Abstract
Objectives
This study investigated the extent of, and patient-related characteristics for, non-persistence with antiplatelet therapy during follow-up in elderly patients after their first ischaemic non-cardioembolic stroke.
Methods
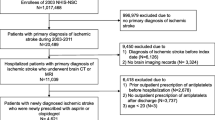
A database of the largest health insurance provider in the Slovak Republic was used to assemble the study cohort of 4319 patients (56.8 % were women) aged ≥65 years in whom antiplatelet therapy was initiated following a hospital-based diagnosis of stroke during the period 1 January 2010 to 31 December 2010. Patients were followed for 3 years from the date on which the first prescription of antiplatelet medication was recorded. Patients with a 6-month treatment gap without antiplatelet medication prescription were designated as non-persistent, and the Cox proportional hazards model was used to identify predictors of non-persistence.
Results
At the end of the 3-year follow-up period, 1184 (27.4 %) patients were considered non-persistent with antiplatelet medication. In 1244 (28.8 %) patients, a switch in the use of a particular antiplatelet drug was registered during this follow-up period. Female sex (hazard ratio [HR] 1.25) was associated with increased risk of non-persistence. In contrast, factors associated with lower probability of non-persistence were age ≥75 years (HR 0.72), switch in antiplatelet medication use (HR 0.76), diabetes mellitus (HR 0.81), dementia (HR 0.69) and epilepsy (HR 0.69).
Conclusions
Our results suggest that women, patients aged <75 years, and patients without certain comorbid conditions may need improved assistance in secondary prevention management after an ischaemic stroke.

Similar content being viewed by others
References
Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe: epidemiological update. Eur Heart J. 2013;34(39):3028–34.
Jorgensen H, Nakayama H, Reith J, Raaschou H, Olsen T. Stroke recurrence: predictors, severity, and prognosis. The Copenhagen Stroke Study. Neurology. 1997;48(4):891–5.
Mozaffarian D, Benjamin EJ, Go AS, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
Arnan MK, Burke GL, Bushnell C. Secondary prevention of stroke in the elderly: focus on drug therapy. Drugs Aging. 2014;31(10):721–30.
The European Stroke Organization (ESO) Executive Committee, ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008;25(5):457–507.
Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–236.
Grau AJ, Weimar C, Buggle F, et al. Risk factors, outcome, and treatment in subtypes of ischemic stroke: the German stroke data bank. Stroke. 2001;32(11):2559–66.
Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–7.
Dezii CM. Persistence with drug therapy: a practical approach using administrative claims data. Manag Care. 2001;10(2):42–5.
McKenzie SJ, McLaughlin D, Clark J, Doi SAR. The Burden of non-adherence to cardiovascular medications among the aging population in Australia: a meta-analysis. Drugs Aging. 2015;32(3):217–25.
Mukhtar O, Weinman J, Jackson SHD. Intentional non-adherence to medications by older adults. Drugs Aging. 2014;31(3):149–57.
Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705.
Burke JP, Sander S, Shah H, Zarotsky, Henk H. Impact of persistence with antiplatelet therapy on recurrent ischemic stroke and predictors of nonpersistence among ischemic stroke survivors. Curr Med Res Opin. 2010;26(5):1023–30.
Bushnell CD, Olson DM, Zhao X, et al. Secondary preventive medication persistence and adherence 1 year after stroke. Neurology. 2011;77(12):1182–90.
Flynn RW, MacDonald TM, Murray GD, MacWalter RS, Doney AS. Persistence, adherence and outcomes with antiplatelet regimens following cerebral infarction in the Tayside Stroke Cohort. Cerebrovasc Dis. 2012;33(2):190–7.
Glader EL, Sjölander M, Eriksson M, Lundberg M. Persistent use of secondary preventive drugs declines rapidly during the first 2 years after stroke. Stroke. 2010;41(2):397–401.
Ji R, Liu G, Shen H, et al. Persistence of secondary prevention medications after acute ischemic stroke or transient ischemic attack in Chinese population: data from China National Stroke Registry. Neurol Res. 2013;35(1):29–36.
Lummis HL, Sketris IS, Gubitz GJ, Joffres MR, Flowerdew GJ. Medication persistence rates and factors associated with persistence in patients following stroke: a cohort study. BMC Neurol. 2008;8:25.
Østergaard K, Hallas J, Bak S, Christensen R, Gaist D. Long-term use of antiplatelet drugs by stroke patients: a follow-up study based on prescription register data. Eur J Clin Pharmacol. 2012;68(12):1631–7.
Health Statistics Yearbook of the Slovak Republic 2013. Available at: http://www.nczisk.sk/en/Publications/Edition_Health_Statistics_Yearbooks/Pages/default.aspx. Accessed 12 Oct 2015.
Casper ML, Nwaise IA, Croft JB, Nilasena DS. Atlas of stroke hospitalizations among medicare beneficiaries. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2008.
World Health Organization. International statistical classification of diseases and related health problems. 10th revision. Geneva: World Health Organization; 1992. p. 191.
Williamson J, Chopin JM. Adverse reactions to prescribed drugs in the elderly: a multicentre investigation. Age Ageing. 1980;9(2):73–80.
World Health Organization Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment, 2015. Oslo: World Health Organization; 2014.
The secondary prevention of ischemic strokes. The guideline of the scientific society [in Slovak]. Available at: http://snes.sk/cms/wp-content/uploads/Usmernenie-odb-spol_sek_prevencia_iCMP.pdf. Accessed 25 Feb 2016.
Newman SC. Biostatistical methods in epidemiology. Chichester: Wiley; 2001. p. 382.
Bushnell CD, Zimmer LO, Pan W, Adherence Evaluation After Ischemic Stroke-Longitudinal Investigators, et al. Persistence with stroke prevention medications 3 months after hospitalization. Arch Neurol. 2010;67(12):1456–63.
Erkens JA, Panneman MM, Klungel OH, van den Boom G, Prescott MF, Herings RM. Differences in antihypertensive drug persistence associated with drug class and gender: a PHARMO study. Pharmacoepidemiol Drug Saf. 2005;14(11):795–803.
White RD. Patient empowerment and optimal glycemic control. Curr Med Res Opin. 2012;28(6):979–89.
Shaya FT, El Khoury AC, Mullins CD, et al. Drug therapy persistence and stroke recurrence. Am J Manag Care. 2006;12(6):313–9.
O’Shea MP, Teeling M, Bennett K. Regional variation in medication-taking behaviour of new users of oral anti-hyperglycaemic therapy in Ireland. Ir J Med Sci. 2015;184(2):403–10.
Helin-Salmivaara A, Lavikainen P, Ruokoniemi P, Korhonen M, Huupponen R. Persistence with statin therapy in diabetic and non-diabetic persons: a nation-wide register study in 1995–2005 in Finland. Diabetes Res Clin Pract. 2009;84(1):e9–11.
Johnston S, Janning SW, Haas GP, et al. Comparative persistence and adherence to overactive bladder medications in patients with and without diabetes. Int J Clin Pract. 2012;66(11):1042–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by grants from the Scientific Grant Agency of the Ministry of Education, Science, Research and Sport of the Slovak Republic (VEGA 1/0886/14 and VEGA 1/0939/14). The providers of these Grants played no role in the design, methods, data collection, analysis and interpretation of the data, preparation of the paper or the decision to submit the manuscript.
Conflict of interest
Martin Wawruch, Dusan Zatko, Gejza Wimmer Jr, Jan Luha, Lenka Kuzelova, Peter Kukumberg, Jan Murin, Adam Hloska, Tomas Tesar, Zoltan Kallay and Rashmi Shah declare that they have no conflicts of interest.
Ethical approval
Under applicable legal instruments of our country, the study did not require the approval of an Ethical Committee. The laws and rules of personal data confidentiality were fully complied with.
Rights and permissions
About this article
Cite this article
Wawruch, M., Zatko, D., Wimmer, G. et al. Factors Influencing Non-Persistence with Antiplatelet Medications in Elderly Patients After Ischaemic Stroke. Drugs Aging 33, 365–373 (2016). https://doi.org/10.1007/s40266-016-0365-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-016-0365-2