Abstract
Introduction
The Food and Drug Administration Adverse Event Reporting System (FAERS) is a vital source of new drug safety information, but whether adverse event (AE) information collected from these systems adequately captures experiences of the overall United States (US) population is unknown.
Objective
To examine determinants of consumer AE reporting in the USA.
Methods
Five-year AE reporting rate per 100,000 residents per US county were calculated, mapped, and quartiled for AE reports received directly from consumers between 2011 and 2015. Associations between county-level sociodemographic factors obtained from County Health Rankings and AE reporting rates were evaluated using negative binomial regression.
Results
Reporting rates were variable across US counties with > 17.6 reports versus ≤ 5.5 reports/100,000 residents in the highest and lowest reporting quartile, respectively. Controlling for drug utilization, counties with higher reporting rates had higher proportions of individuals age ≥ 65 years (e.g., 2.4% reporting increase per 1% increase in individuals age > 65, incidence rate ratio (IRR): 1.024, 95% confidence interval (CI): 1.017–1.030), higher proportions of females (IRR: 1.027, 95% CI 1.012–1.043), uninsured (IRR: 1.009, 95% CI 1.005–1.013), higher median log household incomes (IRR: 1.897, 95% CI 1.644–2.189) and more mental health providers per 100,000 residents (IRR: 1.003, 95% CI 1.001–1.004). Lower reporting was observed in counties with higher proportions of individuals age ≤ 18 years (IRR: 0.966, 95% CI 0.959–0.974), American Indian or Alaska Native individuals (IRR: 0.991, 95% CI 0.986–0.996), individuals not proficient in English (IRR: 0.978, 95% CI 0.965–0.991), and individuals residing in rural areas within a county (IRR: 0.998, 95% CI 0.997–0.998).
Conclusions
Observed variations in consumer AE reporting may be related to sociodemographic factors and healthcare access. Because these factors may also correspond to AE susceptibility, voluntary AE reporting systems may be suboptimal for capturing emerging drug safety concerns among more vulnerable populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Findings from this study support targeted efforts to improve engagement in AE reporting systems. |
Because health disparities appear to extend to reporting AEs, complementary data sources are needed for monitoring the safety of medicines among more vulnerable populations. |
1 Introduction
The primary purpose of a postmarket drug safety surveillance system is to identify adverse drug reactions (ADRs) that were unobserved during the pre-approval clinical trials and to evaluate those events for further follow-up in formal drug safety studies or regulatory action [1]. Postmarketing surveillance is necessary because real-world populations are generally more diverse demographically, commonly have more co-morbidities, and may take more concomitant medications than those studied in pre-approval clinical trials. Studies have documented that patients in clinical trials are not representative of all patients who use the drug once it is marketed [2]. In most studies that have compared patients in clinical trials to real-world patients, those in the real world tend to be older, more frequently female, and have poorer prognoses. In the United States (USA), these findings have been documented in clinical areas as diverse as cardiology, mental health, and oncology, underscoring the need for data from real-world experiences as a critical component in drug safety surveillance [3,4,5,6]. In addition, the much large number of patients in the real world who use a drug potentially far beyond the follow-up periods in clinical trials allows for detection of rare or long-latency ADRs [7].
While large administrative healthcare claims databases, electronic health records, and other data sources are increasingly providing safety information on marketed medical products, spontaneous reporting of adverse events (AEs) remains an integral part of monitoring the safety of medical products [8,9,10,11]. In the USA, the Food and Drug Administration (FDA) Adverse Event Reporting System (FAERS) is a repository of reports of AEs associated with drug and biological products. FAERS relies on the public—healthcare professionals, patients, caregivers, and others—to voluntarily report AEs either directly to the FDA through the MedWatch program, or to the product’s manufacturer, which must submit these reports to the FDA according to regulatory requirements [12, 13]. Although the value of reporting by non-clinicians has previously been challenged, more recent published evaluations suggest that consumer reporting makes a positive contribution to the general knowledge about ADRs [14, 15]. Several studies have demonstrated that consumer reports produce unique, informative, and early safety signals [14,15,16,17,18,19,20]. Consumers are also more likely than healthcare professionals to report information about symptoms and patient-centered aspects such as the emotional, occupational, or social consequences of ADRs [21].
To generalize findings from surveillance data to the population at-large, reporting systems aimed at identifying new safety information should be reflective of those receiving the medicines [22]. The voluntary nature of reporting to spontaneous reporting systems such as FAERS results in significant under-reporting and little is known about how sociodemographic factors may impact the likelihood of reporting [21, 23, 24]. Pervasive disparities exist in healthcare across different US geographies, socioeconomic groups, and race and ethnicity groups [25,26,27]. Specific to medications, differences in prescribing and adherence not attributable to clinical appropriateness or patient preferences are present across a range of illnesses [28, 29]. The factors contributing to healthcare utilization are complex and multifactorial, and may expand to patients’ ability or willingness to report AEs. If AE reporting is not representative of the general population and is associated with development of ADRs, then signal detection could be biased and potentially miss drug safety problems specific to vulnerable populations. The identification of sociodemographic factors associated with under-reporting may also inform the development of tailored interventions to increase AE reporting. We therefore sought to examine the association between county-level sociodemographic factors and AE reporting.
2 Methods
2.1 Data Sources
2.1.1 Adverse Event (AE) Reports in the Food and Drug Administration Adverse Event Reporting System (FAERS) by US County
FAERS is a database containing over 25 million AE reports (1969–2022) supporting the US FDA’s postmarketing safety surveillance of drug and non-vaccine biologic products [30]. Each AE report describes the experience of an individual person after taking a drug or therapeutic biological product. The FAERS data structure adheres to the international safety reporting guidance issued by the International Council on Harmonisation and utilizes the Medical Dictionary for Regulatory Activities (MedDRA) to code AEs [31]. Approximately 95% of reports come to the FDA via manufacturers of drugs and biologics; the remaining 5% come directly to the FDA from consumers, healthcare professionals (HCPs), and others, including, in some cases, organizations other than manufacturers.
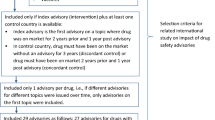
For this study we extracted all FAERS reports with an FDA initial received date from 1 January 2011 through 31 December 2015 submitted by consumers directly to the FDA. Reporter type (i.e., consumer, HCP, or other) was determined using the health professional and occupation fields from the reporting form [32]. We limited our analysis to consumer reports submitted by individuals directly to the FDA for several reasons. First, geographic identifiers in reports submitted by manufacturers are typically limited to the country-level and are otherwise generally listed as “private” in accordance with individual manufacturer’s standard operating procedures. Second, manufacturer reports may have multiple reporters because of follow-up sought by manufacturers (e.g., a manufacturer may contact the patient and subsequently the patient’s HCP for additional information regarding a potential ADR). This can result in multiple discordant reporter addresses pertaining to the same AE report. Third, we excluded direct reports from certain organizations because they do not reflect the spontaneous reporting of an AE but rather may be submitted based on established agreements between the FDA and the organization, submitted in batches, or as a result of planned contact with consumers. Fourth, reports from HCPs were excluded because of clustering of reporting from large treatment facilities and those with institution-specific reporting procedures, such as the use of drug information centers or committees that curate reports and routinely submit them on behalf of their organization.
Because US county is not reported to FAERS, we geocoded reports with complete address information and aggregated them by county using ArcGIS 10.3 (Environmental Systems Research Institute, Inc., Redlands, CA, USA). Reports missing street-level addresses but containing a ZIP code were assigned to counties using the US Department of Housing and Urban Development’s (HUD) 2015 residential crosswalk data, which relates US Postal Service Zone Improvement Plan (ZIP) codes to Census Bureau geographies [33]. If a ZIP code was associated with only one county, all reports listing that ZIP code were assigned to that county. To assign reports that listed a ZIP code that spans multiple counties to each of the associated counties, the total number of reports for the ZIP code was multiplied by the residential ratio (residential addresses in the county associated with the ZIP/the total number of residential addresses associated with that ZIP code) for each of the associated counties.
2.1.2 US County-Level Sociodemographic and Prescription Data
Individual reporter-level sociodemographic data are not collected in the MedWatch form outside of occupation and address; therefore, county-level measures were ascribed to reporters using geographic linkage. County-level factors included demographics (age, sex, race, and ethnicity), educational attainment, English language proficiency, insurance status, health resources, health status, income, rurality, and prescription drug utilization. The County Health Rankings and Roadmaps Program Data, created through collaboration between the Robert Wood Johnson Foundation and the University of Wisconsin Population Health Institute, was the source of sociodemographic county-level information [34]. The dataset includes measures gathered from several underlying data sources (e.g., US Census Bureau, American Community Survey). Online Supplementary Materials (OSM) Table 1 provides the definition and source of each factor.
Symphony Health Integrated Dataverse (IDV®) was used to determine total prescription fills dispensed from retail pharmacies based on prescriber ZIP codes. The annual numbers of prescriptions assigned to each US county were then aggregated across the study period (2011–2015). This data repository represents approximately 93% of all US retail prescription fills and is projected to national and sub-national levels [35].
2.2 Statistical Analyses
For each county, we estimated a reporting rate per 100,000 residents using the number of direct consumer reports received between 2011 and 2015 as the numerator, and the corresponding county population as the denominator. For descriptive purposes, we cross-tabulated potential county-level determinants of reporting rates, categorized into quartiles. For each factor evaluated, the average of the populations in areas of high reporting (highest reporting rate quartile) was compared to that in areas of low reporting (lowest reporting rate quartile) using Chi-square and t-tests. We repeated the quartile analysis by limiting it to counties with more than 20,000 residents as a sensitivity analysis.
To further explore the association between reporting rates and county-level factors, we conducted a descriptive spatial analysis of reporting in a single state, Texas. We illustrated trends by mapping the quartiles of the factors that demonstrated differences between counties in the highest reporting quartile and those in the lowest reporting quartile. We chose Texas for two reasons: (1) Texas has 254 counties, more than any other state, allowing for a large sample of counties, and (2) Texas has 32 counties located along the US-Mexico border and consequently has unique demographic factors. In 89 counties across the USA, 10% or more of the population aged 5 years and over speak English less than “well.” Texas accounts for 38 (42%) of these counties, most of which are in close proximity to the US-Mexico border [36]. The absence of a Spanish version of the MedWatch form during this study period has been cited as a potential barrier to consumer reporting [37].
Finally, we conducted a multivariate analysis using all US counties to evaluate county-level determinants of reporting including all previously described county-level sociodemographic and healthcare variables as well as the number of dispensed prescriptions per number of residents. Missing data for the number of primary-care physicians (132 counties) and mental health providers (287 counties) was imputed with estimates from regression models consisting of the other determinants evaluated and county population. We used a negative binomial model with a log(Population) offset and robust standard errors to estimate associations between county-level determinants of reporting and report counts as incidence rate ratios (IRRs) with corresponding 95% confidence intervals (CIs) using R Statistical Software (v4.1.2).
3 Results
We identified 52,430 direct consumer reports (33% of all direct reports) from 2011 to 2015. Using the full address, 45,738 reports (87.3%) were geocoded and 1616 reports (3%) were assigned to counties using their ZIP codes, yielding a total of 47,354 reports (90.3%) with a geographic match. Of the 3136 counties evaluated in the USA, 611 counties (19.5%, median population = 6572) had no direct consumer reports in FAERS. Forty-one of these counties had a population of greater than 20,000, two had a population greater than 50,000, and none had a population greater than 100,000.
Overall, there were 14.7 geocoded reports per 100,000 US residents. The median number of reports per 100,000 residents across all counties was 12.1 (Table 1), and ranged from 0 to 262. The top 10 counties with the highest reporting rates had fewer than 20,000 residents. US counties were aggregated by reporting rate quartiles with the lowest reporting quartile: Q1 having counties with ≤ 5.5 reports per 100,000 residents, Q2 having counties with > 5.5–12.1 reports per 100,000 residents, Q3 having counties with > 12.1–17.6 reports per 100,000 residents, and Q4 having counties with > 17.6 reports per 100,000 residents. Figure 1 displays the observed AE reports per 100,000 residents for all US counties. Counties in the highest reporting quartile had significantly lower proportions of Hispanic or Latino residents (6.5 vs. 11.8%, p < 0.01), American Indian or Alaska Native residents (1.5 vs. 4.0%, p < 0.01), and residents residing in rural areas within a county (57.7 vs. 75.4%, p < 0.01) than counties in the lowest reporting quartile. Counties in the highest reporting quartile also had higher proportions of White individuals (81.7 vs. 74.0%, p < 0.01), higher household incomes ($50,506 vs. $45,651, p < 0.01), more primary-care physicians per 100,000 residents (642 vs. 437, p < 0.01), more mental health providers per 100,000 residents (1508 vs. 951, p < 0.01), and more prescription fills dispensed per resident over 5 years (58.2 vs. 44.2, p < 0.01) than counties in the lowest reporting quartile. The proportion of residents with some college education was higher in the highest reporting quartile than in the lowest, though this difference did not reach statistical significance (59.1 vs. 54.4%, p < 0.06).
When restricting quartile comparisons to counties with more than 20,000 residents (1301 counties excluded), the patterns observed across quartiles were consistent with the results using all counties (OSM Table 2). The median number of reports per 100,000 residents across all counties was 13.5 reports and ranged from 0 to 59 reports. One additional variable became statistically significant, Black or African American race, with a lower proportion of Black or African American residents in the highest reporting quartile than in the lowest (7.9 vs. 12.4%, p = 0.02).
Descriptive maps of Texas county-level reporting per 100,000 residents and county factors by quartile are presented in Fig. 2. Counties situated along the US-Mexico border were commonly in the lowest quartiles of reporting. These counties generally had the highest percentage of Hispanic or Latino residents, lowest percentage of English proficiency, highest percentage of fair/poor health, and lower household incomes. The northernmost counties located between New Mexico and Oklahoma were also generally associated with lower quartiles of reporting. These counties tended to have a higher extent of their residents living in rural areas and higher proportions of uninsured residents.
Observed direct consumer adverse events reported to the Food and Drug Administration (FDA) Adverse Event Reporting System per 100,000 Texas residents between 1 January 2011 and 31 December 2015. The largest panel provides the county-level reporting ratio divided into quartiles for comparison to the smaller panels of individual county factors divided into quartiles
In the multivariate model, we noted several county-level variables that were associated with AE reporting rates. An increase of the percentage of the population that was age ≥ 65 years by one percent point resulted in a 2.4% increase in AE reporting rates (IRR: 1.024, 95% CI 1.017–1.030, Table 2). Counties with a higher proportion of female residents (IRR: 1.027, 95% CI 1.012–1.043), uninsured (IRR: 1.009, 95% CI 1.005–1.013), and more mental health providers were also associated with more reports (IRR: 1.003 95% CI 1.001–1.004, respectively). Counties with higher median log household incomes had higher reporting rates (IRR: 1.897, 95% CI 1.644–2.189). Using the median reporting rate observed across the US, a county with 250,000 individuals is estimated to contribute 30 AE reports. If this county exhibits median national income ($46,788), then an increase in income of $10,000 (21.4%) would increase reporting from 30 to 34 reports (13% increase) based on our multivariate model.
Lower reporting was observed among counties with a higher percentage of the population that was ≤ 18 years of age (IRR: 0.966, 95% CI 0.959–0.974), American Indian or Alaska Native (IRR: 0.991, 95% CI 0.986–0.996), not proficient in English (IRR: 0.978, 95% CI 0.965–0.991), and living in rural areas within a county (IRR: 0.998, 95% CI 0.997–0.998). The number of dispensed prescriptions dispensed per county resident had no association with reporting (IRR: 1.0, 95% CI 0.999–1.001).
4 Discussion
The FDA’s national, passive surveillance system shows considerable variability in direct consumer AE reporting at the county level and suggests that sociodemographic context is an important determinant of this heterogeneity. Counties in the highest reporting quartile had reporting rates that were three times higher than counties in the lowest reporting quartile. Low reporting was associated with higher proportions of Hispanic or Latino and American Indian or Alaska Native individuals, as well as lower median incomes and fewer healthcare providers per county resident. While ecological studies cannot determine a causal relationship between sociodemographic factors and AE reporting, we identified several factors that may have important implications for the representativeness of FAERS data and, by extension, on the sensitivity of this AE surveillance system to detect signals of AEs in specific populations.
Some of the observed patterns suggest that variability in reporting could be attributable to differences in engagement in reporting, which includes both awareness of the reporting system and ability to use it [24]. Awareness is a commonly cited barrier to AE reporting despite required statements on how to report AEs to the FDA on all outpatient drug prescriptions dispensed and in direct-to-consumer advertisements [38, 39]. Living in a county with higher English language proficiency and college education was associated with higher reporting, perhaps corresponding to higher health literacy [40, 41]. Using the observed US median reporting rate and our model, a county with 250,000 individuals is estimated to contribute 30 AE reports; with all other factors constant, if the county had a 10% lower English proficiency the county would contribute 24 reports, a 20% reduction in reporting. Our subanalysis of Texas also provided a compelling suggestion that language may be a significant factor for some populations, although this analysis was not intended to determine causal factors. An estimated 31% of Starr County, Texas (population 61,962), which is situated on the US-Mexico border, is not proficient in English (compared to 8% overall in Texas). This was the second largest US county with no AE reports during the study period. In 2019, the FDA made available a Spanish-language version of the form and online consumer reporting website, but its impact has not been assessed [42, 43]. Consumers with limited English and Spanish proficiency may need to rely on external translation services, such as web browser tools, as reporting forms are currently available only in these two languages.
Less access to HCPs and community health resources may also explain our observation of lower reporting in counties with larger rural populations and counties with lower household incomes. Rural areas also tend to have larger proportions of individuals who are less likely to have a college degree relative to an urban population [44]. Our findings that reporting rates may be influenced by healthcare access and economic resources align with a country-level study conducted by Inácio et al. [45]. Using data from 44 countries, the study found factors such as per capital public health expenditure were relevant for identifying countries with higher reporting rates. We also observed differences in reporting by a county’s racial composition when controlling for other variables. This finding is consistent with observations in other healthcare domains [46]. The largest county with no AE reports in our study was McKinley County, New Mexico (population 73,308), which is the largest US county with a majority American Indian population, with 77% of residents identifying as American Indian or Alaska Native. Our results suggest the reporting variability may be attributable to a higher frequency of AEs in certain populations. Specifically, when controlling for drug utilization and other variables, we found higher proportions of individuals > 65 years of age and female sex were independently associated with higher reporting. Older adults are particularly susceptible to AEs given pharmacokinetic/dynamic changes, polypharmacy, and comorbidities [47, 48]. Females may also be at greater risk for certain AEs [49, 50]; however, differences in willingness to report may also contribute to reporting observations [43]. While these associations were not unexpected, our finding that counties with higher proportions of uninsured individuals had higher reporting is less intuitive because uninsured individuals are less likely to fill prescriptions [51, 52]. One hypothesis is uninsured individuals may be more likely to experience preventable or severe AEs because they are less likely to have regular care [52, 53] where appropriate medication monitoring and management could occur; consequently, these individuals may have more compelling experiences to report. Alternatively, this finding may have been a chance finding.
4.1 Limitations
Our study has limitations. First, we limited our study to AE reports submitted directly to the FDA and excluded reports that pharmaceutical manufacturers sent to the FDA, which account for approximately 95% of AE reports in FAERS. Because these reports usually lack information about the person who sent the report to the manufacturer or their geographic location, county assignment was not possible. However, AE reports that manufacturers submit to FDA, like AE reports that consumer and HCPs submit directly to FDA, originate at the point of care, generally through patients and HCPs contacting the pharmaceutical manufacturer. To the extent that consumer engagement with the AE reporting system explains our findings, it is plausible that factors associated with decreased consumer reporting directly to the FDA would also apply to a consumer reporting AEs to manufacturers. Second, our drug utilization data did not account for products obtained over the counter, during an inpatient hospitalization, via mail order, or through other non-retail channels. Further, AE reporting probabilities may differ by medicine and severity; for instance, serious acute events are more likely to be reported than mild events with a prolonged onset. Thirdly, the data evaluated were not from recent years and thus avoided any impact COVID-19 may have had on reporting patterns [54] as well as the other datasets utilized in this study. To address concerns about generalizability, we subsequently evaluated the characteristics of reports received by FAERS in 2019 and found patterns to be largely consistent with earlier years (OSM Table 3). Data for all other data elements evaluated for the same time period (e.g., county-level prescriptions dispensed) were not readily available to repeat the multivariate analysis. Finally, due to the absence of individual-level reporter data, there is potential for ecological fallacy. County-level characteristics were ascribed to the individuals reporting the AE even though they may not accurately represent those individuals [32]. Individuals within a county can be highly heterogenous, but the use of more granular geographic areas was not feasible for this study.
Awareness, acceptability, and usability are critical factors for engagement in AE reporting systems [21, 55,56,57]. To that end, broad educational campaigns, transparency efforts, electronic reporting modes, and improvements to reporting forms have sought to improve engagement [20, 58, 59]. However, results from our study suggest targeted efforts would also be beneficial given the geographic and demographic reporting variations observed. The complexity of communities across the US and multifactorial nature of underlying healthcare disparities means there is not a singular solution for improving reporting. Approaches could include tailored educational materials with culturally appropriate messaging delivered through channels that match the preferences of each targeted population [60]. For some communities with lower reporting rates, such as those we observed with low English literacy, the translation of materials into native languages may be impactful. For others, different interventions, such as educational efforts to overcome trust barriers associated with sharing health information with authorities, may be warranted. Additional data on consumer beliefs, attitudes, and preferences among different communities is needed to inform individualized approaches.
For pharmacovigilance practitioners, understanding limitations in the representativeness of FAERS data underscores the importance of integrating data sources to gain a more comprehensive picture of a medicine’s safety profile. Leveraging other large, population-based healthcare databases, such as claims and electronic health records, can provide information on AEs on the population studied as a whole. To the extent that these databases contain information on the sociodemographic factors, they may be able to determine if such factors impact the development and characteristics of adverse reactions [61, 62]. Recently, the Medicines and Healthcare products Regulatory Agency and Genomics England initiated a novel project, Yellow Card Biobank, that will collect genetic samples from patients who have had certain AEs reported to the United Kingdom’s spontaneous reporting system [63]. Infrastructure advancements that enable the routine integration of complementary data sources like Biobank may strengthen our capacity to identify and assess emerging risks, further characterize known risks, and, ultimately, contribute to enhancing the safe use of medicines for individual patients.
5 Conclusions
Valuable drug safety insights are derived from spontaneous reporting systems; however, their data may not fully capture the diversity of the exposed population. Our study found variations in consumer AE reporting to FAERS that may be related to sociodemographic factors and healthcare access. Because these factors may also correspond to AE susceptibility, complementary data sources are needed for monitoring the safety of medicines among more vulnerable populations.
References
Dal Pan GJ, Lindquist M, Gelperin K. Postmarketing spontaneous pharmacovigilance reporting systems. In: Strom BL, Kimmel SE, Hennessy S, editors. Textbook of pharmacoepidemiology. 2021. pp. 113–35.
Kennedy-Martin T, Curtis S, Faries D, Robinson S, Johnston J. A literature review on the representativeness of randomized controlled trial samples and implications for the external validity of trial results. Trials. 2015;3(16):495.
Blanco C, Olfson M, Goodwin RD, Ogburn E, Liebowitz MR, Nunes EV, et al. Generalizability of clinical trial results for major depression to community samples: results from the National Epidemiologic Survey on alcohol and related conditions. J Clin Psychiatry. 2008;69(8):1276–80.
Tahhan AS, Vaduganathan M, Greene SJ, Alrohaibani A, Raad M, Gafeer M, et al. Enrollment of older patients, women, and racial/ethnic minority groups in contemporary acute coronary syndrome clinical trials: a systematic review. JAMA Cardiol. 2020;5(6):714–22.
Loree JM, Anand S, Dasari A, Unger JM, Gothwal A, Ellis LM, et al. Disparity of race reporting and representation in clinical trials leading to cancer drug approvals from 2008 to 2018. JAMA Oncol. 2019;5(10): e191870.
Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291(22):2720–6.
Chamberlain C, Kortepeter C, Muñoz M. Clinical analysis of adverse drug reactions and pharmacovigilance. In: Huang S-M, Lertora JJL, Vicini P, Atkinson AJ, editors. Atkinson's principles of clinical pharmacology. 2022. pp. 499–517.
Lester J, Neyarapally GA, Lipowski E, Graham CF, Hall M, Dal Pan G. Evaluation of FDA safety-related drug label changes in 2010. Pharmacoepidemiol Drug Saf. 2013;22(3):302–5.
Ishiguro C, Hall M, Neyarapally GA, Dal Pan G. Post-market drug safety evidence sources: an analysis of FDA drug safety communications. Pharmacoepidemiol Drug Saf. 2012;21(10):1134–6.
Croteau D, Pinnow E, Wu E, Munoz M, Bulatao I, Dal Pan G. Sources of evidence triggering and supporting safety-related labeling changes: a 10-year longitudinal assessment of 22 new molecular entities approved in 2008 by the US Food and Drug Administration. Drug Saf. 2022;45(2):169–80.
Best practices in drug and biological product postmarket safety surveillance for FDA staff. January 2024. Available: https://www.fda.gov/media/130216/download.
21 CFR 310.305 (prescription drugs marketed for human use without an approved application), 21 CFR 314.80 (human drugs with approved NDAs), 21 CFR 314.98 (human drugs with approved ANDAs), 21 CFR 600.80 (human biological products with approved BLAs), section 760 of the FD&C Act (nonprescription human drug products marketed without an approved application), and 21 CFR Part 4, Subpart B (combination products). Available: http://www.regulations.gov.
MedWatch: The FDA Safety Information and Adverse Event Reporting Program. Available: https://www.fda.gov/safety/medwatch-fda-safety-information-and-adverse-event-reporting-program. Accessed 4 July 2021.
Inacio P, Cavaco A, Airaksinen M. The value of patient reporting to the pharmacovigilance system: a systematic review. Br J Clin Pharmacol. 2017;83(2):227–46.
van Hunsel F, Harmark L, Rolfes L. Fifteen years of patient reporting—what have we learned and where are we heading to? Expert Opin Drug Saf. 2019;18(6):477–84.
Hazell L, Cornelius V, Hannaford P, Shakir S, Avery AJ, Yellow Card Study C. How do patients contribute to signal detection? A retrospective analysis of spontaneous reporting of adverse drug reactions in the UK’s Yellow Card Scheme. Drug Saf. 2013;36(3):199–206.
Harmark L, van Hunsel F, Grundmark B. ADR reporting by the general public: lessons learnt from the Dutch and Swedish systems. Drug Saf. 2015;38(4):337–47.
Harmark L, van Puijenbroek E, van Grootheest K. Intensive monitoring of duloxetine: results of a web-based intensive monitoring study. Eur J Clin Pharmacol. 2013;69(2):209–15.
Harmark L, van Puijenbroek E, Straus S, van Grootheest K. Intensive monitoring of pregabalin: results from an observational, web-based, prospective cohort study in the Netherlands using patients as a source of information. Drug Saf. 2011;34(3):221–31.
Munoz MA, Delcher C, Dal Pan GJ, Kortepeter CM, Wu E, Wei YJ, et al. Impact of a new consumer form on the quantity and quality of adverse event reports submitted to the United States Food and Drug Administration. Pharmacotherapy. 2019;39(11):1042–52.
Avery A, Anderson C, Bond C, Fortnum H, Gifford A. Evaluation of patient reporting of adverse drug reactions to the UK ‘Yellow Card Scheme’: literature review, descriptive and qualitative analyses, and questionnaire surveys. Health Technol Assess. 2011;15(20):234.
German RR, Lee LM, Horan JM, Milstein RL, Pertowski CA, Waller MN, et al. Updated guidelines for evaluating public health surveillance systems: recommendations from the Guidelines Working Group. MMWR Recomm Rep. 2001;50(RR-13):1–35.
McAdams M, Staffa J, Dal Pan G. Estimating the extent of reporting to FDA: a case study of statin-associated rhabdomyolysis. Pharmacoepidemiol Drug Saf. 2008;17(3):229–39.
Al Dweik R, Stacey D, Kohen D, Yaya S. Factors affecting patient reporting of adverse drug reactions: a systematic review. Br J Clin Pharmacol. 2017;83(4):875–83.
Agency for Healthcare Research and Quality. 2019 National Healthcare Quality and Disparities Report. Available: https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html. Accessed 5 Sept 2021.
Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003.
Serchen J, Doherty R, Atiq O, Hilden D, Health, Public Policy Committee of the American College of P. A comprehensive policy framework to understand and address disparities and discrimination in health and health care: a policy paper from the American College of Physicians. Ann Intern Med. 2021;174(4):529–32.
Hall-Lipsy EA, Chisholm-Burns MA. Pharmacotherapeutic disparities: racial, ethnic, and sex variations in medication treatment. Am J Health Syst Pharm. 2010;67(6):462–8.
McQuaid EL, Landier W. Cultural issues in medication adherence: disparities and directions. J Gen Intern Med. 2018;33(2):200–6.
FDA Adverse Event Reporting System (FAERS) Public Dashboard. Available: https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Surveillance/AdverseDrugEffects/ucm070093.htm. Accessed: 13 Feb 2022.
International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH). Efficacy guidelines. Available: https://www.ich.org/page/efficacy-guidelines. Accessed: 21 Feb 2022.
MedWatch forms for FDA safety reporting. Available: https://www.fda.gov/Safety/MedWatch/HowToReport/DownloadForms/default.htm. Accessed 8 Mar 2022.
HUD USPS ZIP Code Crosswalk Files. U.S. Department of Housing and Urban Development. Available: https://www.huduser.gov/portal/datasets/usps_crosswalk.html. Accessed 4 Feb 2018.
County Health Rankings & Roadmaps. Robert Wood Johnson Foundation and University of Wisconsin Population Health Institute. Available: http://www.countyhealthrankings.org/. Accessed 6 Aug 2017.
Symphony Health Integrated Dataverse Placeholder. To be updated.
United States Census Bureau. American FactFinder. Available: https://factfinder.census.gov/. Accessed 4 June 2017.
Agency Information Collection Activities; Submission for Office of Management and Budget Review; Comment Request; MedWatch: The Food and Drug Administration Medical Products Reporting Program. Available: https://www.regulations.gov/document?D=FDA-2014-N-1960-0002. Accessed 6 Aug 2017.
21 CFR 201.57. Specific requirements on content and format of labeling for human prescription drug and biological products described in § 201.56(b)(1). Available: https://www.ecfr.gov/current/title-21/chapter-I/subchapter-C/part-201/subpart-B/section-201.57. Accessed 4 Apr 2023.
The Food and Drug Administration Amendments Act of 2007 (Public Law 110-85), amending the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. §301.
Rikard RV, Thompson MS, McKinney J, Beauchamp A. Examining health literacy disparities in the United States: a third look at the National Assessment of Adult Literacy (NAAL). BMC Public Health. 2016;13(16):975.
Sentell T, Braun KL. Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. J Health Commun. 2012;17(Suppl 3):82–99.
United States Federal Register. Agency Information Collection Activities; Proposed Collection; Comment Request; MedWatch: The Food and Drug Administration Medical Products Reporting Program. Available: https://www.federalregister.gov/documents/2021/06/30/2021-13943/agency-information-collection-activities-proposed-collection-comment-request-medwatch-the-food-and. Accessed 12 Sept 2021.
Watson S, Caster O, Rochon PA, den Ruijter H. Reported adverse drug reactions in women and men: aggregated evidence from globally collected individual case reports during half a century. EClinicalMedicine. 2019;17: 100188.
Bolin JN, Bellamy G, Ferdinand AO, Kash BA, Helduser JW, editors. Rural healthy people 2020, vol 1. College Station: Texas A&M Health Science Center School of Public Health, Southwest Rural Health Research Center; 2015. Available: https://srhrc.tamhsc.edu/docs/rhp2020-volume-1.pdf. Accessed: 15 Apr 2018.
Inacio P, Gomes JJ, Airaksinen M, Cavaco A. Exploring sociodemographic and economic factors that promote adverse drug reactions reporting by patients. Health Policy. 2018;122(3):263–8.
Kivistö KT, Kantola T, Neuvonen PJ. Different effects of itraconazole on the pharmacokinetics of fluvastatin and lovastatin. Br J Clin Pharmacol. 1998;46(1):49–53.
Yadesa TM, Kitutu FE, Deyno S, Ogwang PE, Tamukong R, Alele PE. Prevalence, characteristics and predicting risk factors of adverse drug reactions among hospitalized older adults: a systematic review and meta-analysis. SAGE Open Med. 2021;9:20503121211039100.
Lavan AH, Gallagher P. Predicting risk of adverse drug reactions in older adults. Ther Adv Drug Saf. 2016;7(1):11–22.
Jenkins MR, Munoz MA, Bak D, Chai G, Ready T, South EM, et al. Food and Drug Administration beyond the 2001 Government Accountability Office Report: promoting drug safety for women. J Womens Health (Larchmt). 2021;30(7):927–34.
FDA Drug Safety Communication. Risk of next-morning impairment after use of insomnia drugs; FDA requires lower recommended doses for certain drugs containing zolpidem (Ambien, Ambien CR, Edluar, and Zolpimist). Available: https://wayback.archive-it.org/7993/20170404172106/https://www.fda.gov/Drugs/DrugSafety/ucm334033.htm. Accessed 19 Mar 2022.
Cohen RA, Boersma P, Vahratian A. Strategies used by adults aged 18–64 to reduce their prescription drug costs, 2017. NCHS Data Brief. 2019;333:1–8.
Institute of Medicine (US) Committee on the Consequences of Uninsurance. Care without coverage: too little, too late. National Academies Press (US); 2002. https://doi.org/10.17226/10367.
Woolhandler S, Himmelstein DU. The relationship of health insurance and mortality: is lack of insurance deadly? Ann Intern Med. 2017;167(6):424–31.
Diak IL, Swank K, McCartan K, Beganovic M, Kidd J, Gada N, et al. The Food and Drug Administration’s (FDA’s) drug safety surveillance during the COVID-19 pandemic. Drug Saf. 2023;46(2):145–55.
Inman WH. Attitudes to adverse drug reaction reporting. Br J Clin Pharmacol. 1996;41(5):434–5.
Lopez-Gonzalez E, Herdeiro MT, Figueiras A. Determinants of under-reporting of adverse drug reactions: a systematic review. Drug Saf. 2009;32(1):19–31.
van Hunsel F, van der Welle C, Passier A, van Puijenbroek E, van Grootheest K. Motives for reporting adverse drug reactions by patient-reporters in the Netherlands. Eur J Clin Pharmacol. 2010;66(11):1143–50.
Du D, Goldsmith J, Aikin KJ, Encinosa WE, Nardinelli C. Despite 2007 law requiring FDA hotline to be included in print drug ads, reporting of adverse events by consumers still low. Health Aff (Millwood). 2012;31(5):1022–9.
Rose BJ, Fritsch BF. FDA's MedWatch program turns 20: what's new? American Pharmacist Association: Pharmacy Today. Available: http://www.pharmacist.com/fdas-medwatch-program-turns-20-whats-new Accessed: 23 Apr 2017.
Spinner JR, Haynes E, Nunez C, Baskerville S, Bravo K, Araojo RR. Enhancing FDA’s reach to minorities and under-represented groups through training: developing culturally competent health education materials. J Prim Care Community Health. 2021;12:21501327211003690.
Wong A, Seger DL, Lai KH, Goss FR, Blumenthal KG, Zhou L. Drug hypersensitivity reactions documented in electronic health records within a large health system. J Allergy Clin Immunol Pract. 2019;7(4):1253–60.
Sato T, Cheng CL, Park HW, Kao Yang YH, Yang MS, Fujita M, et al. Real-world evidence of population differences in allopurinol-related severe cutaneous adverse reactions in East Asians: a population-based cohort study. Clin Transl Sci. 2021;14(3):1002–14.
Medicines and Healthcare products Regulatory Agency. Yellow Card Biobank. Available: https://yellowcard.mhra.gov.uk/biobank. Accessed: 10 Dec 2023.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were received for the preparation of this article.
Conflict of interest
None of the authors has any conflicts of interest to disclose.
Availability of data and material
The FAERS data are available via the FAERS Public Dashboard and as Quarterly Data files. Additionally, individual case reports can be requested via a Freedom of Information Act request to the FDA. Additional details can be found at: https://www.fda.gov/drugs/surveillance/questions-and-answers-fdas-adverse-event-reporting-system-faers. County Health Rankings and Roadmaps data are available for download at: https://www.countyhealthrankings.org/.
Ethics approval
This study was approved by both the US FDA’s and University of Florida’s Institutional Review Boards (approval numbers: 18-051D, 201802111).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
The analytic code can be made available upon request to the corresponding author.
Author contributions
Study conceptualization: MAM, GDP, YJW, HX, CD, AGW; data analysis: MAM, AG, NS; interpretation of the data (all authors); All authors contributed to and approved the final version of the manuscript.
Disclaimer
The views expressed are those of the authors and do not necessarily represent the position of, nor imply endorsement from, the US Food and Drug Administration or the US Government.
Additional information
Hong Xiao was employed by the University of Florida when this research was conceived and conducted.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Muñoz, M.A., Dal Pan, G.J., Wei, YJ.J. et al. Sociodemographic Characteristics of Adverse Event Reporting in the USA: An Ecologic Study. Drug Saf 47, 377–387 (2024). https://doi.org/10.1007/s40264-024-01397-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-024-01397-6