Abstract
Background
Cholinesterase inhibitors (ChEIs) are prescribed to dementia patients despite their poor tolerance. Low tolerability potentially reduces persistence and adherence, while inducing switching between medications. Comparisons of these utilization measures contribute to knowledge of the relative tolerability of these medications.
Aim
The aim was to compare persistence, adherence, and switching between donepezil, galantamine, oral rivastigmine, and rivastigmine patch.
Methods
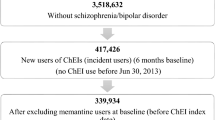
A population-based cohort study, using British Columbia claims data (2009–2013), assessed ChEI new users aged 40 and older. We conducted survival analysis to compare persistence and Poisson regression to estimate switching rates. Good adherence, defined as a medication possession ratio of ≥80%, was modeled using log-binomial regression. Analyses were adjusted using propensity scores.
Results
Patients on galantamine had longer mean persistence and better adherence compared with patients on donepezil, with a hazard ratio for discontinuation of 0.91 [95% confidence interval (CI) 0.87–0.96] and a relative risk for good adherence of 1.01 (95% CI 1.002–1.03). Rivastigmine was associated with the shortest mean persistence [3.6 months (95% CI 3.0–4.2) and 5.0 (95% CI 4.7–5.3) for oral and patch, respectively] and the highest mean switching rates. Comparing the two rivastigmine preparations, the patch was associated with decreased discontinuation compared with oral [hazard ratio 0.79 (95% CI 0.71–0.89)] and decreased switching [relative risk 0.63 (95% CI 0.46–0.87) during the first 6 months of treatment]. Paradoxically, the patch was also associated with poorer adherence [relative risk for good adherence 0.94 (95% CI 0.91–0.98)] than the oral formulation.
Conclusions
Based on estimates of persistence, adherence, and switching, galantamine was the best tolerated ChEI and rivastigmine the least.



Similar content being viewed by others
References
Raina P, Santaguida P, Ismaila A, Patterson C, Cowan D, Levine M, Booker L, Oremus M. Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline. Ann Intern Med. 2008; 148(5):379–397. doi:10.7326/0003-4819-148-5-200803040-00009.
National Institute for Clinical Excellence (NICE), UK. Donepezil, galantamine, rivastigmine and memantine for the treatment of Alzheimer’s disease. Technology appraisal guidance TA217. 2011. https://www.nice.org.uk/guidance/ta217 Accessed 11 Nov 2015.
Gauthier S, Patterson C, Chertkow H, Gordon M, Herrmann N, Rockwood K, Rosa-Neto P, Soucy JP. Recommendations of the 4th Canadian consensus conference on the diagnosis and treatment of dementia (CCCDTD4). Can Geriatr J. 2012;. doi:10.5770/cgj.15.49.
Birks J. Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database Syst Rev. 2006;. doi:10.1002/14651858.CD005593.
Hansen RA, Gartlehner G, Webb AP, Morgan LC, Moore CG, Jonas DE. Efficacy and safety of donepezil, galantamine, and rivastigmine for the treatment of Alzheimer’s disease: a systematic review and meta-analysis. Clin Interv Aging. 2008;3(2):211–25.
Bond M, Rogers G, Peters J, Anderson R, Hoyle M, Miners A, Moxham T, Davis S, Thokala P, Wailoo A, Jeffreys M, Hyde C. The effectiveness and cost-effectiveness of donepezil, galantamine, rivastigmine and memantine for the treatment of Alzheimer’s disease (review of Technology Appraisal No. 111): a systematic review and economic model. Health Technol Assess. 2012;. doi:10.3310/hta16210.
Tan CC, Yu JT, Wang HF, Tan MS, Meng XF, Wang C, Jiang T, Zhu XC, Tan L. Efficacy and safety of donepezil, galantamine, rivastigmine, and memantine for the treatment of Alzheimer’s disease: a systematic review and meta-analysis. J Alzheimers Dis. 2014;. doi:10.3233/JAD-132690.
Kobayashi H, Ohnishi T, Nakagawa R, Yoshizawa K. The comparative efficacy and safety of cholinesterase inhibitors in patients with mild-to-moderate Alzheimer’s disease: a Bayesian network meta-analysis. Int J Geriatr Psychiatry. 2016;. doi:10.1002/gps.4405.
Colovic MB, Krstic DZ, Lazarevic-Pasti TD, Bondzic AM, Vasic VM. Acetylcholinesterase inhibitors: pharmacology and toxicology. Curr Neuropharmacol. 2013;. doi:10.2174/1570159X11311030006.
Inglis F. The tolerability and safety of cholinesterase inhibitors in the treatment of dementia. Int J Clin Pract Suppl. 2002;127:45–63.
Hogan DB. Long-term efficacy and toxicity of cholinesterase inhibitors in the treatment of Alzheimer disease. Can J Psychiatry. 2014;59(12):618–23.
Ali TB, Schleret TR, Reilly BM, Chen WY, Abagyan R. Adverse effects of cholinesterase inhibitors in dementia, according to the pharmacovigilance databases of the United-States and Canada. PLoS One. 2015;. doi:10.1371/journal.pone.0144337.
Leinonen A, Koponen M, Hartikainen S. Systematic review: representativeness of participants in RCTs of acetylcholinesterase inhibitors. PLoS One. 2015;. doi:10.1371/journal.pone.0124500.
Aikens JE, NeaseDE, Jr, Nau DP, Klinkman MS, Schwenk TL. Adherence to maintenance-phase antidepressant medication as a function of patient beliefs about medication. Ann Fam Med. 2005; doi:10.1370/afm.238
Cassell B, Gyawali CP, Kushnir VM, Gott BM, Nix BD, Sayuk GS. Beliefs about GI medications and adherence to pharmacotherapy in functional GI disorder outpatients. Am J Gastroenterol. 2015;. doi:10.1038/ajg.2015.132.
Olazaran J, Navarro E, Rojo JM. Persistence of cholinesterase inhibitor treatment in dementia: insights from a naturalistic study. Dement Geriatr Cogn Dis Extra. 2013;. doi:10.1159/000345279.
Maxwell CJ, Stock K, Seitz D, Herrmann N. Persistence and adherence with dementia pharmacotherapy: relevance of patient, provider, and system factors. Can J Psychiatry. 2014;59(12):624–31.
Herrmann N, Gill SS, Bell CM, Anderson GM, Bronskill SE, Shulman KI, Fischer HD, Sykora K, Shi HS, Rochon PA. A population-based study of cholinesterase inhibitor use for dementia. J Am Geriatr Soc. 2007;. doi:10.1111/j.1532-5415.2007.01377.x.
Mucha L, Wang SS, Cuffel B, McRae T, Mark TL, del Valle M. Comparison of cholinesterase inhibitor utilization patterns and associated health care costs in Alzheimer’s disease. J Manag Care Spec Pharm. 2008;14(5):451–61.
Haider B, Schmidt R, Schweiger C, Forstner T, Labek A, Lampl C. Medication adherence in patients with dementia: an Austrian cohort study. Alzheimer Dis Assoc Disord. 2014;. doi:10.1097/WAD.0000000000000006.
Gardette V, Lapeyre-Mestre M, Piau A, Gallini A, Cantet C, Montastruc J, Vellas B, Andrieu S. A 2-year prospective cohort study of antidementia drug non-persistency in mild-to-moderate Alzheimer’s disease in Europe: predictors of discontinuation and switch in the ICTUS study. CNS Drugs. 2014;. doi:10.1007/s40263-013-0133-3.
Ahn SH, Choi NK, Kim YJ, Seong JM, Shin JY, Jung SY, Park BJ. Drug persistency of cholinesterase inhibitors for patients with dementia of Alzheimer type in Korea. Arch Pharm Res. 2015;. doi:10.1007/s12272-014-0500-8.
Chappell NL, Beattie BL, Hsiung JYR, Dormuth C, Maclure M. Alzheimer’s drug therapy initiative (ADTI): research report. 2015. http://www2.gov.bc.ca.ezproxy.library.ubc.ca/assets/gov/health/health-drug-coverage/pharmacare/adtiresearchstudiesuvic.pdf. Accessed 19 July 2016.
Fisher A, Carney G, Basset K, Chappell NL. Cholinesterase inhibitor utilization: the impact of provincial drug policy on discontinuation. Value Health. 2016;. doi:10.1016/j.jval.2016.03.1832.
British Columbia Ministry of Health website. How your coverage is calculated in Fair PharmaCare plan. 2009. http://www2.gov.bc.ca.ezproxy.library.ubc.ca/gov/content/health/health-drug-coverage/pharmacare-for-bc-residents/who-we-cover/fair-pharmacare-plan/how-your-coverage-is-calculated. Accessed 21 Aug 2015.
Caetano PA, Lam JM, Morgan SG. Toward a standard definition and measurement of persistence with drug therapy: examples from research on statin and antihypertensive utilization. Clin Ther. 2006;. doi:10.1016/j.clinthera.2006.09.021.
Peterson AM, Nau DP, Cramer JA, Benner J, Gwadry-Sridhar F, Nichol M. A checklist for medication compliance and persistence studies using retrospective databases. Value Health. 2007;. doi:10.1111/j.1524-4733.2006.00139.x.
Steiner JF, Prochazka AV. The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol. 1997;. doi:10.1016/S0895-4356(96)00268-5.
Schwalbe O, Scheerans C, Freiberg I, Schmidt-Pokrzywniak A, Stang A, Kloft C. Compliance assessment of ambulatory Alzheimer patients to aid therapeutic decisions by healthcare professionals. BMC Health Serv Res. 2010;. doi:10.1186/1472-6963-10-232.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;. doi:10.1093/biomet/70.1.41.
British Columbia Ministry of Health. Premiums. 2015. http://www2.gov.bc.ca.ezproxy.library.ubc.ca/gov/topic.page?id=59DDCB8DB15241D899168C65EE095393. Accessed 19 June 2015.
British Columbia Ministry of Health. Who we cover. 2015. http://www2.gov.bc.ca.ezproxy.library.ubc.ca/gov/topic.page?id=B454413672454141871930584C01A693. Accessed 19 June 2015.
Taylor DH Jr, Fillenbaum GG, Ezell ME. The accuracy of Medicare claims data in identifying Alzheimer’s disease. J Clin Epidemiol. 2002;55(9):929–37.
Taylor DH Jr, Sloan FA, Doraiswamy PM. Marked increase in Alzheimer’s disease identified in Medicare claims records between 1991 and 1999. J Gerontol A Biol Sci Med Sci. 2004;59(7):762–6.
Sturmer T, Rothman KJ, Avorn J, Glynn RJ. Treatment effects in the presence of unmeasured confounding: dealing with observations in the tails of the propensity score distribution—a simulation study. Am J Epidemiol. 2010;. doi:10.1093/aje/kwq198.
Southern DA, Faris PD, Brant R, Galbraith PD, Norris CM, Knudtson ML, Ghali WA, APPROACH Investigators. Kaplan–Meier methods yielded misleading results in competing risk scenarios. J Clin Epidemiol. 2006;. doi:10.1016/j.jclinepi.2006.07.002.
Satagopan JM, Ben-Porat L, Berwick M, Robson M, Kutler D, Auerbach AD. A note on competing risks in survival data analysis. Br J Cancer. 2004;. doi:10.1038/sj.bjc.6602102.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;. doi:10.2307/2670170.
Lunn M, McNeil D. Applying Cox regression to competing risks. Biometrics. 1995;. doi:10.2307/2532940.
Lambert PC, Dickman PW, Nelson CP, Royston P. Estimating the crude probability of death due to cancer and other causes using relative survival models. Stat Med. 2010;. doi:10.1002/sim.3762.
Grams ME, Coresh J, Segev DL, Kucirka LM, Tighiouart H, Sarnak MJ. Vascular disease, ESRD, and death: interpreting competing risk analyses. Clin J Am Soc Nephrol. 2012;. doi:10.2215/CJN.03460412.
Andersen PK, Geskus RB, de Witte T, Putter H. Competing risks in epidemiology: possibilities and pitfalls. Int J Epidemiol. 2012;. doi:10.1093/ije/dyr213.
Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;. doi:10.1093/aje/kwf215.
Fisher A, Bassett K, Goel G, Stanely D, Brookhart MA, Freeman HJ, Wright JM, Dormuth CR. Heterogeneity in comparisons of discontinuation of tumor necrosis factor antagonists in rheumatoid arthritis—a meta-analysis. PLoS One. 2016;. doi:10.1371/journal.pone.0168005.
Massoud F, Dorais M, Charbonneau C, Lescrauwaet B, Boucher J, LeLorier J. Drug utilization review of cholinesterase inhibitors in Quebec. Can J Neurol Sci. 2008;. doi:10.1017/S0317167100009215.
Herrmann N, Binder C, Dalziel W, Smyth S, Camacho F. Persistence with cholinesterase inhibitor therapy for dementia: an observational administrative health database study. Drugs Aging. 2009;. doi:10.2165/00002512-200926050-00004.
Gadzhanova S, Roughead L, MacKson J. Anticholinesterase duration in the Australian veteran population. Aust N Z J Psychiatry. 2010;. doi:10.3109/00048670903555104.
Brewer L, Bennett K, McGreevy C, Williams D. A population-based study of dosing and persistence with anti-dementia medications. Eur J Clin Pharmacol. 2013;. doi:10.1007/s00228-013-1483-y.
Taipale H, Tanskanen A, Koponen M, Tolppanen AM, Tiihonen J, Hartikainen S. Antidementia drug use among community-dwelling individuals with Alzheimer’s disease in Finland: a nationwide register-based study. Int Clin Psychopharmacol. 2014;. doi:10.1097/YIC.0000000000000032.
Abughosh SM, Kogut SJ. Comparison of persistence rates of acetylcholine-esterase inhibitors in a state Medicaid program. Patient Prefer Adher. 2008;2:79–85.
Suh DC, Thomas SK, Valiyeva E, Arcona S, Vo L. Drug persistency of two cholinesterase inhibitors: rivastigmine versus donepezil in elderly patients with Alzheimer’s disease. Drugs Aging. 2005;. doi:10.2165/00002512-200522080-00006.
Singh G, Thomas SK, Arcona S, Lingala V, Mithal A. Treatment persistency with rivastigmine and donepezil in a large state Medicaid program. J Am Geriatr Soc. 2005;. doi:10.1111/j.1532-5415.2005.53384_9.x.
Mauskopf JA, Paramore C, Lee WC, Snyder EH. Drug persistency patterns for patients treated with rivastigmine or donepezil in usual care settings. J Manag Care Pharm. 2005;. doi:10.18553/jmcp.2005.11.3.231.
Weinstock M. Selectivity of cholinesterase inhibition: clinical implications for the treatment of Alzheimer’s disease. CNS Drugs. 1999;. doi:10.2165/00023210-199912040-00005.
Bishara D, Sauer J, Taylor D. The pharmacological management of Alzheimer’s disease. Prog Neurol Psychiatry. 2015;. doi:10.1002/pnp.387.
Humbert IA, McLaren DG, Kosmatka K, Fitzgerald M, Johnson S, Porcaro E, Kays S, Umoh EO, Robbins J. Early deficits in cortical control of swallowing in Alzheimer’s disease. J Alzheimers Dis. 2010;. doi:10.3233/JAD-2010-1316.
Fernandez-Nebro A, Irigoyen MV, Urena I, Belmonte-Lopez MA, Coret V, Jimenez-Nunez FG, Diaz-Cordoves G, Lopez-Lasanta MA, Ponce A, Rodriguez-Perez M, Calero E, Gonzalez-Santos P. Effectiveness, predictive response factors, and safety of anti-tumor necrosis factor (TNF) therapies in anti-TNF-naive rheumatoid arthritis. J Rheumatol. 2007;34(12):2334–42.
Blesa Gonzalez R, Boada Rovira M, Martinez Parra C, Gil-Saladie D, Almagro CA, Gobartt Vazquez AL, en representacion del grupo de investigadores del estudio kAPA. Evaluation of the convenience of changing the rivastigmine administration route in patients with Alzheimer disease. Neurologia. 2011;. doi:10.1016/j.nrl.2010.10.007.
Hausner L, Sartorius A, Froelich L. The treatment compliance with rivastigmine patch in clinical practice versus trial data: a case series. Alzheimers Dement. 2009;. doi:10.1016/j.jalz.2009.04.263.
Lefevre G, Sedek G, Jhee SS, Leibowitz MT, Huang HL, Enz A, Maton S, Ereshefsky L, Pommier F, Schmidli H, Appel-Dingemanse S. Pharmacokinetics and pharmacodynamics of the novel daily rivastigmine transdermal patch compared with twice-daily capsules in Alzheimer’s disease patients. Clin Pharmacol Ther. 2008; 83(1):106–114.doi:10.1038/sj.clpt.6100242
Davis SA, Feldman SR. Using Hawthorne effects to improve adherence in clinical practice: lessons from clinical trials. JAMA Dermatol. 2013;. doi:10.1001/jamadermatol.2013.2843.
McGinnis B, Olson KL, Magid D, Bayliss E, Korner EJ, Brand DW, Steiner JF. Factors related to adherence to statin therapy. Ann Pharmacother. 2007; 41(11):1805–1811.doi:10.1345/aph.1K209.
Kim DH, Schneeweiss S. Measuring frailty using claims data for pharmacoepidemiologic studies of mortality in older adults: evidence and recommendations. Pharmacoepidemiol Drug Saf. 2014;. doi:10.1002/pds.3674.
Bhardwaja B, Carroll N, Korner E, Nair KV. Impact of prescription benefit coverage limits on sevelamer hydrochloride adherence for patients with ESRD. Am Health Drug Benefits. 2009;2(6):242–50.
Kaisaeng N, Harpe SE, Carroll NV. Out-of-pocket costs and oral cancer medication discontinuation in the elderly. J Manag Care Pharm. 2014;20(7):669–75.
Park H, Rascati KL, Lawson KA, Barner JC, Richards KM, Malone DC. Adherence and persistence to prescribed medication therapy among Medicare part D beneficiaries on dialysis: comparisons of benefit type and benefit phase. J Manag Care Pharm. 2014;. doi:10.18553/jmcp.2014.20.8.862.
Winblad B, Kawata AK, Beusterien KM, Thomas SK, Wimo A, Lane R, Fillit H, Blesa R. Caregiver preference for rivastigmine patch relative to capsules for treatment of probable Alzheimer’s disease. Int J Geriatr Psychiatry. 2007;. doi:10.1002/gps.1806.
Fisher A, Bassett K, Wright JM, Brookhart MA, Freeman HJ, Dormuth CR. Prescriber preference for a particular tumour necrosis factor antagonist drug and treatment discontinuation: population-based cohort. BMJ Open. 2014;. doi:10.1136/bmjopen-2014-005532.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The study is funded by the Pharmaceutical Services Division, Ministry of Health, Provincial Government of British Columbia as part of the Alzheimer’s Drug Therapy Initiative (ADTI) for the purpose of developing evidence for the use of ChEI treatment in the community. All inferences, opinions, and conclusions drawn in this publication are those of Anat Fisher, Greg Carney, Ken Bassett, and Colin R. Dormuth, and do not reflect the opinions or policies of the BC Ministry of Health.
Conflicts of interest
Anat Fisher, Greg Carney, Ken Bassett, and Colin R. Dormuth declare that they have no conflicts of interest directly relevant to the content of this study.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Clinical Research Ethics Board, the University of British Columbia, and the Human Research Ethics Board, the University of Victoria. For this type of study formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fisher, A., Carney, G., Bassett, K. et al. Tolerability of Cholinesterase Inhibitors: A Population-Based Study of Persistence, Adherence, and Switching. Drugs Aging 34, 221–231 (2017). https://doi.org/10.1007/s40266-017-0438-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-017-0438-x