J Clin Pharm Ther. 2010;35(4):429–38.
Scottish Medicines Consortium. Sunitinib 50mg capsules (Sutent) No. (343/07). Scottish Medicines Consortium; 2007. https://www.scottishmedicines.org.uk/files/sunitinib_Sutent_MRCC_343_07.pdf. Accessed 17 Oct 2016.
Smith WD, Arbuckle R. Pharmacoeconomic analysis of sorafenib and sunitinib for first-line treatment of advanced renal cell carcinoma (ARCC) at a comprehensive cancer center. Arlington: ISPOR International; 2007.
Purmonen T, Martikainen JA, Soini EJO, et al. Sunitinib malate provides additional survival and value for money as second line treatment for metastatic renal cell carcinoma (MRCC): an economic evaluation using bayesian approach. Dublin: ISPOR Europe; 2007.
Purmonen T, Martikainen JA, Soini EJO, et al. Economic evaluation of sunitinib malate in second-line treatment of metastatic renal cell carcinoma in Finland. Clin Ther. 2008;30:382–92.
Hopper C, Niziol C, Sidhu M. The cost-effectiveness of Foscan mediated photodynamic therapy (Foscan-PDT) compared with extensive palliative surgery and palliative chemotherapy for patients with advanced head and neck cancer in the UK. Oral Oncol. 2004;40:372–82.
Kübler A, Niziol C, Sidhu M, et al. Eine Kosten-Effektivitäts-Analyse der photodynamischen Therapie mit Foscan® (Foscan®-PDT) im Vergleich zu einer palliativen Chemotherapie bei Patienten mit fortgeschrittenen Kopf-Halstumoren in Deutschland. Laryngo Rhino Otol. 2005;84:725–32.
Dinnes J, Cave C, Huang S, et al. The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma. National Institute for Health and Clinical Excellence; 2000. https://www.nice.org.uk/guidance/ta23/documents/ta23-brain-cancer-temozolomide-hta-report2. Accessed 17 Oct 2016.
Scottish Medicines Consortium. Tocofersolan, 50 mg/mL (corresponding to 74.5 IU tocopherol) oral solution (Vedrop®) SMC No. (696/11). Scottish Medicines Consortium; 2012. https://www.scottishmedicines.org.uk/files/advice/tocofersolan_Vedrop.pdf. Accessed 17 Oct 2016.
Soini EJO, Garcia San Andres B, Joensuu T. Trabectedin in the treatment of metastatic soft tissue sarcoma: cost-effectiveness, cost-utility and value of information. Ann Oncol. 2011;22:215–23.
Soini E, García San Andrés B, Joensuu T. Economic evaluation of trabectedin in the treatment of metastatic soft-tissue sarcoma (mSTS) in the Finnish setting. Paris: ISPOR Europe; 2009.
Scottish Medicines Consortium. Trabectedin 0.25 mg, 1 mg power for concentrate for solution for infusion (Yondelis) No. (452/08). Scottish Medicines Consortium; 2008. https://www.scottishmedicines.org.uk/files/trabectedin__Yondelis__FINAL_July_2008.doc_for_website.pdf. Accessed 17 Oct 2016.
AWMSG. Final appraisal report: trabectedin (Yondelis) for advanced soft tissue sarcoma. All Wales Medicines Strategy Group; 2008. http://www.awmsg.org/awmsgonline/grabber;jsessionid=2064f61ddd25570cee81d9956c22?resId=394. Accessed 17 Oct 2016.
Scottish Medicines Consortium. Trabectedin, 0.25 and 1 mg powder for concentrate for solution for infusion (Yondelis). Scottish Medicines Consortium; 2010. https://www.scottishmedicines.org.uk/files/advice/trabectedin_Yondelis_RESUBMISSION_FINAL_October_2010.doc_for_website.pdf. Accessed 17 Oct 2016.
Scottish Medicines Consortium. 2nd re-submission in confidence—trabectedin, 0.25 and 1 mg powder for concentrate for solution for infusion (Yondelis). Scottish Medicines Consortium; 2011. https://www.scottishmedicines.org.uk/files/advice/trabectedin_Yondelis_2ND_RESUBMISSION_FINAL_JUNE_2011_for_website.pdf. Accessed 17 Oct 2016.
Simpson E, Rafia R, Stevenson M. Trabectedin for the treatment of advanced metastatic soft tissue sarcoma. National Institute for Health and Clinical Excellence; 2009. https://www.nice.org.uk/guidance/TA185/documents/evidence-review-group-report2. Accessed 17 Oct 2016.
Simpson E, Rafia R, Stevenson M, Papaioannou D. Trabectedin for the treatment of advanced metastatic soft tissue sarcoma. Health Technol Assess. 2010;14(Suppl 1):63–7.
Rafia R, Simpson E, Stevenson M, Papaioannou D. Trabectedin for the treatment of advanced metastatic soft tissue sarcoma: a NICE single technology appraisal. PharmacoEconomics. 2013;31:471–8.
Amdahl J, Manson SC, Isbell R, et al. Cost-effectiveness of pazopanib in advanced soft tissue sarcoma in the United Kingdom. Sarcoma. 2014;2014:1–14.
Villa G, Hernández-Pastor LJ, Guix M, et al. Cost-effectiveness analysis of pazopanib in second-line treatment of advanced soft tissue sarcoma in Spain. Clin Transl Oncol. 2015;17(1):24–33.
Author contributions
The study was designed by AJH, GB and NF, the literature searches were conducted by AJH, and interpretation was provided by AJH, GB and NF. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was receiving for the preparation of this article.
Conflict of interest
AJH, GB and NF have no conflicts of interest directly relevant to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hatswell, A.J., Freemantle, N. & Baio, G. Economic Evaluations of Pharmaceuticals Granted a Marketing Authorisation Without the Results of Randomised Trials: A Systematic Review and Taxonomy. PharmacoEconomics 35, 163–176 (2017). https://doi.org/10.1007/s40273-016-0460-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-016-0460-6