Abstract
Background and Objective
Cholinesterase inhibitors (ChEIs) are used as first-line pharmacotherapy to manage dementia. However, there are limited data regarding their relative safety. This study evaluated the risk of serious adverse events (SAEs) associated with individual ChEIs in older adults with dementia and also examined sex-based and dose-based effects on this risk.
Methods
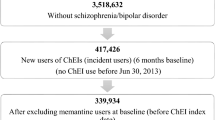
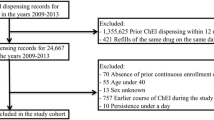
This was a retrospective cohort study using 2013–2015 US Medicare claims data involving Parts A, B, and D. Patients aged ≥ 65 years with a dementia diagnosis and incident use of the ChEIs, namely donepezil, galantamine, or rivastigmine, were included. The primary outcome of interest was SAEs defined as emergency department visits, inpatient hospitalizations, or death within 6 months of ChEI initiation. Multivariable Cox proportional hazards regression with propensity score (PS) as a covariate and inverse probability of treatment weighting generated using generalized boosted models was used to assess the risk of SAEs across individual ChEIs.
Results
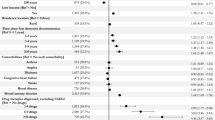
The study included 767,684 older adults with dementia who were incident new users of ChEIs (donepezil 79.42%, rivastigmine 17.67%, galantamine 2.91%). SAEs were observed in 15.5% of the cohort within 6 months of ChEI prescription. Cox regression model with PS as covariate found that patients prescribed rivastigmine (adjusted hazard ratio [aHR] 1.12; 95% CI 1.03–1.33) and galantamine (aHR 1.51; 95% CI 1.24–1.84) were at increased risk of SAEs compared with patients on donepezil. Stratified analyses revealed that rivastigmine was associated with an 18% increased risk for SAEs in females (aHR 1.18; 95% CI 1.06–1.31), and galantamine was associated with a 71% increased risk in males (aHR 1.71; 95% CI 1.17–2.51) compared with donepezil. High and recommended index doses of rivastigmine and galantamine were associated with an increased risk of SAEs compared with donepezil. The findings were consistent in sensitivity analyses.
Conclusion
The study found that the risk of SAEs varied across individual ChEIs, with sex and dose moderating these effects. Therefore, these moderating effects should be carefully considered in personalizing dementia care.



Similar content being viewed by others
References
2021 Alzheimer's disease facts and figures. Alzheimers Dement. 2021;17(3):327–406.
Kaduszkiewicz H, Zimmermann T, Beck-Bornholdt HP, van den Bussche H. Cholinesterase inhibitors for patients with Alzheimer’s disease: systematic review of randomised clinical trials. BMJ. 2005;331(7512):321–7.
Koller D, Hua T, Bynum JP. Treatment patterns with antidementia drugs in the United States: medicare cohort study. J Am Geriatr Soc. 2016;64(8):1540–8.
Suh DC, Arcona S, Thomas SK, et al. Risk of antipsychotic drug use in patients with Alzheimer’s disease treated with rivastigmine. Drugs Aging. 2004;21(6):395–403.
Scharre DW, Vekeman F, Lefebvre P, Mody-Patel N, Kahler KH, Duh MS. Use of antipsychotic drugs in patients with Alzheimer’s disease treated with rivastigmine versus donepezil: a retrospective, parallel-cohort, hypothesis-generating study. Drugs Aging. 2010;27(11):903–13.
Knight R, Khondoker M, Magill N, Stewart R, Landau S. A systematic review and meta-analysis of the effectiveness of acetylcholinesterase inhibitors and memantine in treating the cognitive symptoms of dementia. Dement Geriatr Cogn Disord. 2018;45(3–4):131–51.
Matsunaga S, Fujishiro H, Takechi H. Efficacy and safety of cholinesterase inhibitors for mild cognitive impairment: a systematic review and meta-analysis. J Alzheimers Dis. 2019;71(2):513–23.
Kavirajan H, Schneider LS. Efficacy and adverse effects of cholinesterase inhibitors and memantine in vascular dementia: a meta-analysis of randomised controlled trials. Lancet Neurol. 2007;6(9):782–92.
Rochon PA, Gruneir A, Gill SS, et al. Initial cholinesterase inhibitor therapy dose and serious events in older women and men. J Am Geriatr Soc. 2018;66(9):1692–9.
Gill SS, Anderson GM, Fischer HD, et al. Syncope and its consequences in patients with dementia receiving cholinesterase inhibitors: a population-based cohort study. Arch Intern Med. 2009;169(9):867–73.
Gill SS, Mamdani M, Naglie G, et al. A prescribing cascade involving cholinesterase inhibitors and anticholinergic drugs. Arch Intern Med. 2005;165(7):808–13.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509.
Kim HT. Cumulative incidence in competing risks data and competing risks regression analysis. Clin Cancer Res. 2007;13(2 Pt 1):559–65.
Edwards K, Royall D, Hershey L, et al. Efficacy and safety of galantamine in patients with dementia with Lewy bodies: a 24-week open-label study. Dement Geriatr Cogn Disord. 2007;23(6):401–5.
Emre M, Poewe W, De Deyn PP, et al. Long-term safety of rivastigmine in parkinson disease dementia: an open-label, randomized study. Clin Neuropharmacol. 2014;37(1):9–16.
Barosso G. How to identify hospital claims for emergency room visits in the Medicare claims data. 2015. In:2018.
Management: ICoHCSD, Reporting. DaSfE. 994 (online). Available at http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/ Guidelines/Efficacy/E2A/Step4/E2A_Guideline.pdf. Accessed June 12, 2021.
Arnegard ME, Whitten LA, Hunter C, Clayton JA. Sex as a biological variable: a 5-year progress report and call to action. J Womens Health (Larchmt). 2020;29(6):858–64.
Semla TP, Beizer JL, Higbee MD. Geriatric dosage handbook: Including monitoring, clinical recommendations, and OBRA guidelines. Lexi-Comp. 2009;2:2.
Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. 1973;51(1):95–124.
Masurkar PP, Chatterjee S, Sherer JT, Aparasu RR. Antimuscarinic cascade across individual cholinesterase inhibitors in older adults with dementia. Drugs Aging. 2021;38(7):593–602.
Chekani F, Holmes HM, Johnson ML, Chen H, Sherer JT, Aparasu RR. Use of atypical antipsychotics in long-term care residents with parkinson’s disease and comorbid depression. Drug Healthc Patient Saf. 2020;12:23–30.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10.
Kamble P, Chen H, Johnson ML, Bhatara V, Aparasu RR. Concurrent use of stimulants and second-generation antipsychotics among children with ADHD enrolled in Medicaid. Psychiatr Serv. 2015;66(4):404–10.
Williams JW, Plassman BL, Burke J, Benjamin S. Preventing Alzheimer’s disease and cognitive decline. Evid Rep Technol Assess (Full Rep). 2010;193:1–727.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
Information® AD. American Society of Health-System Pharmacists Available at http://onlinestatref.com/document/cQfe8yqMRNqgSGqm4Qo8Qj (Accessed May 2021). 2019.
Kim DH, Patorno E, Pawar A, Lee H, Schneeweiss S, Glynn RJ. Measuring frailty in administrative claims data: comparative performance of four claims-based frailty measures in the US medicare data. J Gerontol A Biol Sci Med Sci. 2020;75(6):1120–5.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Boustani M, Campbell N, Munger S, Maidment I, Fox C. Impact of anticholinergics on the aging brain: a review and practical application. Aging Health. 2008;4(3):311–20.
Austin PC, Fine JP. Practical recommendations for reporting Fine-Gray model analyses for competing risk data. Stat Med. 2017;36(27):4391–400.
Gray RJ. A class of k-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16(3):1141–54.
Haushona N, Esterhuizen TM, Thabane L, Machekano R. An empirical comparison of time-to-event models to analyse a composite outcome in the presence of death as a competing risk. Contemp Clin Trials Commun. 2020;19: 100639.
Kohl M, Plischke M, Leffondré K, Heinze G. PSHREG: a SAS macro for proportional and nonproportional subdistribution hazards regression. Comput Methods Programs Biomed. 2015;118(2):218–33.
Spreeuwenberg MD, Bartak A, Croon MA, et al. The multiple propensity score as control for bias in the comparison of more than two treatment arms: an introduction from a case study in mental health. Med Care. 2010;48(2):166–74.
Chatterjee S, Chen H, Johnson ML, Aparasu RR. Comparative risk of cerebrovascular adverse events in community-dwelling older adults using risperidone, olanzapine and quetiapine: a multiple propensity score-adjusted retrospective cohort study. Drugs Aging. 2012;29(10):807–17.
Kwak C, Clayton-Matthews A. Multinomial logistic regression. Nurs Res. 2002;51(6):404–10.
Austin PC. An Introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424.
Armstrong K. Methods in comparative effectiveness research. J Clin Oncol. 2012;30(34):4208–14.
Brookhart MA, Wyss R, Layton JB, Sturmer T. Propensity score methods for confounding control in nonexperimental research. Circ Cardiovasc Qual Outcomes. 2013;6(5):604–11.
McCaffrey DF, Ridgeway G, Morral AR. Propensity score estimation with boosted regression for evaluating causal effects in observational studies. Psychol Methods. 2004;9(4):403–25.
Griffin BA, Stelzner C, Sanchez R, Cefalu M, McCaffrey DF. Toolkit for Weighting and Analysis of Nonequivalent Groups: A Tutorial on the TWANG Shiny Application for Three or More Treatment Groups. RAND Corporation; 2020.
Parikh RB, Manz C, Chivers C, et al. Machine learning approaches to predict 6-month mortality among patients with cancer. JAMA Netw Open. 2019;2(10): e1915997.
Desai RJ, Franklin JM. Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: a primer for practitioners. BMJ. 2019;367: l5657.
Parast L, McCaffrey DF, Burgette LF, et al. Optimizing variance-bias trade-off in the TWANG package for estimation of propensity scores. Health Serv Outcomes Res Method. 2017;17(3):175–97.
Dunkler D, Ploner M, Schemper M, Heinze G. Weighted Cox Regression Using the R Package coxphw. J Stat Softw. 2018;1(2):1–5.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the e-value. Ann Intern Med. 2017;167(4):268–74.
Di Santo SG, Prinelli F, Adorni F, Caltagirone C, Musicco M. A meta-analysis of the efficacy of donepezil, rivastigmine, galantamine, and memantine in relation to severity of Alzheimer’s disease. J Alzheimers Dis. 2013;35(2):349–61.
Tricco AC, Soobiah C, Berliner S, et al. Efficacy and safety of cognitive enhancers for patients with mild cognitive impairment: a systematic review and meta-analysis. CMAJ. 2013;185(16):1393–401.
Cummings J, Lefevre G, Small G, Appel-Dingemanse S. Pharmacokinetic rationale for the rivastigmine patch. Neurology. 2007;69(4 Suppl 1):S10-13.
Hansen RA, Gartlehner G, Webb AP, Morgan LC, Moore CG, Jonas DE. Efficacy and safety of donepezil, galantamine, and rivastigmine for the treatment of Alzheimer’s disease: a systematic review and meta-analysis. Clin Interv Aging. 2008;3(2):211–25.
Jhee SS, Shiovitz T, Hartman RD, et al. Centrally acting antiemetics mitigate nausea and vomiting in patients with Alzheimer’s disease who receive rivastigmine. Clin Neuropharmacol. 2002;25(2):122–3.
Alva G, Cummings JL, Galvin JE, Meng X, Velting DM. Skin reactions at the application site of rivastigmine patch (4.6 mg/24 h, 9.5 mg/24 h or 13.3 mg/24 h): a qualitative analysis of clinical studies in patients with Alzheimer’s disease. Int J Clin Pract. 2015;69(5):518–30.
Lilienfeld S. Galantamine–a novel cholinergic drug with a unique dual mode of action for the treatment of patients with Alzheimer’s disease. CNS Drug Rev. 2002;8(2):159–76.
Tricco AC, Vandervaart S, Soobiah C, et al. Efficacy of cognitive enhancers for Alzheimer’s disease: protocol for a systematic review and network meta-analysis. Syst Rev. 2012;1:31.
Field TS, Gurwitz JH, Avorn J, et al. Risk factors for adverse drug events among nursing home residents. Arch Intern Med. 2001;161(13):1629–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of Interest
Dr Aparasu has received research funding from Astellas Inc., Incyte Corp., Gilead and Novartis Inc. for projects unrelated to the current work. Prajakta P. Masurkar, Satabdi Chatterjee, Jeffrey T. Sherer, Hua Chen, and Michael L. Johnson declare no conflicts of interest for this article.
Ethical approval
This study was approved by the Institutional Review Board for the Protection of Human Subjects at the University of Houston under the exempt category (Exemption approval #STUDY00002792).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Author contributions
Masurkar and Aparasu had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: All authors. Acquisition of data: Masurkar and Aparasu. Analysis of data: Masurkar. Interpretation of data: All authors. Drafting of the manuscript: Masurkar. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Masurkar, Johnson, Aparasu. Administrative, technical, or material support, and study supervision: Aparasu.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Masurkar, P.P., Chatterjee, S., Sherer, J.T. et al. Risk of Serious Adverse Events Associated With Individual Cholinesterase Inhibitors Use in Older Adults With Dementia: A Population-Based Cohort Study. Drugs Aging 39, 453–465 (2022). https://doi.org/10.1007/s40266-022-00944-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-022-00944-z