Abstract
Cardiac arrhythmias remain a common cause of death and disability. Antiarrhythmic drugs (AADs) and antiarrhythmic agents remain a cornerstone of current cardiac arrhythmia management, despite moderate efficacy and the potential for significant adverse proarrhythmic effects. Due to conceptual, regulatory and financial considerations, the number of novel antiarrhythmic targets and agents in the development pipeline has decreased substantially during the last few decades. However, several promising candidates remain and there are exciting developments in repurposing and reformulating already existing drugs for indications related to cardiac arrhythmias. This review discusses the key conceptual considerations for the development of new antiarrhythmic agents, summarizes new compounds and formulations currently in clinical development for rhythm control of atrial fibrillation, and highlights the potential for drug repurposing. Finally, future directions in AAD development are discussed. Together with an ever-increasing understanding of the molecular mechanisms underlying cardiac arrhythmias, these components support a cautiously optimistic outlook towards improved pharmacological treatment opportunities for patients suffering from cardiac arrhythmias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cardiac arrhythmias remain a major clinical problem and although current antiarrhythmic drugs have significant limitations, pharmacological treatment is expected to remain a cornerstone of cardiac arrhythmia management. |
Development of novel antiarrhythmic drugs has decreased over the last decades. |
Repurposing and reformulating existing drugs may provide novel opportunities for management of cardiac arrhythmias. |
1 Introduction
Cardiac arrhythmias remain a common cause of death and disability [1, 2]. Antiarrhythmic drugs (AADs) and antiarrhythmic agents are prescribed for termination of atrial and ventricular arrhythmias (acute cardioversion) and/or prevention of arrhythmia recurrence (long-term maintenance of normal sinus rhythm). Despite significant advances in device and catheter ablation-based therapies of cardiac arrhythmias over the last decades [3, 4], AADs remain a cornerstone of antiarrhythmic therapy. For example, the prescription rate of AADs nearly tripled between 2004 and 2016 in a large retrospective nationwide study in the USA. This increase was mainly due to increased prescription rates of amiodarone, sotalol, flecainide and dofetilide [5]. Similar results were observed in a Danish nationwide study, showing a 16% increase in the use of AADs over a 19-year time period mainly due to increased use of amiodarone and flecainide [6]. The increased prescription rates of AADs are primarily driven by increased diagnosis rates of atrial arrhythmias such as atrial fibrillation (AF) [7], which clinically is the most common cardiac arrhythmia [8]. The rising prevalence of AF can be partly attributed to an increase in AF prevalence and incidence promoted by an aging population, the obesity pandemic, and an increased number of patients living with chronic diseases [8]. However, the increasing use of screening modalities and improvements in AF detection by mobile health solutions have also contributed to the rising diagnosis rates [7, 9, 10]. Accumulating evidence suggests that (early) antiarrhythmic therapy to restore and maintain sinus rhythm (rhythm control) improves outcomes in AF patients [11,12,13,14]. However, despite the increased incidence of cardiac arrhythmias and the central role for AADs in arrhythmia therapy, the number of novel AADs has been very limited in recent years.
Initial AAD development efforts during the 1970s and 1980s focused primarily on the treatment of ventricular arrhythmias. However, after the failures of the Cardiac Arrhythmia Suppression Trial (CAST) [15] and Survival With Oral D-Sotalol (SWORD) trial [16], which showed worse outcomes in patients treated with AADs compared to placebo control, the focus has shifted more to atrial arrythmias, notably AF [17, 18]. Nevertheless, ventricular pro-arrhythmic side effects of novel AADs for rhythm control of AF have proven to be one of the hardest hurdles to overcome in AAD development, although recent trials showed a comparable rate of adverse effects between AADs and ablation, with AADs showing a trend towards a lower rate of adverse effects [19].
Prominent challenges for de novo development of AADs for the pharmaceutical industry include a costly and long process of preclinical development and large-scale clinical trials, concerns about drug safety, increased regulatory hurdles, and growing economic pressure from generics [20]. Furthermore, the initial success and clinical excitement for development of ablation therapy, which has significantly lowered arrhythmia recurrence rates than currently available AADs [21,22,23], has likely hampered the development of AADs. At present, the number of novel antiarrhythmic targets and agents in the development pipeline is limited. However, their results are promising and there are exciting developments in repurposing and reformulating already approved drugs to novel therapeutic indications and delivery methods, which gives renewed hope for improved pharmacological treatment opportunities for patients suffering from cardiac arrhythmias.
In this review we aim to provide insights into conceptual considerations for AAD development and provide an overview of recent advances in pharmacological antiarrhythmic therapy for AF, including repurposing and reformulating already approved drug and agents.
2 Conceptual Considerations for Antiarrhythmic Drug (AAD) Development
2.1 Multi-target Effects and Drug Combinations
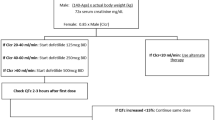
There are several criteria that an ideal AAD must meet in order to become available clinically. The primary criterion is safety. Cardiac pro-arrhythmic effects and extracardiac side effects represent significant challenges when developing AADs and need to be carefully evaluated (Fig. 1). Significant efforts have been made to target ion channels selectively expressed in the atria, thereby reducing the risk of ventricular pro-arrhythmia. However, few channels are truly atrial selective and disease-related remodeling can differentially affect the regional expression of AAD targets. This ionic remodeling can negatively affect both therapeutic efficacy (in case of down-regulation of the primary therapeutic target in the atria, thereby reducing the drug-induced antiarrhythmic effect) and safety (due to up-regulation in the ventricles thereby increasing the risk of pro-arrhythmia). Moreover, the majority of AADs do not only affect one ion channel, but, to a different degree, target multiple membrane ion currents and/or intracellular ion fluxes (Fig. 1). This multi-channel effect can modulate the risk of pro-arrhythmic and extra-cardiac side effects depending on whether the multi-channel block effect is synergistic or antagonistic. For example, combined inhibition of multiple repolarizing potassium channels can synergistically reduce repolarization reserve [24], whereas simultaneous inhibition of depolarizing and repolarizing currents by amiodarone limits excessive reverse rate-dependent repolarization prolongation compared to pure class III potassium channel blockers [25], contributing to its relatively low pro-arrhythmic potential [26]. Furthermore, targeting multiple channels at once could improve therapeutic efficacy and limit polypharmacy thereby increasing compliance and drug persistence. For example, the HARMONY trial showed that combining midrange doses of oral ranolazine with reduced doses of dronedarone synergistically reduced the AF burden in patients with paroxysmal AF and was well tolerated [27]. Similarly, the recent multinational randomized controlled Secondary Prevention of Cardiovascular Disease in the Elderly (SECURE) trial sought to investigate the efficacy of a polypill-based therapeutic strategy. The SECURE study included patients with a myocardial infarction within the previous 6 months and investigated a polypill comprising aspirin, ramipril (an angiotensin-converting enzyme [ACE] inhibitor) and atorvastatin (a statin) versus routine care. The study found a significantly lower risk of major adverse cardiovascular events including cardiovascular death, nonfatal ischemic stroke or urgent revascularization in patients receiving the polypill [28]. The polypill approach also resulted in higher patient compliance [28], highlighting the opportunity to combine already existing therapies to reduce polypharmacy, increase compliance, and ideally increase efficacy. However, apart from the HARMONY trial, the combination of AADs to improve long-term rhythm control has not been systematically evaluated. Finally, it should be noted that drug combinations may increase the risk of adverse drug-drug interactions with other pharmacological therapies, which are common in patients with AF [29].
2.2 Drug Formulation and Route of Administration
Other important criteria that require consideration in the development of AADs are the chemical drug design, drug formulation and route of administration. Numerous cardiac ion channels are also expressed in the brain, where they play a pivotal role in regulating the central nervous system, which is why novel antiarrhythmic agents need to be designed in ways that prevent them from passing the protective blood-brain barrier in order to avoid serious neurological side effects. In general, oral drug formulations are preferred over other types of formulations. Patient compliance is higher with oral formulation compared to other routes of administration, as this is more convenient for the patients, and oral formulations can easily be transferred to large-scale production due to a higher cost-effectiveness for the pharmaceutical industry. However, oral bioavailability can be highly variable due to shifts in physiochemical and metabolic processes that dictate pharmacokinetics. Intestinal metabolism, reverse transport in the gut and the first-pass hepatic metabolism represent major obstacles that critically determine bioavailability of orally applied drugs. In addition, more targeted organ drug delivery needs to be considered using alternative routes of administration in order to obtain better therapeutic outcome and reduced side effects. This includes alternative routes of administration (Fig. 1), e.g., nasal administration or local cardiac injections, for which examples are given below.
2.3 Direct Versus Indirect Modulation of the Vulnerable Electrophysiological Substrate
A conceptual distinction should be made between direct modulators of cardiac electrophysiology (typically inhibitors of cardiac ion channels) and targeting of key nodal signaling pathways involved in proarrhythmic cardiac remodeling. Successful lifestyle and risk factor management have been shown to have antiarrhythmic potential—especially in AF [30]. Obesity, diabetes mellitus, sleep apnea and hypertension are all examples of factors that can be regulated successfully to improve the management of AF. The PREVEntion and RegReSsive Effect of weight-loss and risk factor modification on Atrial Fibrillation (REVERSE-AF) study showed that a weight loss of ≥ 10% could prevent further progression of AF and also reverse persistent to paroxysmal AF or no arrhythmia [31]. Upstream therapy similarly aims to prevent or reverse the progression of cardiac remodeling to prevent arrhythmia recurrence through pharmacological targeting of processes similar to those affected with successful lifestyle and risk-factor management, e.g., hypertrophy, fibrosis and inflammation (Fig. 1). While traditional ‘upstream therapy’, involving systemic inhibition of major receptor systems and pathways to prevent the development of a vulnerable substrate might represent a more causative therapy, its true effectiveness can only be evaluated with long-term follow-up and is likely limited when a substrate is already present [32, 33], presenting challenges for both clinical trial design and real-world application. Indeed, considering the fact that AF is often detected quite late in many patients, traditional upstream therapy has proven to be only moderately effective for primary prevention and even less successful for secondary prevention of AF [34, 35]. By contrast, selective molecular targeting of key signaling molecules and nodal points could be an alternative to achieve both decent efficacy along with satisfactory reduction of symptoms and consequent improvement of quality of life. While this may also be partially achieved by targeting modifiable risk factors, we focus below on potential pharmacological approaches.
3 Recent Advances in AAD Therapies
It has been more than a decade since a novel AAD was marketed for AF therapy and there are currently very few AADs in the development pipeline [36]. On the other hand, there are several promising developments related to new formulations of already approved AADs, as well as repurposing of drugs used for other indications to the antiarrhythmic therapy regime. In this section, we review the novel targets and recent compounds that are currently in clinical development. An overview of compounds, their primary therapeutic targets, and ongoing clinical trials is provided in Table 1.
3.1 Novel AAD Targets
3.1.1 Small Conductance Ca2+-activated K+ (SK) Channels
Small conductance Ca2+-activated K+ (SK) channels have gained interest over the last two decades in the treatment of AF due to their apparent atrial selectivity. Although expressed in both atrial and ventricular tissue, under normal physiological conditions SK channels play a role in atrial, but not ventricular repolarization [37, 38]. Numerous preclinical studies have demonstrated clear antiarrhythmic effects of SK-channel inhibition on the termination of AF as well as prevention of arrhythmia reinduction due to prolongation of the action potential duration and the effective refractory period [39,40,41,42,43,44,45], even in the presence of relatively advanced forms of AF that were refractory to cardioversion by currently approved and rather effective AADs [43]. Recent work demonstrated that SK current is up-regulated in patients with persistent AF due to a functional up-regulation resulting from phosphatase-2A-dependent calmodulin-Thr80 dephosphorylation and enhanced SK-channel trafficking to the sarcolemma. The action potential duration shortening resulting from the enhanced SK channels current promotes re-entry and AF, supporting the importance of further development of SK-channel blockers for both cardioversion and maintenance of SR in AF patients [46]. In Phase 1 clinical trials, the SK-channel blocker AP30663 proved to be safe and well-tolerated when given intravenously. Apart from the reported infusion site-related side-effects, which were mild and temporary, the blocker induced small and transient QTc prolongation of approximately 18 ms, which did not give rise to serious concerns [47]. Recently, Acesion Pharma announced that the Phase 2 clinical trial for AP30663 successfully met the efficacy and safety end-points for pharmacological cardioversion of patients with recent-onset AF (NCT04571385). This novel SK-channel blocker showed a dose-dependent effect and exceeded 50% cardioversion rate to SR within 90 min of infusion start. The trial included 63 patients who were followed for 30 days. No serious adverse events including ventricular arrhythmias were observed. Acesion Pharma has also announced that their 2nd generation oral lead compound AP31969 indicated for SR maintenance is planned for a Phase 1 clinical trial starting in 2023 [48] (Table 1).
3.1.2 Acetylcholine-Activated Inward-Rectifier K+ Channel Blockers
The autonomic nervous system plays a critical role in AF pathophysiology [49] and the acetylcholine-dependent inward-rectifier K+-current (IK,ACh) has been shown to be constitutively active during caffeine phosphodiesterase (cAF) inhibition [50, 51]. The constitutively-active IK,ACh has been attributed to increased phosphorylation of protein kinase C epsilon type (PKCε), increased activity of the nucleoside diphosphate kinase B and changes in channel stoichiometry [52,53,54]. Despite promising antiarrhythmic effects for acute cardioversion of AF in numerous large animal models [55,56,57,58,59], the clinical effects of IK,ACh blockers in human subjects have not yet been proven and many development programs for IK,ACh blockers have been terminated (Table 1).
3.1.3 HSY244
HSY244 is a novel AAD with undisclosed mechanism of action. It is currently investigated in a randomized, placebo-controlled, double-blinded study to evaluate the efficacy for cardioversion of AF, safety, tolerability, and pharmacokinetics of HSY244 in patients with AF (NCT04582409) [36]. However, the trial was terminated in April 2023 based on business decisions (NCT04582409) (Table 1).
3.1.4 Multi-channel Blocker
HBI-3000 is a multi-channel blocker currently investigated in a Phase 2 trial for acute intravenous cardioversion of patients with recent-onset AF (NCT04680026). In vitro HBI-3000 shows inhibitory effects on INa,peak, INa,late, ICa,L and IKr in ventricular cardiomyocytes [60]. HBI-3000 was well-tolerated in the Phase 1 clinical trial and showed no pro-arrhythmic effects, despite dose-dependent ECG changes (prolonged QRS, P wave duration, PR interval), which are suspected to be due to the potent multi-channel block. The Phase 2 trial is estimated to be completed in December 2023 (NCT04680026) (Table 1).
3.2 Novel AAD Formulations
3.2.1 Flecainide
Flecainide is a Na+ blocker approved for prevention of both atrial and ventricular arrhythmias and cardioversion of recent-onset AF in patients without known relevant structural heart disease [61]. The cardioversion rate of intravenous flecainide is 51–55% and high-dose oral flecainide is available as a ‘pill-in-the-pocket approach’ for more convenient pharmacological cardioversion [61, 62]. Recently, inhaled flecainide acetate has been developed to achieve a superior administration form that can produce faster and higher plasma concentrations for acute pharmacological cardioversion than orally administered flecainide. A recent dose-escalation study investigated the feasibility, tolerability and efficacy of inhaled flecainide acetate given in doses of 30, 60, 90 and 120 mg for cardioversion of patients with recent-onset AF [63]. Conversion rates were dose-dependent and correlated with plasma concentrations. Patients given the highest dose of flecainide that achieved a plasma concentration > 200 ng/mL had a cardioversion rate of 50% within 90 minutes [63]. The latter is comparable to that reported for oral and intravenous administration of flecainide. Administration of flecainide via oral inhalation might provide a safe and effective alternative to intravenous or pill-in-the-pocket cardioversion, reducing the need for hospital admissions of AF patients (Table 2).
3.2.2 Etripamil
Etripamil is an L-type Ca2+-blocker, which is still under development for termination of atrioventricular nodal-dependent paroxysmal supraventricular tachycardia (PSVT). The recently conducted Phase 3 trial ‘Efficacy and Safety of Intranasal MSP-2017 (Etripamil) for the Conversion of PSVT to Sinus Rhythm (NODE-301) of 70 mg nasal spray used during systematic sustained PSVT failed to meet the primary endpoint, which was cardioversion within 5 hours. However, at earlier timepoints, e.g., 30 min, the cardioversion rated reached 53.7% compared to 34.7% with placebo [64]. Nasal administration of etripamil has been evaluated to be safe and well tolerated, but further investigations are necessary to identify effective and convenient options for cardioversion of patients with PSVT [65] (Table 2).
3.2.3 Bisoprolol
Bisoprolol is a selective β1-receptor blocker used for the treatment of hypertension. In a retrospective study including 61 patients undergoing non-cardiac surgery treated with bisoprolol transdermal patches, 77% cardioverted to sinus rhythm within 24 hours following development of post-operative AF [66]. The major limitation of this study was the lack of a control group confirming that this high cardioversion rate was not partly due to spontaneous cardioversion in some patients [66]. In a different retrospective study investigating the difference in post-operative AF between orally administered bisoprolol and transdermal patches in patients undergoing cardiac surgery, the investigators found that only 24% of patients treated with transdermal patches developed AF compared to 46% of patients treated with oral bisoprolol [67]. Both studies were retrospective and enrolled a relatively low number of patients, therefore it remains to be validated whether bisoprolol patches provide a therapeutic option for prevention of post-operative AF (Table 2).
3.2.4 Amiodarone
Amiodarone is the most effective AAD to date and is available in oral and intravenous formulations. Although still in a preclinical stage, the epicardial application of amiodarone-eluting patches is an interesting approach for targeted drug delivery in patients at risk of developing post-operative AF. The targeted delivery in theory makes it possible to achieve therapeutic doses of amiodarone locally in the atrial tissue, minimizing the systemic exposure to the drug and thereby the long list of extracardiac adverse effects of amiodarone. In goats, the epicardial application of bi-layered amiodarone-eluting patches resulted in increased effective refractory period and conduction time, as well as reduced vulnerability to burst pacing-induced atrial arrhythmia up to 28 days post-implantation of the patches [68]. Future clinical studies in patients undergoing open heart surgery are needed to evaluate the true antiarrhythmic potential of this approach (Table 2).
3.3 Repurposing of Approved Agents
3.3.1 Doxapram
The two-pore-domain K+ channels or K2P channels are among the most recently discovered therapeutic targets for AF. K2P channels are a large family of K+ channels responsible for an instantaneous and non-inactivating ‘leak’ current [69]. TASK-1 (K2P3.1) channels are predominantly expressed in atrial tissue and appear to be up-regulated both in terms of expression level and function in AF patients [70, 71]. This makes them an interesting atrial-selective target in AF therapy [72]. Doxapram is a potent TASK-1 inhibitor. Traditionally, doxapram has been used as a respiratory stimulant in patients with moderate to severe ventilatory failure and in patients with chronic obstructive pulmonary disease [72]. However, doxapram is rarely applied today for these indications because of development of other pharmacological approaches. Preclinical studies have shown the antiarrhythmic potential of doxapram in pigs [73]. Doxapram is currently being investigated for cardioversion of paroxysmal or persistent non-valvular AF in patients in the DOxapram Conversion TO Sinus rhythm (DOCTOS-Trial) (EudraCT No: 2018-002978-17) (Table 3).
3.3.2 Botulinum Toxin A
Botulinum toxin A is a neurotoxin that reduces the exocytotic release of acetylcholine from nerve endings and is commonly used for cosmetic treatments but is also used for medical indications such as neurological conditions and bladder disorders. Recent and ongoing clinical trials have investigated the antiarrhythmic potential of botulinum toxin A injections into the ganglionated plexi-enriched fat pads during open heart surgery for prevention of post-operative AF [74]. Although the first two large randomized clinical trials showed a reduced relative risk and an absolute difference in the occurrence of post-operative AF [75, 76], only one of the studies could demonstrate a significant difference between botulinum toxin A injections and placebo [75, 77, 78]. The recently completed Phase 2 trial (NOVA study, NCT03779841) investigating botulinum toxin type A (AGN-151607) for the prevention of post-operative AF in patients undergoing open-chest cardiac surgery [79] revealed no differences in the prevalence of post-operative AF upon injection of AGN-151607. In a sub-group analysis, lower rates of post-operative AF and re-hospitalization were found in patients aged ≥ 65 years undergoing coronary artery bypass grafting [80]. The current ongoing Prevention of Atrial Fibrillation by Botulinum Toxin Injections (BOTAF) study (NCT04075981) will further clarify the safety and efficacy of botulinum toxin A injection for prevention of post-operative AF.
Of note, botulinum toxin A has not only drawn attention for the prevention of post-operative AF but has also been proposed for prevention of ventricular arrhythmias post-myocardial infarction. Recently, a preclinical study demonstrated that injection of botulinum toxin A into the left stellate ganglion in a canine model of chronic myocardial infarction lead to inhibition of left stellate ganglion function, which improved heart rate variability and alleviated ventricular remodeling, ameliorated cardiac function, and prevented ventricular arrhythmias 30 days after induction of myocardial infarction. The ultrasound-guided percutaneous injection of botulinum toxin is noninvasive and therefore constitutes a clinically relevant approach [81] (Table 3).
3.3.3 Colchicine
Colchicine is a well-known drug used for decades to treat gout and familial Mediterranean fever [82]. Due to its microtubule-disrupting properties, colchicine is able to inhibit the assembly and activation of the NLRP3-inflammasome [83, 84]. Therapeutic low-dose colchicine has been shown to be safe and its therapeutic potential within the cardiovascular field has greatly expanded to atherosclerosis, pericarditis, heart failure and myocardial infarction [85]. In addition, colchicine has found its way into clinical use as an AAD. In particular, colchicine has been tested for the prevention of post-operative AF following both open-heart surgery and catheter ablation. Although some trials have demonstrated positive outcomes [86, 87], others were unable to reproduce these results [88, 89]. Currently, four clinical trials are investigating the antiarrhythmic potential of colchicine in AF patients (Table 3).
3.3.4 Metformin
Metformin is a 5′adenosine monophosphate-activated kinase activator widely used as oral antidiabetic drug [90]. Observational studies indicate that metformin use is associated with a lower risk of AF compared to other oral antidiabetic drugs such as sulfonylureas [91]. In a mouse model of bleomycin-induced lung fibrosis the anti-fibrotic properties of metformin were clearly demonstrated [92], but whether the same effects apply to cardiac fibrosis is unknown. Metformin was in a recent transcriptomics-based network medicine-based analysis of drug gene signatures and functional analysis in human inducible pluripotent stem cell-derived cardiomyocytes identified as promising candidates for AF therapy by reducing the risk of AF compared to standard anti-diabetic therapy [93, 94]. Currently, three clinical trials are investigating metformin as an upstream therapy against AF (Table 3).
3.3.5 Canakinumab
Increasing evidence suggests an important role for inflammation in AF. Serum inflammatory biomarkers correlate with low atrial voltages in patients with AF [95]. Similarly, COVID-19 infection causes AF [96] and AF is a risk factor for major adverse cardiovascular events in COVID-19 patients [97]. A potentially promising anti-inflammatory target is the multimeric protein complex, NLRP3 inflammasome (NACHT, LRR, and PYD domain-containing protein 3). Enhanced cardiomyocyte-specific NLRP3 inflammasome activation was recently reported in patients with AF [99], as well as those who go on to develop post-operative AF [98], which established the NLRP3 inflammasome as a potential novel AF target [99, 100]. Currently there are no NLRP3 inflammasome inhibiting drugs in development pipeline for AF prevention. However, downstream effects of NLRP3-activation can be targeted. Canakinumab is a monoclonal IL-1β antibody that reduced major cardiac events in patients with atherosclerosis in the CANTOS trial (The Canakinumab Anti-Inflammatory Thrombosis Outcome Study) [101]. The effects of canakinumab for AF were investigated in the small pilot clinical trial CONVERT-AF, which evaluated the recurrence rate of AF after electrical cardioversion of patients with persistent AF treated with either canakinumab or placebo [102]. Atrial fibrillation recurrence at 6 months was 77% in the placebo group and 36% in the canakinumab group [102], but this did not reach conventional statistical significance, most likely due to the very small sample size of the study population. The promising results of this pilot trial require further proof and verification in future studies investigating the potential of NLRP3-inflammasome inhibitors [83] (Table 3).
3.3.6 Sodium Glucose Co-transporter Inhibitors (SGLTi)
Sodium glucose co-transporter inhibitors (SGLTi) are known to reduce cardiovascular outcomes including mortality. A recent meta-analysis including 31 trials and 75,279 participants revealed a moderately lower risk of total and serious AF-associated events with SGLTi and a lower risk of heart failure hospitalization and cardiovascular disease-related deaths [103, 104]. Preclinical studies have also demonstrated a direct effect of SGLT2i on cardiomyocytes. A recent study employing mice with heart failure with preserved ejection fraction has demonstrated that the SGLT2i empagliflozin reduces the late Na+ current and prevents pro-arrhythmic action potential prolongation [105]. Currently there are six ongoing clinical trials investigating the effect of SGLTi in patients with persistent AF (NCT05252624), AF and type 2 diabetes mellitus (NCT05029115, NCT05174052, NCT04583813) or in patients undergoing catheter ablation therapy to investigate the reoccurrence of AF (NCT04780438, NCT04792190) (Table 3).
3.3.7 Angiotensin Receptor-Neprilysin Inhibitor (ARNI)
Angiotensin receptor-neprilysin inhibitors (ARNIs) such as the combination of sacubitril and valsartan appear to have beneficial effects on both atrial and ventricular arrhythmias in several studies [106]. While a few studies point towards a reduced burden and recurrence of atrial arrhythmias in patients with heart failure with reduced ejection fraction (HFrEF) [107, 108], others do not observe this effect [109, 110]. However, it should be noted that these studies were not explicitly designed to focus on rhythm monitoring, which is why the burden of AF might be underestimated. Furthermore, studies showing a reversed cardiac remodeling by sacubitril/valsartan treatment in terms of increased left-ventricular ejection fraction (LVEF) and other ventricular functional measures reported a lower incidence of ventricular arrhythmias and sudden cardiac death [111,112,113]. Preclinical studies have shown that sacubitril/valsartan can reverse the reduction of L-type Ca2+ current, atrial and ventricular effective refractory period (ERP) shortening as well as fibrosis in the setting of atrial pacing induced AF in a rabbit model [106]. Together, these data suggest that ARNI might sufficiently reverse cardiac remodeling to show antiarrhythmic efficacy. Clearly, further prospective studies are required to test and validate the antiarrhythmic potential of ARNI in different patient populations (Table 3).
4 Future Directions
The clinical excitement of technological advances and changing patterns of medical practice in combination with a relatively lenient device legislation gave patients in Europe fast and constantly changing access to new device-based therapies. However, this development has also resulted in approval of new devices without direct evidence from clinical trials to show whether the manufacturer could provide evidence that the new device was similar to an already approved device. These regulations stand in contrast to the large amount of evidence required for approval of a novel pharmacological agent. However, the new European medical device legislation, which became fully effective from May 2021, may change the industrial development of device therapies and might reduce the number of approvals based on the principle of equivalence compared to what has been the case so far [114]. Perhaps this will make a shift towards development of novel AADs an appealing task once again.
Moreover, there is evidence for socioeconomic disparities in the use of rhythm-control therapies in patients with AF, particularly for ablation [115], which suggests that besides increasing our efforts to develop novel AADs, making them broadly accessible to all patients should be another important future objective.
Unlike ventricular fibrillation, AF is not an immediately life-threatening disease. Therefore, novel AADs to be used in AF therapy have to have a high efficacy, a high safety profile, and be well tolerated. In contrast to anticancer drugs where prolongation of life even for a few months is the therapeutic end-point, for atrial arrhythmias the quality of life is currently the most frequently used primary end-point. It is much more difficult to develop effective approaches against a complex disease such as AF [116]. Because of these considerations, the regulations are much stricter for drug development against arrhythmias than against cancer. Favoring small molecules over complex genetic approaches and repurposing or reformulating already existing drugs with a known safety profile might therefore be preferable. Alternatively, local delivery with cardiac-specific cargo of viruses directed against defined molecular targets and gene-editing might provide highly-specific mechanism-based antiarrhythmic therapies in the future. For example, novel nano delivery systems may enable target-oriented delivery of drugs [117]. Nanoparticles can be either organic or inorganic structures less than 100 nm. The use of nanoparticles in different cardiovascular diseases is currently being explored for more target-oriented delivery [118]. For example, silica nanoparticles containing adenosine have been shown to reduce infarct size post-myocardial infarction, while the adverse effects such as hypotension and slow heart rate, commonly observed by systemic application, are avoided [119]. The nano delivery approach could potentially improve both the efficacy and safety profiles of novel and already existing antiarrhythmic agents.
For many years, anti-fibrotic therapy has been an appealing approach to prevent or even reverse the progression of cardiac diseases and cardiac arrhythmias. However, the difficulties of targeting the complex mechanism of pro-fibrotic signaling has hindered progression in the development of anti-fibrotic drugs. Promising targets include the NLRP3-inflammasome [98, 120] and the renin-angiotensin-aldosterone system (RAAS), which could prove to reduce the fibrotic remodeling in humans [121, 122].
The complex nature of atrial arrhythmias combined with the fact that patients are highly heterogeneous, elderly, and comorbid requires careful selection and design of clinically relevant and measurable outcomes in the clinical trials when developing novel antiarrhythmic agents [123, 124] (Fig. 1).
5 Outlook
Development of novel antiarrhythmic agents has declined over the last decades. However, despite the advances in ablation therapy there remains an unmet need for arrhythmia management with antiarrhythmic agents showing sufficient efficacy and good safety, as evidenced in recent large clinical trials. Although there are only a few new drugs in the development pipeline, their initial results appear promising and some might make it to the clinical setting. Importantly, the repurposing and reformulating of already approved drugs to novel therapeutic indications along with new and ideally atrial-selective delivery methods offer new avenues for the development of novel antiarrhythmic therapies that may help reduce the cardiac arrhythmia-related morbidity and mortality and improve the quality of life of millions of patients.
References
Coute RA, Nathanson BH, Panchal AR, Kurz MC, Haas NL, McNally B, et al. Disability-adjusted life years following adult out-of-hospital cardiac arrest in the United States. Circ Cardiovasc Qual Outcomes. 2019;12(3): e004677.
Dong XJ, Wang BB, Hou FF, Jiao Y, Li HW, Lv SP, et al. Global burden of atrial fibrillation/atrial flutter and its attributable risk factors from 1990 to 2019. Europace. 2023;25(3):793–803.
Richard Tilz R, Sano M, Vogler J, Fink T, Saraei R, Sciacca V, et al. Very high-power short-duration temperature-controlled ablation versus conventional power-controlled ablation for pulmonary vein isolation: the fast and furious—AF study. Int J Cardiol Heart Vasc. 2021;35: 100847.
Mugnai G, Cecchini F, Stroker E, Paparella G, Iacopino S, Sieira J, et al. Durability of pulmonary vein isolation following cryoballoon ablation: lessons from a large series of repeat ablation procedures. Int J Cardiol Heart Vasc. 2022;40: 101040.
Markman TM, Geng Z, Epstein AE, Nazarian S, Deo R, Marchlinski FE, et al. Trends in antiarrhythmic drug use among patients in the United States between 2004 and 2016. Circulation. 2020;141(11):937–9.
Poulsen CB, Damkjær M, Løfgren B, Schmidt M. Trends in antiarrhythmic drug use in Denmark over 19 years. Am J Cardiol. 2020;125(4):562–9.
Kalarus Z, Mairesse GH, Sokal A, Boriani G, Średniawa B, Casado-Arroyo R, et al. Searching for atrial fibrillation: looking harder, looking longer, and in increasingly sophisticated ways. An EHRA position paper. Europace. 2023;25(1):185–98.
Kornej J, Börschel CS, Benjamin EJ, Schnabel RB. Epidemiology of atrial fibrillation in the 21st century: novel methods and new insights. Circ Res. 2020;127(1):4–20.
Hermans ANL, Gawalko M, Dohmen L, van der Velden RMJ, Betz K, Duncker D, et al. Mobile health solutions for atrial fibrillation detection and management: a systematic review. Clin Res Cardiol. 2022;111(5):479–91.
Noubiap JJ, Agbaedeng TA, Kamtchum-Tatuene J, Fitzgerald JL, Middeldorp ME, Kleinig T, et al. Rhythm monitoring strategies for atrial fibrillation detection in patients with cryptogenic stroke: a systematic review and meta-analysis. Int J Cardiol Heart Vasc. 2021;34: 100780.
Kirchhof P, Camm AJ, Goette A, Brandes A, Eckardt L, Elvan A, et al. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med. 2020;383(14):1305–16.
Rillig A, Borof K, Breithardt G, Camm AJ, Crijns H, Goette A, et al. Early rhythm control in patients with atrial fibrillation and high comorbidity burden. Circulation. 2022;146(11):836–47.
Jensen M, Suling A, Metzner A, Schnabel RB, Borof K, Goette A, et al. Early rhythm-control therapy for atrial fibrillation in patients with a history of stroke: a subgroup analysis of the EAST-AFNET 4 trial. Lancet Neurol. 2023;22(1):45–54.
Rillig A, Magnussen C, Ozga AK, Suling A, Brandes A, Breithardt G, et al. Early rhythm control therapy in patients with atrial fibrillation and heart failure. Circulation. 2021;144(11):845–58.
Echt DS, Liebson PR, Mitchell LB, Peters RW, Obias-Manno D, Barker AH, et al. Mortality and morbidity in patients receiving encainide, flecainide, or placebo. The cardiac arrhythmia suppression trial. N Engl J Med. 1991;324(12):781–8.
Waldo AL, Camm AJ, deRuyter H, Freidman PL, MacNeil DJ, Pitt B, et al. Survival with oral d-sotalol in patients with left ventricular dysfunction after myocardial infarction: rationale, design, and methods (the SWORD trial). Am J Cardiol. 1995;75(15):1023–7.
Kowey PR, Robinson VM. The relentless pursuit of new drugs to treat cardiac arrhythmias. Circulation. 2020;141(19):1507–9.
Heijman J, Hohnloser SH, Camm AJ. Antiarrhythmic drugs for atrial fibrillation: lessons from the past and opportunities for the future. Europace. 2021;23(23 Suppl 2):ii14–22.
Turagam MK, Musikantow D, Whang W, Koruth JS, Miller MA, Langan MN, et al. Assessment of catheter ablation or antiarrhythmic drugs for first-line therapy of atrial fibrillation: a meta-analysis of randomized clinical trials. JAMA Cardiol. 2021;6(6):697–705.
Murteira S, Ghezaiel Z, Karray S, Lamure M. Drug reformulations and repositioning in pharmaceutical industry and its impact on market access: reassessment of nomenclature. J Mark Access Health Policy. 2013;1.
Mont L, Bisbal F, Hernández-Madrid A, Pérez-Castellano N, Viñolas X, Arenal A, et al. Catheter ablation vs antiarrhythmic drug treatment of persistent atrial fibrillation: a multicentre, randomized, controlled trial (SARA study). Eur Heart J. 2014;35(8):501–7.
Andrade JG, Wells GA, Deyell MW, Bennett M, Essebag V, Champagne J, et al. Cryoablation or drug therapy for initial treatment of atrial fibrillation. N Engl J Med. 2021;384(4):305–15.
Saglietto A, Gaita F, De Ponti R, De Ferrari GM, Anselmino M. Catheter ablation vs. anti-arrhythmic drugs as first-line treatment in symptomatic paroxysmal atrial fibrillation: a systematic review and meta-analysis of randomized clinical trials. Front Cardiovasc Med. 2021;8:664647.
Varró A, Baczkó I. Cardiac ventricular repolarization reserve: a principle for understanding drug-related proarrhythmic risk. Br J Pharmacol. 2011;164(1):14–36.
Sutanto H, Laudy L, Clerx M, Dobrev D, Crijns H, Heijman J. Maastricht antiarrhythmic drug evaluator (MANTA): a computational tool for better understanding of antiarrhythmic drugs. Pharmacol Res. 2019;148: 104444.
Schrickel JW, Schwab JO, Yang A, Bielik H, Bitzen A, Lüderitz B, et al. Pro-arrhythmic effects of amiodarone and concomitant rate-control medication. Europace. 2006;8(6):403–7.
Reiffel JA, Camm AJ, Belardinelli L, Zeng D, Karwatowska-Prokopczuk E, Olmsted A, et al. The HARMONY trial: combined ranolazine and dronedarone in the management of paroxysmal atrial fibrillation: mechanistic and therapeutic synergism. Circ Arrhythm Electrophysiol. 2015;8(5):1048–56.
Castellano JM, Pocock SJ, Bhatt DL, Quesada AJ, Owen R, Fernandez-Ortiz A, et al. Polypill strategy in secondary cardiovascular prevention. N Engl J Med. 2022;387(11):967–77.
Shurrab M, Koh M, Jackevicius CA, Qiu F, Conlon M, Caswell J, et al. Prescribing of two potentially interacting cardiovascular medications in atrial fibrillation patients on direct oral anticoagulants. Int J Cardiol Heart Vasc. 2021;34: 100788.
Chung MK, Eckhardt LL, Chen LY, Ahmed HM, Gopinathannair R, Joglar JA, et al. Lifestyle and risk factor modification for reduction of atrial fibrillation: a Scientific Statement from the American Heart Association. Circulation. 2020;141(16):e750–72.
Middeldorp ME, Pathak RK, Meredith M, Mehta AB, Elliott AD, Mahajan R, et al. PREVEntion and regReSsive effect of weight-loss and risk factor modification on atrial fibrillation: the REVERSE-AF study. Europace. 2018;20(12):1929–35.
Savelieva I, Kakouros N, Kourliouros A, Camm AJ. Upstream therapies for management of atrial fibrillation: review of clinical evidence and implications for European Society of Cardiology guidelines. Part II: secondary prevention. Europace. 2011;13(5):610–25.
Savelieva I, Kakouros N, Kourliouros A, Camm AJ. Upstream therapies for management of atrial fibrillation: review of clinical evidence and implications for European Society of Cardiology guidelines. Part I: primary prevention. Europace. 2011;13(3):308–28.
Fang WT, Li HJ, Zhang H, Jiang S. The role of statin therapy in the prevention of atrial fibrillation: a meta-analysis of randomized controlled trials. Br J Clin Pharmacol. 2012;74(5):744–56.
Mazurek M, Shantsila E, Lane DA, Wolff A, Proietti M, Lip GYH. Secondary versus primary stroke prevention in atrial fibrillation: insights from the Darlington Atrial Fibrillation Registry. Stroke. 2017;48(8):2198–205.
Nattel S, Sager PT, Hüser J, Heijman J, Dobrev D. Why translation from basic discoveries to clinical applications is so difficult for atrial fibrillation and possible approaches to improving it. Cardiovasc Res. 2021;117(7):1616–31.
Skibsbye L, Poulet C, Diness JG, Bentzen BH, Yuan L, Kappert U, et al. Small-conductance calcium-activated potassium (SK) channels contribute to action potential repolarization in human atria. Cardiovasc Res. 2014;103(1):156–67.
Darkow E, Nguyen TT, Stolina M, Kari FA, Schmidt C, Wiedmann F, et al. Small conductance Ca2+-activated K+ (SK) channel mRNA expression in human atrial and ventricular tissue: comparison between donor, atrial fibrillation and heart failure tissue. Front Physiol. 2021;12: 650964.
Linz B, Hesselkilde EM, Skarsfeldt MA, Hertel JN, Sattler SM, Yan Y, et al. Pharmacological inhibition of SK-channels with AP14145 prevents atrial arrhythmogenic changes in a porcine model for obstructive respiratory events. J Cardiovasc Electrophysiol. 2023;34(1):126–34.
Gatta G, Sobota V, Citerni C, Diness JG, Sørensen US, Jespersen T, et al. Effective termination of atrial fibrillation by SK channel inhibition is associated with a sudden organization of fibrillatory conduction. Europace. 2021;23(11):1847–59.
Fenner MF, Gatta G, Sattler S, Kuiper M, Hesselkilde EM, Adler DMT, et al. Inhibition of small-conductance calcium-activated potassium current (IK, Ca) leads to differential atrial electrophysiological effects in a Horse Model of persistent atrial fibrillation. Front Physiol. 2021;12: 614483.
Saljic A, Soattin L, Trachsel DS, Boddum K, Jespersen T. In vivo knockdown of SK3 channels using antisense oligonucleotides protects against atrial fibrillation in rats. J Mol Cell Cardiol. 2020;147:18–26.
Diness JG, Skibsbye L, Simó-Vicens R, Santos JL, Lundegaard P, Citerni C, et al. Termination of vernakalant-resistant atrial fibrillation by inhibition of small-conductance Ca2+-activated K+ channels in pigs. Circ Arrhythm Electrophysiol. 2017;10(10): e005125.
Yan Y, Skarsfeldt MA, Diness JG, Bentzen BH. Small conductance calcium activated K+ channel inhibitor decreases stretch induced vulnerability to atrial fibrillation. Int J Cardiol Heart Vasc. 2021;37: 100898.
Heijman J, Rahm AK, Dobrev D. Stretching the limits of antiarrhythmic drug therapy: the promise of small-conductance calcium-activated potassium channel blockers. Int J Cardiol Heart Vasc. 2021;37: 100924.
Heijman J, Zhou X, Morotti S, Molina CE, Abu-Taha IH, Tekook M, et al. Enhanced Ca2+-dependent SK-channel gating and membrane trafficking in human atrial fibrillation. Circ Res. 2023;132(9):e116–33.
Gal P, Klaassen ES, Bergmann KR, Saghari M, Burggraaf J, Kemme MJB, et al. First clinical study with AP30663—a KCa2 channel inhibitor in development for conversion of atrial fibrillation. Clin Transl Sci. 2020;13(6):1336–44.
Acesion. Positive phase 2 data from atrial fibrillation clinical trial—primary endpoint met 2023. Available from: https://www.acesionpharma.com/post/positive-phase-2-data-from-atrial-fibrillation-clinical-trial-primary-endpoint-met.
Linz D, Elliott AD, Hohl M, Malik V, Schotten U, Dobrev D, et al. Role of autonomic nervous system in atrial fibrillation. Int J Cardiol. 2019;287:181–8.
Dobrev D, Friedrich A, Voigt N, Jost N, Wettwer E, Christ T, et al. The G protein-gated potassium current IK, ACh is constitutively active in patients with chronic atrial fibrillation. Circulation. 2005;112(24):3697–706.
Voigt N, Maguy A, Yeh YH, Qi X, Ravens U, Dobrev D, et al. Changes in IK, ACh single-channel activity with atrial tachycardia remodelling in canine atrial cardiomyocytes. Cardiovasc Res. 2008;77(1):35–43.
Makary S, Voigt N, Maguy A, Wakili R, Nishida K, Harada M, et al. Differential protein kinase C isoform regulation and increased constitutive activity of acetylcholine-regulated potassium channels in atrial remodeling. Circ Res. 2011;109(9):1031–43.
Voigt N, Friedrich A, Bock M, Wettwer E, Christ T, Knaut M, et al. Differential phosphorylation-dependent regulation of constitutively active and muscarinic receptor-activated IK, ACh channels in patients with chronic atrial fibrillation. Cardiovasc Res. 2007;74(3):426–37.
Voigt N, Heijman J, Trausch A, Mintert-Jancke E, Pott L, Ravens U, et al. Impaired Na+-dependent regulation of acetylcholine-activated inward-rectifier K+ current modulates action potential rate dependence in patients with chronic atrial fibrillation. J Mol Cell Cardiol. 2013;61:142–52.
Hashimoto N, Yamashita T, Tsuruzoe N. Tertiapin, a selective IKACh blocker, terminates atrial fibrillation with selective atrial effective refractory period prolongation. Pharmacol Res. 2006;54(2):136–41.
Hashimoto N, Yamashita T, Tsuruzoe N. Characterization of in vivo and in vitro electrophysiological and antiarrhythmic effects of a novel IKACh blocker, NIP-151: a comparison with an IKr-blocker dofetilide. J Cardiovasc Pharmacol. 2008;51(2):162–9.
Walfridsson H, Anfinsen OG, Berggren A, Frison L, Jensen S, Linhardt G, et al. Is the acetylcholine-regulated inwardly rectifying potassium current a viable antiarrhythmic target? Translational discrepancies of AZD2927 and A7071 in dogs and humans. Europace. 2015;17(3):473–82.
Sobota V, Gatta G, van Hunnik A, van Tuijn I, Kuiper M, Milnes J, et al. The acetylcholine-activated potassium current inhibitor XAF-1407 terminates persistent atrial fibrillation in goats. Front Pharmacol. 2020;11: 608410.
Fenner MF, Carstensen H, Dalgas Nissen S, Melis Hesselkilde E, Scott Lunddahl C, Adler Hess Jensen M, et al. Effect of selective IK, ACh inhibition by XAF-1407 in an equine model of tachypacing-induced persistent atrial fibrillation. Br J Pharmacol. 2020;177(16):3778–94.
Guo D, Liu Q, Liu T, Elliott G, Gingras M, Kowey PR, et al. Electrophysiological properties of HBI-3000: a new antiarrhythmic agent with multiple-channel blocking properties in human ventricular myocytes. J Cardiovasc Pharmacol. 2011;57(1):79–85.
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498.
Crijns HJ, Weijs B, Fairley AM, Lewalter T, Maggioni AP, Martín A, et al. Contemporary real life cardioversion of atrial fibrillation: results from the multinational RHYTHM-AF study. Int J Cardiol. 2014;172(3):588–94.
Crijns H, Elvan A, Al-Windy N, Tuininga YS, Badings E, Aksoy I, et al. Open-label, multicenter study of flecainide acetate oral inhalation solution for acute conversion of recent-onset, symptomatic atrial fibrillation to sinus rhythm. Circ Arrhythm Electrophysiol. 2022;15(3): e010204.
Stambler BS, Plat F, Sager PT, Shardonofsky S, Wight D, Potvin D, et al. First randomized, multicenter, placebo-controlled study of self-administered intranasal etripamil for acute conversion of spontaneous paroxysmal supraventricular tachycardia (NODE-301). Circ Arrhythm Electrophysiol. 2022;15(12): e010915.
Stambler BS, Dorian P, Sager PT, Wight D, Douville P, Potvin D, et al. Etripamil nasal spray for rapid conversion of supraventricular tachycardia to sinus rhythm. J Am Coll Cardiol. 2018;72(5):489–97.
Yasui T, Oka T, Shioyama W, Oboshi M, Fujita M. Bisoprolol transdermal patch treatment for patients with atrial fibrillation after noncardiac surgery: a single-center retrospective study of 61 patients. SAGE Open Med. 2020;8:2050312120907817.
Okamura H, Arakawa M, Miyagawa A, Adachi H. Incidence of postoperative atrial fibrillation in transdermal β-blocker patch users is lower than that in oral β-blocker users after cardiac and/or thoracic aortic surgery. Gen Thorac Cardiovasc Surg. 2019;67(12):1007–13.
Bolderman RW, Bruin P, Hermans JJ, Boerakker MJ, Dias AA, van der Veen FH, et al. Atrium-targeted drug delivery through an amiodarone-eluting bilayered patch. J Thorac Cardiovasc Surg. 2010;140(4):904–10.
Goldstein SA, Bayliss DA, Kim D, Lesage F, Plant LD, Rajan S. International Union of Pharmacology. LV. Nomenclature and molecular relationships of two-P potassium channels. Pharmacol Rev. 2005;57(4):527–40.
Schmidt C, Wiedmann F, Voigt N, Zhou XB, Heijman J, Lang S, et al. Upregulation of K2P3.1 K+ current causes action potential shortening in patients with chronic atrial fibrillation. Circulation. 2015;132(2):82–92.
Schmidt C, Wiedmann F, Zhou XB, Heijman J, Voigt N, Ratte A, et al. Inverse remodelling of K2P3.1 K+ channel expression and action potential duration in left ventricular dysfunction and atrial fibrillation: implications for patient-specific antiarrhythmic drug therapy. Eur Heart J. 2017;38(22):1764–74.
Kraft M, Büscher A, Wiedmann F, L’Hoste Y, Haefeli WE, Frey N, et al. Current drug treatment strategies for atrial fibrillation and TASK-1 inhibition as an emerging novel therapy option. Front Pharmacol. 2021;12: 638445.
Wiedmann F, Beyersdorf C, Zhou XB, Kraft M, Paasche A, Jávorszky N, et al. Treatment of atrial fibrillation with doxapram: TASK-1 potassium channel inhibition as a novel pharmacological strategy. Cardiovasc Res. 2022;118(7):1728–41.
Saljic A, Hansen MEH, Dobrev D. Botulinum toxin for prevention of post-operative atrial fibrillation. Naunyn Schmiedebergs Arch Pharmacol. 2023;396(3):385–8.
Pokushalov E, Kozlov B, Romanov A, Strelnikov A, Bayramova S, Sergeevichev D, et al. Botulinum toxin injection in epicardial fat pads can prevent recurrences of atrial fibrillation after cardiac surgery: results of a randomized pilot study. J Am Coll Cardiol. 2014;64(6):628–9.
Waldron NH, Cooter M, Haney JC, Schroder JN, Gaca JG, Lin SS, et al. Temporary autonomic modulation with botulinum toxin type A to reduce atrial fibrillation after cardiac surgery. Heart Rhythm. 2019;16(2):178–84.
Pokushalov E, Kozlov B, Romanov A, Strelnikov A, Bayramova S, Sergeevichev D, et al. Long-term suppression of atrial fibrillation by botulinum toxin injection into epicardial fat pads in patients undergoing cardiac surgery: one-year follow-up of a randomized pilot study. Circ Arrhythm Electrophysiol. 2015;8(6):1334–41.
Romanov A, Pokushalov E, Ponomarev D, Bayramova S, Shabanov V, Losik D, et al. Long-term suppression of atrial fibrillation by botulinum toxin injection into epicardial fat pads in patients undergoing cardiac surgery: three-year follow-up of a randomized study. Heart Rhythm. 2019;16(2):172–7.
Piccini JP, Ahlsson A, Dorian P, Gillinov MA, Kowey PR, Mack MJ, et al. Design and rationale of a phase 2 study of neurotoxin (botulinum toxin type A) for the PreVention of Post-Operative Atrial Fibrillation—the NOVA study. Am Heart J. 2022;245:51–9.
Abbvie. AbbVie announces late-breaking results from phase 2 exploratory NOVA trial of novel investigational neurotoxin AGN-151607 for the prevention of postoperative atrial fibrillation in cardiac surgery patients 2022. Available from: https://cardiologynownews.org/nova-no-significant-difference-in-rate-of-post-op-af-with-botulinum-toxisn-vs-placebo/.
Zhang S, Wang M, Jiao L, Liu C, Chen H, Zhou L, et al. Ultrasound-guided injection of botulinum toxin type A blocks cardiac sympathetic ganglion to improve cardiac remodeling in a large animal model of chronic myocardial infarction. Heart Rhythm. 2022;19(12):2095–104.
Molad Y. Update on colchicine and its mechanism of action. Curr Rheumatol Rep. 2002;4(3):252–6.
Li N, Brundel B. Inflammasomes and proteostasis novel molecular mechanisms associated with atrial fibrillation. Circ Res. 2020;127(1):73–90.
Misawa T, Takahama M, Kozaki T, Lee H, Zou J, Saitoh T, et al. Microtubule-driven spatial arrangement of mitochondria promotes activation of the NLRP3 inflammasome. Nat Immunol. 2013;14(5):454–60.
Imazio M, Nidorf M. Colchicine and the heart. Eur Heart J. 2021;42(28):2745–60.
Imazio M, Brucato A, Ferrazzi P, Rovere ME, Gandino A, Cemin R, et al. Colchicine reduces postoperative atrial fibrillation: results of the colchicine for the prevention of the postpericardiotomy syndrome (COPPS) atrial fibrillation substudy. Circulation. 2011;124(21):2290–5.
Deftereos S, Giannopoulos G, Panagopoulou V, Bouras G, Raisakis K, Kossyvakis C, et al. Anti-inflammatory treatment with colchicine in stable chronic heart failure: a prospective, randomized study. JACC Heart Fail. 2014;2(2):131–7.
Tabbalat RA, Hamad NM, Alhaddad IA, Hammoudeh A, Akasheh BF, Khader Y. Effect of ColchiciNe on the InciDence of atrial fibrillation in open heart surgery patients: END-AF trial. Am Heart J. 2016;178:102–7.
Zarpelon CS, Netto MC, Jorge JC, Fabris CC, Desengrini D, Jardim Mda S, et al. Colchicine to reduce atrial fibrillation in the postoperative period of myocardial revascularization. Arq Bras Cardiol. 2016;107(1):4–9.
Foretz M, Guigas B, Bertrand L, Pollak M, Viollet B. Metformin: from mechanisms of action to therapies. Cell Metab. 2014;20(6):953–66.
Ostropolets A, Elias PA, Reyes MV, Wan EY, Pajvani UB, Hripcsak G, et al. Metformin is associated with a lower risk of atrial fibrillation and ventricular arrhythmias compared with sulfonylureas: an observational study. Circ Arrhythm Electrophysiol. 2021;14(3): e009115.
Rangarajan S, Bone NB, Zmijewska AA, Jiang S, Park DW, Bernard K, et al. Metformin reverses established lung fibrosis in a bleomycin model. Nat Med. 2018;24(8):1121–7.
Lal JC, Mao C, Zhou Y, Gore-Panter SR, Rennison JH, Lovano BS, et al. Transcriptomics-based network medicine approach identifies metformin as a repurposable drug for atrial fibrillation. Cell Rep Med. 2022;3(10): 100749.
Vinciguerra M, Olier I, Ortega-Martorell S, Lip GYH. New use for an old drug: metformin and atrial fibrillation. Cell Rep Med. 2022;3(12): 100875.
Kawaji T, Ono K, Sowa N, Aizawa T, Hojo S, Yaku H, et al. Association between serum inflammatory biomarkers and atrial low voltage in patients with atrial fibrillation: a phase 1 FIB-MARK study. Int J Cardiol Heart Vasc. 2021;37: 100904.
Gawałko M, Kapłon-Cieślicka A, Hohl M, Dobrev D, Linz D. COVID-19 associated atrial fibrillation: incidence, putative mechanisms and potential clinical implications. Int J Cardiol Heart Vasc. 2020;30: 100631.
Cutler MJ, May HT, Bair TL, Crandall BG, Osborn JS, Miller JD, et al. Atrial fibrillation is a risk factor for major adverse cardiovascular events in COVID-19. Int J Cardiol Heart Vasc. 2022;43: 101127.
Heijman J, Muna AP, Veleva T, Molina CE, Sutanto H, Tekook M, et al. Atrial myocyte NLRP3/CaMKII nexus forms a substrate for postoperative atrial fibrillation. Circ Res. 2020;127(8):1036–55.
Dobrev D, Heijman J, Hiram R, Li N, Nattel S. Inflammatory signalling in atrial cardiomyocytes: a novel unifying principle in atrial fibrillation pathophysiology. Nat Rev Cardiol. 2023;20(3):145–67.
Scott L Jr, Li N, Dobrev D. Role of inflammatory signaling in atrial fibrillation. Int J Cardiol. 2019;287:195–200.
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377(12):1119–31.
Krisai P, Blum S, Schnabel RB, Sticherling C, Kühne M, von Felten S, et al. Canakinumab after electrical cardioversion in patients with persistent atrial fibrillation: a pilot randomized trial. Circ Arrhythm Electrophysiol. 2020;13(7): e008197.
Pandey AK, Okaj I, Kaur H, Belley-Cote EP, Wang J, Oraii A, et al. Sodium-glucose co-transporter inhibitors and atrial fibrillation: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. 2021;10(17): e022222.
Philippaert K, Kalyaanamoorthy S, Fatehi M, Long W, Soni S, Byrne NJ, et al. Cardiac late sodium channel current is a molecular target for the sodium/glucose cotransporter 2 inhibitor empagliflozin. Circulation. 2021;143(22):2188–204.
Hegyi B, Mira Hernandez J, Shen EY, Habibi NR, Bossuyt J, Bers DM. Empagliflozin reverses late Na+ current enhancement and cardiomyocyte proarrhythmia in a translational murine model of heart failure with preserved ejection fraction. Circulation. 2022;145(13):1029–31.
Sutanto H, Dobrev D, Heijman J. Angiotensin receptor-neprilysin inhibitor (ARNI) and cardiac arrhythmias. Int J Mol Sci. 2021;22(16).
Guerra F, Pimpini L, Flori M, Contadini D, Stronati G, Gioacchini F, et al. Sacubitril/valsartan reduces atrial fibrillation and supraventricular arrhythmias in patients with HFrEF and remote monitoring: preliminary data from the SAVE THE RHYTHM. Eur Heart J. 2020;41(Supplement_2).
De Vecchis R, Paccone A, Di Maio M. Favorable effects of sacubitril/valsartan on the peak atrial longitudinal strain in patients with chronic heart failure and a history of one or more episodes of atrial fibrillation: a retrospective cohort study. J Clin Med Res. 2020;12(2):100–7.
Martens P, Nuyens D, Rivero-Ayerza M, Van Herendael H, Vercammen J, Ceyssens W, et al. Sacubitril/valsartan reduces ventricular arrhythmias in parallel with left ventricular reverse remodeling in heart failure with reduced ejection fraction. Clin Res Cardiol. 2019;108(10):1074–82.
McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371(11):993–1004.
Rohde LE, Chatterjee NA, Vaduganathan M, Claggett B, Packer M, Desai AS, et al. Sacubitril/valsartan and sudden cardiac death according to implantable cardioverter-defibrillator use and heart failure cause: a PARADIGM-HF analysis. JACC Heart Fail. 2020;8(10):844–55.
de Diego C, González-Torres L, Núñez JM, Centurión Inda R, Martin-Langerwerf DA, Sangio AD, et al. Effects of angiotensin-neprilysin inhibition compared to angiotensin inhibition on ventricular arrhythmias in reduced ejection fraction patients under continuous remote monitoring of implantable defibrillator devices. Heart Rhythm. 2018;15(3):395–402.
Valentim Gonçalves A, Pereira-da-Silva T, Galrinho A, Rio P, Moura Branco L, Soares R, et al. Antiarrhythmic effect of sacubitril-valsartan: cause or consequence of clinical improvement? J Clin Med. 2019;8(6).
Fraser AG, Butchart EG, Szymański P, Caiani EG, Crosby S, Kearney P, et al. The need for transparency of clinical evidence for medical devices in Europe. Lancet. 2018;392(10146):521–30.
Teppo K, Jaakkola J, Biancari F, Halminen O, Linna M, Haukka J, et al. Socioeconomic disparities in use of rhythm control therapies in patients with incident atrial fibrillation: a Finnish Nationwide Cohort Study. Int J Cardiol Heart Vasc. 2022;41: 101070.
Kotecha D, Breithardt G, Camm AJ, Lip GYH, Schotten U, Ahlsson A, et al. Integrating new approaches to atrial fibrillation management: the 6th AFNET/EHRA consensus conference. Europace. 2018;20(3):395–407.
Patra JK, Das G, Fraceto LF, Campos EVR, Rodriguez-Torres MDP, Acosta-Torres LS, et al. Nano based drug delivery systems: recent developments and future prospects. J Nanobiotechnol. 2018;16(1):71.
Yang F, Xue J, Wang G, Diao Q. Nanoparticle-based drug delivery systems for the treatment of cardiovascular diseases. Front Pharmacol. 2022;13: 999404.
Galagudza M, Korolev D, Postnov V, Naumisheva E, Grigorova Y, Uskov I, et al. Passive targeting of ischemic-reperfused myocardium with adenosine-loaded silica nanoparticles. Int J Nanomed. 2012;7:1671–8.
Yao C, Veleva T, Scott L Jr, Cao S, Li L, Chen G, et al. Enhanced cardiomyocyte NLRP3 inflammasome signaling promotes atrial fibrillation. Circulation. 2018;138(20):2227–42.
Novo G, Guttilla D, Fazio G, Cooper D, Novo S. The role of the renin-angiotensin system in atrial fibrillation and the therapeutic effects of ACE-Is and ARBS. Br J Clin Pharmacol. 2008;66(3):345–51.
Mascolo A, Urbanek K, De Angelis A, Sessa M, Scavone C, Berrino L, et al. Angiotensin II and angiotensin 1–7: which is their role in atrial fibrillation? Heart Fail Rev. 2020;25(2):367–80.
Savelieva I, Kirchhof P, Danchin N, de Graeff PA, Camm AJ. Regulatory pathways for development of antiarrhythmic drugs for management of atrial fibrillation/flutter. Europace. 2011;13(8):1063–76.
Goette A, Kalman JM, Aguinaga L, Akar J, Cabrera JA, Chen SA, et al. EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterisation, and clinical implication. J Arrhythm. 2016;32(4):247–78.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. No external funding was used in the preparation of this manuscript. AS is supported by the Independent Research Fund Denmark (102900011B). JH is supported by the Netherlands Organization for Scientific Research (NWO/ZonMW Vidi 09150171910029). DD is supported by the National Institutes of Health (R01-HL131517, R01-HL136389, R01-HL089598, R01-HL163277, and R01-HL160992) and the European Union (large-scale integrative project MAESTRIA, No. 965286).
Conflict of interest
Dobromir Dobrev has obtained honoraria for educational lectures from Daiichi Sankyo and Novartis and for consultancy from AbbVie. Arnela Saljic and Jordi Heijman declare that they have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Data availability statement
Data sharing not applicable to this article as no datasets were generated.
Code availability
Not applicable.
Author contributions
All authors have participated in writing and reviewing this manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Saljic, A., Heijman, J. & Dobrev, D. Recent Advances in Antiarrhythmic Drug Therapy. Drugs 83, 1147–1160 (2023). https://doi.org/10.1007/s40265-023-01923-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-023-01923-3