Abstract
Nedosiran (RIVFLOZA™), a once-monthly subcutaneous small interfering RNA (siRNA) therapy, is being developed by Dicerna Pharmaceuticals, a Novo Nordisk company, for the treatment of primary hyperoxaluria (PH). It reduces oxalate overproduction by inhibiting the expression of the hepatic lactate dehydrogenase (LDH) enzyme. Nedosiran received its first approval on 29 September 2023 in the USA to lower urinary oxalate levels in children aged ≥ 9 years and adults with PH type 1 (PH1) and relatively preserved kidney function [e.g. estimated glomerular filtration rate (eGFR) ≥ 30 mL/min/1.73 m2]. This article summarizes the milestones in the development of nedosiran leading to this first approval for PH1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Digital Features for this AdisInsight Report can be found at https://doi.org/10.6084/m9.figshare.24530836. |
A once-monthly subcutaneous siRNA therapy is being developed by Dicerna Pharmaceuticals, a Novo Nordisk company, for the treatment of PH |
Received its first approval on 29 September 2023 in the USA |
Approved for lowering urinary oxalate levels in children aged ≥ 9 years and adults with PH1 and relatively preserved kidney function (e.g. eGFR ≥ 30 mL/min/1.73 m2) |
1 Introduction
Primary hyperoxaluria (PH) is a family of rare autosomal recessive genetic disorders characterized by the excessive synthesis of oxalate in the liver [1]. Oxalate is typically excreted by the kidneys, but when there is an excess, it accumulates as insoluble calcium oxalate crystals in the kidneys. This accumulation leads to the development of kidney stones, nephrocalcinosis, and the potential progression to chronic kidney disease. Based on the underlying deficient enzyme, PH is classified into three distinct subtypes, namely type 1 (PH1), type 2 (PH2) and type 3 (PH3) [1]. PH1 is the most clinically common (79% of all PH cases) and severe subtype [1, 2]. Hepatic lactate dehydrogenase (LDH) encoded by the LDHA gene catalyzes the conversion of glyoxylate to oxalate in hepatocytes, the last step of oxalate formation in the liver [3]. Consequently, reducing LDH is a promising treatment strategy for all subtypes of PH [3, 4]. Inhibiting LDHA with RNA interference therapies offers a novel approach to treating PH [5].

Key milestones in the development of nedosiran for lowering urinary oxalate levels in patients with primary hyperoxaluria (PH) type 1 (PH1). IND investigational new drug application
Nedosiran (RIVFLOZA™), a once-monthly subcutaneous (SC) small interfering RNA (siRNA) therapy that targets LDH, is being developed by Dicerna Pharmaceuticals, a Novo Nordisk company, for the treatment of PH [6]. Nedosiran is developed using Dicerna’s proprietary GalXC™ platform, which facilitates the delivery of liver-targeted siRNA with high specificity and reversibility [6]. Nedosiran received its first approval on 29 September 2023 in the USA to lower urinary oxalate levels in children aged ≥ 9 years and adults with PH1 and relatively preserved kidney function [e.g. estimated glomerular filtration rate (eGFR) ≥ 30 mL/min/1.73 m2] [7, 8]. Nedosiran is administered once monthly. The recommended dosage is 160 mg in patients aged ≥ 9 years weighing ≥ 50 kg, 128 mg in those aged ≥ 12 years weighing < 50 kg and 3.3 mg/kg in children aged 9–11 years weighing < 50 kg [7]. Clinical development of nedosiran for PH is underway in several countries worldwide.
Nedosiran, following lumasiran (Alnylam Pharmaceuticals), is the second siRNA to obtain approval for treating PH1 [9]. Lumasiran reduces oxalate formation in patients with PH1 by decreasing glyoxylate overproduction in peroxisomes through inhibition of glycolate oxidase. In contrast, nedosiran inhibits hepatic LDH and therefore has the potential to reduce oxalate formation in all PH subtypes [9].
1.1 Company Agreements
In December 2021, Dicerna Pharmaceuticals was acquired by Novo Nordisk [10].
In April 2020, Alnylam Pharmaceuticals and Dicerna Pharmaceuticals finalized their cross-licensing agreement, granting non-exclusive licenses for lumasiran and nedosiran in the treatment of PH1. The companies will receive royalty payments from one another based on the global sales of these drugs [11].
2 Scientific Summary
2.1 Pharmacodynamics
Nedosiran is a synthetic double-stranded siRNA conjugated to a N-acetyl-D-galactosamine (GalNAc) amino sugar residue [12]. Upon SC injection, it is preferentially taken up by hepatocytes via the asialoglycoprotein receptor (ASGPR). Inside the cell, it is loaded into the RNA-induced silencing complex (RISC), where it leverages RNA interference to degrade LDHA mRNA, reducing LDH production and subsequently preventing oxalate accumulation [12]. Nedosiran effectively lowered urinary oxalate levels in mouse models of PH1 and PH2, as well as in a model of ethylene glycol-induced PH [4, 12]. Results from studies conducted in nonhuman primates and a humanized mouse model further suggest the translatability of these findings to human subjects [4, 12].
2.2 Pharmacokinetics
In patients with PH1 or PH2, plasma exposure to nedosiran increased in a dose-proportional manner over a single dose ranging from 1.5 to 6.0 mg/kg [7]. Following multiple monthly administrations at the recommended dosage, nedosiran exhibits time-independent pharmacokinetics, with no accumulation. The key pharmacokinetic parameters of SC nedosiran are as follows: median time to reach maximum plasma concentration 6 h; estimated apparent volume of distribution 126 L; protein binding 85.6%; mean half-life 15 h; and estimated apparent clearance 5.7 L/h. Nedosiran primarily distributes to the liver and undergoes metabolism by endonucleases and exonucleases to shorter oligonucleotides. Approximately 27% of the administered nedosiran dose is excreted unchanged into the urine within 24 h of administration [7]. Nedosiran exposure in patients with PH3 is generally similar to that in those with PH1 or PH2 [13].
No clinically significant differences in the pharmacokinetics of nedosiran were observed based on age (9–73 years), sex, race/ethnicity, mild-to-moderate kidney function impairment (eGFR 30–89 mL/min/1.73 m2) or mild hepatic function impairment [total bilirubin ≤ upper limit of normal (ULN) and aspartate aminotransferase (AST) > ULN; or total bilirubin > 1 to 1.5 × ULN and any AST) [7]. In patients with PH1, nedosiran exposure is increased in those with severe kidney function impairment (eGFR < 30 mL/min/1.73 m2) compared to those with mild-to-moderate impairment [14]. The effect of moderate or severe liver function impairment (total bilirubin > 1.5 ULN with any AST) on the pharmacokinetics of nedosiran has not been studied [7]. Coadministration of pyridoxine (vitamin B6) does not significantly alter nedosiran pharmacokinetics [7].
Features and properties of nedosiran
Alternative names | DCR PHXC; Nedosiran sodium; NN-7022; RivflozaTM |
Class | Amides; amino sugars; drug conjugates; small interfering RNA; urologic |
Mechanism of action | Lactate dehydrogenase 5 expression inhibitors; RNA interference |
Route of administration | Subcutaneous |
Pharmacodynamics | Prevents oxalate production by inhibiting hepatic lactate dehydrogenase expression |
Pharmacokinetics | Tmax ≈ 6 h; Vz/F 126 L; protein binding 85.6%; t1/2 15 h; CL/F 5.7 L/h. ≈ 27% of the administered nedosiran dose is excreted unchanged into the urine within 24 h |
Most frequent adverse reaction | Injection-site reactions |
ATC codes | |
WHO ATC code | A16A-X (various alimentary tract and metabolism products) |
EphMRA ATC code | A16A (other alimentary tract and metabolism products) |
Molecular formula (CAS registry number) | C662H808F19N231O413P57S6Na57 (2247026-22-6) |
2.3 Therapeutic Trials
2.3.1 Pivotal Phase 2 Trial
In a randomized, double-blind, placebo-controlled, multinational phase 2 trial (PHYOX2; NCT03847909), nedosiran treatment was associated with clinically meaningful reduction in urinary oxalate excretion in patients with PH1 [15]. Eligibility criteria included: age ≥ 6 years, genetically confirmed PH1 (n = 29) or PH2 (n = 6), 24-h urinary oxalate excretion ≥ 0.7 mmol (≥ 1.6 mmol in at least one instance in ≥ 12 participants; based on adjusted per 1.73 m2 body surface area [BSA] in participants aged < 18 years) and eGFR ≥ 30 mL/min per 1.73 m2 BSA. Key exclusion criteria included no prior or planned kidney or liver transplantation, no current or planned dialysis and no use of an RNA interference therapy in the last 6 months. Patients were randomized 2:1 to nedosiran or placebo once monthly for 6 months. Nedosiran dose was based on age and body weight (≥ 12 years: 136 mg for < 50 kg and 170 mg for ≥ 50 kg; 6–11 years: 3.5 mg/kg to a maximum of 136 mg) [15].
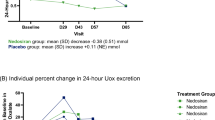
In the modified intent-to-treat (mITT) population, the percent reduction from baseline in 24-h urinary oxalate excretion, as assessed by area under the curve (AUC) from day 90 to day 180 (primary endpoint; recommended by the US FDA) was significantly greater in the nedosiran group than in the placebo group (least squares mean + 3507.4 vs − 1664.4; difference 5171.7; p < 0.001) [15]. In a prespecified analysis, this effect was even more pronounced in the PH1 subgroup (+ 4575.1 vs − 1316.7; p < 0.001). In this subgroup, mean 24-h urinary oxalate excretion levels steadily decreased beginning at the first visit (day 30) and reached the near-normal range by day 120. Whereas no consistent pattern for this endpoint was seen in patients with PH2 [15].
In the mITT population, significantly more nedosiran recipients than placebo recipients reached normal or near-normal 24-h urinary oxalate excretion on ≥ 2 consecutive visits starting at day 90 in the overall population (50% vs. 0%; p = 0.002) and in the PH1 subgroup (64.7% vs. 0%; p < 0.001) [key secondary endpoint] [15]. Among evaluable adults in the ITT population, the nedosiran group demonstrated a greater mean percent reduction in plasma oxalate from baseline at day 180 compared to the placebo group (– 25% vs. 0%; p = 0.026). A post hoc analysis revealed that this effect was statistically significant (− 25% vs + 6.25%; p = 0.017) in the PH1 subgroup. Nedosiran significantly reduced kidney stone burden (number and summed surface area of kidney stones) in the PH1 subgroup (p = 0.024) but not in the overall population. In the ITT population, there were no significant changes in the 36-Item Short Form Survey, EuroQol-5-dimensions-5-levels, or Pediatric Quality of Life Inventory measures either within or between treatment groups from baseline to day 180 [15].
2.3.2 Phase 1 Trials
Nedosiran demonstrated preliminary efficacy in a 2-part, randomized, single-ascending-dose, phase 1 trial (PHYOX1; NCT03392896) [16]. PHYOX1 enrolled 25 healthy volunteers and 18 patients with PH1 or PH2. Patients received a single open-label dose of nedosiran at 1.5, 3.0, or 6.0 mg/kg. Across all dose levels, the mean maximum percentage reduction in 24-hour urinary oxalate excretion from baseline at day 57 was 55%, and the mean time to reach the maximum reduction was 45.9 days. A greater reduction was observed with increasing doses. In total, 24-h urinary oxalate excretion normalized in 5 out of 15 patients with PH1 and 1 out of 3 patients with PH2, with an additional 6 patients with PH1 showing values that were nearly normal [16].
Nedosiran showed the potential to reduce urinary oxalate in six patients with PH3 in a multinational, randomized, double-blind, placebo-controlled phase 1 trial (PHYOX4; NCT04555486) [13]. Patients received a single dose of nedosiran 3 mg/kg or a placebo. None of the patients met the primary pharmacodynamic endpoint, requiring a > 30% reduction from baseline in 24-h urinary oxalate at two consecutive visits (assessed at days 29, 43, 57, and 85 post-dose). However, it's worth noting that this endpoint was reached during at least one visit in 3 out of 4 nedosiran recipients, with one patient achieving near-normal 24-h urinary oxalate levels from day 29 to day 85. Additionally, 24-h urinary oxalate excretion decreased by 24.5% from baseline at day 85 in nedosiran recipients, while it increased by 10% in placebo recipients [13].
2.3.3 Long-Term Extension Study
Patients who have successfully completed any PHYOX trial, as well as their siblings under 18 years old with genetically confirmed PH, could enrol in an ongoing open-label long-term extension study (PHYOX3; NCT04042402) where all patients could receive nedosiran for up to 6 years [7, 17, 18]. In PHYOX3, 13 patients with PH1 who transitioned from PHYOX2 and received an additional 6 months of treatment demonstrated a sustained reduction in urinary oxalate levels [7].
Similarly, 13 patients with PH1 who transitioned from PHYOX1 were retreated with nedosiran once their 24-h urinary oxalate levels returned to baseline [17,18,19]. Following retreatment, these patients experienced a sustained reduction of ≥ 60% in mean urinary oxalate excretion levels from baseline at month 30 [19]. Moreover, at each visit starting at month 2, ≥ 77% of the patients were able to achieve normal or near-normal levels of 24-h urinary oxalate excretion [19].
In four patients with PH3, including three nedosiran recipients and one placebo recipient, who transitioned from PHYOX4 to PHYOX3, 24-h urinary oxalate levels decreased by a mean 46.7% from the baseline at month 6 [20].
Key clinical trials of nedosiran (Dicerna Pharmaceuticals, a Novo Nordisk company)
Drug(s) | Indication | Phase | Status | Location(s) | Identifier |
|---|---|---|---|---|---|
Nedosiran | PH | 3 | Enrolling by invitation | Global | NCT04042402; PHYOX3 |
Nedosiran | PH | 2 | Recruiting | Global | NCT05001269; PHYOX8 |
Nedosiran | PH1, PH2 | 2 | Recruiting | Global | NCT04580420; PHYOX7 |
Nedosiran, placebo | PH1, PH2 | 2 | Completed | Global | NCT03847909; PHYOX2 |
Nedosiran, placebo | PH3 | 1 | Completed | Global | NCT04555486; PHYOX4 |
2.4 Adverse Events
Nedosiran was generally well tolerated in patients with PH participating in clinical trials [13,14,15,16,17,18]. The most common (incidence ≥ 20%) adverse reaction to nedosiran was injection-site reactions [7].
In PHYOX2, adverse events (AEs) lead to treatment discontinuation in 1 of 23 (4%) nedosiran recipients and 1 of 12 (8%) placebo recipients [15]. Treatment-related AEs occurred in 44% and 25% of patients in the respective groups, with the most common being injection-site erythema (22% vs 0%) and injection-site pain (9% vs 0%). A serious AE involving severe, fluctuating tachycardia of undetermined origin was reported in one nedosiran recipient and it was considered possibly related to the treatment. Treatment-emergent AEs (TEAEs) occurred in 83% of patients in each treatment group. Most TEAEs were of mild or moderate severity, with severe TEAE reported in 1 (4%) nedosiran recipient and 4 (33%) placebo recipients. TEAEs that occurred more frequently (difference ≥ 2%) with nedosiran than with placebo included injection-site erythema (11% vs 0%), headache (6% vs 3%) and nausea (4% vs 1%). The incidences of TEAEs of special interest with nedosiran (vs placebo) were as follows: injection-site reaction (9% vs 0%), kidney stone events (13% vs 42%) and muscle pain or weakness (0% vs 0%). Nedosiran was not associated with any clinically significant changes in laboratory parameters, physical examinations, or electrocardiograms; there were no clinically significant trends in creatine kinase elevations [15].
During the 30-month treatment period in PHYOX3, no new safety signals emerged. There were no treatment-related serious AEs or treatment discontinuations due to AEs [19]. Across all clinical studies, nedosiran did not induce or boost anti-drug antibodies [7].
2.5 Ongoing Clinical Trials
The PHYOX3 study is still ongoing. A phase 2 (PHYOX8; NCT05001269) trial is evaluating the safety, pharmacokinetics and efficacy of nedosiran in paediatric patients from birth to 11 years of age with PH and relatively intact kidney function. Another phase 2 trial (PHYOX7; NCT04580420) is evaluating the safety and efficacy of nedosiran in patients with PH1 or PH2 and severe renal impairment, with or without dialysis.
Change history
22 January 2024
A Correction to this paper has been published: https://doi.org/10.1007/s40265-024-01996-8
References
Cochat P, Rumsby G. Primary hyperoxaluria. N Engl J Med. 2013;369(7):649–58.
Soliman NA, Nabhan MM, Abdelrahman SM, et al. Clinical spectrum of primary hyperoxaluria type 1: experience of a tertiary center. Nephrol Ther. 2017;13(3):176–82.
Ariceta G, Barrios K, Brown BD, et al. Hepatic lactate dehydrogenase A: an RNA interference target for the treatment of all known types of primary hyperoxaluria. Kidney Int Rep. 2021;6(4):1088–98.
Lai C, Pursell N, Gierut J, et al. Specific inhibition of hepatic lactate dehydrogenase reduces oxalate production in mouse models of primary hyperoxaluria. Mol Ther. 2018;26(8):1983–95.
Forbes TA, Brown BD, Lai C. Therapeutic RNA interference: a novel approach to the treatment of primary hyperoxaluria. Br J Clin Pharmacol. 2022;88(6):2525–38.
Dicerna Pharmaceuticals. RNAi therapies to target the cause of disease. 2021. https://dicerna.com/. Accessed 9 Nov 2023.
Novo Nordisk. RIVFLOZATM (nedosiran) injection, for subcutaneous use: US prescribing information. 2023. https://www.fda.gov/. Accessed 9 Nov 2023.
Novo Nordisk. FDA approves Rivfloza™ for children ≥ 9 years old and adults living with primary hyperoxaluria type 1 (PH1), a rare genetic condition [media release]. 2 Oct 2023. https://www.novonordisk.com/.
Bacchetta J, Lieske JC. Primary hyperoxaluria type 1: novel therapies at a glance. Clin Kidney J. 2022;15(Suppl 1):i17–22.
Novo AS. Novo Nordisk announces completion of Dicerna Pharmaceuticals acquisition [media release]. 28 Dec 2021. http://www.novonordisk.com.
Dicerna Pharmaceuticals, Alnylam Pharmaceuticals. Alnylam and Dicerna form RNAi therapeutics collaboration on alpha-1 antitrypsin deficiency-associated liver disease and complete cross-license agreement for primary hyperoxaluria programs [media release]. 6 Apr 2020. http://www.dicerna.com.
Liu A, Zhao J, Shah M, et al. Nedosiran, a candidate siRNA drug for the treatment of primary hyperoxaluria: design, development, and clinical studies. ACS Pharmacol Transl Sci. 2022;5(11):1007–16.
Goldfarb DS, Lieske JC, Groothoff J, et al. Nedosiran in primary hyperoxaluria subtype 3: results from a phase I, single-dose study (PHYOX4). Urolithiasis. 2023;51(1):80.
Amrite A, Fuentes E, Marbury TC, et al. Safety, pharmacokinetics, and exposure-response modeling of nedosiran in participants with severe chronic kidney disease. Clin Pharmacol Drug Dev. 2023. https://doi.org/10.1002/cpdd.1320.
Baum MA, Langman C, Cochat P, et al. PHYOX2: a pivotal randomized study of nedosiran in primary hyperoxaluria type 1 or 2. Kidney Int. 2023;103(1):207–17.
Hoppe B, Koch A, Cochat P, et al. Safety, pharmacodynamics, and exposure-response modeling results from a first-in-human phase 1 study of nedosiran (PHYOX1) in primary hyperoxaluria. Kidney Int. 2022;101(3):626–34.
Hoppe B, Coenen M, Schalk G, et al. Nedosiran in primary hyperoxaluria subtype 1: interim results from an open-label extension trial (PHYOX3) [abstract no. P1-050]. Pediatr Nephrol. 2023;38(7):2289.
Hoppe B, Coenen M, Schalk G, et al. PHYOX3: a long-term, open-label extension trial of nedosiran in patients with primary hyperoxaluria type 1, 2, or 3 [abstract no. PO1625 plus poster]. J Am Soc Nephrol. 2020;31(Suppl):515.
Groothoff J, Sellier-Leclerc AL, Deesker L, et al. Long-term nedosiran safety and efficacy in primary hyperoxaluria type 1 (PH1): interim analysis of PHYOX3 [abstract no. TH-PO1128]. In: American Society of Nephrology Kidney Week. 2023.
Goldfarb DS, Groothoff J, Vrhnjak B. Nedosiran in patients with primary hyperoxaluria 3: interim results from an ongoing open label, safety extension trial (PHYOX3) [poster]. In: 14th International Hyperoxaluria Workshop. 2023.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and Conflict of interest
During the peer review process the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes resulting from any comments received were made by the authors on the basis of scientific completeness and accuracy. Yahiya Y. Syed is a salaried employee of Adis International Ltd/Springer Nature, and declares no relevant conflicts of interest. All authors contributed to this article and are responsible for its content.
Ethics approval, Consent to participate, Consent to publish, Availability of data and material, Code availability
Not applicable.
Additional information
This profile has been extracted and modified from the AdisInsight database. AdisInsight tracks drug development worldwide through the entire development process, from discovery, through pre-clinical and clinical studies to market launch and beyond.
The original article has been revised due to retrospective open choice order.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Syed, Y.Y. Nedosiran: First Approval. Drugs 83, 1729–1733 (2023). https://doi.org/10.1007/s40265-023-01976-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-023-01976-4