Abstract
Background
Data regarding the importance of multidimensional frailty to guide clinical decision making for remdesivir use in older patients with coronavirus disease 2019 (COVID-19) are largely unexplored.
Objective
The aim of this research was to evaluate if the Multidimensional Prognostic Index (MPI), a multidimensional frailty tool based on the Comprehensive Geriatric Assessment (CGA), may help physicians in identifying older hospitalized patients affected by COVID-19 who might benefit from the use of remdesivir.
Methods
This was a multicenter, prospective study of older adults hospitalized for COVID-19 in 10 European hospitals, followed-up for 90 days after hospital discharge. A standardized CGA was performed at hospital admission and the MPI was calculated, with a final score ranging between 0 (lowest mortality risk) and 1 (highest mortality risk). We assessed survival with Cox regression, and the impact of remdesivir on mortality (overall and in hospital) with propensity score analysis, stratified by MPI = 0.50.
Results
Among 496 older adults hospitalized for COVID-19 (mean age 80 years, female 59.9%), 140 (28.2% of patients) were treated with remdesivir. During the 90 days of follow-up, 175 deaths were reported, 115 in hospital. Remdesivir treatment significantly reduced the risk of overall mortality (hazard ratio [HR] 0.54, 95% confidence interval CI 0.35–0.83 in the propensity score analysis) in the sample as whole. Stratifying the population, based on MPI score, the effect was observed only in less frail participants (HR 0.47, 95% CI 0.22–0.96 in propensity score analysis), but not in frailer subjects. In-hospital mortality was not influenced by remdesivir use.
Conclusions
MPI could help to identify less frail older adults hospitalized for COVID-19 who could benefit more from remdesivir treatment in terms of long-term survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Remdesivir was largely used during the coronavirus disease 2019 (COVID-19) epidemic, but the data regarding older people are still limited. |
Remdesivir use reduced 3-month, but not in-hospital, mortality among older patients hospitalized for COVID-19. |
Based on the Multidimensional Prognostic Index stratification, mortality reduction by remdesivir use was observed only in robust people, not in frailer subjects. |
1 Introduction
The coronavirus disease 2019 (COVID-19) pandemic had an impressive impact on the older population. Almost three of four subjects who died as a result of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection were older adults [1]. During the first pandemic waves, with the maximum spread of contagion and before the availability of COVID-19 vaccines, there was a need for treatments able to mitigate the severity of the manifestations, especially among older adults, to reduce the risk of acute respiratory failure (ARF) and mortality. In July 2020, in the middle of the COVID-19 pandemic, remdesivir was the first drug authorized by the European Medicines Agency (EMA) for the treatment of COVID-19.
Remdesivir is an antiviral drug, developed over a decade ago for the treatment of hepatitis C and infections from respiratory syncytial virus, that had already been previously tested against other coronaviruses, i.e. Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS) [2]. Molecularly, remdesivir acts as a nucleotide analog that blocks replication of SARS-CoV-2 inhibiting the viral RNA-dependent RNA polymerase (RdRp) [3]. Initially, based on the results of the NIAID-ACTT-1 trial, a randomized controlled trial (RCT) involving 1063 hospitalized patients with COVID-19 [4], the EMA gave a ‘conditional marketing authorization’ for remdesivir to treat COVID-19 in adults and adolescents from 12 years of age with pneumonia who required oxygen therapy. The drug could also be used in adults who did not require supplemental oxygen but were at increased risk of developing severe COVID-19. However, since the findings of the Solidarity trial promoted by the World Health Organization (WHO) [5], as well as subsequent reports, inconsistency has emerged in regard to remdesivir efficacy [6, 7]. This may suggest that remdesivir could provide benefits on the clinical course of COVID-19 disease only in specific groups of patients. Indeed, recently revised WHO guidelines recommending treatment with remdesivir only in subjects with non-severe disease, conversely state that treatment could be potentially effective in patients with severe COVID-19, but not in those with critical COVID-19 [8].
Noteworthy, current indications for remdesivir use are mainly based on COVID-19 severity; however, for identification of optimal candidates for this treatment, it might be useful to consider the patients’ multidimensional frailty that is a crucial factor to define the individual’s prognosis and an important driver for clinical decisions, especially in older adults [9, 10]. Indeed, accumulated evidence shows that measurement of multidimensional frailty, through well-validated prognostic tools based on the Comprehensive Geriatric Assessment (CGA) as the Multidimensional Prognostic Index (MPI), may improve the selection of patients for several pharmacological and non-pharmacological treatments [9]. Furthermore, in older adults with COVID-19, higher MPI scores have already been associated with poorer short-term outcomes (e.g., in-hospital mortality and duration of hospitalization) and at 3 months of follow-up (e.g., rehospitalization and mortality) [11, 12]. Finally, MPI is already used in clinical decision making for older adults affected by COVID-19 for better tailoring the use or non-use of mechanical ventilation [12]. However, data regarding the use of remdesivir in older adults, which are usually excluded from RCTs, are still not available [13].
Given this background, using the data from the multicenter MPI COVID-19 study, we aimed to evaluate whether the CGA-based MPI may help physicians in identifying older patients hospitalized for COVID-19 who might benefit in terms of reduced mortality from the use of remdesivir.
2 Materials and Methods
2.1 Study Design and Population
For this research, we included (1) patients ≥ 65 years of age; (2) patients consecutively admitted to hospital in the acute wards of Geriatrics, Infectious Diseases, or Internal Medicine with an ascertained diagnosis of COVID-19 through nasopharyngeal swab with real time-polymerase chain reaction; and (3) patients able to sign an informed consent. Exclusion criteria were the unwillingness to participate in the study and an inability to provide informed consent. The period of enrollment and follow-up was between April 2020 and August 2021. None of the participants was vaccinated as the vaccinations were not available during the study period. Patients were enrolled after admission in each ward across 10 European centers located in Italy, Spain, Czech Republic, Portugal, and Germany.
This was a prospective, observational study conducted according to the World Medical Association's 2008 Declaration of Helsinki, the guidelines for Good Clinical Practice, and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [14]. The Ethical Committees of each center formally approved the study. Informed consent was provided by participants who underwent initial evaluation and/or their proxies in the case of a participant’s inability to understand and sign the informed consent (e.g., severe dementia) for their clinical records to be used in clinical studies according to the local law.
2.2 Outcomes
Data regarding the outcomes of interest were ascertained using death certificates. The primary outcomes of our research were in-hospital and all-cause mortality, during a maximum follow-up period of 90 days from admission in each ward.
2.3 Exposure: Remdesivir
The use of remdesivir was recorded using medical records available, including the period of administration, in days. The administration of remdesivir was in line with the recommendations of the EMA, i.e., pneumonia requiring supplemental oxygen (low- or high-flow oxygen or other non-invasive ventilation at the start of treatment), particularly if patients were at increased risk of developing severe COVID-19 forms [15]. We excluded patients with severe renal or hepatic failure. The period of administration was a minimum of 5 days and a maximum of 10, according to the EMA indications.
2.4 Multidimensional Prognostic Index (MPI)
The evaluation, made with the MPI, was conducted at admission into the medical ward and included information from eight different domains of the CGA [11, 16]. MPI was then calculated, as follows:
-
1.
Functional status—Activities of Daily Living (ADL) index [17].
-
2.
Independence status—Instrumental Activities of Daily Living (IADL) [18].
-
3.
Cognitive status—Short Portable Mental Status Questionnaire (SPMSQ) [19].
-
4.
Co-morbidity—Cumulative Illness Rating Scale (CIRS) [20]. The CIRS uses a 5-point ordinal scale (score 1–5) to estimate the severity of pathology in each of 13 systems. Based on the ratings, the Comorbidity Index (CIRS-CI) scores, reflecting the number of concomitant diseases, were derived from the total number of categories in which moderate or severe levels (grades 3–5) of disease were identified (range 0–13).
-
5.
Nutritional status was investigated using the Mini Nutritional Assessment-Short Form (MNA-SF) [21], which includes information on several nutritional aspects.
-
6.
Risk of developing pressure sores was evaluated through the Exton Smith Scale (ESS) [22].
-
7.
Medication use was defined according to the Anatomical Therapeutic Chemical (ATC) classification code system, and the number of drugs used by patients at admission was also recorded.
-
8.
Social domain was categorized as living alone, in family (or with other support), and in institution.
For each domain, a tripartite hierarchy was used, i.e. 0 = no problems, 0.5 = minor problems, and 1 = major problems, based on conventional cut-off points derived from the literature for the singular items [16]. The sum of the calculated scores from the eight domains was divided by 8 to obtain a final MPI risk score ranging from 0 = no risk, to 1 = higher risk of mortality. MPI requires between 15 and 25 min for its complete execution [23]. In the case of impossibility of completing the CGA (e.g., hyperactive delirium), the evaluation was postponed to the following day, but within 48 h from admission for all participants included [11].
2.5 Clinical, Bio-humoral and Radiological Parameters
Among clinical signs and symptoms, information regarding fever (body temperature ≥ 37.5 °C) and the presence of cough, diarrhea and dyspnea were recorded. Moreover, we investigated the presence of delirium at hospital admission using the 4AT score, a short tool for delirium assessment designed to be easy to use in clinical care [24]. X-ray findings were categorized as bilateral ground-glass opacities versus other findings, while computed tomography findings were suggestive of pneumonia in COVID-19 versus other findings, according to a standardized classification [25]. Finally, data regarding serum inflammatory parameters (i.e., white blood cells, C-reactive protein [CRP] serum levels) and arterial blood gas parameters (pH, pO2, SpO2, pCO2, PaO2/FiO2 ratio) were measured using standard methods across the 10 European centers.
2.6 Statistical Analysis
All patient records and information were anonymized and de-identified prior to the analysis.
To minimize the effect of potential confounders, we used a propensity score matching with one case (remdesivir) and one control that never experienced this kind of intervention during hospitalization. Data on continuous variables were normally distributed according to the Kolmogorov–Smirnov test and then reported as means and standard deviation (SD) values for quantitative measures and percentages for categorical variables, according to use or non-use of remdesivir. Levene’s test was used to test the homoscedasticity of variances and, if its assumption was violated, Welch’s analysis of variance (ANOVA) was used. P-values were calculated using Student’s t-test for continuous variables and the Mantel–Haenszel Chi-square test for categorical variables.
The association between remdesivir and mortality was made using a Cox regression analysis, using a multivariable analysis in which the factors were included if statistically different between patients with remdesivir and controls, or if associated with mortality in univariate analyses (p < 0.05). Age, sex and MPI were included since previous literature suggests a relevant prognostic role for these factors in COVID-19 [26]. No collinearity emerged. Similarly, we did run a propensity-score model. ARF was included as a covariate in the propensity score analysis, since it was not balanced between the two groups. The results were reported as hazard ratios (HRs) with their 95% confidence intervals (CIs). Since the interaction MPI by remdesivir in predicting mortality was significant (p < 0.05), we have reported the HRs stratified according to an MPI value of less than or equal to/more than 0.50 that was identified as the best cut-off as sensitivity and specificity using the Youden’s index [27] and that has since been used in other works as the cut-off for clinical decision making in older adults affected by COVID-19 [12]. The accuracy of prognostic factors predicting negative outcomes during follow-up, in terms of area under the curve (AUC), was analyzed using, as exposure, MPI adjusted for age and sex. Calibration was analyzed using the C-statistic.
All analyses were performed using SPSS 26.0 for Windows (IBM Corporation, Armonk, NY, USA). All statistical tests were two-tailed and statistical significance was assumed for a p-value < 0.05.
3 Results
We initially enrolled 548 subjects (mean age 80.4 years, range 65–99 years; 58% females), of whom 496 were analyzed after removing 9 subjects without an available MPI score, 6 without information regarding remdesivir, and 37 without information regarding mortality. The excluded subjects did not significantly differ from those included, in terms of mean age or prevalence of females (p > 0.05 for both comparisons).
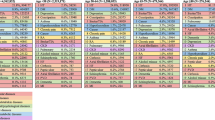
Compared with the 356 patients not using remdesivir, the 140 patients using this medication were significantly younger (p < 0.0001) and less frail, according to the MPI values (p = 0.001), while no significant differences in terms of sex were observed (Table 1). Among the clinical and bio-humoral parameters included, patients using remdesivir had lower white cell counts but similar serum CRP values. Patients taking remdesivir had a worse profile in respiratory parameters, as reported in Table 1, although the difference in prevalence of ARF was not statistically significant between the two groups. Finally, patients using remdesivir presented a worse clinical presentation in terms of presence of pneumonia and signs and symptoms typical of COVID-19. Table 1 shows the baseline characteristics, matched using a propensity score, between remdesivir and controls in which age and MPI scores were similar between the two groups but the prevalence of ARF was unbalanced.
The mean length of stay in hospital was 22 days and the mean time to death was 73 days after hospital admission. During the 90 days of follow-up, 175 deaths were reported, 115 in hospital. As shown in Table 2, remdesivir did not affect in-hospital mortality in the whole sample and in the propensity score model. Similarly, the analyses stratified for MPI did not show any significant interaction in more or less frail patients. At the same time, the use of remdesivir significantly decreased the risk of overall mortality (HR 0.54, 95% CI 0.35–0.83; p = 0.005 in the propensity score analysis) in the sample as a whole. However, when stratified for MPI value (< 0.50 vs. ≥ 0.50) the effect was only present in less frail participants (HR 0.47, 95% CI 0.22–0.96 in the propensity score analysis) and not in frailer individuals (Fig. 1).
Finally, the accuracy of MPI in predicting mortality was good (AUC 0.74, 95% CI 0.69–0.78; p < 0.0001), without differences between patients treated or not treated with remdesivir (AUC 0.72 [95% CI 0.67–0.78] in the non-treated group vs. 0.74 [95% CI 0.66–0.83] in the treated group; p = 0.83 between the two AUCs). Similarly, the calibration of MPI in predicting mortality was good in the sample as whole (C-statistics = 0.71), without differences between patients treated and not treated (0.70 vs. 0.71; p = 0.85).
4 Discussion
In this prospective, observational study on older adults hospitalized with COVID-19 across different European countries, we found that remdesivir administration was associated with a reduction of all-cause mortality at 3 months of follow-up, but not with in-hospital mortality, particularly among less frail patients, according to the MPI, and independently by age, sex, and the presence of ARF at admission. In a real-world experience, we observed that older adults judged as candidates for remdesivir treatment were younger and less frail but with worse pulmonary and respiratory manifestations. When matching patients treated or not treated with remdesivir, using a propensity score, and adjusting for the presence of ARF, the results of in-hospital and 3-month mortality did not change. Finally, MPI showed good accuracy and calibration in predicting mortality, independently from remdesivir treatment.
Systematic revision of the results from five RCTs on 7643 patients suggests that remdesivir could have little or no impact on in-hospital mortality (odds ratio 0.95, 95% CI 0.84–1.07) among patients with severe and critical COVID-19 [8]. As for many RCTs testing pharmacological treatments, one of the main limitations of these trials is the enrollment of a relatively younger population and the exclusion of multimorbid, frail older adults that are, on the contrary, typical of daily clinical practice of a geriatrician. A few observational studies offer a better picture of remdesivir effect among hospitalized older adults [28, 29]. In a cohort of 2344 US veterans hospitalized with COVID-19, remdesivir therapy was not associated with improved 30-day survival [28]. Conversely, in a Spanish population of patients aged 80 years and older hospitalized for COVID-19, those treated with remdesivir exhibited a 60% lower 30-day mortality rate, but these data refer only to the first and second pandemic waves before the vaccination campaign [29]. We showed that remdesivir treatment was not associated with a reduced risk of in-hospital mortality nor in the population as a whole, with neither stratifying according to multidimensional frailty.
However, few studies explored the long-term effects of remdesivir administration on survival. In an observational study of 3889 patients aged ≥ 70 years, remdesivir treatment was associated with a significant improvement (up to 59%) of survival over approximately 8 months of follow-up, halving the mortality risk among those with severe disease as defined by those requiring high-flow oxygen therapy, mechanical ventilation, or extracorporeal membrane oxygenation therapy [30]. In this study, we found a reduction of mortality risk by 46% at 3 months in the whole population and up to 53% among less frail older adults. The severity of respiratory symptoms did not impact on these results, considering that one of four older patients receiving remdesivir had an ARF. The long-term benefit on survival needs to be verified in further randomized studies, but it might potentially justify wider use of remdesivir in older adults when taking into account multidimensional frailty rather than the mere COVID-19 severity for decision making.
Furthermore, during the COVID-19 pandemic, the role of CGA-based assessment has emerged as crucial for clinical decision making [12, 31, 32]. Some controversies on the effectiveness of treatments against COVID-19 disease among the older population [33] might be solved by proper implementation of the CGA-based approach. The MPI, an easy-to-use tool directly derived from a standard CGA, has already demonstrated excellent properties for applying, in routine clinical practice, a tailored approach based on an individual patient’s prognosis [9]. Indeed, the MPI may help to stratify older patients in different settings, including the hospital [16], defining the best candidate for pharmacological treatments as statins [34, 35], oral anticoagulants [36], or anti-dementia drugs [37]. In this study, we found that an MPI score < 0.50 could be a strong prognostic indicator of remdesivir effects, regardless of the presence of an ARF.
The present findings should be interpreted considering some limitations. First, due to the observational nature of this research, we cannot completely rule out selection bias and the effects of residual or unobserved confounding factors. The propensity score matched remdesivir recipients and controls, but there may have been residual confounding related to illness severity, onset of COVID-19 symptoms, or SARS-CoV-2 variants. Second, we were not able to verify remdesivir response based on COVID-19 disease severity according to the WHO guidelines [13]. However, it should be considered that almost 26% of subjects receiving remdesivir had ARF at the beginning of the treatment, and critical subjects, based on the WHO definition, whenever possible were managed in the intensive care unit setting. Finally, our results are not generalizable to the outpatient setting and thus need to be confirmed by ad hoc studies.
5 Conclusion
Older adults hospitalized for COVID-19 with lower levels of multidimensional frailty, as measured by the MPI, might have greater long-term survival when treated with remdesivir. Thus, independently by age, comorbidities and respiratory impairment, CGA-based prognostic tools, such as the MPI, may help to identify older adults who can benefit more from remdesivir treatment.
References
National Center for Health Statistics. Provisional COVID-19 deaths by sex and age. 2022. https://data.cdc.gov/d/9bhg-hcku. Cited 2 Dec 2022.
Yao TT, Qian JD, Zhu WY, Wang Y, Wang GQ. A systematic review of lopinavir therapy for SARS coronavirus and MERS coronavirus—a possible reference for coronavirus disease-19 treatment option. J Med Virol. 2020;92(6):556–63.
Kokic G, Hillen HS, Tegunov D, Dienemann C, Seitz F, Schmitzova J, et al. Mechanism of SARS-CoV-2 polymerase stalling by remdesivir. Nat Commun. 2021;12(1):1–7.
Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of covid-19—final report. N Engl J Med. 2020;383(19):1813–26.
Consortium WHOST, Pan H, Peto R, Henao-Restrepo AM, Preziosi MP, Sathiyamoorthy V, et al. Repurposed antiviral drugs for covid-19—interim WHO solidarity trial results. N Engl J Med. 2021;384(6):497–511.
Young B, Tan TT, Leo YS. The place for remdesivir in COVID-19 treatment. Lancet Infect Dis. 2021;21(1):20–1.
Ansems K, Grundeis F, Dahms K, Mikolajewska A, Thieme V, Piechotta V, et al. Remdesivir for the treatment of COVID-19. Cochrane Database Syst Rev. 2021;8(8):CD014962.
Therapeutics and COVID-19: living guideline, 16 September 2022. 2022. WHO/2019-nCoV/therapeutics/2022.5.
Pilotto A, Custodero C, Maggi S, Polidori MC, Veronese N, Ferrucci L. A multidimensional approach to frailty in older people. Ageing Res Rev. 2020;60: 101047.
Heyns A, Dupont J, Gielen E, Flamaing J, Peers K, Gosselink R, et al. Impact of COVID-19: urging a need for multi-domain assessment of COVID-19 inpatients. Eur Geriatr Med. 2021;12(4):741–8.
Pilotto A, Azzini M, Cella A, Cenderello G, Castagna A, Pilotto A, et al. The multidimensional prognostic index (MPI) for the prognostic stratification of older inpatients with COVID-19: a multicenter prospective observational cohort study. Arch Gerontol Geriatr. 2021;95: 104415.
Pilotto A, Topinkova E, Michalkova H, Polidori MC, Cella A, Cruz-Jentoft A, et al. Can the multidimensional prognostic index improve the identification of older hospitalized patients with COVID-19 likely to benefit from mechanical ventilation? An observational, prospective, multicenter study. J Am Med Dir Assoc. 2022;23(9):1608.e1-e8.
Agarwal A, Rochwerg B, Lamontagne F, Siemieniuk RA, Agoritsas T, Askie L, et al. A living WHO guideline on drugs for covid-19. BMJ. 2020;370: m3379.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guildelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Cavaleri M, Sweeney F, Gonzalez-Quevedo R, Carr M. Shaping EU medicines regulation in the post COVID-19 era. Lancet Reg Health Europe. 2021;9: 100192.
Pilotto A, Ferrucci L, Franceschi M, D’Ambrosio LP, Scarcelli C, Cascavilla L, et al. Development and validation of a multidimensional prognostic index for one-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rejuven Res. 2008;11(1):151–61.
Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10(1):20–30.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–86.
Pfeiffer E. A Short Portable Mental Status Questionnaire (SPMSQ). J Am Geriatr Soc. 1975;23(10):1975.
Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16(5):622–6.
Guigoz Y, Vellas B. The Mini Nutritional Assessment (MNA) for grading the nutritional state of elderly patients: presentation of the MNA, history and validation. In: Nestle nutrition workshop series clinical & performance programme, vol. 1. 1999. pp. 3–11 (discussion-2).
Bliss MR, McLaren R, Exton-Smith AN. Mattresses for preventing pressure sores in geriatric patients. Mon Bull Minist Health Public Health Lab Serv. 1966;25:238–68.
Pilotto A, Veronese N, Daragjati J, Cruz-Jentoft AJ, Polidori MC, Mattace-Raso F, et al. Using the multidimensional prognostic index to predict clinical outcomes of hospitalized older persons: a prospective, multicenter, international study. J Gerontol Ser A. 2019;74(10):1643–9.
Bellelli G, Morandi A, Davis DH, Mazzola P, Turco R, Gentile S, et al. Validation of the 4AT, a new instrument for rapid delirium screening: a study in 234 hospitalised older people. Age Ageing. 2014;43(4):496–502.
Wong CK, Wong JY, Tang EH, Au CH, Wai AK. Clinical presentations, laboratory and radiological findings, and treatments for 11,028 COVID-19 patients: a systematic review and meta-analysis. Sci Rep. 2020;10(1):1–16.
Figliozzi S, Masci PG, Ahmadi N, Tondi L, Koutli E, Aimo A, et al. Predictors of adverse prognosis in COVID-19: a systematic review and meta-analysis. Eur J Clin Investig. 2020;50(10): e13362.
Fluss R, Faraggi D, Reiser B. Estimation of the Youden Index and its associated cutoff point. Biometr J. 2005;47(4):458–72.
Ohl ME, Miller DR, Lund BC, Kobayashi T, Richardson Miell K, Beck BF, et al. Association of remdesivir treatment with survival and length of hospital stay among US veterans hospitalized with COVID-19. JAMA Netw Open. 2021;4(7): e2114741.
Ramos-Rincon JM, Lopez-Carmona MD, Cobos-Palacios L, Lopez-Sampalo A, Rubio-Rivas M, Martin-Escalante MD, et al. Remdesivir in very old patients (>/=80 years) hospitalized with COVID-19: real world data from the SEMI-COVID-19 registry. J Clin Med. 2022;11(13).
Yu M, Kim BI, Kim J, Gwack J. Clinical outcomes of remdesivir-treated COVID-19 patients in South Korea. Osong Public Health Res Perspect. 2022;13(5):370–6.
Inzitari M, Arnal C, Ribera A, Hendry A, Cesari M, Roca S, et al. Comprehensive geriatric hospital at home: adaptation to referral and case-mix changes during the COVID-19 pandemic. J Am Med Dir Assoc. 2023;24(1):3-9.e1.
O’Hanlon S, Dhesi J, Aronson L, Inouye SK. Covid-19: a call for mobilizing geriatric expertise. Eur Geriatr Med. 2021;12(3):597–600.
Senderovich H, Vinoraj D, Stever M, Waicus S. Efficacy of COVID-19 treatments among geriatric patients: a systematic review. Ther Adv Infect Dis. 2022;9:20499361221095666.
Pilotto A, Gallina P, Panza F, Copetti M, Cella A, Cruz-Jentoft A, et al. Relation of statin use and mortality in community-dwelling frail older patients with coronary artery disease. Am J Cardiol. 2016;118(11):1624–30.
Pilotto A, Panza F, Copetti M, Simonato M, Sancarlo D, Gallina P, et al. Statin treatment and mortality in community-dwelling frail older patients with diabetes mellitus: a retrospective observational study. PLoS ONE. 2015;10(6): e0130946.
Pilotto A, Gallina P, Copetti M, Pilotto A, Marcato F, Mello AM, et al. Warfarin treatment and all-cause mortality in community-dwelling older adults with atrial fibrillation: a retrospective observational study. J Am Geriatr Soc. 2016;64(7):1416–24.
D’Onofrio G, Sancarlo D, Addante F, Ciccone F, Cascavilla L, Paris F, et al. A pilot randomized controlled trial evaluating an integrated treatment of rivastigmine transdermal patch and cognitive stimulation in patients with Alzheimer’s disease. Int J Geriatr Psychiatry. 2015;30(9):965–75.
Acknowledgements
This paper is under the auspices of the SIGOT (Italian Geriatric Hospital and Community Society) and the Special Interest Group in CGA of the European Geriatric Medicine Society (EuGMS). An abstract of this work has been previously presented and published in the ‘Abstracts of the 18th Congress of the European Geriatric Medicine Society: Live from London and Online, 28–30 September 2022’.
MPI-COVID-19 Study Group Investigators: Mario Barbagallo (Department of Internal Medicine and Geriatrics, University of Palermo, Palermo, Italy), Simone Dini (Department of Geriatric Care, Orthogeriatrics and Rehabilitation, Galliera Hospital, Genoa, Italy), Naima Madlen Diesner (Division of Geriatrics, University Medical Center Goettingen, Goettingen, Germany), Marilia Fernandes (Serviço de Medicina Interna, Hospital Curry Cabral, Centro Hospitalar Universitário Lisboa Central/Universidade Nova de Lisboa, Lisbon, Portugal), Federica Gandolfo (Department of Geriatric Care, Orthogeriatrics and Rehabilitation, Galliera Hospital, Genoa, Italy), Sara Garaboldi (Department of Geriatric Care, Orthogeriatrics and Rehabilitation, Galliera Hospital, Genoa, Italy), Clarissa Musacchio (Department of Geriatric Care, Orthogeriatrics and Rehabilitation, Galliera Hospital, Genoa, Italy), Andrea Pilotto (Neurology Unit, Department of Clinical and Experimental Sciences, University of Brescia, Brescia, Italy), Lena Pickert (Ageing Clinical Research, Department II of Internal Medicine and Center for Molecular Medicine, University of Cologne, Cologne, Germany), Silvia Podestà (Department of Geriatric Care, Orthogeriatrics and Rehabilitation, Galliera Hospital, Genoa, Italy), Giovanni Ruotolo (Geriatrics Unit, “Pugliese Ciaccio” Hospital, Catanzaro, Italy), Katiuscia Sciolè (Infectious Disease Unit, Sanremo Hospital, ASL 1 Imperiese, Sanremo, Italy), Julia Schlotmann (Klinikum Oldenburg AöR, Oldenburg University, Oldenburg, Germany).
Funding
Open access funding provided by Università degli Studi di Palermo within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
Christine A.F. von Arnim received honoraria from serving on the scientific advisory boards of Biogen, Roche, Novo Nordisk, and Dr. Willmar Schwabe GmbH &Co. KG; funding for travel and speaker honoraria from Biogen, Roche Diagnostics AG, Novartis, Medical Tribune Verlagsgesellschaft GmbH, Landesvereinigung für Gesundheit und Akademie für Sozialmedizin Niedersachsen e. V. and Dr. Willmar Schwabe GmbH &Co. KG; and has received research support from Roche Diagnostics AG. Funding was received from Innovationsfond (Fund of the Federal Joint Committee, Gemeinsamer Bundesausschuss, G-BA Grants No. VF1_2016-201; 01NVF21010; 01VSF21019). Carlo Custodero, Nicola Veronese, Eva Topinkova, Helena Michalkova, Maria Cristina Polidori, Alberto Cella, Alfonso J. Cruz-Jentoft, Margherita Azzini, Heidi Gruner, Alberto Castagna, Giovanni Cenderello, Romina Custureri, Tania Zieschang, Alessandro Padovani, Elisabet Sanchez-Garcia, and Alberto Pilotto declare they have no conflicts of interest.
Funding
None.
Consent to participate
Informed consent was obtained from all individual participants included in the study or from their legal guardians.
Consent for publication
All the listed authors have read and approved the final manuscript and have agreed to publication.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval
The Ethical Committees of each of the centers formally approved the study.
Authors’ contributions
AP and NV conceived and designed the study. CC and NV wrote the original draft. NV performed the statistical analysis and takes responsibility for the accuracy of the data analysis. ET, HM, MCP, AC, ACJ, CAFvA, MA, HG, AC, GC, RC, TZ, AP, ESG contributed to data collection, assisted in data interpretation, and wrote the manuscript. AP critically revised the final manuscript.
Additional information
The members of the Study Group Investigators are listed in Acknowledgements.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Custodero, C., Veronese, N., Topinkova, E. et al. The Role of Multidimensional Prognostic Index to Identify Hospitalized Older Adults with COVID-19 Who Can Benefit from Remdesivir Treatment: An Observational, Prospective, Multicenter Study. Drugs Aging 40, 643–651 (2023). https://doi.org/10.1007/s40266-023-01036-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-023-01036-2