Abstract
Background
Infliximab pharmacokinetic studies have been performed in patients receiving chronic infliximab therapy. In these patients, infliximab antidrug antibodies (ADAs) increase infliximab clearance and decrease serum levels and drug efficacy.
Objective
This study analyzed the pharmacokinetic effect of infliximab ADAs in healthy subjects receiving a single dose of intravenous infliximab.
Methods
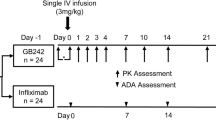
Data were obtained from a single-blind, parallel-group, single-dose study of healthy subjects receiving 5 mg/kg of intravenous SB2 (infliximab biosimilar), EU-sourced Remicade (EU-IFX) or US-sourced Remicade (US-IFX). Serum infliximab was measured at 1, 2, 3, 6, 12, 24, 48, and 72 h and at 5, 7, 14, 21, 28, 42, 56, and 70 days after administration. ADAs were measured pre-dose and at 29 and 71 days. Data from the first ten subjects randomized to each treatment arm were utilized for this study. A two-compartment model of the serum infliximab vs. time curve was developed using nonlinear regression.
Results
At 10 weeks, 11 subjects (37%) developed ADAs. ADAs were detected in four subjects after SB2, one subject after EU-IFX, and six subjects after US-IFX infusion. Of these, neutralizing antibodies occurred in one subject after SB2, in no subjects after EU-IFX, and in three subjects after US-IFX infusion. Infliximab clearance was increased in subjects with ADAs vs. those without ADAs (12.89 ± 2.69 vs. 9.90 ± 1.74 ml/h; p < 0.0005). The elimination half-time was shorter in subjects with ADAs (282.4 ± 56.4 vs. 343.3 ± 61.9 h; p < 0.01). Serum infliximab measured at 8 weeks correlated closely with infliximab clearance (R 2 = 0.5494; p < 0.0001).
Conclusion
ADAs are common in healthy subjects after a single intravenous dose of infliximab and result in faster infliximab clearance, shorter elimination time, and lower serum infliximab levels. These data confirm that ADAs are common with biologic therapy and significantly impact the efficacy of these drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This is the first study detailing the pharmacokinetic effects of antidrug antibodies (ADAs) following a single dose of intravenous infliximab in a group of healthy subjects. |
The study demonstrates that ADAs to infliximab develop in 37% of healthy subjects and that clearance of infliximab is more rapid, elimination half times are shorter, and trough levels are decreased in subjects with ADAs. |
This information enhances our understanding of the development of ADA formation after initiation of biologic therapy and adds to the literature on adverse effects of biologic therapy. |
1 Introduction
Infliximab, a chimeric immunoglobulin (Ig)-G1 monoclonal antibody (mAb) against tumor necrosis factor (TNF)-α, is used as a treatment for multiple cytokine-mediated inflammatory disorders [1]. Detailed analyses of infliximab pharmacokinetics have been reported in patients with Crohn’s disease [2], ulcerative colitis [3, 4], rheumatoid arthritis [5], and ankylosing spondylitis [6, 7]. Published formal pharmacokinetic studies of infliximab in healthy subjects have focused on comparison of infliximab biosimilars [8,9,10]. In clinical practice, serum levels obtained before administration of ongoing infusions of infliximab are used as a surrogate for the measurement of systemic infliximab clearance (CL). These serum trough levels are used to make clinical decisions regarding changes in dosage, dosing interval, and discontinuation of infliximab [11]. The development of antidrug antibodies (ADAs) has an important influence on the utility of biologic therapy in an individual patient. ADAs have been documented in patients receiving multiple doses of a variety mAbs, including infliximab. The development of infliximab ADAs is associated with infusion reactions, lower trough levels, and decreased drug efficacy in patients receiving ongoing infliximab treatment [12, 13]. This study investigated the timing and incidence of ADAs and their effect on formal infliximab pharmacokinetics in a group of healthy subjects receiving a single dose of intravenous infliximab.
2 Materials and Methods
Data were obtained from a single-blind, parallel-group, single-dose study of healthy subjects in three treatment groups: SB2 (an infliximab biosimilar; Samsung Bioepis, Incheon, Republic of Korea); EU-sourced Remicade (EU-IFX; MSD, Haar Germany); and US-sourced Remicade (US-IFX; Janssen Biotech, Malvern, PA, USA) [10]. In that study, 159 subjects received 5 mg/kg of intravenous SB2, EU-IFX, or US-IFX for 120 min on study day 1 and were followed for 10 weeks for safety, pharmacokinetic, and immunogenicity measurements. Intravenous hydrocortisone, oral acetaminophen, and oral loratadine were given prior to the infusion. Baseline height and weight was measured for each subject. Serum infliximab levels were measured at 1, 2, 3, 6, 12, 24, 48, and 72 h and at 5, 7, 14, 21, 28, 42, 56, and 70 days after administration. Samples were collected for ADA and neutralizing antibodies (Nabs) at pre-dose and 28 and 70 days after dosing. ADAs were detected by electrochemiluminescent (ECL) immunoassay, and a functional cell-based assay was used to detect Nabs [10]. Samples were kept frozen at −70 °C or colder prior to analysis. The serum concentration of infliximab was measured using an enzyme-linked immunosorbent assay (ELISA) specific for the detection and quantification of infliximab by TNFα (R&D Systems, product no. 210-TA-001MG/CF) coated in wells of an ELISA plate (PPD Bioanalytical Laboratory, Richmond, VA, USA). The concentration limit of quantification was from 100 to 3200 ng/ml. Inter-assay precision measured as the percent coefficient of variation (%CV) were from 6.1 to 9.2%, and the inter-assay accuracy expressed as the percent difference of the mean value were from 1.9 to 4.8% within the quantification limit. The analysis of the samples for immunogenicity used validated, tiered ECL immunoassays. Following an initial screen for the presence of ADAs, a confirmation assay was performed to indicate whether a positive screened sample had a specific reaction with free drug. The ECL method employed a bridging ligand binding assay, using labelled versions of the three forms of infliximab, to minimize inter-assay variability and both false-positive and false-negative results due to the labelling of multiple antigens. A previously validated cell-based assay was used to determine whether ADA-positive samples also had neutralizing activities [14]. The %CV for the negative control and high positive control for ADA detection were 33.7 and 26.4%, respectively [10]. The drug tolerance level of the ADA assay is 100 µg/ml to detect ADA concentrations of 77–10,000 ng/ml.
Prior analysis showed similar pharmacokinetic and ADA development with the three infliximab preparations [10]. Data from the first ten subjects who were randomized to each treatment arm constituted the group of 30 subjects examined in this study. Serum infliximab levels were analyzed using a one-compartment model and a two-compartment model assuming a biphasic distribution of the serum infliximab vs. time curve [15]. Nonlinear regression was performed with the Prism program (Graph Pad Software, San Diego, CA, USA). These analyses revealed the following parameters: distribution rate constant (K 1), elimination rate constant (K 2), and area under the serum vs. time curve to the last measured data point (AUC C 0 –C last). Formulas for calculated parameters were as follows:
Volume of distribution (V d) was calculating by finding the Y intercept (Y0 elim) of the log values for the elimination portion of each curve beginning at day 21 using the following formula:
Comparison for parameters of interest (Cl, t ½ elim, serum infliximab at 8 and 10 weeks) in subjects with and without ADAs were performed using unpaired t tests.
The relationships between infliximab clearance and V d, body mass index (BMI), and age were measured as correlation coefficients using Spearman rank tests. A linear regression model was developed to explore the relationship with 8-week serum infliximab levels. The extra-sum-of-squares F test compared the goodness of fit of two alternative nested models while favoring the simpler (one compartment) model. p values for the F test are calculated from rations of F values of the two models. Comparisons of R 2 for both analysis in each case were also performed.
We calculated the sample size for the study as follows: 12 subjects per group would be required to detect a >30% difference in infliximab clearance with a standard deviation of 3 ml/h with 80% power.
3 Results
At 70 days (10 weeks) after dosing, 11 of 30 subjects (37%) developed ADAs and four of these (13% of total) had Nabs. No ADAs were detected at baseline or at 28 days after dosing. ADAs were detected in four subjects after SB2, one subject after EU-IFX, and six subjects after US-IFX. Of these, Nabs occurred in one subject after SB2, no subjects after EU-IFX, and three subjects after US-IFX. Infliximab clearance was markedly increased in subjects with ADAs compared with those without ADAs (12.89 ± 2.69 vs. 9.90 ± 1.74 ml/h, respectively, p < 0.0005). Infliximab clearance in subjects with ADAs may also be expressed as 309.36 ± 64.56 ml/day and for subjects without ADAs as 237.6 ± 41.76 ml/day. As shown in Fig. 1, t ½ elim was shorter in subjects with ADAs than in those without ADAs (282.4 ± 56.4 vs. 343.3 ± 61.9 h, respectively, p < 0.01. t ½ elim may also be expressed as 11.77 ± 2.35 days in subjects with ADAs and 14.3 ± 2.58 days in subjects without ADAs. Figure 2 shows serum infliximab vs. time curves in two representative patients, one with and one without ADAs. Decreased serum infliximab at 8 and 10 weeks was also seen in subjects with ADAs. Table 1 shows comparative parameter values in subjects with and without ADAs. Peak infliximab levels occurred 3 h after the start of infusion in 19 subjects (63%) and 2 h after the start in 11 subjects (37%). No statistically significant correlations were found between clearance or V d and body weight, BMI, or peak infliximab levels. There was a trend toward a decreasing infliximab V d with increasing patient age (r = −0.3588; p = 0.0551; see Table 2).
As shown in Fig. 3, linear regression demonstrated a closely defined relationship between infliximab clearance and 8-week serum infliximab levels, defined by the equation Y = −1.076 × X + 17.11 (r 2 = 0.5494; p < 0.0001). The two-compartment model was shown to be superior to a single-compartment model in 29 of 30 cases using the extra-sum-of-squares F test and in all studies by comparison of R 2 for both models. Values for K 1 elimination for the one-compartment model and for K 1 distribution and K 2 elimination are shown in Table 1 in the Electronic Supplementary Material (ESM). Comparison of the one- and two-compartment models using the extra-sum-of-squares F test are shown in Table 2 in the ESM.
4 Discussion
Literature on the pharmacokinetics of mAbs, including infliximab, is extensive [15]. Some of these publications are based on formal pharmacokinetic studies and have generally focused on patients with chronic inflammatory diseases, including inflammatory bowel disease, rheumatoid arthritis, and ankylosing spondylitis [2,3,4,5,6,7]. These formal pharmacokinetic studies are performed in patients receiving chronic infliximab therapy. Published studies in patients with chronic inflammatory diseases have not focused on the analysis of single-dose pharmacokinetics that occur on initiation of therapy in these patients. In addition, few studies have focused on the timing of the occurrence of ADAs as related to the infliximab treatment cycle in patients with chronic inflammatory diseases [16]. Prior research has demonstrated that the presence of infliximab ADAs alter its pharmacokinetics by increasing infliximab clearance [13, 15,16,17,18]. Several recent studies of infliximab biosimilars have noted the presence of ADAs in healthy subjects after a single infliximab dose [9, 10]. This is the first study to formally evaluate the timing, frequency of development, and pharmacokinetic effects of ADAs that occur after the first dose of infliximab in healthy subjects. Our study demonstrates that 37% of healthy subjects receiving a single dose of infliximab will develop ADAs and that these appear 10 weeks after dose administration. Furthermore, the presence of ADAs in this population profoundly increases infliximab clearance. This finding has implications related to the administration of both infliximab and other biologic therapies. Since the development of infliximab ADAs probably begins at the time of the first injection and evolves during its presence in circulation, it is likely that an even higher rate of ADA formation is prevented by premedication with intravenous hydrocortisone. These ADA rates are also comparable to results in studies of patients with autoimmune disorders receiving infliximab as chronic therapy. In these patients, it is anticipated that an overall lower rate of ADA formation compared with in healthy subjects is likely because of immune dysregulation and the concomitant use of immunomodulating agents. However, comparative studies are lacking and are unlikely to be performed. This analysis also investigates factors that were previously determined to influence the pharmacokinetic parameters Vd and clearance of infliximab in patients with chronic diseases. Factors proposed to alter Vd include age, body weight, serum albumin, and hemoglobin levels, and infliximab clearance is reportedly influenced by disease severity, body weight, serum albumin, and the presence of ADAs [17, 20]. In the present study, neither age nor body weight were shown to influence the Vd or clearance of infliximab in healthy subjects (Table 2). Furthermore, because the dose of infliximab is based on body weight, it is likely that modification of infliximab dosing based on subject weight will result in adjustments in V d and clearance calculations [21]. Our study also demonstrates that single-dose pharmacokinetics of infliximab are best described using a two-compartment model with rapid distribution to a tissue compartment followed by a slower process of elimination from the central compartment.
Potential limitations of this study are that the relatively small number of subjects analyzed may not be representative of the entire healthy population. In addition, pharmacokinetic analysis of a single intravenous dose of infliximab in healthy subjects may only be extrapolated to compare results with prior patient-based pharmacokinetic studies of infliximab. Another potential limitation of this study is that data were combined for subjects receiving three different forms of infliximab, including a recently developed biosimilar. These data represent a detailed analysis of a sampling of a larger study of 159 healthy subjects who received one of three forms of infliximab (SB2, EU-IFX or US-IFX) for comparison of infliximab pharmacokinetics and antibody development [10]. They found that mean infliximab clearances were 10.9 ± 3.2, 11.1 ± 3.0, and 10.7 ± 2.9 ml/h for SB2, EU-IFX, and US-IFX, respectively. All other pharmacokinetic parameters for the three forms of infliximab showed no statistical differences. The overall incidence of post-dose ADAs to infliximab was 47.2, 37.7, and 37.7% in subjects treated with SB2, EU-IFX, and US-IFX, respectively (p = 0.432 between SB2 and EU-IFX; p = 0.432 between SB2 and US-IFX; and p = 1.000 between EU-IFX and US-IFX). The percentage of ADAs with Nabs at 70 days for SB2, EU-IFX, and US-IFX were 56.70 and 35%, respectively [10].
A number of studies investigating the effects of infliximab ADAs have utilized the serum trough level of infliximab as an indirect marker of infliximab clearance [13, 17, 19, 22]. However, without the performance of formal pharmacokinetic studies, including the use of two-compartment models for mAbs, use of a single trough level is a potentially unreliable marker of actual drug clearance. In this study, use of compartment-based pharmacokinetic modeling showed a close relationship between the serum infliximab level determined 8 weeks after the administration of a single dose of infliximab and infliximab clearance determined by formal pharmacokinetic analysis. Previous studies have shown that patients with inflammatory bowel disease who demonstrate a trough level of <3 µg/ml are more likely to experience a lack of efficacy of infliximab and are more likely to have ADAs [11]. The equation derived from linear regression in this study suggests that the trough level measured at 8 weeks can be used to estimate infliximab clearance using the formula infliximab clearance (ml/h) = −1.076 × serum infliximab trough + 17.11. This method suggests that an infliximab trough level of >3 µg/ml used as a marker for adequate infliximab levels in the serum may represent an infliximab clearance rate of >13.882 ml/h. However, serum infliximab levels measured after a single dose may be lower than serum infliximab “trough” levels following multiple infliximab doses, as drug accumulation may occur with repeated dosing. Prospective studies can be used to create standard curves from serum infliximab trough levels and to calculate infliximab clearance in patients with chronic inflammatory disorders. Formalization of the relationship between measured trough levels and infliximab clearance can be used to compare patient groups and to more accurately define infliximab clearance in clinical decision making situations such as dosage adjustment or discontinuation of infliximab.
The occurrence of ADAs in 37% of healthy subjects who received a single intravenous dose of infliximab has important implications for the administration of this and other biologic therapies. Further clinical studies will be required to interpret the significance of rapid ADA development to biologic therapy. Strategies for early intervention to prevent this occurrence may be warranted. However, it is important to recognize that ADAs, at least in patients with inflammatory bowel disease, may be transient regardless of whether attempts are made to prevent their occurrence [22]. Nonetheless, this study shows that development of ADAs has the profound effect of increasing drug clearance following the first dose of biologic therapy. When these medications are used clinically, decreased or failed drug efficacy is anticipated to occur in these patients. The presence of Nabs following a single dose of infliximab and the overall effect of ADAs on increasing infliximab clearance have been identified previously as issues in patients with autoimmune diseases that are treated with these medications on a chronic basis. However, mAbs are also used to treat patients without autoimmune diseases, including patients with a variety of cancers, asthma, hypercholesterolemia, and anthrax infections. Further studies on the development of ADAs and their natural history in the absence of autoimmunity are warranted.
In the future, further understanding of the relationship between serum trough levels and measured values of infliximab clearance will allow clinicians to determine appropriate dosage and dose adjustments in patients receiving this drug. Our study also suggests that body weight and age are unlikely to have a strong effect on Vd or infliximab clearance, although further studies in patients with chronic inflammatory diseases will be needed to confirm or refute these findings.
5 Conclusions
The development of ADAs occurs in more than one-third of healthy subjects after a single intravenous dose of infliximab. More rapid infliximab clearance, shorter elimination time, and lower serum infliximab levels at 8 and 10 weeks are a consequence of the development of infliximab ADAs. These data indicate that ADAs are common with biologic therapy, even following a single dose in healthy patients. Because the presence of ADAs enhances the clearance of these drugs, this study suggests they may be a significant adverse consequence of biologic therapy.
References
Monaco C, Nanchahal J, Taylor P, Feldmann M. Anti-TNF therapy: past, present and future. Int Immunol. 2015;27(1):55–62.
Fasanmade AA, Adedokun OJ, Blank M, Zhou H, Davis HM. Pharmacokinetic properties of infliximab in children and adults with Crohn’s disease: a retrospective analysis of data from 2 phase III clinical trials. Clin Ther. 2011;33(7):946.
Adedokun OJ, Xu Z, Padgett L, Blank M, Johanns J, Griffiths A, Ford J, Zhou H, Guzzo C, Davis HM, Hyams J. Pharmacokinetics of infliximab in children with moderate-to-severe ulcerative colitis: results from a randomized, multicenter, open-label, phase 3 study. Inflamm Bowel Dis. 2013;19(13):2753–62.
Fasanmade AA, Adedokun OJ, Ford J, Hernandez D, Johanns J, Hu C, Davis HM, Zhou H. Population pharmacokinetic analysis of infliximab in patients with ulcerative colitis. Eur J Clin Pharmacol. 2009;65(12):1211–28.
Mori S. A relationship between pharmacokinetics (PK) and the efficacy of infliximab for patients with rheumatoid arthritis: characterization of infliximab-resistant cases and PK-based modified therapy. Mod Rheumatol. 2007;17(2):83–91.
Xu Z, Seitz K, Fasanmade A, Ford J, Williamson P, Xu W, Davis HM, Zhou H. Population pharmacokinetics of infliximab in patients with ankylosing spondylitis. J Clin Pharmacol. 2008;48(6):681–95.
Ternant D, Mulleman D, Lauféron F, Vignault C, Ducourau E, Wendling D, Goupille P, Paintaud G. Influence of methotrexate on infliximab pharmacokinetics and pharmacodynamics in ankylosing spondylitis. Br J Clin Pharmacol. 2012;73(1):55–65.
Shin D, Kim Y, Kim YS, Körnicke T, Fuhr R. A randomized, phase I pharmacokinetic study comparing SB2 and infliximab reference product (Remicade®) in healthy subjects. BioDrugs. 2015;29(6):381–8.
Lambert J, Wyand M, Lassen C, Shneyer L, Thomson E, Knight A, Willers J, Kay J. Bioavailability, safety and immunogenicity of biosimilar infliximab (BOW015) compared to reference infliximab. Int J Clin Pharmacol Ther. 2016;54(4):315–22.
Park W, Lee SJ, Yun J, Yoo DH. Comparison of the pharmacokinetics and safety of three formulations of infliximab (CT-P13, EU-approved reference infliximab and the US-licensed reference infliximab) in healthy subjects: a randomized, double-blind, three-arm, parallel-group, single-dose, phase I study. Expert Rev Clin Immunol. 2015;11(Suppl 1):S25–31.
Vande Casteele N, Ferrante M, Van Assche G, Ballet V, Compernolle G, Van Steen K, Simoens S, Rutgeerts P, Gils A, Vermeire S. Trough concentrations of infliximab guide dosing for patients with inflammatory bowel disease. Gastroenterology. 2015;148(7):1320–9.
Mould DR. The pharmacokinetics of biologics: a primer. Dig Dis. 2015;14(33 Suppl 1):61–9.
Edlund H, Steenholdt C, Ainsworth MA, Goebgen E, Brynskov J, Thomsen OØ, Huisinga W, Kloft C. Increased infliximab clearance imposed by anti-infliximab antibodies in Crohn’s disease is determined by their concentration. AAPS J. 2017;19(1):223–33.
Lee YJ, Shin D, Kim Y, Kang J, Gauliard A, Fuhr R. A randomized phase l pharmacokinetic study comparing SB4 and etanercept reference product (Enbrel®) in healthy subjects. Br J Clin Pharmacol. 2016;82:64–73.
Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84(5):548–58.
van den Bemt BJ, den Broeder AA, Wolbink GJ, Hekster YA, van Riel PL, Benraad B, van den Hoogen FH. Anti-infliximab antibodies are already detectable in most patients with rheumatoid arthritis halfway through an infusion cycle: an open-label pharmacokinetic cohort study. BMC Musculoskelet Disord. 2011;13(12):12.
Buurman DJ, Maurer JM, Keizer RJ, Kosterink JG, Dijkstra G. Population pharmacokinetics of infliximab in patients with inflammatory bowel disease: potential implications for dosing in clinical practice. Aliment Pharmacol Ther. 2015;42(5):529–39.
Passot C, Mulleman D, Bejan-Angoulvant T, Aubourg A, Willot S, Lecomte T, Picon L, Goupille P, Paintaud G, Ternant D. The underlying inflammatory chronic disease influences infliximab pharmacokinetics. MAbs. 2016;8(7):1407–16 Epub 2016 Aug 9.
Dotan I, Ron Y, Yanai H, Becker S, Fishman S, Yahav L, Yehoyada MB, Mould DR. Patient factors that increase infliximab clearance and shorten half-life in inflammatory bowel disease: a population pharmacokinetic study. Inflamm Bowel Dis. 2014;20:2247–59.
University of Lausanne. Pharmacokinetics: an online resource for students. Volume of distribution. http://sepia.unil.ch/pharmacology/?id=61. Accessed 18 Dec 2016.
Gonczi L, Vegh Z, Golovics PA, et al. Prediction of short- and medium-term efficacy of biosimilar infliximab therapy. Do trough levels and antidrug antibody levels or clinical and biochemical markers play the more important role? J Crohns Colitis. 2017;11(6):697–705.
Roblin X, Marotte H, Leclerc M, Del Tedesco E, Phelip JM, Peyrin-Biroulet L, Paul S. Combination of C-reactive protein, infliximab trough levels, and stable but not transient antibodies to infliximab are associated with loss of response to infliximab in inflammatory bowel disease. J Crohns Colitis. 2015;9(7):525–31.
Acknowledgements
Data utilized for this study were provided by Samsung Corporation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was performed without funding.
Conflict of interest
Dr. Ehrenpreis has acted as a consultant for CR Pharmaceuticals and been a member of the Pfizer Advisory Board.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ehrenpreis, E.D. Pharmacokinetic Effects of Antidrug Antibodies Occurring in Healthy Subjects After a Single Dose of Intravenous Infliximab. Drugs R D 17, 607–613 (2017). https://doi.org/10.1007/s40268-017-0211-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-017-0211-y