Abstract
Lumasiran (Oxlumo®), a first-in-class synthetic, double-stranded, ribonucleic acid (RNA) interference molecule targeting glycolate oxidase through silencing HAO1 mRNA, is approved in several countries for patients of any age and stage of kidney function with primary hyperoxaluria type 1 (PH1). Approval was based on results from the phase III ILLUMINATE trials. In the double-blind, placebo-controlled, ILLUMINATE-A trial, subcutaneous lumasiran was significantly more effective than placebo in reducing 24-h urinary oxalate excretion in patients aged ≥ 6 years with PH1; this effect was sustained for ≥ 36 months in ongoing longer-term analyses. In the single-arm ILLUMINATE-B trial, lumasiran reduced urinary oxalate:creatinine ratios and plasma oxalate levels in patients aged < 6 years with PH1. In the single-arm ILLUMINATE-C trial, lumasiran reduced plasma oxalate levels in patients with PH1 receiving dialysis as well as those not receiving dialysis. In secondary and exploratory analyses of these trials, nephrocalcinosis grade, kidney stone event rates and estimated glomerular filtration rates were either stable or improved with lumasiran. Lumasiran had an acceptable tolerability profile that remained consistent in longer-term analyses; the most common adverse events were mild and transient injection-site reactions. Thus, lumasiran is an effective treatment option, with an acceptable tolerability profile, in patients with PH1.
Plain Language Summary
Primary hyperoxaluria type 1 (PH1) is a rare genetic disorder that leads to excess oxalate in urine or plasma requiring removal by the kidneys. This overproduction is damaging and can lead to kidney failure. Management of PH1 is typically not curative, eventually ending in kidney and/or liver transplantation. Lumasiran (Oxlumo®) is the first medicine to be approved in several countries for use in patients with PH1, regardless of their age or level of kidney function. It reduces liver oxalate production, lessening damage to the kidneys and potentially reducing the need for organ transplantation. In clinical trials, lumasiran was effective in reducing oxalate levels (in urine and/or plasma) in patients of all ages with PH1, and irrespective of whether they were receiving dialysis or not. Lumasiran either improved or stabilized the severity of calcium deposition in the kidneys, number of kidney stone events and kidney function. Lumasiran had an acceptable tolerability profile; the most common side effects were mild injection-site reactions that resolved quickly. Thus, lumasiran is an effective treatment option, with an acceptable tolerability profile, in patients with PH1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Digital Features for this Adis Drug Evaluation can be found at https://doi.org/10.6084/m9.figshare.24629649 |
First-in-class synthetic, double-stranded, ribonucleic acid interference molecule targeting glycolate oxidase |
Approved for the treatment of primary hyperoxaluria type 1 in patients of any age |
Reduces urinary oxalate excretion and plasma oxalate levels; effect is sustained in longer-term analyses |
Acceptable tolerability profile; injection-site reactions are the most common adverse event |
1 Introduction
Primary hyperoxalurias are rare and inherited genetic disorders of metabolism where the overproduction of oxalate can cause kidney stones, nephrocalcinosis and, eventually, kidney failure [1]. Primary hyperoxaluria type 1 (PH1) is the most common, occurring in about 80% of all cases of the disease [2], with an estimated prevalence of 1–3 per million population [3]. The disorder develops due to mutations in AGXT, the gene that encodes the alanine–glyoxylate aminotransferase (AGT) enzyme [2]. Deficiency in AGT activity causes glyoxylate to oxidise to oxalate instead of converting to glycine. Subsequent increases in plasma oxalate (POx) levels may lead to systemic oxalosis, and excess urinary oxalate (UOx) has also been established as a major factor in patients with PH1 progressing to kidney failure [2]. Excess UOx (i.e. hyperoxaluria) can lead to acute and chronic kidney damage through crystal tubular deposition and tubular epithelium damage, and its deposition in kidney parenchyma has been associated with inflammatory responses [4].
Management of PH1 has traditionally been very conservative, using strategies such as hyperhydration, crystallization inhibitors (e.g. potassium citrate, neutral phosphorus) and pyridoxine (an AGT co-factor which reduces oxalate overproduction in the subset of patients with specific pyridoxine-responsive mutations) to slow disease progression [1, 2]. In patients with kidney failure, haemodialysis is required but cannot sufficiently remove the overproduced oxalate [2]. The only curative option is liver transplantation (as the new organ will not have mutant AGT), and typically both the liver and the kidney are transplanted in patients with kidney failure [2]. However, patient quality of life is substantially reduced following transplantation of one or both organs, and combined kidney-liver transplant is associated with significant risk of morbidity and mortality [1].
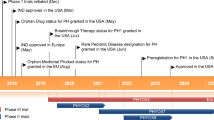
An emerging treatment option for PH1 utilises ribonucleic acid interference (RNAi) to reduce substrate availability for the hepatic production of oxalate [1]. Subcutaneous (SC) lumasiran (Oxlumo®), a first-in-class synthetic, double-stranded, RNAi molecule, is the first RNAi molecule to be approved in several countries for the treatment of PH1 in patients of any age and stage of kidney function, including those with kidney failure [5,6,7]. This article summarizes the pharmacological properties of lumasiran and reviews clinical data relevant to its use in PH1.
2 Pharmacodynamic Properties of Lumasiran
Lumasiran is targeted specifically to the liver by binding to the asialoglycoprotein receptor on the surface of hepatocytes, resulting in intracellular silencing of hydroxyacid oxidase 1 gene (HAO1) messenger RNA (mRNA) [8]. This lowers levels of glycolate oxidase (and therefore decreases conversion of glycolate to glyoxylate by this enzyme) [7], subsequently leading to lowered levels of glyoxylate and normalisation of the overproduction of oxalate in the liver [7, 9]. As glycolate oxidase acts upstream of AGT, lumasiran efficacy is not affected by mutant AGT [7, 9]. Like some other oligonucleotide therapeutics [10], the pharmacodynamics of lumasiran are not directly affected by its pharmacokinetics in plasma, due to its rapid systemic clearance and distribution to the liver, and are comparable between paediatric (4 months to 17 years of age) and adult patients [7]. In animal models, lumasiran demonstrated its ability to durably silence HAO1 mRNA, thereby increasing serum glycolate levels and reducing UOx levels; data suggest there is an approximately equal relationship between HAO1 mRNA silencing and UOx reduction [8].
In a phase I/II trial in healthy participants (n = 32), single doses of SC lumasiran of increasing strength (0.3, 1, 3 and 6 mg/kg) resulted in increased levels of plasma glycolate [3]. The median time for plasma glycolate levels to return to < 20% above baseline or ≤ upper limit of normal (ULN) was 134.5 days. In the randomized, placebo-controlled part of the trial in patients with PH1 (n = 20), SC lumasiran 1 or 3 mg/kg once monthly or 3 mg/kg once every 3 months rapidly reduced UOx excretion: the mean maximum reduction in 24-h UOx excretion from baseline across all dosages assessed was 75%. A 24-h UOx excretion of ≤ 1.5 × ULN (defined as ≤ 0.69 mmol/24 h/1.73 m2) was achieved in all patients [3]. Exploratory pharmacodynamic endpoints in phase III trials showed initially increasing plasma glycolate levels following multiple doses of lumasiran, which then plateaued; this indicates lumasiran was able to reduce hepatic glycolate oxidase activity in patients with PH1 [11, 12].
The immunogenicity of lumasiran was evaluated in all healthy participants and patients with PH1 who received lumasiran in clinical trials (n = 120); although 5.8% tested positive for anti-drug antibodies, no clinically significant effects were observed with respect to the pharmacodynamics, pharmacokinetics or safety of lumasiran [6, 7].
3 Pharmacokinetic Properties of Lumasiran
Lumasiran exhibited time-independent pharmacokinetics in patients with PH1 following multiple SC doses of 1 or 3 mg/kg once monthly or 3 mg/kg once every 3 months [6, 7]. The median maximum plasma drug concentration (Cmax) in patients with PH1 weighing ≥ 20 kg and those weighing < 20 kg who received 3 mg/kg dosing were 529 ng/mL and 7400 ng/mL, respectively [7]. In patients who weighed < 20 kg and received 6 mg/kg dosing, the Cmax (912 ng/mL [7]) was almost twice that of patients who received 3 mg/kg dosing, due to the higher dose and a faster absorption rate [6, 7]. In contrast, the lumasiran median area under the concentration-time curve from time zero to the last measurable concentration after dosing (AUC0–last) AUC0–last was similar across a bodyweight range of 6.2–110.0 kg. The median time to Cmax was 4 h [6, 7].
Lumasiran did not accumulate in plasma following multiple doses, instead distributing to the liver; 77–85% of the dose was bound to protein in the liver [7]. The estimated apparent volume of distribution was 4.9 L [6, 7]. The mean apparent elimination half-life in plasma was 5.2 h, with an estimated apparent clearance of 26.5 L/h. Lumasiran is primarily metabolized to oligonucleotides of shorter lengths by both endo- and exonucleases [6, 7]. Data from in vitro studies show lumasiran is not metabolized by (nor is a substrate for or an inhibitor of) CYP450 enzymes [7]. Lumasiran is mainly excreted as inactive metabolite; up to 26% of the dose is excreted unchanged into the urine within 24 h [6, 7].
The pharmacokinetics of lumasiran were not affected to any clinically relevant extent by patient age (4 months to < 65 years), sex, race, ethnicity, abnormal kidney function, use of haemodialysis or mild-to-moderate hepatic impairment [total bilirubin ≤ ULN and aspartate aminotransferase (AST) > ULN, or total bilirubin ≤ 3 × ULN] [6]. The effects of severe hepatic impairment on lumasiran pharmacokinetics are unknown [6].
4 Therapeutic Efficacy of Lumasiran
The efficacy of lumasiran in PH1 has been (and is continuing to be) assessed in three ongoing phase III trials: the randomized, double-blind, placebo-controlled, multicentre ILLUMINATE-A trial in paediatric and adult patients with PH1 [9], the open-label, single-arm, multicentre ILLUMINATE-B trial in patients aged < 6 years with PH1 [12], and the open-label, single-arm, multicentre ILLUMINATE-C trial in patients with PH1 and advanced kidney disease [11]. In ILLUMINATE-A, patients were randomized (2:1) to receive SC lumasiran 3 mg/kg or placebo, initially once monthly for 3 months, then once every 3 months as maintenance doses [9]. Patients in ILLUMINATE-B and -C received weight-based doses of SC lumasiran [11, 12]. Patients who weighed < 10 kg received 6 mg/kg doses once monthly for 3 months, then 3 mg/kg once monthly. Patients who weighed 10 to < 20 kg received 6 mg/kg doses once monthly for 3 months, then 6 mg/kg once every 3 months. Patients who weighed ≥ 20 kg received 3 mg/kg once monthly for 3 months then 3 mg/kg once every 3 months [11, 12].
All three trials had a primary analysis after 6 months of treatment, after which patients could enter the long-term extension period (54 months) of their respective trial [9, 11, 12]. In the extension period of ILLUMINATE-A, patients who received placebo during the initial double-blinded period could be administered lumasiran at the same dosage (hereafter placebo/lumasiran recipients) as patients who received lumasiran during the initial double-blinded period (lumasiran/lumasiran recipients) [9]. The first 3 months of the extension were also double-blinded (to enable placebo/lumasiran recipients to transition from placebo to lumasiran while remaining blinded). Thereafter, all patients received open-label lumasiran [9]. During the trials, patients continued to receive standard-of-care treatment for PH1 (including hyperhydration, crystallization inhibitors, pyridoxine therapy or a combination thereof) [9, 11, 12]. Patients receiving pyridoxine must have been stable for ≥ 90 days before receiving their first dose of lumasiran [9, 11, 12].
4.1 ILLUMINATE-A
Eligible patients were aged ≥ 6 years with genetically confirmed PH1, an estimated glomerular filtration rate (eGFR) of ≥ 30 mL/min/1.73 m2 and 24-h UOx excretion ≥ 0.70 mmol/24 h/1.73 m2 [9]. Patients were stratified by mean UOx excretion (> 1.70 or ≤ 1.70 mmol/24 h/1.73 m2) [9].
The primary endpoint was the percent change in 24-h UOx excretion [corrected for body surface area (BSA) to normalize age-related variance in oxalate excretion] from baseline to month 6, using an estimate of the least-squares mean percent change from baseline across months 3–6 [9].
Baseline patient demographics and disease characteristics were generally balanced between the treatment groups: the mean age was 14 (range 6–60) years, 33% of patients were female, and the majority (77%) were white [9]. Baseline pyridoxine use was reported in 56% of patients. The overall eGFR was 81.6 mL/min/1.73 m2 (49% of patients had an eGFR of 60 to < 90 mL/min/1.73 m2). Median 24-h UOx excretion was 1.82 mmol/24 h/1.73 m2 and the mean POx level was 15.0 µmol/L. Medullary nephrocalcinosis was present in 54% of patients. Most (85%) patients had a history of kidney stone events (defined as ≥ 1 of: visit to a health care provider, receipt of medication for renal colic, stone passage or macroscopic hematuria due to a kidney stone); the kidney stone event rate [per person per year (/PY)] in the 12 months prior to study entry was 3.19/PY in lumasiran recipients and 0.54/PY in placebo recipients [9].
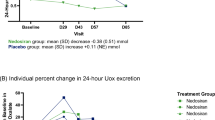
Treatment with lumasiran resulted in rapid and sustained reductions in UOx levels compared with placebo in patients with PH1 [9]. At primary analysis, the reduction in 24-h UOx excretion was significantly (p < 0.001) greater in lumasiran than placebo recipients (Table 1; confirmed by sensitivity analyses); the least-squares mean difference (lumasiran minus placebo) was − 53.5% (95% CI − 62.3 to − 44.8), where a difference less than 0 was a favourable outcome for lumasiran. The mean maximum reduction in 24-h UOx excretion in lumasiran recipients was 76.0%. Prespecified subgroup analyses (of patient age, sex, race, geographical region, history of symptomatic kidney stone events in lifetime, as well as baseline pyridoxine use, 24-h UOx excretion and eGFR) of the primary endpoint consistently demonstrated the superiority of lumasiran over placebo, with the exception of the 12 to < 18 years age group, wherein assessment was limited by a small group size (n = 6) [9].
Treatment with lumasiran also resulted in statistically significant (p < 0.001) improvements over placebo on all of the six secondary endpoints that were hierarchically tested at the time of the primary analysis (i.e. month 6) [9]. Listed in order, these were: absolute change in mean BSA-adjusted 24-h UOx excretion, percent change in mean UOx:creatinine (UOx:Cr) ratio, percent change in mean POx level, proportion of patients with BSA-adjusted 24-h UOx excretion ≤ ULN (defined as 0.514 mmol/24h/1.73 m2), proportion of patients with BSA-adjusted 24-h UOx excretion ≤ 1.5 × ULN, and absolute change in mean POx level. Patient eGFR (a secondary endpoint excluded from the hierarchy) was stable in both treatment groups at 6 months. An exploratory endpoint analysis showed lumasiran did not worsen the nephrocalcinosis grade (assessed by ultrasound using a 4-point scale; a higher number/grade means greater severity) in any patient (grade worsened in one placebo recipient) and reduced the kidney stone event rate (1.09/PY during the first 6 months of treatment vs 3.19/PY over the 12 months prior to consent) [9].
Reductions in 24-h UOx were sustained through 36 months of treatment in the extension period of ILLUMINATE-A (lumasiran/lumasiran recipients received 36 months of treatment and placebo/lumasiran recipients received 30 months; Table 1) [13]. The mean reductions in POx levels from baseline in the core study to month 36 were 36% and 35% in lumasiran/lumasiran and placebo/lumasiran recipients, respectively. In both treatment groups, eGFR remained stable, the nephrocalcinosis grade generally remained stable or improved, and the kidney stone event rate further decreased (to 0.70/PY and 0.39/PY, respectively) through to month 36 [13].
4.2 ILLUMINATE-B
Eligible patients were < 6 years of age with PH1 (confirmed by genetic analysis) who had a UOx:Cr ratio > ULN for their age, an eGFR of > 45 mL/min/1.73 m2 (if aged ≥ 12 months) or normal serum creatinine (if aged < 12 months), and no evidence of extra-renal systemic oxalosis [12].
The primary endpoint was the mean percent change in UOx from baseline to month 6, using an estimate of the least-squares mean percent change from baseline averaged across months 3–6 [12]. Due to the difficulties associated with 24-h urine collections in young children, this endpoint was assessed using UOx:Cr ratios from random spot urine collections, as they correlate to 24-h UOx levels. Secondary endpoints included mean absolute change in spot UOx:Cr ratio, mean percent and absolute changes in POx, and mean percent change in eGFR [12].
The median age at consent to study was 50.1 (range 3–72) months; 56% of patients were female, 89% were white, and patients were mainly from the European (44%) and Middle Eastern (44%) geographical regions [12]. The median baseline eGFR for all patients was 111 mL/min/1.73 m2. Baseline disease characteristics varied across patient weights and ages [12].
Lumasiran produced rapid and sustained reductions in spot UOx:Cr ratios in patients with PH1 aged < 6 years [12]. At primary analysis (median duration of treatment 5.6 months), the least-squares mean change from baseline to month 6 in spot UOx:Cr ratio was − 72.0% (Table 1). Due to the natural age-related decline in UOx levels in young patients, sensitivity analyses and 24-h urine analyses were conducted, and confirmed the robustness of this primary endpoint result. Prespecified subgroup analyses of the primary endpoint according to patient weight categories (< 10 kg, 10 to < 20 kg and ≥ 20 kg) showed mean observed changes in spot UOx:Cr ratios of − 84%, − 69% and − 70%, respectively; reductions in spot UOx:Cr ratios were seen regardless of patient age [12].
Secondary endpoint results confirmed the ability of lumasiran to reduce spot UOx:Cr ratios and POx levels [12]. eGFR remained stable, and lumasiran did not negatively impact the exploratory endpoints of nephrocalcinosis grade (no patients worsened following treatment, and 8 of 14 patients with baseline nephrocalcinosis showed improvement) and the kidney stone event rate (the low historical rate was unchanged following treatment) [12].
Longer-term analyses showed reductions in spot UOx:Cr ratios were sustained to month 30 (Table 1). Reduced POx levels were also maintained to month 30 (mean reduction of 42% from baseline in the core study) [14]. The nephrocalcinosis grade was improved in 86% of patients at month 24 (no patients showed worsening grade), and the kidney stone event rate remained low throughout [14].
4.3 ILLUMINATE-C
Patients of all ages were eligible to enter the study if they had genetically confirmed PH1, POx level ≥ 20 µmol/L, and an eGFR ≤ 45 mL/min/1.73 m2 (if aged ≥ 12 months) or elevated serum creatinine level (if aged < 12 months) [11]. Cohort A included patients who were not receiving haemodialysis at the time of enrolment, whereas cohort B included patients who had been receiving a stable haemodialysis regimen for ≥ 4 weeks prior to screening. During the study, patients from cohort A were able to cross over to cohort B if their kidney function deteriorated and they subsequently required dialysis. Patients were excluded if they were receiving peritoneal dialysis, either alone or in combination with haemodialysis [11].
The primary endpoints were the mean percent change in POx level for patients in cohort A and the mean percent change in pre-dialysis POx level for those in cohort B, from baseline to month 6, using estimates of the least-squares mean percent change from baseline averaged across months 3–6 [11]. Secondary endpoints (all mean values) included absolute change in POx level, percent and absolute change in spot UOx:Cr ratio, and percent and absolute change in BSA-adjusted 24-h UOx excretion [11].
Baseline characteristics were generally balanced between the two cohorts: the median patient age was 8 (range 0–59) years, 43% of patients were female and 76% were white [11]. Median baseline POx levels were 57.9 and 103.7 µmol/L in cohorts A and B, respectively. Patients in cohort B underwent a median of six dialysis sessions per week. Nephrocalcinosis was present at baseline in five patients in cohort A and two patients in cohort B. The kidney stone event rates in the 12 months before study onset were 3.20/PY and 0.07/PY, respectively. Mean baseline eGFR was 19.8 mL/min/1.73 m2 for cohort A [11].
Treatment with lumasiran was able to reduce POx levels regardless of dialysis status in patients with PH1 [11]. At primary analysis, treatment with lumasiran resulted in least-squares mean changes from baseline to month 6 in POx levels of − 33.3% and − 42.4% in cohorts A and B, respectively (Table 1); this reduction was seen as early as month 1 of treatment. Prespecified subgroup analyses showed a consistent reduction in POx levels across the patient age (0 to < 6 years, 6 to < 18 years, ≥ 18 years) and weight (0 to < 10 kg, 10 to < 20 kg, ≥ 20 kg) categories evaluated in cohort B; no results are available for cohort A due to insufficient patient data [11].
Numerical reductions were seen in all secondary endpoints (statistical analyses not available) [11]. Patients with nephrocalcinosis at baseline either had improved grade or remained stable at primary analysis; one patient without nephrocalcinosis at baseline had bilateral worsening. At month 6, the kidney stone event rates were 1.48/PY and 0.00/PY in cohorts A and B, respectively. For cohort A, the mean eGFR was 16.4 mL/min/1.73 m2 [11].
In a longer-term analysis, reductions in POx levels were maintained to month 24 in patients from both cohorts (Table 1) [15]. Two patients from cohort A started haemodialysis and four cohort B patients underwent transplantation (two kidney-only with continued lumasiran treatment and two combined kidney-liver) [15].
5 Tolerability of Lumasiran
SC lumasiran had an acceptable tolerability profile in paediatric and adult patients with PH1, as demonstrated in the ILLUMINATE trials [9, 11, 12]; this profile was sustained in the extension periods of these core trials [13,14,15,16,17,18]. The tolerability profiles of lumasiran in the ILLUMINATE-B and -C trials were similar to that of lumasiran in ILLUMINATE-A, and the most common adverse reactions in all three trials were injection-site reactions [ISRs; in 34.7% of 98 patients at primary analysis (pooled data) [7]] [6]. ISRs most commonly included erythema, swelling, pain, haematoma, pruritus and discolouration; they typically developed on the day of dose administration and generally resolved within two days [7]. Abdominal pain was also commonly reported (in 16.3% of patients at primary analysis). Both of these adverse reactions were generally mild in severity and did not lead to treatment discontinuation [7]. No clinically significant changes were seen in laboratory findings, electrocardiograms, vital signs or physical examinations in any patient in these trials [9, 11, 12].
At primary analysis in the ILLUMINATE trials, adverse events (AEs) were reported in 85% of lumasiran recipients (n = 26) and 69% of placebo recipients (n = 13) in ILLUMINATE-A [9], all patients in ILLUMINATE-B (n = 18) [12], and 81% of patients in ILLUMINATE-C (n = 6 for cohort A and n = 15 for cohort B) [11]. The most common (in ≥ 15% of patients in any group) AEs in the trials included: ISRs (38% of lumasiran recipients vs 0% of placebo recipients), headache (12% vs 23%), rhinitis (8% vs 15%) and upper respiratory tract infection (URTI; 8% vs 15%) in ILLUMINATE-A [9]; pyrexia (33%), rhinitis (22%), URTI and vomiting (both 17%) in ILLUMINATE-B; and pyrexia and ISRs (both 17%) in cohort A, and pyrexia (33%) and ISRs (27%) in cohort B, of ILLUMINATE-C [11]. Treatment-related AEs (TRAEs) were reported in 3 (17%) patients in ILLUMINATE-B: ISRs (mild and transient) in two (11%) patients and headache in one (6%) patient [12].
No serious AEs were reported in ILLUMINATE-A [9]. One patient in ILLUMINATE-B, who weighed ≥ 20 kg, experienced a serious AE of viral infection (moderate in severity) that was not considered related to treatment [12]. In ILLUMINATE-C, serious AEs were reported in 29% of patients (17% and 33% in cohort A and B), most frequently hypokalaemia and vomiting (both 17%) in cohort A and device-related infection in cohort B (13%) [11]. None were considered related to lumasiran treatment. Of note, severe AEs were reported in 20% of patients in cohort B of ILLUMINATE-C (vs none in ILLUMINATE-A [9] and -B [12]) during the 6-month primary analysis period [11]. With the exception of fatigue and disturbance in attention that led to treatment discontinuation in one (4%) lumasiran recipient in ILLUMINATE-A, no other AEs led to treatment discontinuation, study withdrawal or death in the three trials [9, 11, 12].
Longer-term, analyses conducted during the extension periods of the ILLUMINATE trials showed tolerability results consistent with those performed at the time of the primary analyses in patients with PH1 [13,14,15,16,17,18]. At the 36-month extension period analysis of ILLUMINATE-A (n = 39), AEs were reported in 92% of patients in both groups, most commonly ISRs (50% of lumasiran/lumasiran recipients and 46% of placebo/lumasiran recipients), abdominal pain (27% and 8%), headache (19% and 15%) and COVID-19 (12% and 23%) [13]. In a longer-term analysis of ILLUMINATE-B (median 32.6 months of treatment; n = 18), TRAEs were reported in 28% of patients, most commonly mild and transient ISRs (17%) [14]. At 24 months of treatment in ILLUMINATE-C, the most frequently reported TRAEs were mild ISRs (in 24% of 21 patients) [15]. No TRAEs were considered serious or severe, and no AEs led to treatment discontinuation, study withdrawal or death [15].
6 Dosage and Administration of Lumasiran
Lumasiran is approved in several countries, including the USA [6] and those of the EU [7], for the treatment of PH1 (to lower UOx and POx levels [6]) in paediatric and adult patients. The approved dosage regimen of lumasiran, administered by SC injection, is based on patient bodyweight, and involves a loading dose (6 mg/kg for patients who weigh < 20 kg and 3 mg/kg for patients who weigh ≥ 20 kg) once monthly for 3 months, then maintenance doses starting 1 month after the last loading dose: 3 mg/kg once monthly for patients who weigh < 10 kg, 6 mg/kg once every 3 months for patients who weigh 10 to < 20 kg, and 3 mg/kg once every 3 months for patients who weigh ≥ 20 kg [6, 7]. For patients who weigh < 20 kg, a higher starting dose is required to achieve similar liver concentration of lumasiran and target suppression than for patients who weigh ≥ 20 kg, and patients who weigh < 10 kg require more frequent maintenance dosing to compensate for their rapid rate of growth [12]. For patients who require dialysis, lumasiran should be administered after dialysis if it is required on the same day [6, 7].
Due to limited data, lumasiran should be used with caution in the EU in patients with moderate-to-severe hepatic impairment (monitor for decreased lumasiran efficacy), kidney failure (including patients on dialysis; monitor for metabolic acidosis due to increased plasma glycolate levels) and in patients aged < 1 year [7]. As stated in the US label, lumasiran has not been studied in patients with severe hepatic impairment (total bilirubin > 3 × ULN with any AST level); thus, recommendations for use or potential dosage adjustment in this special population cannot be made [6]. As there are no data available on the effects of lumasiran in pregnant or breastfeeding patients, the potential risks associated with the drug will need to be assessed against the potential benefits of treatment [6, 7]. Local prescribing information should be consulted for detailed information regarding contraindications, missed or delayed doses, and other warnings and precautions.
7 Current Status of Lumasiran in the Management of Primary Hyperoxaluria Type 1
Lumasiran is effective in reducing hepatic oxalate production and preserving kidney function in patients of all ages and stages of kidney function with PH1 (Sect. 4). As demonstrated in the phase III ILLUMINATE trials, reductions in UOx and POx levels were sustained over the longer-term, with data available for up to 36 months in ILLUMINATE-A, 30 months in ILLUMINATE-B and 24 months in ILLUMINATE-C (Sect. 4). Lumasiran had an acceptable tolerability profile in these trials, with mild and transient ISRs being the most common AE across all trials (Sect. 5).
UOx and POx levels were used as surrogate predictors of efficacy in preventing progression to kidney damage in the ILLUMINATE trials [19]. This approach is, however, based on retrospective observational data; hence long-term prospective data are needed to confirm the (dur)ability of lumasiran in slowing disease progression in patients with PH1 [1]. In secondary and exploratory analyses, nephrocalcinosis grade, eGFRs and kidney stone event rates were stable or improved during the lumasiran treatment period (Sect. 4); however, analysis of the full 54 weeks of treatment in the extension periods of each trial is needed to confirm these results.
During the ILLUMINATE trials, patients continued to receive standard-of-care treatment for PH1 alongside lumasiran (Sect. 4). However, there are currently no evidence-based recommendations on whether lumasiran should be used in combination with standard PH1 therapies or can be used as a standalone treatment [20]. Regarding this, two cases have been reported where lumasiran recipients with PH1 discontinued nocturnal hyperhydration therapy; one patient [aged 17 years and with two mutations in the AGXT gene (p.G170R and p.R233C variants)] saw regression in their disease progression and improved quality of life, and another patient [aged 15 years with only one detected mutation in the AGXT gene (p.G170A variant)] experienced improvements in their symptoms (including resolution of enuresis) [20].
A consensus statement from OxalEurope and the European Rare Kidney Disease Reference Network strongly recommends the use of RNAi therapies in patients of any age with genetically established PH1 who are unresponsive to pyridoxine therapy (or have a mutation consistent with unresponsiveness) and have UOx excretion > 1.5 × ULN [21]. Guidance from the National Institute of Health and Care Excellence recommends lumasiran as an option for the treatment of PH1, as lumasiran is estimated to be cost-effective from a UK healthcare perspective for a highly specialised technology [22]. Nedosiran (RIVFLOZATM), another small RNAi molecule, is approved in the US in children aged ≥ 9 years and adults with PH1 and relatively preserved kidney function (e.g. eGFR ≥ 30 mL/min/1.73 m2) [23]. While head-to-head comparison may be difficult given the differences in label (e.g. lumasiran is approved for all ages and stages of kidney function), further investigation will be useful in determining the relative place of lumasiran in the management of PH1.
Thus, lumasiran is an effective treatment option, with an acceptable tolerability profile, in patients with PH1.
Data Selection Lumasiran: 160 records identified
Duplicates removed | 1 |
Excluded during initial screening (e.g. press releases; news reports; not relevant drug/indication; preclinical study; reviews; case reports; not randomized trial) | 62 |
Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomized/phase I/II trials) | 74 |
Cited efficacy/tolerability articles | 9 |
Cited articles not efficacy/tolerability | 14 |
Search Strategy: EMBASE, MEDLINE and PubMed from 1946 to present. Clinical trial registries/databases and websites were also searched for relevant data. Key words were lumasiran, Oxlumo, ALN-GO1, AD-65585, primary hyperoxaluria type 1. Records were limited to those in English language. Searches last updated 6 Dec 2023. | |
Change history
15 March 2024
A Correction to this paper has been published: https://doi.org/10.1007/s40265-024-02014-7
References
Bacchetta J, Lieske J. Primary hyperoxaluria type 1: novel therapies at a glance. Clin Kidney J. 2022;15(Suppl. 1):i17–22.
Hoppe B, Martin-Higueras C. Improving treatment options for primary hyperoxaluria. Drugs. 2022;82(10):1077–94.
Frishberg Y, Deschênes G, Groothoff JW, et al. Phase 1/2 study of lumasiran for treatment of primary hyperoxaluria type 1: a placebo-controlled randomized clinical trial. Clin J Am Soc Nephrol. 2021;16(7):1025–36.
Bargagli M, Tio MC, Waikar SS, et al. Dietary oxalate intake and kidney outcomes. Nutrients. 2020;12(9):2673.
Scott LJ, Keam SJ. Lumasiran: first approval. Drugs. 2021;81(2):277–82.
Alnylam Pharmaceuticals Inc. OXLUMO (lumasiran) injection, for subcutaneous use: US prescribing information. 2020. https://www.accessdata.fda.gov. Accessed 6 Dec 2023.
Alnylam Netherlands B.V. Oxlumo: EU summary of product characteristics. 2020. https://www.ema.europa.eu. Accessed 6 Dec 2023.
Liebow A, Li XS, Racie T, et al. An investigational RNAi therapeutic targeting glycolate oxidase reduces oxalate production in models of primary hyperoxaluria. J Am Soc Nephrol. 2017;28(2):494–503.
Garrelfs SF, Frishberg Y, Hulton SA, et al. Lumasiran, an RNAi therapeutic for primary hyperoxaluria type 1. N Engl J Med. 2021;384(13):1216–26.
US Food and Drug Administration. Clinical pharmacology considerations for the development of oligonucleotide therapeutics: draft guidance for industry. 2022. https://www.fda.gov. Accessed 6 Dec 2023.
Michael M, Groothoff JW, Shasha-Lavsky H, et al. Lumasiran for advanced primary hyperoxaluria type 1: phase 3 ILLUMINATE-C trial. Am J Kidney Dis. 2023;81(2):145-55.e1.
Sas DJ, Magen D, Hayes W, et al. Phase 3 trial of lumasiran for primary hyperoxaluria type 1: a new RNAi therapeutic in infants and young children. Genet Med. 2022;24(3):654–62.
Saland JM, Lieske JC, Groothoff JW, et al. Efficacy and safety of lumasiran in patients with primary hyperoxaluria type 1: 36-month analysis of the ILLUMINATE-A trial [abstract no. 194 plus poster]. Am J Kidney Dis. 2023;81(4 Suppl. 1):S56–7.
Michael M, Magen D, Hayes WN, et al. Efficacy and safety of lumasiran for infants and young children with primary hyperoxaluria type 1: 30-month analysis of the phase 3 ILLUMINATE-B trial [abstract no. 75 plus poster]. In: Pediatric Academic Societies Meeting. 2023.
Lieske JC, Magen D, Sellier-Leclerc AA, et al. Lumasiran for primary hyperoxaluria type 1 and impaired kidney function: 24-month analysis of the phase 3 ILLUMINATE-C trial [abstract no. FR-PO592]. J Am Soc Nephrol. 2023;34:566.
Hayes W, Sas DJ, Magen D, et al. Efficacy and safety of lumasiran for infants and young children with primary hyperoxaluria type 1: 12-month analysis of the phase 3 ILLUMINATE-B trial. Pediatr Nephrol. 2023;38(4):1075–86.
Hulton SA, Groothoff JW, Frishberg Y, et al. Randomized clinical trial on the long-term efficacy and safety of lumasiran in patients with primary hyperoxaluria type 1. Kidney Int Rep. 2022;7(3):494–506.
Lieske J, Groothoff J, Frishberg Y, et al. Efficacy and safety of lumasiran in patients with primary hyperoxaluria type 1: 24-month analysis of the ILLUMINATE-A trial [abstract no. PD05-03]. J Urol. 2022;207(Suppl. 5): e87.
Milliner DS, McGregor TL, Thompson A, et al. End points for clinical trials in primary hyperoxaluria. Clin J Am Soc Nephrol. 2020;15(7):1056–65.
Biebuyck N, Destombes C, Prakash R, et al. Is withdrawal of nocturnal hyperhydration possible in children with primary hyperoxaluria treated with RNAi? J Nephrol. 2023;36(5):1473–6.
Groothoff JW, Metry E, Deesker L, et al. Clinical practice recommendations for primary hyperoxaluria: an expert consensus statement from ERKNet and OxalEurope. Nat Rev Nephrol. 2023;19(3):194–211.
National Institute for Health and Care Excellence. Lumasiran for treating primary hyperoxaluria type 1. 2023. https://www.nice.org.uk/guidance/hst25. Accessed 6 Dec 2023.
Novo Nordisk Inc. RIVFLOZATM (nedosiran) injection, for subcutaneous use: US prescribing information. 2023. https://www.accessdata.fda.gov. Accessed 6 Dec 2023.
Acknowledgements
During the peer review process, the manufacturer of lumasiran was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and Conflict of Interest
C. Kang is a salaried employee of Adis International Ltd/Springer Nature, and declares no relevant conflicts of interest. All authors contributed to this article and are responsible for its content.
Ethics Approval, Consent to Participate, Consent to Publish, Availability of Data and Material, Code Availability
Not applicable.
Additional information
The manuscript was reviewed by: A. Abid, Centre for Human Genetics and Molecular Medicine, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; W.F. Hui, Department of Paediatrics and Adolescent Medicine, Hong Kong Children's Hospital, Kowloon, Hong Kong; S. Zmonarski, Department of Nephrology and Transplantation Medicine, Wroclaw Medical University, Wroclaw, Poland
The original online version of this article was revised due to retrospective open access order.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kang, C. Lumasiran: A Review in Primary Hyperoxaluria Type 1. Drugs 84, 219–226 (2024). https://doi.org/10.1007/s40265-023-01987-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-023-01987-1