Abstract
Purpose
Acid-suppressive drugs (ASDs) are often prescribed for patients with nonvalvular atrial fibrillation (NVAF) taking oral anticoagulants (OACs). However, the risk-benefit balance of ASDs prescription for patients with NVAF taking OACs is still unclear. This study aimed to assess the association between ASDs and clinical outcomes in patients taking OACs for NVAF.
Methods
This study is a subanalysis of an historical registry study from 71 centers in Japan. We included patients taking vitamin K antagonists for NVAF and excluded those with mechanical heart valves or a history of pulmonary thrombosis or deep vein thrombosis. We registered consecutive patients in February 2013 and followed them up until February 2017. The primary outcomes were ischemic events, major bleedings, and all-cause mortality. Ischemic stroke, acute myocardial infarction, and hemorrhagic stroke comprised the secondary outcomes.
Results
We included 7826 patients with a mean age of 73 years, 5274 (67%) of whom were males. The adjusted hazard ratios (95% confidence intervals) for ischemic events, major bleedings, and all-cause mortality in the ASD group compared with the no-ASD group were 0.998 (0.78–1.27), 0.98 (0.81–1.18), and 1.22 (1.02–1.47), respectively, while those for ischemic stroke, acute myocardial infarction, and hemorrhagic stroke were 0.96 (0.74–1.24), 0.82 (0.36–1.88), and 1.17 (0.69–1.99), respectively.
Conclusions
ASDs were significantly associated with all-cause mortality in patients with NVAF taking OACs.
Similar content being viewed by others
Acid-suppressive drugs (ASDs), including proton pump inhibitors and histamine-2 receptor antagonists, are often prescribed for patients with nonvalvular atrial fibrillation (NVAF) taking oral anticoagulants (OACs). |
However, ASDs have various adverse effects, including an increased risk for all-cause mortality and cardiovascular mortality. |
The use of ASDs for patients with NVAF taking OACs and the risk–benefit balance are still unclear and controversial. |
This registry enrolling 7826 consecutive patients with NVAF taking OACs showed a significant association between ASDs and all-cause mortality. |
Physicians need to carefully consider the benefits and risks of ASDs and prescribe ASDs to patients with NVAF having distinct indications for ASDs. |
1 Introduction
Acid-suppressive drugs (ASDs), including proton pump inhibitors (PPIs) and histamine-2 receptor antagonists (H2RAs), are among the most commonly prescribed drugs worldwide, mainly for treating and preventing gastrointestinal symptoms [1]. In particular, PPIs are often prescribed for patients with nonvalvular atrial fibrillation (NVAF) who are taking oral anticoagulants (OACs), which precipitate bleeding events [2, 3]. Concomitant use of PPIs for such patients reportedly reduces the risk of gastrointestinal bleeding [2,3,4,5,6,7]. However, ASDs have various adverse effects [1,2,3, 8,9,10,11,12,13]. For instance, PPIs show an increased risk for all-cause mortality and cardiovascular mortality [1, 8,9,10,11,12,13]. H2RAs also cause cytopenias, nephrotoxicity, and hepatotoxicity, although these adverse events are less severe than PPIs [1]. Furthermore, ASDs cause poor control of vitamin K antagonists (VKAs) owing to their interaction with VKAs [14]. However, the use of ASDs for patients with NVAF taking OACs and the risk–benefit balance remain unclear and considerably controversial [2].
We therefore implemented a subanalysis of patients with NVAF taking OACs in a large registry study. This study aimed to investigate the association between ASDs and clinical outcomes in patients with NVAF prescribed OACs.
2 Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request.
This study was a subanalysis of an historical registry study from 71 centers in Japan [15, 16]. We included patients with NVAF, taking VKAs, on 2 February 2013 and excluded those with mechanical heart valves or a history of pulmonary thrombosis or deep vein thrombosis. We followed up the participants until 25 February 2017. Those with a history of stroke or major bleeding were included. The Institutional Review Boards of all 71 participating centers approved the study protocol (electronic supplementary Table 1), which conforms to the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan [15,16,17]. Written informed consent was replaced with the opt-out method in line with the guidelines.
2.1 Data Collection and Definitions
Clinical research coordinators reviewed the hospital charts to collect clinical information [15, 16]. We collected follow-up information such as patient characteristics, laboratory data, medication use, risk for ischemic stroke (CHADS2 score), and risk for hemorrhagic stroke (HAS-BLED score) at 1, 2, 3, and 4 years for the same procedure. The CHADS2 score, which includes chronic heart failure, hypertension history, age ≥ 75 years, diabetes mellitus (DM), and prior cerebral ischemia, was developed to assess the stroke risk in patients with NVAF [18]. The HAS-BLED score, which consists of hypertension, abnormal renal or liver function, stroke, bleeding history or predisposition, labile international normalized ratio of prothrombin time (PT-INR), age > 65 years, and concomitant use of drugs and alcohol, was developed to predict major bleeding events in anticoagulation for patients with NVAF [19]. The participants were divided into two groups: ASDs group and no-ASDs group. Those who received ASDs at baseline comprised the ASDs group, while all others belonged to the no-ASDs group. Because we did not assess the use of ASDs after the inclusion of patients, we assumed that those in the ASD group continued to use ASDs during the follow-up and vice versa.
2.2 Outcomes
The primary outcomes consist of ischemic events, major bleedings, and all-cause mortality. In this study, ischemic events included ischemic stroke and systemic embolism [20], and major bleedings were defined according to the International Society on Thrombosis and Hemostasis criteria [21]. The secondary outcomes were ischemic stroke (transient ischemic attack), acute myocardial infarction (AMI), and hemorrhagic stroke (intracranial hemorrhage and subarachnoid hemorrhage).
2.3 Statistical Analysis
Clinical characteristics and outcomes of the ASDs and no-ASDs groups are presented as number (%), mean and standard deviation (SD), or median and interquartile range (IQR), as appropriate. Numbers of missing observed variables are also presented. We used the Student t test or Wilcoxon rank-sum test for analyzing continuous data according to their distribution, and the Chi-square test for categorical data. The observation began on 26 February 2013 (index date) until the date of death or last visit at the participating centers. Follow-up periods were separately calculated for each outcome, taking into consideration censoring due to death or last visit to calculate the incidences and survival functions. In estimating the cause-specific survival functions, we ignored nonfatal outcomes, except for the analyzed outcomes. The incidence of clinical outcomes was stratified by group and estimated with cases per 1000 patient-years. In addition, we used the Kaplan–Meier method and log-rank test for evaluating the cumulative incidence and intergroup differences, respectively.
Hazard ratios (HRs) with 95% confidence intervals (CIs) of the outcomes of the ASDs group in comparison with those of the no-ASDs group were estimated using Cox proportional hazard models. We included the clinically relevant variables to adjust the potential confounders in the multivariable Cox proportional hazard models. The adjusters for ischemic events, ischemic stroke, and AMI were age; CHADS2 score; baseline hemoglobin level; medical histories such as coronary artery disease (CAD), malignancy, and major bleeding; hemodialysis (HD) or renal transplant; use of drugs such as aspirin, clopidogrel or prasugrel, ticlopidine, statin, β-blockers, angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs), and nonsteroidal anti-inflammatory drugs (NSAIDs); time in therapeutic range (TTR); and switching from VKAs to direct OACs (DOACs). For major bleedings and hemorrhagic stroke, the adjusters were age; HAS-BLED score; baseline hemoglobin level; medical histories such as CAD and malignancy; use of aspirin, clopidogrel or prasugrel, ticlopidine, statin, β-blockers, ACEIs or ARBs, and NSAIDs; TTR; and switching from VKAs to DOACs. The adjustment for all-cause mortality was a combination of these factors.
To estimate the adjusted HRs for each subgroup and the interaction p values, we constructed the same multivariable Cox proportional hazard models for primary outcomes in the subgroups. The subgroups included age (≥ 75 or < 75 years), sex, NVAF type (paroxysmal or persistent), current smoking, DM history, estimated glomerular filtration rate (eGFR) (≥ 60, < 60 but ≥ 30, < 30 or HD), stroke history, CAD history, malignancy history, use of aspirin and NSAIDs, CHADS2 score (≥ 2 or < 2), HAS-BLED score (≥ 3 or < 3), and switching from VKAs to DOACs.
As sensitivity analysis, we constructed the propensity score for the use of ASDs and estimated the HRs on the propensity score-matched cohort. We constructed the multivariable logistic regression model for the use of ASDs with 16 variables relevant to the selection of ASDs, including age; medical histories such as CAD, chronic liver disease, malignancy, and major bleeding; HD; hemoglobin, platelet < 10 × 104/µL; creatinine; TTR; use of aspirin, clopidogrel or prasugrel, ticlopidine, and NSAIDs; switching from VKAs to DOACs; and HAS-BLED score. After calculating the propensity score by summing up all coefficients of variables, patients in the ASDs group were matched to those in the no-ASDs group using a 1:1 greedy matching technique. We eliminated those patients without counterparts with corresponding propensity score, and finally constructed the propensity score-matched cohort of 5756 patients (ASDs group: 2878 patients; no-ASDs group: 2878 patients). Because some patient characteristics were not balanced even after propensity score matching, we constructed the Cox proportional hazard models adjusting for unbalanced variables such as type of AF, medical history such as hypertension, DM, and heart failure, and use of β-blockers. We evaluated HRs and their 95% CIs to assess the risk of the ASDs group relative to the no-ASDs group for each outcome measure.
A two-sided p value < 0.05 was considered statistically significant. All statistical data were analyzed using JMP 15 (SAS Institute Inc., Cary, NC, USA).
3 Results
3.1 Patient Characteristics
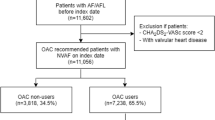
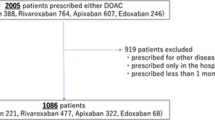
Among 8366 patients initially registered in this study, 540 (7%) were excluded, leaving 7826 patients for analysis (Fig. 1). The mean (SD) age was 73 (10) years and 5274 (67%) patients were males. Paroxysmal NVAF and persistent NVAF were found in 2643 (34%) and 4185 (53%) patients, respectively (Table 1).
The ASDs group included 3476 (44%) patients and was significantly older (mean 74 years vs. 72 years, p < 0.0001) and included fewer males (65% vs. 70%, p < 0.0001) than the no-ASDs group. The ASDs group also had significantly higher incidences of hypertension (80% vs. 77%, p = 0.0002), peripheral arterial disease (10% vs. 7%, p < 0.0001), CAD (33% vs. 21%, p < 0.0001), acute coronary syndrome (14% vs. 8%, p < 0.0001), percutaneous coronary intervention (14% vs. 5%, p < 0.0001), coronary artery bypass graft (4% vs. 2%, p < 0.0001), stroke (27% vs. 23%, p < 0.0001), chronic obstructive pulmonary disease (5% vs. 4%, p = 0.0057), heart failure (46% vs. 39%, p < 0.0001), and major bleeding (5% vs. 2%, p < 0.0001). The incidences of reduced left ventricular ejection fraction (LVEF; 8% vs. 4%, p < 0.0001), reduced eGFR (< 60 mL/min/1.73 m2) or HD (57% vs. 48%, p < 0.0001), and reduced hemoglobin level (< 11 g/dL; 13% vs. 7%, p < 0.0001) were also higher in the ASDs group than in the no-ASDs group. In contrast, TTR was not significantly higher in the ASDs group than in the no-ASDs group (84% vs. 83%, p = 0.29). The ASDs group was also prescribed more aspirin (29% vs. 15%, p < 0.0001), clopidogrel or prasugrel (7% vs. 3%, p < 0.0001), ticlopidine (2% vs. 1%, p = 0.0003), statins (36% vs. 31%, p < 0.0001), β-blockers (46% vs. 39%, p < 0.0001), ACEIs or ARBs (55% vs. 50%, p = 0.0001), and NSAIDs (5% vs. 3%, p < 0.0001) than the no-ASDs group. Switching from VKAs to DOACs was not significantly lower in the ASDs group than in the no-ASDs group (24% vs. 25%, p = 0.25). Moreover, the median CHADS2 score and HAS-BLED score were numerically similar between such groups (2 vs. 2, p < 0.0001; 2 vs. 2, p < 0.0001, respectively) (Table 1).
3.2 Outcomes
Between the ASDs group and the no-ASDs group, the cumulative incidences of primary outcomes such as ischemic events and major bleedings at 4 years were 5.82% vs. 5.31% (p = 0.42) and 9.86% vs. 7.92% (p = 0.19), respectively (Fig. 2a, b). The cumulative incidence of all-cause mortality was significantly different between the two groups (10.75% vs. 6.66%, p < 0.0001) (Fig. 2c). According to cases per 1000 patient-years, the incidences of ischemic events, major bleeding, and all-cause mortality in the ASDs group versus the no-ASDs group were 15.28 vs. 13.84, 25.22 vs. 22.25, and 26.89 vs. 16.93, and the adjusted HRs (95% CIs) were 0.998 (0.78–1.27), 0.98 (0.81–1.18), and 1.22 (1.02–1.47), respectively (Table 2).
For the secondary outcomes, the cumulative incidences of ischemic stroke, AMI, and hemorrhagic stroke between the ASDs and no-ASDs groups were 5.3% vs. 4.83% (p = 0.52), 0.53% vs. 0.46% (p = 0.43), and 1.3% vs. 1.04% (p = 0.42) (Fig. 2d–f) at 4 years, and 13.74 vs. 12.64, 1.61 vs. 1.17, and 3.31 vs. 2.68 in terms of cases per 1000 patient-years, and the adjusted HRs (95% CIs) were 0.96 (0.74–1.24), 0.82 (0.36–1.88), and 1.17 (0.69–1.99), respectively (Table 2).
In the subgroup analyses, we identified those with numerically higher HRs in the switch from VKAs to DOACs, with a significant effect on ischemic events in the ASDs group; the interaction p value was also significant (Fig. 3a). In the subgroups for major bleeding, the higher boundary of 95% CI was lower than 1 in the subgroup of patients with NSAIDs use, and the interaction p value was significant (Fig. 3b). In most subgroups for all-cause mortality, the ASDs group had consistently higher HRs, with no significant interaction p-values in all subgroups (Fig. 3c).
Subgroup analyses on outcomes: a ischemic events; b major bleedings; c all-cause mortality. AF atrial fibrillation, ASDs acid-suppressive drugs, CAD coronary artery disease, CI confidence interval, DOACs direct oral anticoagulants, eGFR estimated glomerular filtration rate, HD hemodialysis, HR hazard ratio, NA not assessed, NSAIDs nonsteroidal anti-inflammatory drugs, VKA vitamin K antagonist
3.3 Sensitivity Analyses
The clinical characteristics were generally similar between the ASDs and no-ASDs groups after propensity score matching, but there were significant differences in some variables we included, such as the type of NVAF, hypertension, DM, percutaneous coronary intervention, heart failure, reduced LVEF (< 40%), reduced eGFR (< 60 mL/min/1.73 m2) or HD, and β-blockers were not balanced (Table 1). In the propensity score-matched cohort, the adjusted HRs (95% CIs) for ischemic events, major bleeding, and all-cause mortality were 0.86 (0.65–1.15), 0.9 (0.72–1.12), and 1.27 (1.02–1.58), respectively (Table 3). The HRs for other outcomes were also consistent with the results of the entire cohort (Table 3).
4 Discussion
Our study shows that patients with NVAF taking ASDs had a significantly higher mortality risk than those with NVAF without ASD prescription; however, the ischemic events and major bleedings were not significantly different between the two groups. This study is the first to describe an increased risk of all-cause mortality among OAC-treated patients with NVAF receiving ASDs.
Singh et al. have reported that despite improvements in the care of patients with atrial fibrillation, all-cause mortality did not significantly change during the study period from 2007 to 2015 [22]. Cardiovascular death significantly decreased, but noncardiovascular death significantly increased, resulting in no significant change in all-cause mortality during the study period. Furthermore, noncardiovascular and cardiovascular death accounted for 61% and 39%, respectively [22]. The noncardiovascular death included cancer (30% of noncardiovascular deaths) and respiratory failure (10%) [22]. Although the causes of death were not examined, such noncardiovascular deaths could be the majority in our study. The increased risk of mortality with ASDs could be explained if the noncardiovascular death was dominant.
PPIs have been reported to be associated with gastric cancer, nosocomial pneumonia, and community-acquired pneumonia [1, 2, 9, 11,12,13, 23]. The long-term exposure to PPIs was reported to increase the risk of gastric cancer due to gastrin-mediated trophic stimulus of gastric mucosa, gastric atrophy, and alteration of gut microbiota and gastric mucosal immunology [11]. The increased risk of death due to upper gastrointestinal cancer was more evident in those without documented indication for ASDs [11]. Micro-aspiration of the altered gut flora due to decreased gastric acidity with PPIs was considered a mechanism for the increased pneumonia risk [24]. Proton pumps were localized in the upper and lower respiratory tract, and pH dysregulation due to PPIs also altered respiratory flora, resulting in the increased risk of respiratory tract infections [24].
Other pathophysiology for increased mortality with ASDs should be considered. The suppression of gastric acidity and the alteration in gut bacterial flora was reported to lead to Clostridium difficile infections among long-term PPI users [23]. Abolishing acid production due to PPIs could interfere with the absorption of nutrients, which enhances the risk of malnutrition, including B12 deficiency, hypomagnesemia, and hypokalemia [23]. The electrolyte disturbances also contributed to the increased cardiovascular death risk, such as arrhythmias [23]. Other risks of PPIs were reported as acute interstitial nephritis, chronic kidney disease, collagenous colitis, anemia, osteoporotic fractures, and dementia [1,2,3, 8,9,10,11,12,13]. H2RAs were also reported to be associated with cytopenia, nephrotoxicity, and hepatotoxicity [1].
In addition to the effects of ASDs on mortality risk, interactions between ASDs and OACs should be considered. Concomitant use of PPIs was reported to reduce dabigatran absorption [14], which could be consistent to our finding that there was significant interaction between ASDs and switching from VKAs to DOACs in terms of ischemic events.
Despite these explanations, other conditions related to concomitant use of ASDs should be considered. Although we adjusted the potential confounders in this study, the ASD group included more patients with comorbidities than the no-ASD group, and the adjustments might not be inadequate. Kimura et al. reported that PPI use is associated with an increased risk for all-cause mortality in patients after undergoing percutaneous coronary intervention [25], although the unobserved differences in patients’ characteristics in these studies might have contributed to the increased risk of death.
In this study, prescribing ASDs to patients with NVAF increased the risk for all-cause mortality. Mizokami et al. reported that PPIs were prescribed to more than half of patients with NVAF without an appropriate indication, including gastrointestinal disorders [2]. Therefore, physicians need to carefully consider the benefits and risks of ASDs and prescribe ASDs to patients with NVAF having distinct indications for ASDs.
4.1 Limitations
This study has several limitations. First, we did not consider the details of the ASDs, including the type, duration, and daily dosage of the medication. Because different types of ASDs have divergent pharmacologic effects on OACs [14], and the pharmacological effects of ASDs depend on the duration of administration, further studies are needed on the prognostic value of different types of ASDs or the duration of administration. Second, our study did not include patients with NVAF who were not taking OACs because this study was a subanalysis of an historical registry study that investigated those taking OACs. Therefore, the effect of ASDs on all patients with NVAF irrespective of the use of OACs could not be investigated. Thus, our findings should be limited in those with NVAF taking OACs. Third, the registry did not include data on the types of ischemic or hemorrhagic strokes, components of major bleedings, or reasons for death. In particular, because death is the most fatal adverse event of PPIs in patients with NVAF [2], causes of death should be further evaluated. Fourth, we did not scrutinize the incidences of acid-related diseases, including gastrointestinal tract examination. Therefore, the effects of ASDs on such gastrointestinal diseases remain uncertain. Finally, the sample size was insufficient to evaluate low-incidence events, such as AMI. Considering that AMI is one of the important adverse events of PPIs [12], we should increase the sample size in future to clarify the association between AMI and ASDs.
5 Conclusions
Among patients with NVAF taking OACs, patients with ASDs had a significantly higher incidence of all-cause mortality than those without ASDs as a co-therapy of OACs. Further clinical studies are needed to confirm the effect of ASDs on clinical outcomes in patients with NVAF.
Change history
18 August 2022
A Correction to this paper has been published: https://doi.org/10.1007/s40268-022-00401-7
References
Fisher L, Fisher A. Acid-suppressive therapy and risk of infections: pros and cons. Clin Drug Investig. 2017;37:587–624.
Mizokami Y, Yamamoto T, Atarashi H, Yamashita T, Akao M, Ikeda T, et al. Current status of proton pump inhibitor use in Japanese elderly patients with non-valvular atrial fibrillation: a subanalysis of the ANAFIE Registry. PLoS ONE. 2020;15(11): e0240859.
Shikata T, Sakaki N, Ueda M, Kimura T, Itohara K, Sugahara M, et al. Use of proton pump inhibitors is associated with anemia in cardiovascular outpatients. Circ J. 2015;79:193–200.
Komen J, Pottegard A, Hjemdahl P, Mantel-Teeuwisse K, Wettermark B, Hellfritzsch M, et al. Non-vitamin K antagonist oral anticoagulants, proton pump inhibitors and gastrointestinal bleeds. Heart. 2022;108:613–8.
Lee SR, Kwon S, Choi E, Jung J, Han K, Oh S, et al. Proton pump inhibitor co-therapy in patients with atrial fibrillation tread with oral anticoagulants and a prior history of upper gastrointestinal tract bleeding. Cardiovasc Drugs Ther. 2021. https://doi.org/10.1007/s10557-021-07170-6 (Epub 17 Mar 2021).
Lee HJ, Kim HK, Kim BS, Han KD, Park JB, Lee H, et al. Risk of upper gastrointestinal bleeding in patinents on oral anticoagulant and proton pump inhibitor co-therapy. PLoS ONE. 2021;16(6): e0253310.
Nicolau JC, Bhatt DL, Hohnloser SH, Kimura T, Lip GYH, Miede C, RE-DUAL PCI Steering Committee and Investigators, et al. dabigatran dual therapy vs warfarin triple therapy post-percutaneous coronary intervention in patients with atrial fibrillation with/without a proton pump inhibitor: a pre-specified analysis of the RE-DUAL PCI trial. Drugs. 2020;80(10):995–1005.
Shiraev TP, Bullen A. Proton pump inhibitors and cardiovascular events: a systematic review. Heart Lung Circ. 2018;27:443–50.
Xie Y, Bowe B, Li T, Xian H, Yan Y, Al-Aly Z. Risk of death among users of proton pump inhibitors: a longitudinal observational cohort study of United States veterans. BMJ Open. 2017;7: e015735.
Kosedo I, Tokushige A, Takumi T, Yoshikawa A, Teraguchi K, Takenouchi K, et al. Use of proton pump inhibitors is associated with an increase in adverse cardiovascular events in patients with hemodialysis: Insight from the kids registry. Eur J Intern Med. 2020;72:79–87.
Xie Y, Bowe B, Yan Y, Xian H, Li T, Al-Aly Z. Estimates of all cause mortality and cause specific mortality associated with proton pump inhibitors among US veterans: cohort study. BMJ. 2019;365: l1580.
Huang M, Han M, Han W, Kuang L. Proton pump inhibitors versus histamine-2 receptor blockers for stress ulcer prophylaxis in patients with sepsis: a retrospective cohort study. Int J Med Res. 2021;49(6):1–12.
Boban M, Persic V, Petricevic M, Biocina B, Sipic T, Pehar-Pejcnovic V, et al. Connections between nutritional status and proton pump inhibitor therapy in patients scheduled for cardiovascular rehabilitation after treatments for ischemic and valvular heart disease. Kardiolojia Polska. 2016;74(5):461–8.
Minno AD, Frigerio B, Spadarella G, Ravani A, Sansaro D, Amato M, et al. Old and new oral anticoagulants: food, herbal medicines and drug interactions. Blood Rev. 2017;31(4):193–203.
Morimoto T, Uchida K, Sakakibara F, Kinjo N, Ueda S. Effect of concomitant antiplatelet therapy on ischemic and hemorrhagic events in patients taking oral anticoagulants for nonvalvular atrial fibrillation in daily clinical practice. Pharmacoepidemiol Drug Saf. 2021;30(10):1321–31.
Arai H, Ueda S, Uchida K, Sakakibara F, Kinjo N, Nezu M, et al. Effect of current smoking on ischemic events in patients with atrial fibrillation taking vitamin K antagonist. Int J Cardiol Cardiovasc Risk Prev. 2022;14: 200135.
Ministry of Health, Labour and Welfare. Ethical guidelines for medical and health research involving human subjects. https://www.mhlw.go.jp/file/06-Seisakujouhou-10600000-Daijinkanboukouseikagakuka/0000080278.pdf. Accessed 14 July 2022
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the national registry of atrial fibrillation. JAMA. 2001;285:2864–70.
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart survey. Chest. 2010;138:1093–100.
Hicks KA, Tcheng JE, Bozkurt B, Chaitman BR, Cutlip DE, Farb A, et al. 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards). J Am Coll Cardiol. 2015;66:403–69.
Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3:692–4.
Singh SM, Abdel-Qadir H, Pang A, Fang J, Koh M, Dorian P, Wijeysundera HC, Ko DT. Population trends in all-cause mortality and cause specific-death with incident atrial fibrillation. J Am Heart Assoc. 2020;9(e016810):1–9.
Pello Lázaro AM, Cristóbal C, Juan Antonio Franco-Peláez JA, Tarín N, Aceña A, Carda R, Huelmos A, et al. Use of proton-pump inhibitors predicts heart failure and death in patients with coronary artery disease. PLoS ONE. 2016;12(1):e0169826. https://doi.org/10.1371/journal.pone.0169826.
Lambert AA, Lam JO, Paik JJ, Ugarte-Gil C, Drummond MB, Crowell TA. Risk of community-acquired pneumonia with outpatient proton-pump inhibitor therapy: a systematic review and meta-analysis. PLoS ONE. 2015;10(6): e0128004. https://doi.org/10.1371/journal.pone.0128004.
Kimura T, Morimoto T, Furukawa Y, Nakagawa Y, Kadota K, Iwabuci M, et al. Association of the use of proton pump inhibitor with adverse cardiovascular and bleeding outcomes after percutaneous coronary intervention in the Japanese real world clinical practice. Cardiocvasc Interv and Ther. 2011;26(3):222–33.
Acknowledgments
The authors are indebted to the data managers of the Institute for Clinical Effectiveness (Ms. Makiko Ohtorii, Ms. Ai Sunagawa, Ms. Kaori Yamamoto, Ms. Sachiko Kitamura, Ms. Hirono Saito, and Ms. Saeko Nagano) for managing the data and performing the statistical analyses.
Funding
This study was supported in part by Bristol Myers Squibb and JSPS KAKENHI (JP21H03176). The funders did not participate in any part of the study from conception to article preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Ethics statement
The Institutional Review Boards of the University of the Ryukyus (No. 597) and all 71 participating centers approved the study protocol in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan (electronic supplementary Table). Written informed consent was replaced with the opt-out method.
Competing Interests
Dr. Morimoto reports lecturer's fees from Bayer, Daiichi Sankyo, Japan Lifeline, Kyocera, Mitsubishi Tanabe, Novartis, and Toray; the manuscript fees from Bristol-Myers Squibb and Kowa; served advisory boards for Asahi Kasei, Boston Scientific, Bristol-Myers Squibb, and Sanofi. Dr. Ueda reports receiving a research grant from Bristol-Myers Squibb, Chugai, Kowa, MSD, Pfizer, and Takeda, lecturer’s fee from Boehringer Ingelheim, MSD, and Taiho, and manuscript fees from Kowa. He served on an advisory board for Otsuka. Dr. Uchida reports lecturer's fees from Daiichi Sankyo. Dr. Arai, Dr. Sakakibara, Dr. Kinjo, and Dr. Nezu declare that they have no competing interests.
Availability of data and materials
Not applicable.
Authorship
TM and SU: study conception and design, and data acquisition and management. HA and TM: statistical analyses. All authors: interpretation of the data, HA and TM: drafting of the manuscript. SU, KU, FS, NK, and MN: critical revision of the manuscript. All authors: final approval of the manuscript.
Additional information
The original online version of this article has been revised as the section “Completing interests” should read as “Competing Interests”.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Arai, H., Ueda, S., Uchida, K. et al. Association between Acid-Suppressive Drugs and Clinical Outcomes in Patients with Nonvalvular Atrial Fibrillation. Drugs R D 22, 213–222 (2022). https://doi.org/10.1007/s40268-022-00392-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-022-00392-5