Abstract
Although cardiovascular mortality has been decreasing in industrialized countries, there continues to be a substantial residual risk; thus, novel therapeutic agents and new targets of therapy have been sought. One highly plausible therapeutic target is high-density lipoprotein (HDL). HDL is a key player in reverse cholesterol transport and possesses a slew of other cardioprotective properties; however, recent trials with agents known to increase HDL levels have generally not shown any reduction in cardiovascular events. Further analysis of these trials suggest that fibrates have consistently reduced some cardiovascular outcomes, at least in the subgroup of patients with high serum triglycerides and low HDL cholesterol (HDLc) levels. Since fibrates, unlike niacin or cholesterol ester transfer protein inhibitors, increase HDLc level mostly through the stimulation of apolipoprotein A-I production, it is suggested that the quality and functionality of HDL are enhanced when de novo synthesis rather than inhibition of turnover is the mechanism of increasing HDL level. In this communication, the evidence for and against the cardioprotective properties of HDL is reviewed and the contemporary clinical trials are discussed.

Similar content being viewed by others
References
Rosenson RS, Brewer HB Jr, Davidson WS, Fayad ZA, Fuster V, Goldstein J, et al. Cholesterol efflux and atherprotection: advancing the concept of reverse cholesterol transport. Circulation. 2012;125:1905–19.
Alwalli K, Awan Z, Alshahrani A, Genest J. High-density lipoproteins and cardiovascular disease: 2010 update. Expert Rev Cardiovasc Ther. 2010;8:413–23.
Barter P. HDL-C: role as a risk modifier. Atherosclerosis Suppl. 2011;12:267–70.
Soran H, Hama S, Yadav R, Durrington PN. HDL functionality. Curr Opin Lipidol. 2012;23:353–66.
Gordon DJ, Rifkind BM. High-density lipoprotein-the clinical implications of recent studies. N Engl J Med. 1989;321:1311–6.
Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, Treating to New Targets Investigators, et al. HDL cholesterol very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med. 2007;357:1301–10.
Iatan I, Palmyre A, Alrasheed S, Ruel I, Genest J. Genetics of cholesterol efflux. Curr Atheroscler Rep. 2012;14:235–46.
Calabresi L, Simonelli S, Gomaraschi M, Franceschini G. Genetic lecithin: cholesterol acyltransferase deficiency and cardiovascular disease. Atherosclerosis. 2012;222:299–306.
Rubin EM, Krauss RM, Spangler EA, Verstuyft JG, Clift SM. Inhibition of early atherogenesis in transgenic mice by human apolipoprotein AI. Nature. 1991;353:265–7.
Plump AS, Scott CJ, Breslow JL. Human apolipoprotein A-I gene expression increases high-density lipoprotein and suppresses atherosclerosis in the apolipoprotein E deficient mouse. Proc Natl Acad Sci. 1994;91:9607–11.
Duverger N, Kruth H, Emmanuel F, Caillaud JM, Viglietta C, Castro G, et al. Inhibition of atherosclerosis development in cholesterol-fed human apolipoprotein A-I-transgenic rabbits. Circulation. 1996;94:713–7.
Benoit P, Emmanuel F, Cailaud JM, Bassinet L, Castro G, Gallix P, et al. Somatic gene transfer of human apo A-I inhibits atherosclerosis progression in mouse models. Circulation. 1999;99:105–10.
Tangirala RK, Tsukamoto K, Chun SH, Usher D, Puré E, Rader DJ. Regression of atherosclerosis induced by liver-directed gene transfer of apolipoprotein A-I in mice. Circulation. 1999;100:1816–22.
Nissen SE, Tsunoda T, Tuzcu EM, Schoenhagen P, Cooper CJ, Yasin M, et al. Effect of recombinant apo A-I Milano on coronary atherosclerosis in patients with acute coronary syndromes: a randomized controlled trial. JAMA. 2003;290:2292–300.
Nissen SE, Tuzcu EM, Schoenhagen P, Brown BG, Ganz P, Vogel RA, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA. 2004;291:1071–80.
Tardif JC, Ballantyne CM, Barter P, Dasseux JL, Fayad ZA, Guertin MC, et al. Can HDL Infusions Significantly QUicken Atherosclerosis REgression (CHI-SQUARE) Investigators. Effects of the high-density lipoprotein mimetic agent CER-001 on coronary atherosclerosis in patients with acute coronary syndromes: a randomized trial. Eur Heart J. 2014;35:3277–86.
Tardif JC, Grégoire J, L’Allier PL, Ibrahim R, Lespérance J, Heinonen TM, et al. Effect of rHDL on Atherosclerosis-Safety and Efficacy (ERASE) Investigators. Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: a randomized controlled trial. JAMA. 2007;297:1675–82.
Rubins HB, Rogins SJ, Collins D, Fye CL, Anderson JW, Elam MB, et al. Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial Study Group. Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. N Engl J Med. 1999;341:410–8.
Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, et al. Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med. 1987;317:1237–45.
Brunner D, Agmon J, Kaplinsky E. Secondary prevention by raising HDL cholesterol and reducing triglycerides in patients with coronary artery disease. Circulation. 2000;102:21–7.
Goldenberg I, Benderly M. Goldbourt U; BIP Study Group. Secondary prevention with bezafibrate therapy for the treatment of dyslipidemia: an extended follow-up of the BIP trial. J Am Coll Cardiol. 2008;51:459–65.
Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, et al. FIELD study investigators. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet. 2005;366:1849–61.
ACCORD Study Group, Ginsberg HN, Elam MB, Lovato LC, Crouse JR 3rd, Leiter LA, Linz P, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010;362:1563–74.
Newman AB, Glynn NW, Taylor CA, Sebastiani P, Perls TT, Mayeux R, et al. Health and function of participants in the Long Live Family Study: a comparison with other cohorts. Aging (Albany NY). 2011;3:63–76.
Rahilly-Tierney CR, Spiro A 3rd, Vokonas P, Gasiano JM. Relation between high-density lipoprotein cholesterol and survival to age 85 years in men (from the VA normative aging study). Am J Cardiol. 2011;107:1173–7.
Odden MC, Shilipak MG, Whitson HE, Katz R, Kearney PM, Defilippi C, et al. Risk factors for cardiovascular disease across the spectrum of older age: the Cardiovascular Health Study. Atherosclerosis. 2014;237:336–42.
Voight BF, Peloso GM, Orho-Melander M, Frikke-Schmidt R, Barbalic M, Jensen MK, et al. Plasma HDL cholesterol and risk of myocardial infarction: a Mendelian randomization study. Lancet. 2012;380:572–80.
Haase CL, Tybjærg-Hansen A, Qayyum AA, Schou J, Nordestgaard BG, Frikke-Schmidt R. LCAT, HDL cholesterol, and ischemic cardiovascular disease: a Mendelian randomization study of HDL cholesterol in 54,500 individuals. J Clin Endocrinol Metabol. 2012;97:E248–56.
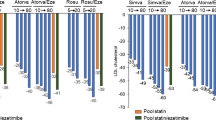
LaRosa JC, Grundy SM, Waters DD, Shear C, Barter P, Fruchart JC, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352:1425–35.
Ridker PM, Danielson E, Fonseca FAH, Genest J, Gotto AM, Kastelein JJP, for the JUPITER Study Group, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–207.
AIM-HIGH Investigators, Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, Koprowicz K, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365:2255–67.
HPS2-THRIVE Collaborative Group, Landray MJ, Haynes R, Hopewell JC, Parish S, Aung T, Tomson J, et al. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371:203–12.
Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, ILLUMINATE Investigators, et al. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357:2109–22.
Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367:2089–99.
Fayad ZA, Mani V, Woodward M, Kallend D, Abt M, Burgess T, the dal-PLAQUE Investigators, et al. Safety and efficacy of dalcetrapib on atherosclerotic disease using novel non-invasive multimodality imaging (dal-PLAQUE): a randomized clinical trial. Lancet. 2011;378:1547–59.
Luscher TF, Taddei S, Kaski JC, Jukema JW, Kallend D, Munzel T, the dal-VESSEL Investigators, et al. Vascular effects and safety of dalcetrapib in patients with or at risk of coronary heart disease: the dal-VESSEL randomized clinical trial. Eur Heart J. 2012;33:857–65.
Hooper AJ, Burnett JR. Dalcetrapib, a cholesterol ester transfer protein modulator. Drugs. 2012;21:1427–32.
Niesor EJ. Different effects of compounds decreasing cholesteryl ester transfer protein activity on lipoprotein metabolism. Curr Opin Lipidol. 2011;22:288–95.
Hu X, Dietz JD, Xia C, Knight DR, Loging WT, Smith AH, et al. Torcetrapib induces aldosterone and cortisol production by an intracellular calcium-mediated mechanism independently of cholesteryl ester transfer protein inhibition. Endocrinol. 2009;150:2211–9.
Nicholls SJ, Tizcu EM, Brennan DM, Tardif JC, Nissen SE. Cholesteryl ester transfer protein inhibition, high-density lipoprotein raising, and progression of coronary atherosclerosis: insights from ILLUSTRATE (Investigation of Lipid Level Management Using Coronary Ultrasound to Assess Reduction of Atherosclerosis by CETP Inhibition and HDL Elevation). Circulation. 2008;118:2506–14.
Barter PJ, Brandrup-Wognsen G, Palmer MK, Nicholls SJ. Effect of statins on HDLc: a complex process unrelated to changes in LDLc: analysis of the VOYAGER Database. J Lipid Res. 2010;51:1546–53.
Ridker PM, Genest J, Bockholdt SM, Libby P, Gotto AM, Nordestgaard BG, the JUPITER Trial Study Group, et al. HDL cholesterol and residual risk of first cardiovascular events after treatment with potent statin therapy: an analysis from the JUPITER trial. Lancet. 2010;376:333–9.
Aronoff S, Rosenblatt S, Braithwaite S, Egan JW, Mathisen AL, Schneider RL. Pioglitazone hydrochloride monotherapy improves glycemic control in the treatment of diabetes: a 6-month study randomized placebo-controlled dose-response study. The Pioglitazone 001 Study Group. Diabetes Care. 2000;23:1605–11.
Dormandy JA, Charbonnel B, Ekland DJ, Erdmann E, Massi-Benedetti M, Moules IK, PROactive investigators, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitazone Clinical Trial in MacroVascular Events): a randomized controlled trial. Lancet. 2005;366:1279–89.
Singh IM, Shishehbor MH, Ansell BJ. High-density lipoprotein as a therapeutic target: a systematic review. JAMA. 2007;298:786–98.
Lamon-Fava LH, Diffenderfer MR, Barrett PH, Buchsbaum A, Nyaku M, Horvath KV, et al. Extended-release niacin alters the metabolism of plasma apolipoprotein (apo) A-I and apoB-containing lipoproteins. Arterioscler Thromb Vasc Biol. 2008;28:1672–8.
Haas MJ, Razzak-Alamir A, Sultan S, Chehade JM, Wong NCW, Mooradian AD. Nicotinic acid induces apo A-I gene expression in HepG2 and Caco-2 cell lines. Metabolism. 2011;60:1790–6.
Vu-Dac N, Schoonjans K, Laine B, Fruchart JC, Auwerx J, Staels B. Negative regulation of the human apolipoprotein A-I promoter by fibrates can be attenuated by the interaction of the peroxisome proliferator-activated receptor with its response element. J Biol Chem. 1994;269:31012–8.
Vu-Dac N, Chopin-Delannoy S, Gervois P, Bonnelye E, Martin G, Fruchart JC, et al. The nuclear receptors peroxisome proliferator-activated receptor α and Rev-erbα mediate the species-specific regulation of apolipoprotein A-I expression by fibrates. J Biol Chem. 1998;273:25713–20.
Staels B, Dallongeville J, Auwerx J, Schoonjans K, Leitersdorf E, Fruchart JC. Mechanism of action of fibrates on lipid and lipoprotein metabolism. Circulation. 1998;98:2088–93.
Pineda Torra I, Gervois P, Staels B. Peroxisome proliferator-activated receptor alpha in metabolic disease, inflammation, and atherosclerosis. Curr Opin Lipidol. 1999;10:151–9.
Marx N, Duez H, Fruchart J-C, Staels B. Peroxisome proliferator-activated receptors and atherogenesis. Regulators of gene expression in vascular cells. Circ Res. 2004;94:1168–78.
Savage DB. PPAR gamma as a metabolic regulator: insights from genomics and pharmacology. Expert Rev Mol Med. 2005;7:1–16.
Sakamoto J, Kimura H, Moriyama S, Odaka H, Momose Y, Sugiyama Y, et al. Activation of human peroxisome proliferator-activated receptor (PPAR) subtypes by pioglitazone. Biochem Biophys Res Commun. 2000;278:704–11.
McNeish J, Aiello RJ, Guyot D, Turi T, Gabel C, Aldinger C, et al. High density lipoprotein deficiency and foam cell accumulation in mice with targeted disruption of ATP-binding cassette tranporter-1. Proc Natl Acad Sci. 2000;97:4245–50.
Wang N, Lan D, Chen W, Matsuura F, Tall AR. Specific binding of ApoA-I, enhanced cholesterol efflux, and altered plasma membrane morphology in cells expressing ABCA1. J Biol Chem. 2000;275:33053–8.
Shao B, Cavigiolio G, Brot N, Oda MN, Heinecke JW. Methionine oxidation impairs reverse cholesterol transport by apolipoprotein A-I. Proc Natl Acad Sci. 2008;105:12224–9.
Shao B, Pennathur S, Pagani I, Oda MN, Witztum JL, Oram JF, et al. Modifying apolipoprotein A-I by malondialdehyde, but not by an array of other reactive carbonyls, blocks cholesterol efflux by the ABCA1 pathway. J Biol Chem. 2010;285:18473–84.
Undurti A, Huang Y, Lupica JA, Smith JD, DiDonato JA, Hazen SL. Modification of high density lipoprotein by myeloperoxidase generates a pro-inflammatory particle. J Biol Chem. 2009;284:30825–35.
Zhang M, Gao X, Wu J, Liu D, Cai H, Fu L, et al. Oxidized high-density lipoprotein enhances inflammatory activity in rat mesangial cells. Diabetes Metabol Res Rev. 2010;26:455–63.
Oram JF. Receptor-mediated transport of cholesterol between cultured cells and high-density lipoproteins. Methods Enzymol. 1986;129:645–59.
Cockerill GW, Rye KA, Gamble JR, Vadas MA, Barter PJ. High-density lipoproteins inhibit cytokine-induced expression of endothelial cells adhesion molecules. Arterioscler Thromb Vasc Biol. 1995;15:1987–94.
Zheng L, Nukuna B, Brennan ML, Sun M, Goormastic M, Settle M, et al. Apolipoprotein A-I is a selective target for myeloperoxidase-catalyzed oxidiation and functional impairment in subjects with cardiovascular disease. J Clin Invest. 2004;114:529–41.
Toth PP, Barter PJ, Rosenson RS, Boden WE, Chapman MJ, Cuchel M, et al. High-density lipoproteins: a consensus statement from the National Lipid Association. J Clin Lipidol. 2013;7:484–525.
Lincoff AM, Tardif JC, Schwartz GG, Nicholls SJ, Rydén L, Neal B, AleCardio Investigators, et al. Effect of aleglitazar on cardiovascular outcomes after acute coronary syndrome in patients with type 2 diabetes mellitus: the AleCardio randomized clinical trial. JAMA. 2014;311:1515–25.
Doggrell SA. Muraglitazar: beneficial or detrimental in the treatment of type 2 diabetes? Expert Opin Pharmacother. 2006;7:1229–33.
Fievet C, Fruchart JC, Staels B. PPARα and PPARγ dual agonists for the treatment of type 2 dibetes and the metabolic syndrome. Curr Opin Pharmacol. 2007;6:606–14.
Pai V, Paneerselvam A, Mukhopadhyay S, et al. A multicenter, prospective, randomized, double-blind study to evaluate the safety and efficacy of saroglitazar 2 and 4 mg compared to pioglitazone 45 mg in diabetic dyslipidemia (PRESS V). Diabetes Sci Technol. 2014;8:132–41.
Jani RH, Pai V, Jha P, et al. A multicenter, prospective, randomized, double-blind study to evaluate the safety and efficacy of Saroglitazar 2 and 4 mg compared with placebo in type 2 diabetes mellitus patients having hypertriglyceridemia not controlled with atorvastatin therapy (PRESS VI). Diabetes Technol Ther. 2014;16:63–71.
Jani RH, Kansagra K, Jain MR, et al. Pharmacokinetics, safety, and tolerability of saroglitazar (ZYH1), a predominantly PPARα agonist with moderate PPARγ agonist activity in healthy human subjects. Clin Drug Investig. 2013;33:809–16.
Bailey D, Jahagirdar R, Gordon A, Hafiane A, Campbell S, Chatur S, et al. RVX-208: a small molecule that increases apolipoprotein A-I and high-density lipoprotein cholesterol in vitro and in vivo. J Am Coll Cardiol. 2010;55:2580–9.
Picaud S, Wells C, Felletar I, Brotherton D, Martin S, Savitsky P, et al. RVX-208, an inhibitor of BET transcriptional regulators with selectivity for the second bromodomain. Proc Natl Acad Sci. 2013;110:19754–9.
Nicholls SJ, Gordon A, Johannson J, Ballantyne CM, Barter PJ, Brewer HB, et al. ApoA-I induction as a potential cardioprotective strategy: rationale for the SUSTAIN and ASSURE studies. Cardiovasc Drugs Ther. 2012;26:181–7.
Resverlogix. Further analysis of the ASSURE data finds a responder group for RVX-208 with statistically significant regression of coronary atherosclerosis [press release]. 2013. Available at: http://www.resverlogix.com/media/press-release.html?id=492. Accessed 6 Mar 2015.
Resverlogix. RVX-208 leads to a 77 % relative risk reduction of major adverse cardiovascular events (MACE) in patients with diabetes mellitus [press release]. 2014. Available at: http://www.resverlogix.com/media/press-release.html?id=508. Accessed 6 Mar 2015.
Resverlogix. Resverlogix presents at Biotech Showcase during JP Morgan week [press release]. 2015. Available at: http://www.resverlogix.com/media/press-release.html?id=512. Accessed 6 Mar 2015.
Navab M, Schechter I, Anantharamaiah GM, et al. Structure and function of HDL mimetics. Arterioscler Thromb Vasc Biol. 2010;30:164–8.
Haas MJ, Mooradian AD. Therapeutic interventions to enhance apolipoprotein A-I-mediated cardioprotection. Drugs. 2010;70:805–21.
Disclosures
No external funding was used in the preparation of this manuscript. Arshag D. Mooradian and Michael J. Haas have no potential conflicts of interest that might be relevant to the contents of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mooradian, A.D., Haas, M.J. Targeting High-Density Lipoproteins: Increasing De Novo Production Versus Decreasing Clearance. Drugs 75, 713–722 (2015). https://doi.org/10.1007/s40265-015-0390-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-015-0390-1