Abstract
Purpose
Treatment with antiplatelet drugs is a key element of secondary stroke prevention. We investigated long-term antiplatelet drug use in stroke patients with a focus on non-persistence.
Methods
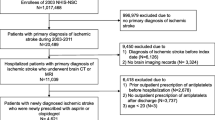
Population-based prescription register data were used to determine antiplatelet drug use in a cohort of stroke patients discharged from a Danish neurology department. The antiplatelet drugs comprised acetylsalicylic acid (ASA), clopidogrel and dipyridamole (if combined with ASA use). Non-persistence was defined as failure to present a prescription for antiplatelet drugs within 180 days after the dosage of a previous prescription had run out, or within 180 days after discharge. Cox regression was used to identify risk factors for non-persistence.
Results
The cohort comprised 503 patients with ischaemic stroke discharged in 1999–2001. During follow-up (median 2.8 years, interquartile range 0.8–7.8 years), 486 of the subjects presented prescriptions for antiplatelets. Most subjects used a dual regimen of ASA and dipyridamole (N = 320). Of 110 non-persistent subjects in this group, 64 stopped using ASA, but continued to use dipyridamole in monotherapy. Overall, 181 patients (36 %) were non-persistent. Stroke severity was inversely associated with the risk of non-persistence [NIHSS score on admission 0–3 (reference); 4–6: hazard risk (HR) 0.87, 95 % confidence interval (CI) 0.61–1.25; 7+: HR 0.47, 95 % CI 0.29–0.74].
Conclusions
Long-term non-persistence with antiplatelet treatment was high and more pronounced in our patients with less severe stroke. Our findings on the use of ASA and dipyridamole indicate that non-persistence may in part be amenable to simple intervention measures.


Similar content being viewed by others
References
Sappok T, Faustich A, Stuckert E, Kruck H, Marx P, Koennecke H-C (2001) Compliance with secondary prevention of ischemic stroke. Stroke 32:1884–1889
Hamann GF, Weimar C, Glahn J et al (2003) Adherence to secondary stroke prevention strategies—results from the German Stroke Data Bank. Cerebrovasc Dis 15:282–288
Burke JP, Sander S, Shah H et al (2010) Impact of persistence with antiplatelet therapy on recurrent ischemic stroke and predictors of nonpersistence among ischemic stroke survivors. Curr Med Res Opin 26:1023–1030
Glader E-L, Sjölander M, Eriksson M, Lundberg M (2010) Persistent use of secondary preventive drugs decline rapidly during the first 2 years after stroke. Stroke 41:397–401
Bushnell CD, Olson DM, Zhao X et al (2011) Secondary preventive medication persistence and adherence 1 year after stroke. Neurology 77:1182–1190
Bak S, Sindrup SH, Alslev T et al (2002) Cessation of smoking after first-ever stroke—a follow-up study. Stroke 33:2263–2269
World Health Organisation (1989) Recommendations on stroke prevention, diagnosis and therapy. Stroke 20:1407–1431
Goldstein LB, Bertels C, Davis JN (1989) Interrater reliability of the NIH Stroke Scale. Arch Neurol 46:660–662
Gaist D, Sørensen HT, Hallas J (1997) The Danish prescription registries. Dan Med Bull 44:445–448
WHO Collaborating Centre for Drug Statistics Methodology (2000) Anatomical therapeutic chemical (ATC) classification index with defined daily doses (DDDs). World Health Organization, Oslo
Pedersen CB, Gøtzche H, Møller JØ et al (2006) The Danish Civil Registration system—a cohort of 8 million people. Dan Med Bull 53:441–449
Andrade SE, Kahler KH, Frech F et al (2006) Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf 15:565–574
StataCorp (2009) Stata: release 11. Statistical software. StataCorp LP, College Station
www.medstat.dk/en (Medicine Sales in Denmark)
Referenceprogram for behandling af patienter med apopleksi (2009) Danish Health Board, 3rd edn. Available at: http://www.sst.dk/publ/Publ2010/Andre/ReferenceprogramApopleksiDSFA.pdf
Nielsen LH, Løkkegaard E, Andreasen AH, Andersen Hundrup Y, Keiding N (2009) Estimating the effect of current, previous, and never use of drugs in studies based on prescription registries. Pharmacoepidemiol Drug Saf 18:147–153
Caetano PA, Lam JMC, Morgan SG (2006) Toward a standard definition and measurement of persistence with drug therapy: examples from research on statin and antihypertensive utilization. Clin Ther 28:1411–1424
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Østergaard, K., Hallas, J., Bak, S. et al. Long-term use of antiplatelet drugs by stroke patients: a follow-up study based on prescription register data. Eur J Clin Pharmacol 68, 1631–1637 (2012). https://doi.org/10.1007/s00228-012-1293-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-012-1293-7