Abstract
Introduction
Understanding how patients value different characteristics of an intervention and make trade-offs in a therapy choice context with potential benefit and possible harm may result in decisions for which a better reflected value is delivered. This systematic review summarizes patient preferences for breast cancer treatments elicited by discrete choice experiments (DCE).
Methodology
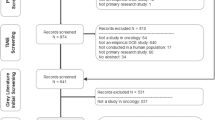
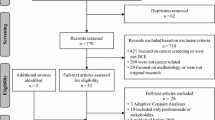
The electronic databases MEDLINE (PubMed), Scopus, PsycINFO, CINAHL, LILACS, and Web of Science were last searched on May 9, 2019 without restrictions regarding language and time of publication. Original studies reporting patient preferences related to breast cancer treatment (surgery, radiotherapy, endocrine therapy, chemotherapy or palliative care) elicited by DCE were eligible. A narrative synthesis of the relative importance and trade-offs of the treatment attributes of each study was reported.
Results
Five studies conducted in Japan, Thailand, USA and the Netherlands with 146–298 participants evaluated preferences regarding chemotherapy regimens for advanced/metastatic disease, and breast reconstruction after mastectomy. The attributes with major relative effects on preferences were greater survival, better aesthetic result of the surgery, and lower side effects and complication rates. Patients would trade a better aesthetic result to minimize complication rates, and, in advanced disease, the willingness to pay was greater for gains in survival and to avoid some severe adverse events.
Conclusion
Despite the relative lack of evidence in this specific context, our review shows that breast cancer patients naturally value greater benefit and, in scenarios of advanced and metastatic disease, are willing to face risks of some side effects for gains in survival.

Similar content being viewed by others
Data availability
Data are available on request to the authors.
References
Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. Br Med J. 2000;320:1530–3.
Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14:403–13.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform health care decision making: a user guide. Pharmacoeconomics. 2008;26:661–77.
Politi MC, Studts JL, Hayslip JW. Shared decision making in oncology practice: what do oncologists need to know? Oncologist. 2012;17:91–100.
Kane HL, Halpern MT, Squiers LB, Treiman KA, McCormack LA. Implementing and evaluating shared decision making in oncology practice. CA Cancer J Clin. 2014;64:377–88.
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013.
Harrison M, Milbers K, Hudson M, Bansback N. Do patients and health care providers have discordant preferences about which aspects of treatments matter most? Evidence from a systematic review of discrete choice experiments. BMJ Open. 2017;7:e014719.
Fraenkel L. Incorporating patients’ preferences into medical decision making. Med Care Res Rev. 2013;70:80S–93S.
Swift JK, Callahan JL. The impact of client treatment preferences on outcome: a meta-analysis. J Clin Psychol. 2009;65:368–81.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Omori Y, Enatsu S, Cai Z, Ishiguro H. Patients’ preferences for postmenopausal hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer treatments in Japan. Breast Cancer. 2019. https://doi.org/10.1007/s12282-019-00965-4.
Ngorsuraches S, Thongkeaw K. Patients’ preferences and willingness-to-pay for postmenopausal hormone receptor-positive, HER2-negative advanced breast cancer treatments after failure of standard treatments. Springer Plus. 2015;4:1–11.
DiBonaventura MC, Copher R, Basurto E, Faria C, Lorenzo R. Patient preferences and treatment adherence among women diagnosed with metastatic breast cancer. Am Health Drug Benefits. 2014;7:386–96.
Lalla D, Carlton R, Santos E, Bramley T, D’Souza A. Willingness to pay to avoid metastatic breast cancer treatment side-effects: results from a conjoint analysis. Springerplus. 2014;3:350.
Damen THC, de Bekker-Grob EW, Mureau MAM, Menke-Pluijmers MB, Seynaeve C, Hofer SOP, et al. Patients’ preferences for breast reconstruction: a discrete choice experiment. J Plast Reconstr Aesthet Surg. 2011;64:75–83.
Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2005.
Nord E, Daniels N, Kamlet M. QALYs: some challenges. Value Health. 2009;12:S10–5.
Zhang Y, Alonso-Coello P, Guyatt GH, Yepes-Nuñez JJ, Akl EA, Hazlewood G, GRADE Guidelines: 19, et al. Assessing the certainty of evidence in the importance of outcomes or values and preferences-risk of bias and indirectness. J Clin Epidemiol. 2018;111:83.
Louviere JJ, Hensher DA, Swait JD. Stated choice methods: analysis and applications. Cambridge: Cambridge University Press; 2000.
Marshall D, Bridges JF, Hauber B, Cameron R, Donnalley L, Fyie K, et al. Conjoint analysis applications in health—how are studies being designed and reported: an update on current practice in the published literature between 2005 and 2008. Patient. 2010;3:249–56.
Soekhai V, de Bekker-Grob EW, Ellis AR, Vass CM. Discrete choice experiments in health economics: past, present and future. Pharmacoeconomics. 2019;37(2):201–26.
de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21:145–72.
Joy SM, Little E, Maruthur NM, Purnell TS, Bridges JF. Patient preferences for the treatment of type 2 diabetes: a scoping review. Pharmacoeconomics. 2013;31:877–92.
Bien DR, Danner M, Vennedey V, Civello D, Evers SM, Hiligsmann M. Patients’ preferences for outcome, process and cost attributes in cancer treatment: a systematic review of discrete choice experiments. Patient. 2017;10:553–65.
Spaich S, Kinder J, Hetjens S, Fuxius S, Gerhardt A, Sütterlin M. Patient preferences regarding chemotherapy in metastatic breast cancer—a conjoint analysis for common taxanes. Front Oncol. 2018;8:535.
Storm-Dickerson T, Das L, Gabriel A, Gitlin M, Farias J, Macarios D. What drives patient choice: preferences for approaches to surgical treatments for breast cancer beyond traditional clinical benchmarks. Plast Reconstr Surg Glob Open. 2018;6(4):e1746.
Ballinger TJ, Kassem N, Shen F, Jiang G, Smith ML, Railey E, Howell J, White CB, Schneider BP. Discerning the clinical relevance of biomarkers in early stage breast cancer. Breast Cancer Res Treat. 2017;164(1):89–97.
Smith ML, White CB, Railey E, Sledge GW Jr. Examining and predicting drug preferences of patients with metastatic breast cancer: using conjoint analysis to examine attributes of paclitaxel and capecitabine. Breast Cancer Res Treat. 2014;145:83–9.
Beusterien K, Grinspan J, Kuchuk I, Mazzarello S, Dent S, Gertler S, Bouganim N, Vandermeer L, Clemons M. Use of conjoint analysis to assess breast cancer patient preferences for chemotherapy side effects. Oncologist. 2014;19(2):127–34.
Beusterien K, Grinspan J, Tencer T, Brufsky A, Visovsky C. Patient preferences for chemotherapies used in breast cancer. Int J Womens Health. 2012;4:279–87.
Wouters H, Maatman GA, Van Dijk L, Bouvy ML, Vree R, Van Geffen EC, Nortier JW, Stiggelbout AM. Trade-off preferences regarding adjuvant endocrine therapy among women with estrogen receptor-positive breast cancer. Ann Oncol. 2013;24(9):2324–9.
Author information
Authors and Affiliations
Contributions
RLG contributed to the conception and design of the work, data collection, data analysis and interpretation, and drafted the article; LC and RCRA contributed to data collection, data analysis and interpretation, and manuscript writing; CBTF contributed to data collection and critical revision of the manuscript; FMC, RRAF and LMA contributed to the conception and design of the work and critical revision of the manuscript. All authors approved the final version of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors Renata Leborato Guerra, Luciana Castaneda, Rita de Cássia Ribeiro de Albuquerque, Camila Belo Tavares Ferreira, Flávia de Miranda Corrêa, Ricardo Ribeiro Alves Fernandes and Liz Maria de Almeida declare that they have no conflict of interest.
Funding
This study was supported by the 54° technical cooperation term between the Brazilian National Institute of Cancer/Ministry of Health and the Pan-American Health Organization/World Health Organization.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Guerra, R.L., Castaneda, L., de Albuquerque, R.d.C.R. et al. Patient Preferences for Breast Cancer Treatment Interventions: A Systematic Review of Discrete Choice Experiments. Patient 12, 559–569 (2019). https://doi.org/10.1007/s40271-019-00375-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-019-00375-w